Efficacy of Small Incision Cataract Surgery: A Multicenter Retrospective Study of Visual Outcomes in Coastal Ecuador
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
More Results
4. Discussion
5. Clinical Implications
6. Suggestions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Foster, A.; Resnikoff, S. The Impact of Vision 2020 on Global Blindness. Eye 2005, 19, 1133–1135. [Google Scholar] [CrossRef]
- Resnikoff, S.; Pascolini, D.; Etya’Ale, D.; Kocur, I.; Pararajasegaram, R.; Pokharel, G.P.; Mariotti, S.P. Global Data on Visual Impairment in the Year 2002. Bull. World Health Organ. 2004, 82, 844–851. [Google Scholar]
- World Health Organization. World Report on Vision; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Bourne, R.R.A.; Steinmetz, J.D.; Flaxman, S.R.; Briant, P.S.; Taylor, H.R.; Resnikoff, S.; Casson, R.J.; Abdoli, A.; Abu-Gharbieh, E.; Afshin, A.; et al. Trends in Prevalence of Blindness and Distance and near Vision Impairment over 30 Years. Lancet Glob. Health 2021, 9, e130–e143. [Google Scholar] [CrossRef] [PubMed]
- Ologunde, R.; Maruthappu, M.; Shanmugarajah, K.; Shalhoub, J. Surgical care in low and middle-income countries: Burden and barriers. Int. J. Surg. 2014, 12, 858–863. [Google Scholar] [CrossRef]
- Riaz, Y.; Mehta, J.S.; Wormald, R.; Evans, J.R.; Foster, A.; Ravilla, T.; Snellingen, T. Surgical Interventions for Age-related Cataract. Cochrane Database Syst. Rev. 2006, 2, CD001323. [Google Scholar] [CrossRef] [PubMed]
- Limburg, H.; Foster, A. Cataract Surgical Coverage: Results from Population-Based Studies. Bull. World Health Organ. 1998, 76, 350–360. [Google Scholar]
- Alkire, B.C.; Raykar, N.P.; Shrime, M.G.; Weiser, T.G.; Bickler, S.W.; Rose, J.A.; Nutt, C.T.; Greenberg, S.L.M.; Kotagal, M.; Riesel, J.N. Global Access to Surgical Care: A Modelling Study. Lancet Glob. Health 2015, 3, e316–e323. [Google Scholar] [CrossRef]
- Meara, J.G.; Leather, A.J.M.; Hagander, L.; Alkire, B.C.; Alonso, N.; Ameh, E.A.; Bickler, S.W.; Conteh, L.; Dare, A.J.; Davies, J. Global Surgery 2030: Evidence and Solutions for Achieving Health, Welfare, and Economic Development. Lancet 2015, 386, 569–624. [Google Scholar] [CrossRef]
- Mock, C.N.; Donkor, P.; Gawande, A.; Jamison, D.T.; Kruk, M.E.; Debas, H.T. Essential Surgery: Key Messages from Disease Control Priorities. Lancet 2015, 385, 2209–2219. [Google Scholar] [CrossRef]
- Limburg, H.; Foster, A. Cataract Surgical Coverage: An Indicator to Measure the Impact of Cataract Intervention Programmes. Community Eye Health 1998, 11, 3. [Google Scholar]
- Duerksen, R.; Limburg, H.; Carron, J.E.; Foster, A. Cataract Blindness in Paraguay–Results of a National Survey. Ophthalmic Epidemiol. 2003, 10, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Duerksen, R.; Limburg, H.; Carron, J.E.; Foster, A. Cataract Blindness and Surgical Outcomes in Paraguay. Br. J. Ophthalmol. 2018, 92, 232–235. [Google Scholar]
- Reis, T.; Lansingh, V.; Ramke, J.; Silva, J.C.; Resnikoff, S.; Furtado, J.M. Cataract as a Cause of Blindness and Vision Impairment in Latin America: Progress Made and Challenges Beyond 2020. Am J. Ophthalmol. 2021, 225, 1–10. [Google Scholar] [CrossRef]
- Wang, W.; Yan, W.; Müller, A.; He, M. A Global View on Output and Outcomes of Cataract Surgery With National Indices of Socioeconomic Development. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3669–3676. [Google Scholar]
- Congdon, N.; O’Colmain, B.; Klaver, C.C.; Klein, R.; Muñoz, B.; Friedman, D.S.; Kempen, J.; Taylor, H.R.; Mitchell, P. Causes and Prevalence of Visual Impairment among Adults in the United States. Arch. Ophthalmol. 2003, 121, 487–494. [Google Scholar]
- Foster, A. Cataract and Vision 2020—The Right to Sight Initiative. Br. J. Ophthalmol. 2001, 85, 635–637. [Google Scholar] [CrossRef]
- Ang, M.; Evans, J.R.; Mehta, J.S. Manual Small Incision Cataract Surgery (MSICS) with Posterior Chamber Intraocular Lens versus Extracapsular Cataract Extraction (ECCE) with Posterior Chamber Intraocular Lens for Age-Related Cataract. Cochrane Database Syst. Rev. 2014, 11, CD008811. [Google Scholar] [CrossRef]
- Gogate, P.; Deshpande, M.; Nirmalan, P.K. Why Do Phacoemulsification? Manual Small Incision Cataract Surgery Is Almost as Effective, but Less Expensive. Br. J. Ophthalmol. 2010, 94, 545–546. [Google Scholar] [CrossRef]
- Ackland, P.; Resnikoff, S.; Bourne, R.R.A. World Blindness and Visual Impairment: Despite Many Successes, the Problem Is Growing. Community Eye Health J. 2017, 30, 71–73. [Google Scholar]
- Murthy, G.V.S.; Gupta, S.; John, N. The Quality of Cataract Surgery in India: A Multicenter Study. Ophthalmic Epidemiol. 2010, 17, 405–414. [Google Scholar]
- Instituto Nacional de Estadística y Censos del Ecuador. Estadísticas de Salud: Morbilidad Hospitalaria; Instituto Nacional de Estadística y Censos del Ecuador: Quito, Ecuador, 2020. [Google Scholar]
- Ministerio de Salud Pública del Ecuador. Indicadores de Salud Visual y Atención Oftalmológica; Ministerio de Salud Pública del Ecuador: Quito, Ecuador, 2022. [Google Scholar]
- Sharma, P.; Thanikachalam, S.; Kedar, S.; Bhola, R. Evaluation of subjective and objective cyclodeviation following oblique muscle weakening procedures. Indian J. Ophthalmol. 2008, 56, 39–43. [Google Scholar] [CrossRef]
- Savini, G.; Barboni, P.; Carbonelli, M.; Hoffer, K.J. Accuracy of corneal power measurements by a new Scheimpflug camera combined with Placido-disk corneal topography for intraocular lens power calculation in unoperated eyes. J. Cataract. Refract. Surg. 2012, 38, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Matta, S.; Kumar, M.; Vashist, P. Cataract Surgery Visual Outcomes and Associated Risk Factors in a Large Community Eye Care Center. PLoS ONE 2016, 11, e0144853. [Google Scholar] [CrossRef] [PubMed]
- Ruit, S.; Tabin, G.; Chang, D.; Bajracharya, L.; Kline, D.C.; Richheimer, W.; Shrestha, M.; Paudyal, G. A Prospective Randomized Clinical Trial of Phacoemulsification versus Manual Sutureless Small-Incision Extracapsular Cataract Surgery in Nepal. Am. J. Ophthalmol. 2007, 143, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Thulasiraj, R. Monitoring Cataract Surgical Outcomes in India: The Aravind Approach. Community Eye Health J. 2003, 16, 58–59. [Google Scholar]
- Lewallen, S.; Courtright, P. Gender and use of cataract surgical services in developing countries. Bull. World Health Organ. 2002, 80, 300–303. [Google Scholar]
- Yorston, D. Cataract Complications. Community Eye Health 2003, 16, 44–45. [Google Scholar]
- Lansingh, V.C.; Carter, M.J.; Martens, M. Global Cost-Effectiveness of Cataract Surgery. Ophthalmology 2007, 114, 1670–1678. [Google Scholar] [CrossRef]
- He, M.; Huang, W.; Zheng, Y. Prevalence and Associations of Cataract in the Adult Population in Rural Southern China: The Liwan Eye Study. Investig. Ophthalmol. Vis. Sci. 2007, 48, 4811–4817. [Google Scholar]
- Venkatesh, R.; Muralikrishnan, R.; Balent, L.C.; Prakash, S.K.; Prajna, N.V. Outcomes of high volume cataract surgeries in a developing country. Br. J. Ophthalmol. 2005, 89, 1079–1083. [Google Scholar] [CrossRef]
- Nirmalan, P.K.; Katz, J.; Robin, A.L.; Krishnadas, R.; Ramakrishnan, R.; Thulasiraj, R.D.; Tielsch, J. Utilisation of Eye Care Services in Rural South India: The Aravind Comprehensive Eye Survey. Br. J. Ophthalmol. 2004, 88, 1237–1241. [Google Scholar] [CrossRef] [PubMed]
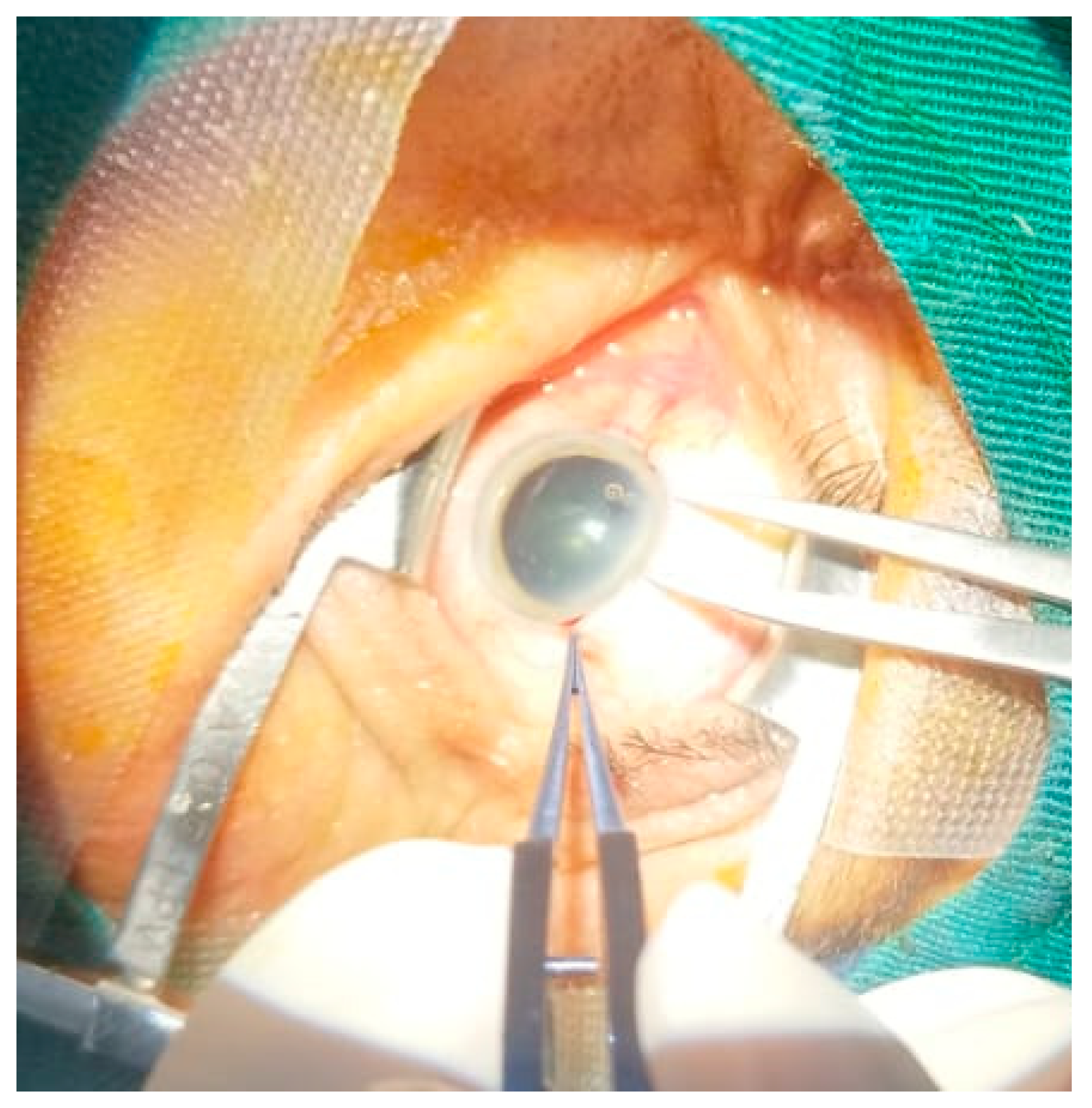
- Berrones, D.; Rocha-de-Lossada, C.; Barraquer-Compte, E.; Valvecchia, G.; Fernández, J. Implementation of SICS (Small Incision Cataract Surgery) in Humanitarian Campaigns: Description of the Surgical Technique and Review of the Literature. Arch. Soc. Esp. Oftalmol. 2025, 100, 91–97. [Google Scholar] [CrossRef]

| Sociodemographic Background | N = 558 (%) | (χ2; gl; p-Value) | |
|---|---|---|---|
| OD | OI | ||
| Age | 20.03; 10; 0.029 | 17.81; 10; 0.058 | |
| 30–39 | 4 (0.7%) | ||
| 40–49 | 12 (2.2%) | ||
| 50–59 | 46 (8.2%) | ||
| 60–69 | 161 (28.9%) | ||
| 70–79 | 260 (46.6%) | ||
| 80≥ | 75 (13.4%) | ||
| Sex | 0.375; 2; 0.829 | 4.27; 2; 0. 1118 | |
| Male | 280 (50.2%) | ||
| Female | 278 (49.8%) | ||
| Zone | 0.37; 2; 0.0829 | 4.27; 2; 0.118 | |
| Rural | 212 (38.0%) | ||
| Urban | 346 (62.0%) | ||
| HTN (hypertension) | 0.636; 2; 0.729 | 1.08; 2; 0.580 | |
| Yes | 237 (42.5%) | ||
| No | 321 (57.5%) | ||
| Dbts (diabetes mellitus) | 4.49; 2; 0.106 | 0.85; 2; 0.653 | |
| Yes | 370 (66.3%) | 20.03; 10; 0.029 | 17.81; 10; 0.058 |
| No | 188 (33.7%) | ||
| Mean | 95% IC | t | gl | Sig. (Bilateral) | |||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Pair 1 | BEFORE CX (OD)–AFTER CX (OD) | 0.5252 | 0.4837 | 0.5667 | 24.872 | 557 | 0 |
| Pair 2 | BEFORE CX (OI)–AFTER CX (OI) | 0.4894 | 0.4481 | 0.5307 | 23.251 | 557 | 0 |
| Sum of Squares | gl | Mean Square | F | Sig. | |
|---|---|---|---|---|---|
| Between groups | 5.999 | 51 | 0.4837 | 1.386 | 0.045 |
| Within groups | 42.935 | 506 | 0.4481 | ||
| Total | 48.934 | 557 |
| Sum of Squares | gl | Mean Square | F | Sig. | |
|---|---|---|---|---|---|
| Between groups | 5.425 | 51 | 0.106 | 1.102 | 0.298 |
| Within groups | 48.838 | 506 | 0.097 | ||
| Total | 54.264 | 557 |
| Sociodemographic Background | Average (>0.3) | Bad (≤1.0) | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value | |
| Lower Upper | Lower Upper | |||||
| Age groups | ||||||
| (30–39) | 593,216,596 | 199.45–542.3 | 0 | 3544 | 543.6–543.6 | |
| (40–49) | 0.265 | 0.030–2.349 | 0.233 | 3.82 | 0.915–15.951 | 0.066 |
| (50–59) | 1.027 | 0.451–2.341 | 0.949 | 2.19 | 0.730–6.574 | 0.162 |
| (60–69) | 1.592 | 0.870–2.912 | 0.131 | 2.084 | 0.851–5.104 | 0.108 |
| (70–79) | 1.23 | 0.704–2.149 | 0.466 | 1.388 | 0.590–3.268 | 0.453 |
| 80≥ | Reference | Reference | Reference | Reference | Reference | Reference |
| Sex | ||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | 0.871 | 0.520–1.459 | 0.6 | 0.572 | 0.339–0.964 | 0.036 |
| Zone | ||||||
| Urban | Reference | Reference | Reference | Reference | Reference | Reference |
| Rural | 0.744 | 0.508–1.089 | 0.128 | 1.179 | 0.706–1.967 | 0.53 |
| Dbts (diabetes mellitus) | ||||||
| Yes | Reference | Reference | Reference | Reference | Reference | Reference |
| No | 1.243 | 0.832–1.857 | 0.287 | 1.226 | 0.702–2.140 | 0.474 |
| HTN (hypertension) | ||||||
| Yes | Reference | Reference | Reference | Reference | Reference | Reference |
| No | 0.953 | 0.651–1.396 | 0.806 | 1.113 | 0.660–1.876 | 0.688 |
| Sociodemographic Background | Average (>0.3) | Bad (≤1.0) | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value | |
| Lower Upper | Lower Upper | |||||
| Age groups | ||||||
| (30–39) | 1.479 | 0.193–11.353 | 0.706 | 1.12E−08 | 0.000–0.000 | - |
| (40–49) | 0.802 | 0.180–3.569 | 0.772 | 1.35 | 0.289–6.313 | 0.703 |
| (50–59) | 1.604 | 0.688–3.741 | 0.274 | 1.774 | 0.659–4.778 | 0.257 |
| (60–69) | 2.663 | 1.4226–4.973 | 0.002 | 1.086 | 0.479–2.463 | 0.843 |
| (70–79) | 1.496 | 0.841–2.663 | 0.171 | 0.63 | 0.294–1.350 | 0.235 |
| 80≥ | Reference | Reference | Reference | Reference | Reference | Reference |
| Sex | ||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | 0.956 | 0.664–1.377 | 0.81 | 1.1 | 0.646–1.874 | 0.725 |
| Zone | ||||||
| Urban | Reference | Reference | Reference | Reference | Reference | Reference |
| Rural | 1.079 | 0.741–1.571 | 0.693 | 1.13 | 0.659–1.938 | 0.657 |
| Dbts (diabetes mellitus) | ||||||
| Yes | Reference | Reference | Reference | Reference | Reference | Reference |
| No | 1.624 | 1.085–2.432 | 0.018 | 0.942 | 0.536–1.654 | 0.835 |
| HTN (hypertension) | ||||||
| Yes | Reference | Reference | Reference | Reference | Reference | Reference |
| No | 1.006 | 0.690–1.466 | 0.977 | 1.173 | 0.678–2.031 | 0.568 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alcívar-Viteri, R.E.; Moreira-Pico, V.D.; Gómez-Cedeño, C.I.; Duran-Ospina, J.P.; Siteneski, A.; Montes-Escobar, K. Efficacy of Small Incision Cataract Surgery: A Multicenter Retrospective Study of Visual Outcomes in Coastal Ecuador. Vision 2025, 9, 60. https://doi.org/10.3390/vision9030060
Alcívar-Viteri RE, Moreira-Pico VD, Gómez-Cedeño CI, Duran-Ospina JP, Siteneski A, Montes-Escobar K. Efficacy of Small Incision Cataract Surgery: A Multicenter Retrospective Study of Visual Outcomes in Coastal Ecuador. Vision. 2025; 9(3):60. https://doi.org/10.3390/vision9030060
Chicago/Turabian StyleAlcívar-Viteri, Roberto Ernesto, Verónica Dolores Moreira-Pico, Carlos Iván Gómez-Cedeño, Julia Patricia Duran-Ospina, Aline Siteneski, and Karime Montes-Escobar. 2025. "Efficacy of Small Incision Cataract Surgery: A Multicenter Retrospective Study of Visual Outcomes in Coastal Ecuador" Vision 9, no. 3: 60. https://doi.org/10.3390/vision9030060
APA StyleAlcívar-Viteri, R. E., Moreira-Pico, V. D., Gómez-Cedeño, C. I., Duran-Ospina, J. P., Siteneski, A., & Montes-Escobar, K. (2025). Efficacy of Small Incision Cataract Surgery: A Multicenter Retrospective Study of Visual Outcomes in Coastal Ecuador. Vision, 9(3), 60. https://doi.org/10.3390/vision9030060






