Unveiling Visual Acuity in 58,712 Four-Year-Olds: Standardized Assessment Defined Normative Visual Acuity Threshold
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size
2.1.1. CRO–READ
2.1.2. Visual Acuity Testing
2.1.3. Definition of Unremarkable Result, Amblyopia, Incorrectly Coded Data, Referral Criteria, and Testability
2.1.4. Exclusion Criteria
2.2. Outcome Measures
2.3. Data Analysis
3. Results
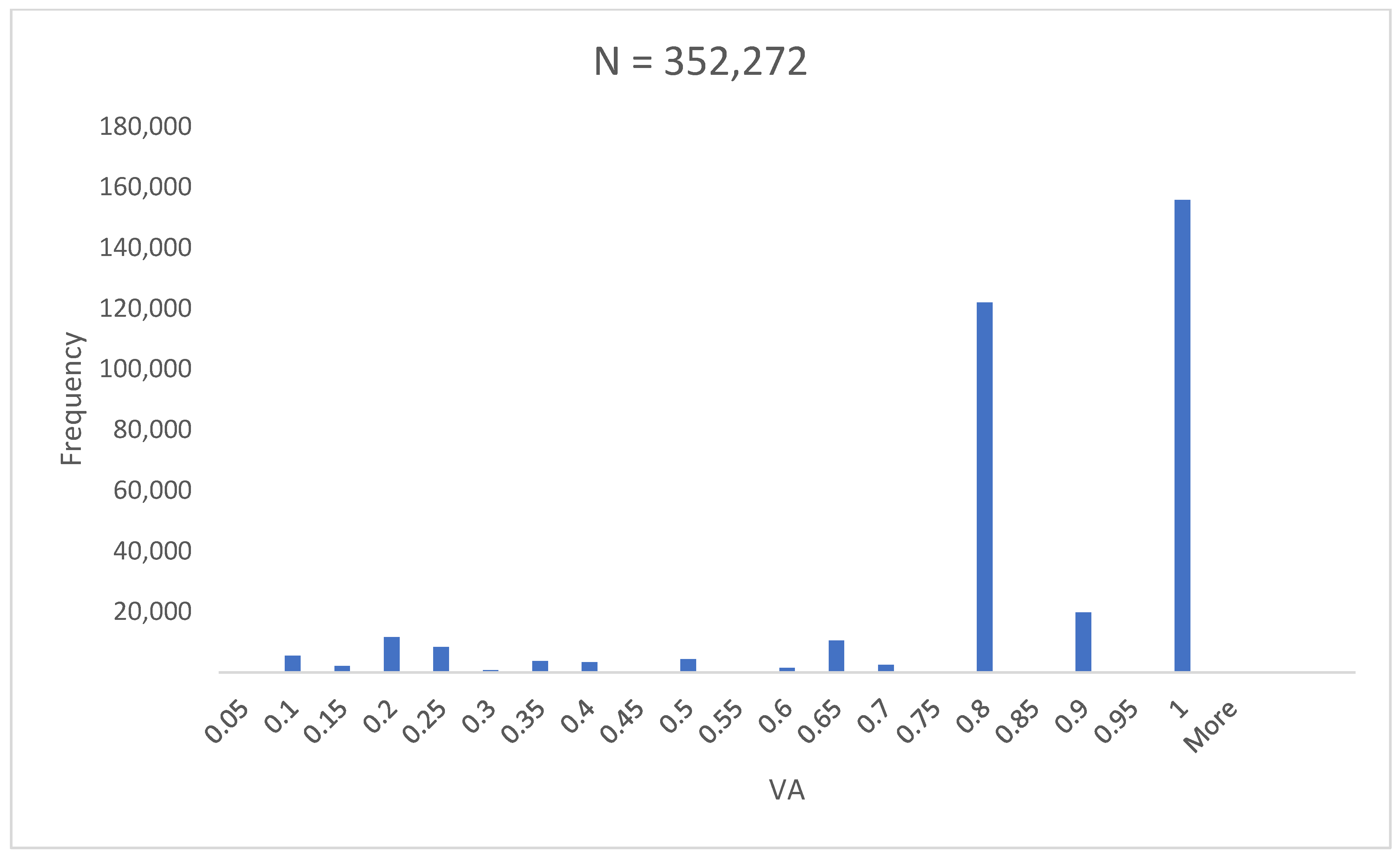
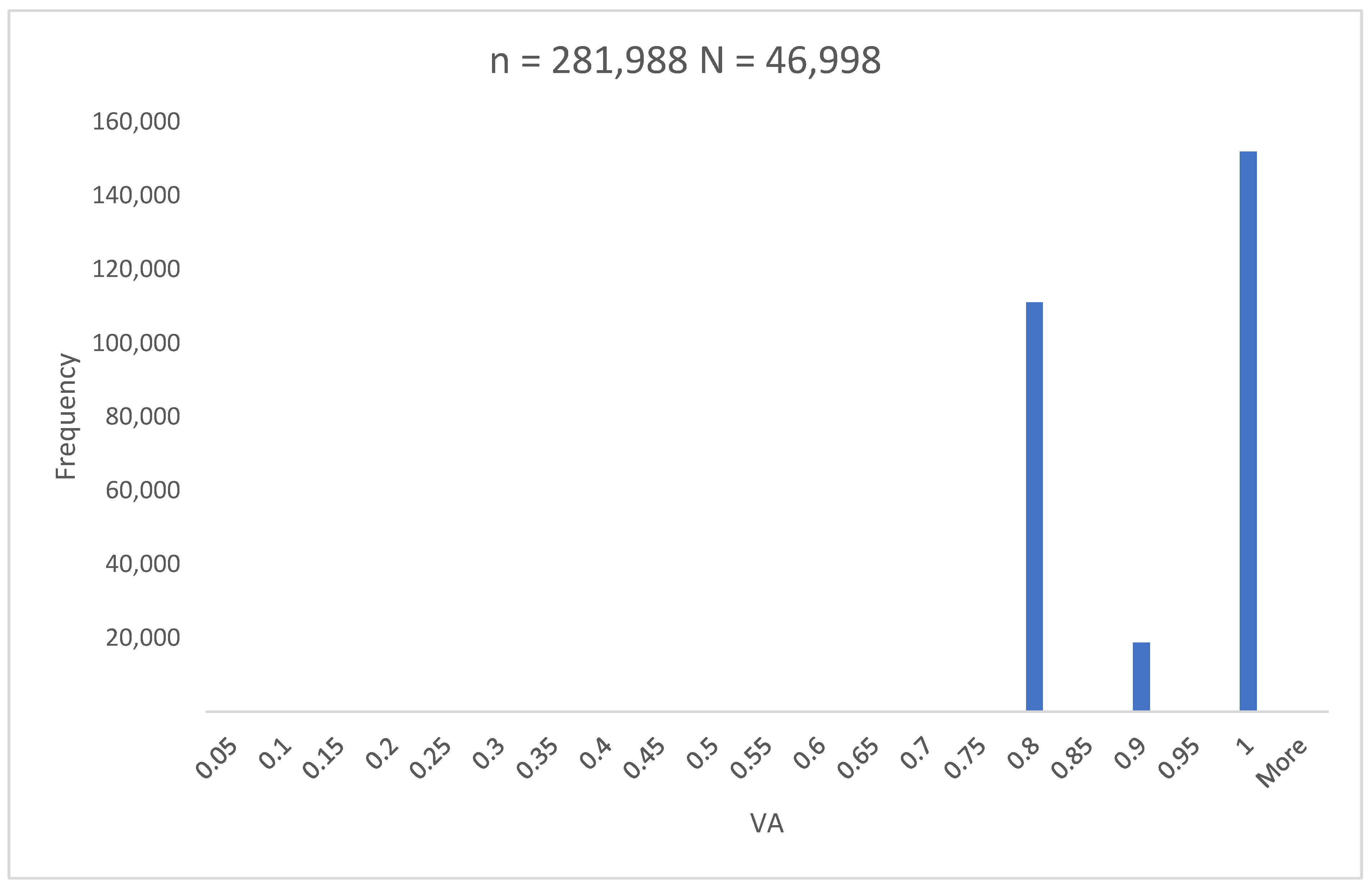
3.1. Sample Size
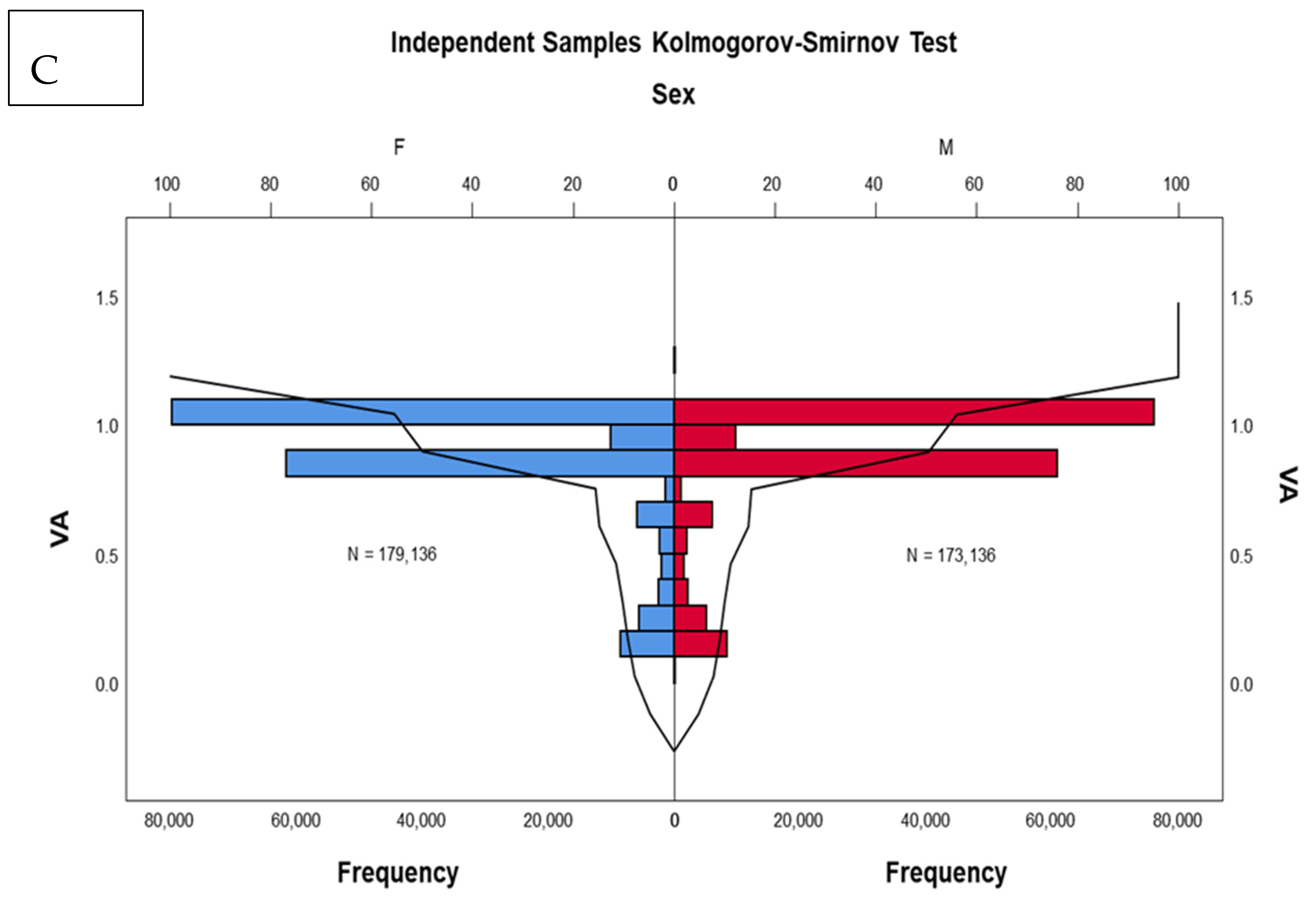
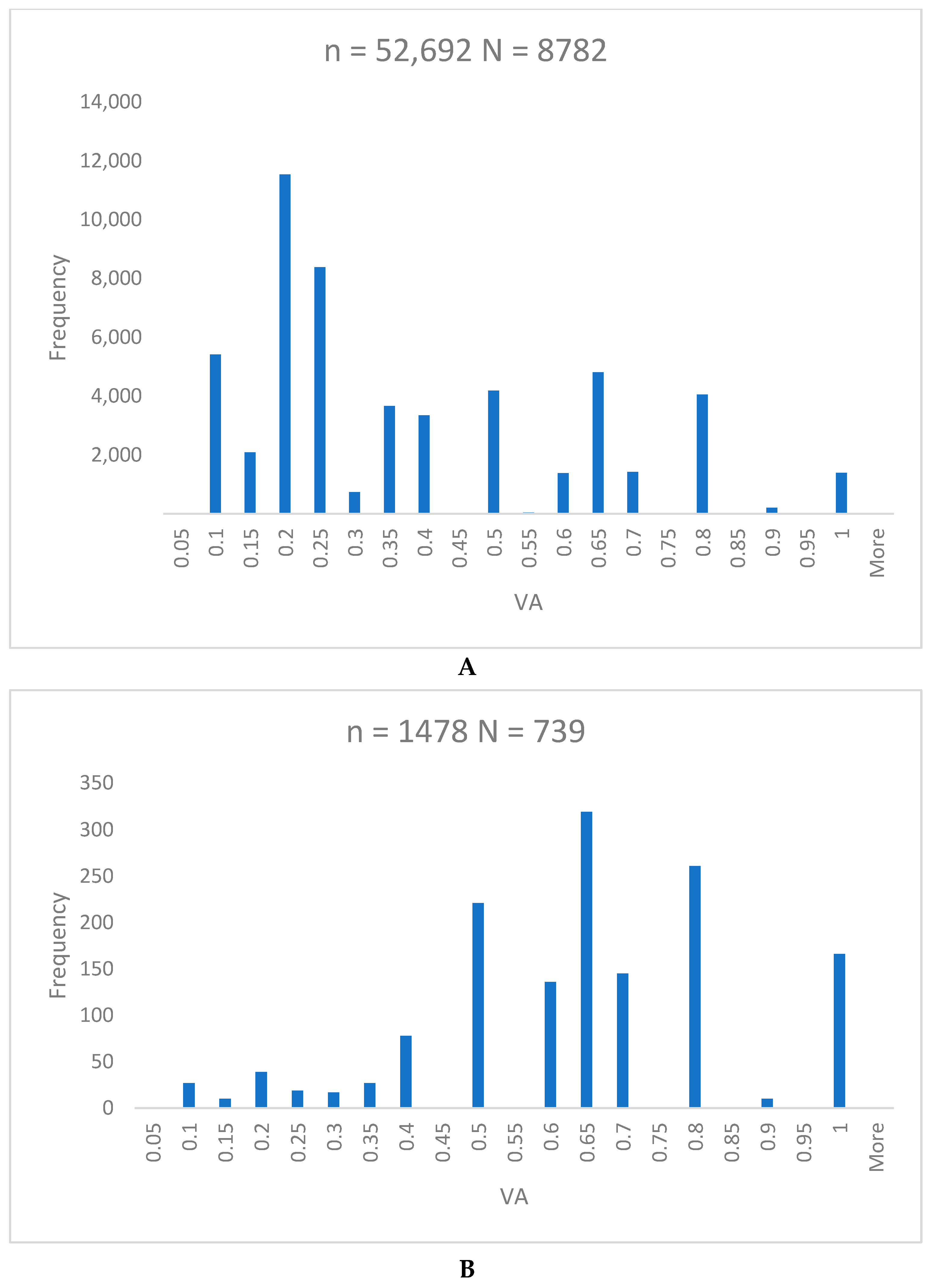
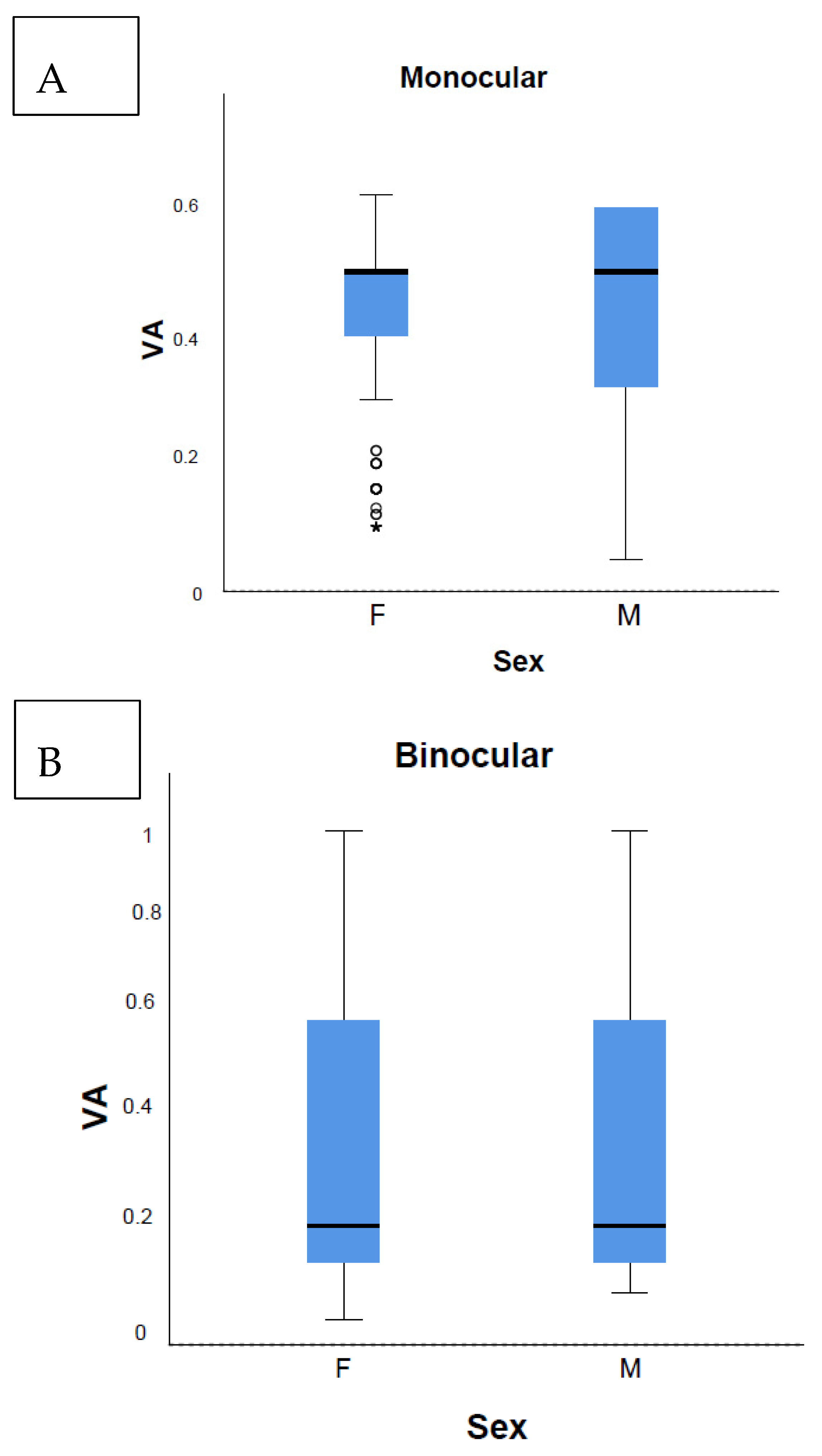
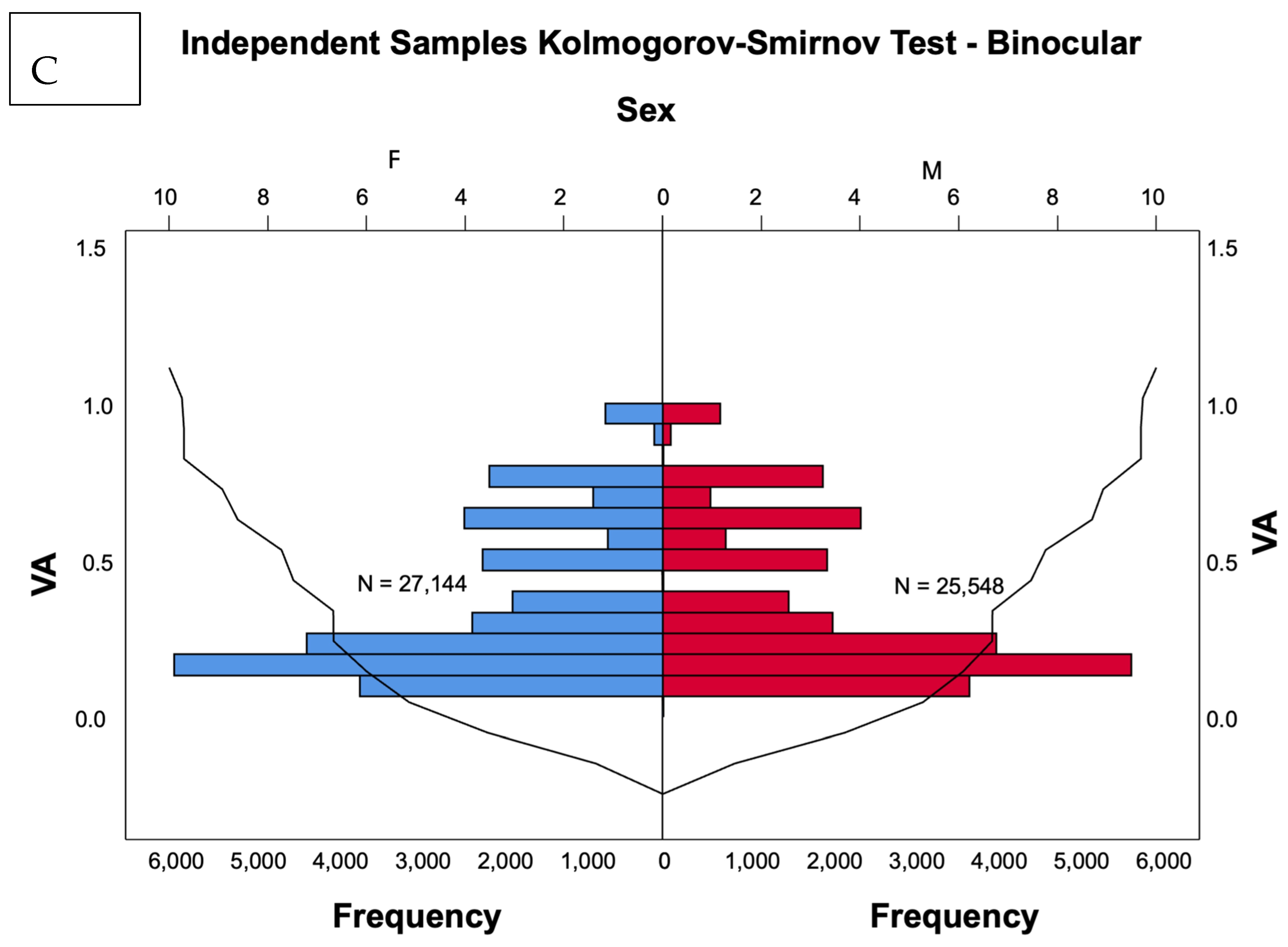
3.2. Primary Outcomes
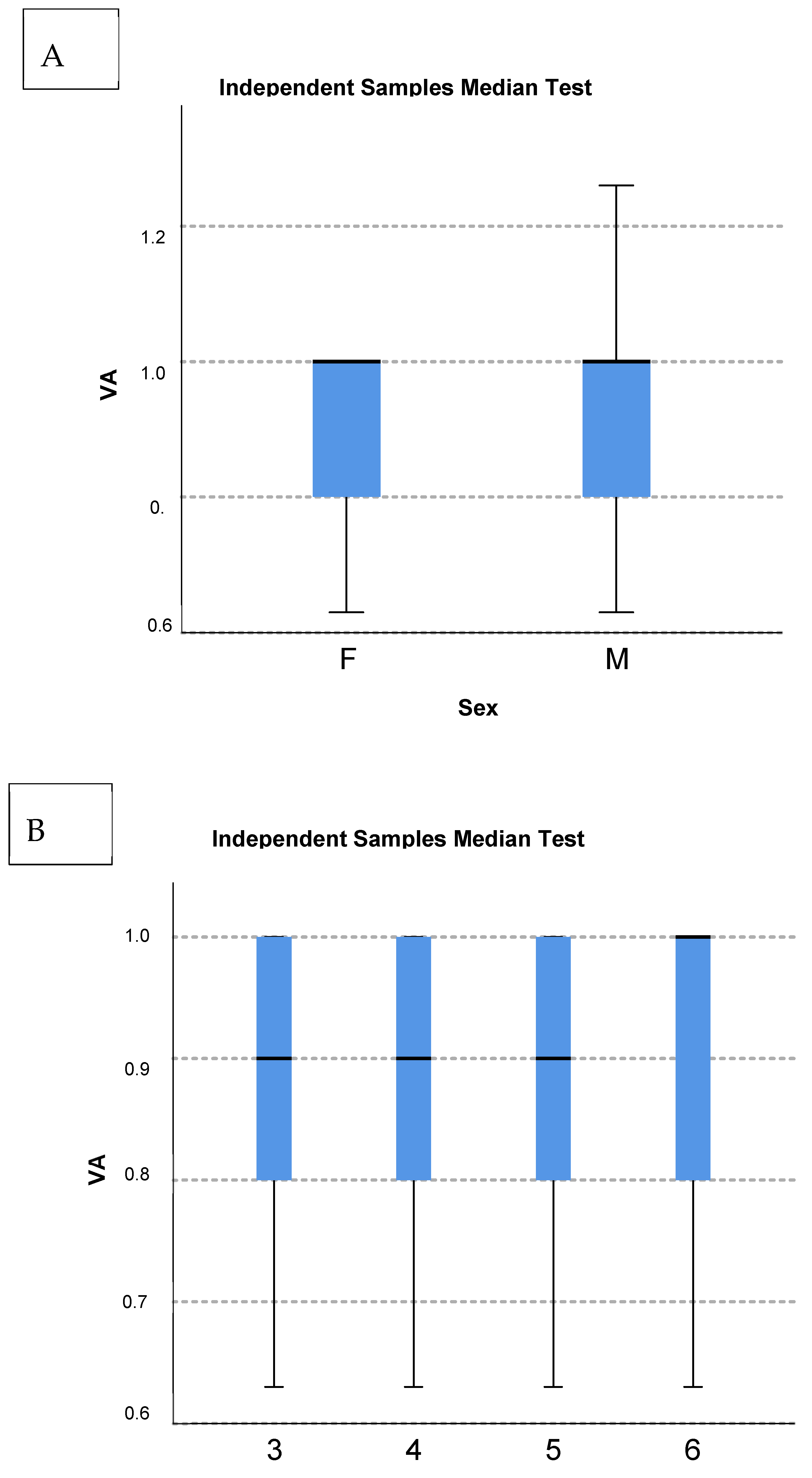
3.3. Secondary Outcomes
Non-Testable Children
4. Discussion
4.1. Age-Specific Normative Visual Acuity
4.2. Development of Vision and Amblyopia Prevalence
4.3. Testability, Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Report on Vision. Available online: https://www.who.int/publications/i/item/9789241516570 (accessed on 28 April 2024).
- World Health Organization. Blindness and Vision Impairment. Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 27 April 2024).
- Birch, E.E. Amblyopia and binocular vision. Prog. Retin. Eye Res. 2013, 33, 67–84. [Google Scholar] [CrossRef]
- Kates, M.M.; Beal, C.J. Amblyopia. JAMA 2021, 325, 408. [Google Scholar] [CrossRef]
- Hu, B.; Liu, Z.; Zhao, J.; Zeng, L.; Hao, G.; Shui, D.; Mao, K. The Global Prevalence of Amblyopia in Children: A Systematic Review and Meta-Analysis. Front. Pediatr. 2022, 10, 819998. [Google Scholar] [CrossRef]
- Chen, A.H.; Abu Bakar, N.F.; Arthur, P. Comparison of the pediatric vision screening program in 18 countries across five continents. J. Curr. Ophthalmol. 2019, 31, 357–365. [Google Scholar] [CrossRef]
- Sloot, F.; Hoeve, H.L.; de Kroon, M.L.; Goedegebure, A.; Carlton, J.; Griffiths, H.J.; Simonsz, H.J.; EUS€REEN Study Group. Inventory of current EU paediatric vision and hearing screening programmes. J. Med. Screen. 2015, 22, 55–64. [Google Scholar] [CrossRef]
- Donahue, S.P.; Johnson, T.M.; Leonard-Martin, T.C. Screening for amblyogenic factors using a volunteer lay network and the MTI PhotoScreener: Initial results from 15,000 preschool children in a statewide effort. Ophthalmology 2000, 107, 1637–1644. [Google Scholar] [CrossRef]
- Cotter, S.A.; Tarczy-Hornoch, K.; Wang, Y.; Azen, S.P.; Dilauro, A.; Borchert, M.; Varma, R.; Multi-Ethnic Pediatric Eye Disease Study Group. Visual acuity testability in African-American and Hispanic Children: The Multi-Ethnic Pediatric Eye Disease Study. Am. J. Ophthalmol. 2007, 144, 663–667. [Google Scholar] [CrossRef][Green Version]
- Leone, J.F.; Gole, G.A.; Mitchell, P.; Kifley, A.; Pai, A.S.I.; Rose, K.A. Visual acuity testability and comparability in Australian preschool children: The Sydney Paediatric Eye Disease Study. Eye 2012, 26, 925–932. [Google Scholar] [CrossRef]
- Schmidt, P.; Maguire, M.; Dobson, V.; Quinn, G.; Ciner, E.; Cyert, L.; Kulp, M.T.; Moore, B.; Orel-Bixler, D.; Redford, M.; et al. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision in Preschoolers Study. Ophthalmology 2004, 111, 637–650. [Google Scholar]
- Bušić, M.; Bjeloš, M.; Petrovečki, M.; Kuzmanović Elabjer, B.; Bosnar, D.; Ramić, S.; Andrijašević, L.; Kondža Krstonijević, E.; Jakovljević, V.; Bišćan Tvrdi, A.; et al. Zagreb Amblyopia Preschool Screening Study: Near and distance visual acuity testing increase the diagnostic accuracy of screening for amblyopia. Croat. Med. J. 2016, 57, 29–41. [Google Scholar] [CrossRef]
- Ministarstvo zdravstva Republike Hrvatske. Nacionalni Preventivni Program Ranog Otkrivanja Slabovidnosti 2018–2028. Available online: https://zdravlje.gov.hr/UserDocsImages/2018%20Natječaji/Nacionalni%20preventivni%20program%20ranog%20otkrivanja%20slabovidnosti%202018.-2028.%20scan.pdf (accessed on 28 April 2024).
- Pravilnik o Minimalnim Uvjetima u Pogledu Prostora, Radnika i Medicinsko-Tehničke Opreme za Obavljanje Zdravstvene djelatnosti. Available online: https://www.hlk.hr/EasyEdit/UserFiles/Pravilnici/pravilnik-o-min-uvjetima-prostora-radnika-i-med-tehn-opreme-za-obavljanje-zdr-djelatnosti.pdf (accessed on 27 May 2024).
- Yuodelis, C.; Hendrickson, A. A qualitative and quantitative analysis of the human fovea during development. Vision. Res. 1986, 26, 847–855. [Google Scholar] [CrossRef]
- Cotter, S.A.; Cyert, L.A.; Miller, J.M.; Quinn, G.E. National Expert Panel to the National Center for Children’s Vision and Eye Health. Vision Screening for Children 36 to <72 Months: Recommended Practices. Optom. Vis. Sci. 2015, 92, 6–16. [Google Scholar]
- Levi, D.M.; Song, S.; Pelli, D.G. Amblyopic reading is crowded. J. Vis. 2007, 7, 21. [Google Scholar] [CrossRef]
- Morad, Y.; Werker, E.; Nemet, P. Visual acuity tests using chart, line, and single optotype in healthy and amblyopic children. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 1999, 3, 94–97. [Google Scholar] [CrossRef]
- Song, S.; Levi, D.M.; Pelli, D.G. A double dissociation of the acuity and crowding limits to letter identification, and the promise of improved visual screening. J. Vis. 2014, 14, 3. [Google Scholar] [CrossRef]
- Kvarnström, G.; Jakobsson, P. Is Vision Screening in 3-year-old Children Feasible? Comparison between the Lea Symbol Chart and the HVOT (LM) Chart. Acta. Ophthalmol. Scand. 2005, 83, 76–80. [Google Scholar] [CrossRef]
- Pan, Y.; Tarczy-Hornoch, K.; Cotter, S.A.; Wen, G.; Borchert, M.S.; Azen, S.P.; Varma, R.; Multi-Ethnic Pediatric Eye Disease Study Group. Visual Acuity norms in preschool children: The multiethnic pediatric eye disease study. Optom. Vis. Sci. 2009, 86, 607–612. [Google Scholar] [CrossRef]
- Friedman, D.S.; Repka, M.X.; Katz, J.; Giordano, L.; Ibironke, J.; Hawes, P.; Burkom, D.; Tielsch, J.M. Prevalence of decreased visual acuity among preschool-aged children in an American urban population: The Baltimore Pediatric Eye Disease Study: Methods and results. Ophthalmology 2008, 115, 1786–1789. [Google Scholar] [CrossRef]
- Cruz, O.A.; Repka, M.X.; Hercinovic, A.; Cotter, S.A.; Lambert, S.R.; Hutchinson, A.K.; Sprunger, D.T.; Morse, C.L.; Wallace, D.K. American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. Amblyopia Preferred Practice Pattern. Ophthalmology 2023, 130, P136–P178. [Google Scholar] [CrossRef]
- Bjeloš, M.; Sonicki, Z.; Bušić, M.; Ćurić, A.; Kuzmanović Elabjer, B. Re: Xiao et al.: Randomized controlled trial of a dichoptic digital therapeutic for amblyopia (Ophthalmology. 2022;129:77-85). Ophthalmology 2022, 129, e151–e152. [Google Scholar] [CrossRef]
- Xiao, S.; Angjeli, E.; Wu, H.C.; Gaier, E.D.; Gomez, S.; Travers, D.A.; Binenbaum, G.; Langer, R.; Hunter, D.G.; Repka, M.X.; et al. Controlled Trial of a Dichoptic Digital Therapeutic for Amblyopia. Ophthalmology 2022, 129, 7–85. [Google Scholar] [CrossRef]
- Guo, X.; Fu, M.; Lü, J.; Chen, Q.; Zeng, Y.; Ding, X.; Morgan, I.G.; He, M. Normative distribution of visual acuity in 3- to 6-year-old Chinese preschoolers: The Shenzhen kindergarten eye study. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1985–1992. [Google Scholar] [CrossRef]
- Drover, J.R.; Felius, J.; Cheng, C.S.; Morale, S.E.; Wyatt, L.; Birch, E.E. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2008, 12, 145–149. [Google Scholar] [CrossRef]
- Pascual, M.; Huang, J.; Maguire, M.G.; Kulp, M.T.; Quinn, G.E.; Ciner, E.; Cyert, L.A.; Orel-Bixler, D.; Moore, B.; Ying, G.S.; et al. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology 2014, 121, 622–629.e1. [Google Scholar] [CrossRef]
- Meier, K.; Giaschi, D. Unilateral Amblyopia Affects Two Eyes: Fellow Eye Deficits in Amblyopia. Investig. Ophthalmol. Vis. Sci. 2017, 58, 1779–1800. [Google Scholar] [CrossRef]
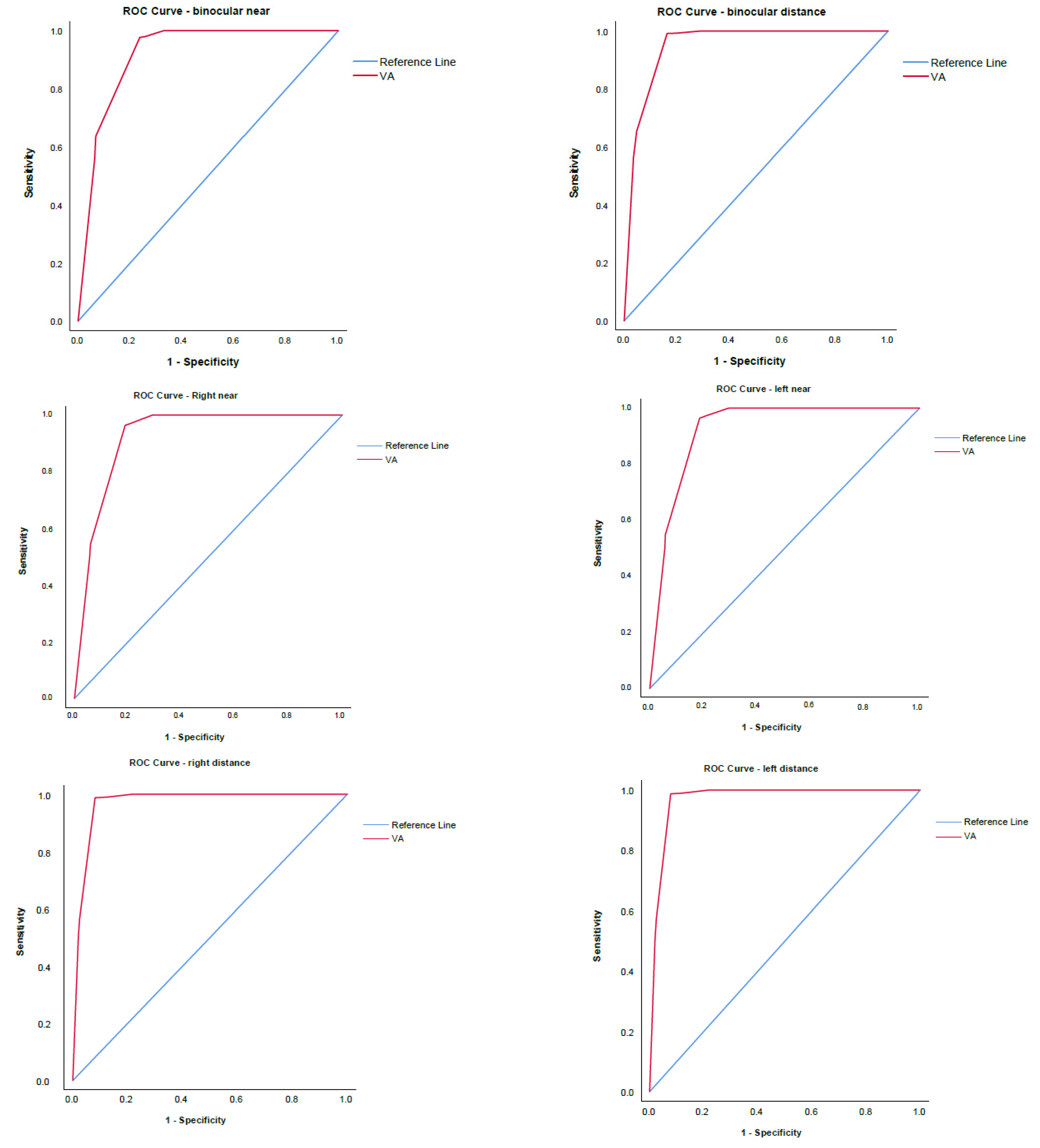
| Binocular Distance | Binocular Near | Right Eye Distance | Right Eye Near | Left Eye Distance | Left Eye Near | |
|---|---|---|---|---|---|---|
| Mean VA ± SD | 0.83 ± 0.24 | 0.83 ± 0.24 | 0.82 ± 0.23 | 0.82 ± 0.23 | 0.82 ± 0.24 | 0.82 ± 0.24 |
| AUC | 0.95 | 0.92 | 0.97 | 0.92 | 0.97 | 0.92 |
| Binocular Distance | Binocular Near | Right Eye Distance | Right Eye Near | Left Eye Distance | Left Eye Near | |
|---|---|---|---|---|---|---|
| Area | 0.95 | 0.919 | 0.925 | 0.923 | 0.971 | 0.97 |
| Std error | 0.001 | 0.002 | 0.002 | 0.002 | 0.001 | 0.001 |
| Asymptotic sig | 0 | 0 | 0 | 0 | 0 | 0 |
| 95% CI low | 0.947 | 0.915 | 0.922 | 0.92 | 0.969 | 0.968 |
| 95% CI upp | 0.953 | 0.923 | 0.929 | 0.927 | 0.973 | 0.972 |
| Youden index | 0.831 | 0.744 | 0.784 | 0.78 | 0.91 | 0.91 |
| N | Females | Males | p Value | |
|---|---|---|---|---|
| Non–testable | 2322 (3.05%) | 1056 (45.48%) | 1266 (54.52%) | p < 0.001 |
| Partially–testable | 1159 (1.52%) | 508 (43.83%) | 651 (56.17%) | p < 0.001 |
| BE Near (n = 514) | BE Distance (n = 1010) | RE Near (n = 184) | LE Near (n = 143) | RE Distance (n = 606) | LE Distance (n = 528) | |
|---|---|---|---|---|---|---|
| Visual acuity | 0.66 ± 0.3 | 0.73 ± 0.26 | 0.61 ± 0.28 | 0.55 ± 0.29 | 0.68 ± 0.24 | 0.68 ± 0.24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bjeloš, M.; Bušić, M.; Rak, B.; Ćurić, A.; Kuzmanović Elabjer, B. Unveiling Visual Acuity in 58,712 Four-Year-Olds: Standardized Assessment Defined Normative Visual Acuity Threshold. Vision 2024, 8, 39. https://doi.org/10.3390/vision8020039
Bjeloš M, Bušić M, Rak B, Ćurić A, Kuzmanović Elabjer B. Unveiling Visual Acuity in 58,712 Four-Year-Olds: Standardized Assessment Defined Normative Visual Acuity Threshold. Vision. 2024; 8(2):39. https://doi.org/10.3390/vision8020039
Chicago/Turabian StyleBjeloš, Mirjana, Mladen Bušić, Benedict Rak, Ana Ćurić, and Biljana Kuzmanović Elabjer. 2024. "Unveiling Visual Acuity in 58,712 Four-Year-Olds: Standardized Assessment Defined Normative Visual Acuity Threshold" Vision 8, no. 2: 39. https://doi.org/10.3390/vision8020039
APA StyleBjeloš, M., Bušić, M., Rak, B., Ćurić, A., & Kuzmanović Elabjer, B. (2024). Unveiling Visual Acuity in 58,712 Four-Year-Olds: Standardized Assessment Defined Normative Visual Acuity Threshold. Vision, 8(2), 39. https://doi.org/10.3390/vision8020039





