Daytime Changes in Tear Film Parameters and Visual Acuity with New-Generation Daily Disposable Silicone Hydrogel Contact Lenses—A Double-Masked Study in Symptomatic Subjects
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Subjects
2.2. Contact Lenses
2.3. Clinical Examination Routine
2.4. Comfort Assessment
2.5. Visual Acuity
2.6. Noninvasive Tear Break-Up Time (NIBUT)
2.7. Dynamic Topography
2.8. Statistical Analysis
3. Results
3.1. Sample Characteristics—Baseline Results
3.2. Visual Acuity
3.3. Pre-Lens NIBUT
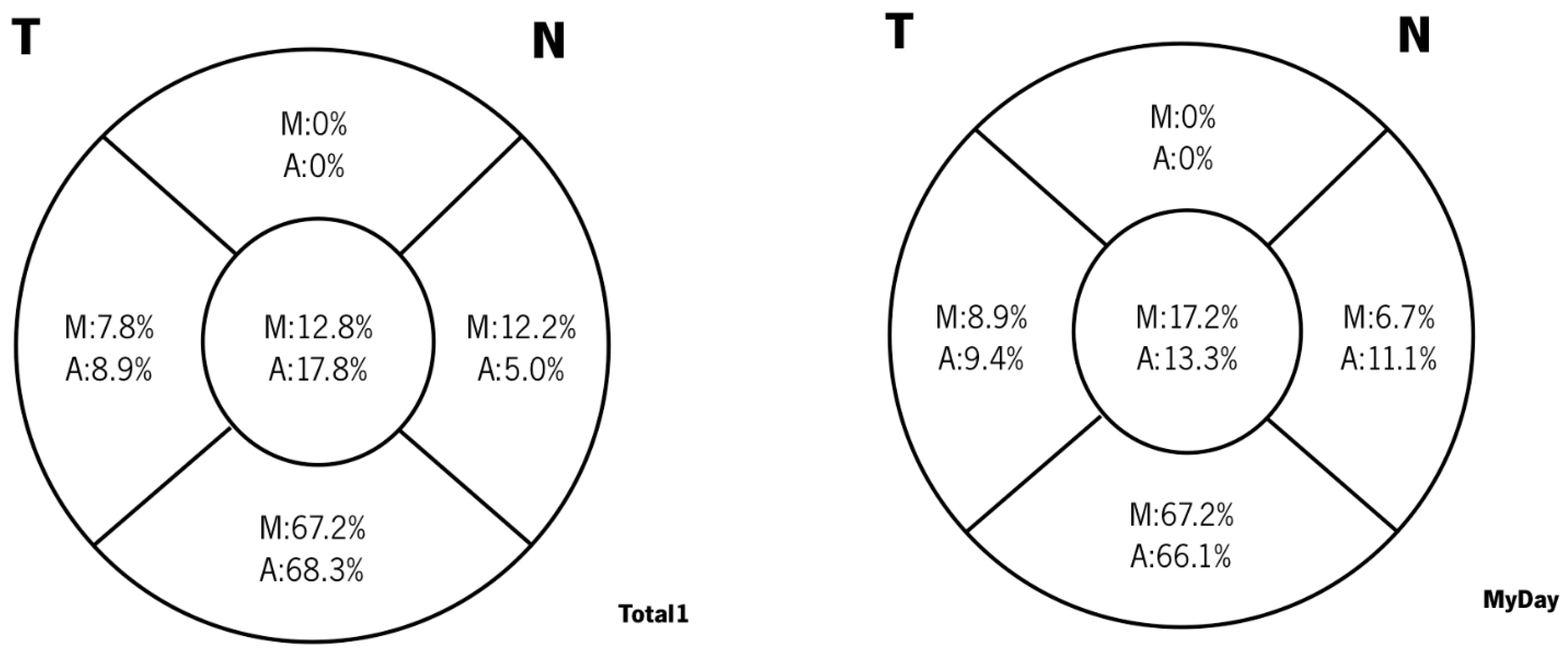
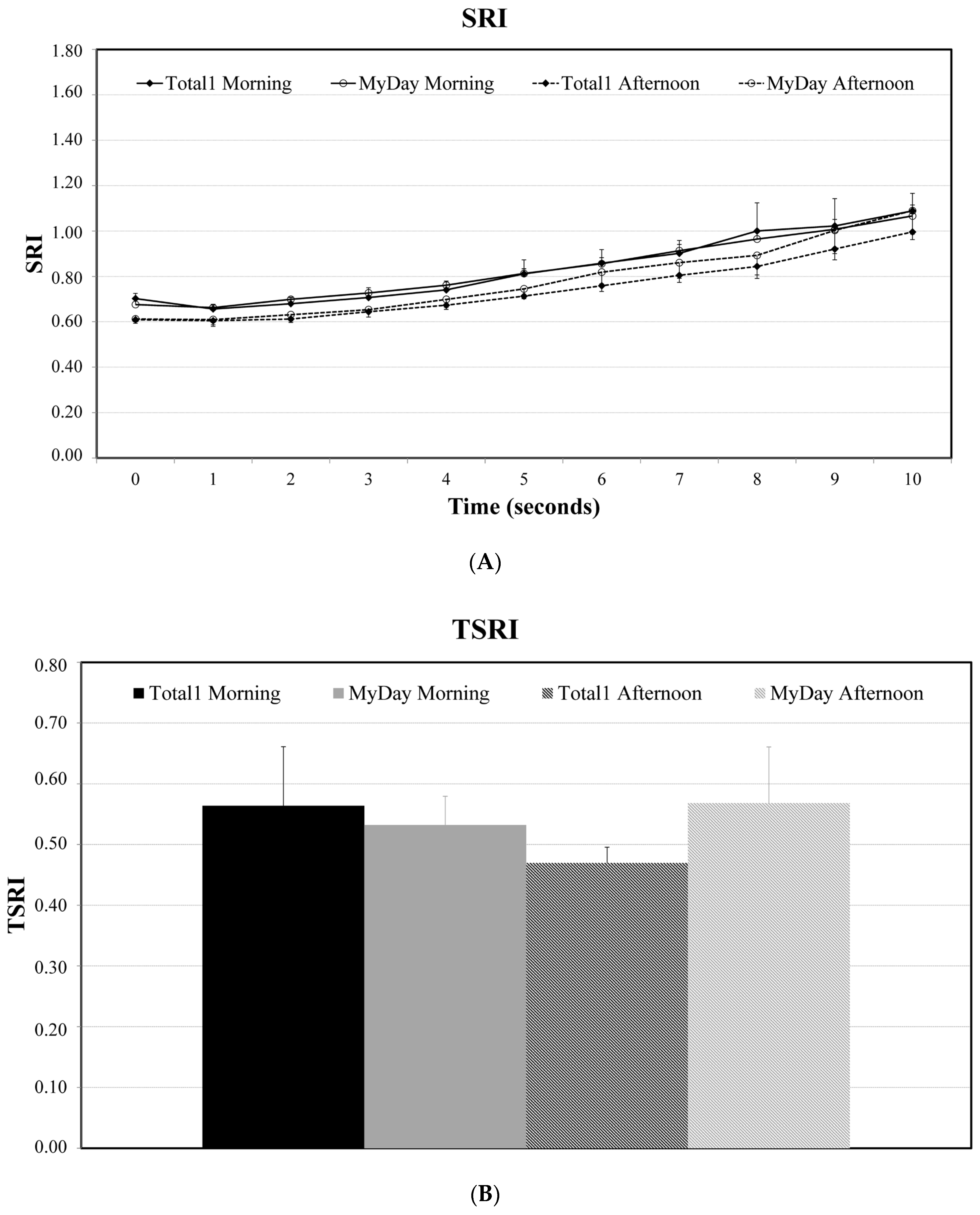
3.4. Dynamic Topography
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koh, S.; Tung, C.I.; Inoue, Y.; Jhanji, V. Effects of tear film dynamics on quality of vision. Br. J. Ophthalmol. 2018, 102, 1615–1620. [Google Scholar] [CrossRef] [PubMed]
- Montés-Micó, R.; Alió, J.L.; MuñOz, G.; Charman, W.N. Temporal Changes in Optical Quality of Air–Tear Film Interface at Anterior Cornea after Blink. Investig. Opthalmol. Vis. Sci. 2004, 45, 1752–1757. [Google Scholar] [CrossRef] [PubMed]
- Albarrán, C.; Pons, A.; Lorente, A.; Montés, R.; Artigas, J. Influence of the tear film on optical quality of the eye. Contact Lens Anterior Eye 1997, 20, 129–135. [Google Scholar] [CrossRef]
- Tutt, R.; Bradley, A.; Begley, C.; Thibos, L.N. Optical and visual impact of tear break-up in human eyes. Investig. Ophthalmol. Vis. Sci. 2000, 41, 4117–4123. [Google Scholar]
- Montés-Micó, R.; Cervino, A.; Ferrer-Blasco, T.; García-Lázaro, S.; Madrid-Costa, D. The Tear Film and the optical Quality of the Eye. Ocul. Surf. 2010, 8, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Montés-Micó, R. Role of the tear film in the optical quality of the human eye. J. Cataract Refract. Surg. 2007, 33, 1631–1635. [Google Scholar] [CrossRef] [PubMed]
- Nagahara, Y.; Koh, S.; Maeda, N.; Nishida, K.; Watanabe, H. Prominent Decrease of Tear Meniscus Height With Contact Lens Wear and Efficacy of Eye Drop Instillation. Eye Contact Lens Sci. Clin. Pract. 2015, 41, 318–322. [Google Scholar] [CrossRef]
- Yokoi, N.; Eftimov, P.; Georgiev, G.A. Dynamic Aspects of Pre-Soft Contact Lens Tear Film and Their Relation to Dry Eye: Basic Science and Clinical Relevance. Life 2023, 13, 859. [Google Scholar] [CrossRef]
- Nichols, K.K.; Redfern, R.L.; Jacob, J.T.; Nelson, J.D.; Fonn, D.; Forstot, S.L.; Huang, J.-F.; Holden, B.A.; Nichols, J.J. The TFOS International Workshop on Contact Lens Discomfort: Report of the Definition and Classification Subcommittee. Investig. Opthalmology Vis. Sci. 2013, 54, TFOS14. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H.; et al. TFOS DEWS II Diagnostic Methodology report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef]
- Kojima, T. Contact Lens-Associated Dry Eye Disease: Recent Advances Worldwide and in Japan. Investig. Opthalmology Vis. Sci. 2018, 59, DES102. [Google Scholar] [CrossRef] [PubMed]
- McMonnies, C.W. Why are soft contact lens wear discontinuation rates still too high? Expert Rev. Ophthalmol. 2023, 18, 11–18. [Google Scholar] [CrossRef]
- Pucker, A.D.; Tichenor, A.A. A Review of Contact Lens Dropout. Clin. Optom. 2020, 12, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Foulks, G.; Chalmers, R.; Keir, N.; Woods, C.A.; Simpson, T.; Lippman, R.; Gleason, W.; Schaumberg, D.A.; Willcox, M.D.P.; Jalbert, I. The TFOS International Workshop on Contact Lens Discomfort: Report of the Subcommittee on Clinical Trial Design and Outcomes. Investig. Opthalmol. Vis. Sci. 2013, 54, TFOS157. [Google Scholar] [CrossRef] [PubMed]
- García-Marqués, J.V.; Macedo-De-Araújo, R.J.; McAlinden, C.; Faria-Ribeiro, M.; Cerviño, A.; González-Méijome, J.M. Short-term tear film stability, optical quality and visual performance in two dual-focus contact lenses for myopia control with different optical designs. Ophthalmic Physiol. Opt. 2022, 42, 1062–1073. [Google Scholar] [CrossRef] [PubMed]
- García-Marqués, J.V.; Macedo-De-Araújo, R.; Lopes-Ferreira, D.; Cerviño, A.; García-Lázaro, S.; González-Méijome, J.M. Tear film stability over a myopia control contact lens compared to a monofocal design. Clin. Exp. Optom. 2022, 105, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Lafosse, E.; Martínez-Albert, N.; Wolffsohn, J.S.W.; Cerviño, A.; García-Lázaro, S. Response of the Aging Eye to First Day of Modern Material Contact Lens Wear. Eye Contact Lens Sci. Clin. Pract. 2019, 45, 40–45. [Google Scholar] [CrossRef]
- Szczesna-Iskander, D.H. Comparison of Tear Film Surface Quality Measured In Vivo on Water Gradient Silicone Hydrogel and Hydrogel Contact Lenses. Eye Contact Lens Sci. Clin. Pract. 2014, 40, 23–27. [Google Scholar] [CrossRef]
- García-Montero, M.; Rico-Del-Viejo, L.; Martínez-Alberquilla, I.; Hernández-Verdejo, J.L.; Lorente-Velázquez, A.; Madrid-Costa, D. Effects of Blink Rate on Tear Film Optical Quality Dynamics with Different Soft Contact Lenses. J. Ophthalmol. 2019, 2019, 4921538. [Google Scholar] [CrossRef]
- García-Montero, M.; Rico-Del-Viejo, L.; Llorens-Quintana, C.; Lorente-Velázquez, A.; Hernández-Verdejo, J.L.; Madrid-Costa, D. Randomized crossover trial of silicone hydrogel contact lenses. Contact Lens Anterior Eye 2019, 42, 475–481. [Google Scholar] [CrossRef]
- Patel, S.; Bevan, R.; Farrell, J.C. Diurnal Variation in Precorneal Tear Film Stability. Optom. Vis. Sci. 1988, 65, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Lira, M.; Oliveira, M.E.C.R.; Franco, S. Comparison of the tear film clinical parameters at two different times of the day. Clin. Exp. Optom. 2011, 94, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Bitton, E.; Keech, A.; Jones, L.; Simpson, T. Subjective and Objective Variation of the Tear Film Pre- and Post-Sleep. Optom. Vis. Sci. 2008, 85, 740–749. [Google Scholar] [CrossRef] [PubMed]
- Pena-Verdeal, H.; García-Resúa, C.; Ramos, L.; Yebra-Pimentel, E.; Giráldez, M.J. Diurnal variations in tear film break-up time determined in healthy subjects by software-assisted interpretation of tear film video recordings. Clin. Exp. Optom. 2016, 99, 142–148. [Google Scholar] [CrossRef] [PubMed]
- DU Toit, R.; Situ, P.; Simpson, T.; Fonn, D. The Effects of Six Months of Contact Lens Wear on the Tear Film, Ocular Surfaces, and Symptoms of Presbyopes. Optom. Vis. Sci. 2001, 78, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Cho, P.B.O.; Yap, M.O. Age, Gender, and Tear Break-Up Time. Optom. Vis. Sci. 1993, 70, 828–831. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Boyd, K.E.; Burns, J. Age, stability of the precorneal tear film and the refractive index of tears. Contact Lens Anterior Eye 2000, 23, 44–47. [Google Scholar] [CrossRef]
- Maïssa, C.; Guillon, M. Tear film dynamics and lipid layer characteristics—Effect of age and gender. Contact Lens Anterior Eye 2010, 33, 176–182. [Google Scholar] [CrossRef]
- Sweeney, D.F.; Millar, T.J.; Raju, S.R. Tear film stability: A review. Exp. Eye Res. 2013, 117, 28–38. [Google Scholar] [CrossRef]
- Özcura, F.; Aydin, S.; Helvaci, M.R. Ocular Surface Disease Index for the Diagnosis of Dry Eye Syndrome. Ocul. Immunol. Inflamm. 2007, 15, 389–393. [Google Scholar] [CrossRef]
- Pastor-Zaplana, J.; Borrás, F.; Gallar, J.; Acosta, M.C. OSDI Questions on Daily Life Activities Allow to Detect Subclinical Dry Eye in Young Contact Lens Users. J. Clin. Med. 2022, 11, 2626. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and Validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 2000, 118, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Németh, J.; Erdélyi, B.; Csákány, B.; Gaspar, P.; Soumelidis, A.; Kahlesz, F.; Lang, Z. High-speed videotopographic measurement of tear film build-up time. Investig. Ophthalmol. Vis. Sci. 2002, 43, 1783–1790. [Google Scholar]
- Wilson, S.E.; Klyce, S.D. Advances in the analysis of corneal topography. Surv. Ophthalmol. 1991, 35, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Burns, D.M.; Johnston, F.M.; Frazer, D.G.; Patterson, C.; Jackson, A.J. Keratoconus: An analysis of corneal asymmetry. Br. J. Ophthalmol. 2004, 88, 1252–1255. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.E.; Lin, D.T.; Klyce, S.D. Corneal topography of keratoconus. Cornea 1991, 10, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T.; Ishida, R.; Dogru, M.; Goto, E.; Takano, Y.; Matsumoto, Y.; Kaido, M.; Ohashi, Y.; Tsubota, K. A New Noninvasive Tear Stability Analysis System for the Assessment of Dry Eyes. Investig. Opthalmology Vis. Sci. 2004, 45, 1369–1374. [Google Scholar] [CrossRef]
- Belda-Salmerón, L.; Ferrer-Blasco, T.; Albarrán-Diego, C.; Madrid-Costa, D.; Montés-Micó, R. Diurnal Variations in Visual Performance for Disposable Contact Lenses. Optom. Vis. Sci. 2013, 90, 682–690. [Google Scholar] [CrossRef]
- Pettersson, A.L.; Mårtensson, L.; Salkic, J.; Unsbo, P.; Brautaset, R. Spherical aberration in relation to visual performance in contact lens wear. Contact Lens Anterior Eye 2011, 34, 12–16. [Google Scholar] [CrossRef]
- Mengher, L.S.; Bron, A.J.; Tonge, S.R.; Gilbert, D.J. A non-invasive instrument for clinical assessment of the pre-corneal tear film stability. Curr. Eye Res. 1985, 4, 1–7. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Mroczkowska, S.; Hunt, O.A.; Bilkhu, P.; Drew, T.; Sheppard, A. Crossover Evaluation of Silicone Hydrogel Daily Disposable Contact Lenses. Optom. Vis. Sci. 2015, 92, 1063–1068. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, G.S.; Sujakhu, D.; Shrestha, J.B.; Shrestha, J.K. Tear Film Evaluation in Contact Lens Wearers and Non-Wearers. J. Inst. Med. 2012, 34, 14–20. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Hunt, O.A.; Chowdhury, A. Objective clinical performance of ‘comfort-enhanced’ daily disposable soft contact lenses. Contact Lens Anterior Eye 2010, 33, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Glasson, M.J.; Stapleton, F.; Keay, L.; Willcox, M. The effect of short term contact lens wear on the tear film and ocular surface characteristics of tolerant and intolerant wearers. Contact Lens Anterior Eye 2006, 29, 41–47. [Google Scholar] [CrossRef] [PubMed]
- de Paiva, C.S.; Lindsey, J.L.; Pflugfelder, S.C. Assessing the severity of keratitis sicca with videokeratoscopic indices. Ophthalmology 2003, 110, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Kopf, M.; Yi, F.; Iskander, D.R.; Collins, M.J.; Shaw, A.J.; Straker, B. Tear Film Surface Quality with Soft Contact Lenses Using Dynamic Videokeratoscopy. J. Optom. 2008, 1, 14–21. [Google Scholar] [CrossRef]
- Iskander, D.R.; Collins, M.J. Applications of high-speed videokeratoscopy. Clin. Exp. Optom. 2005, 88, 223–231. [Google Scholar] [CrossRef][Green Version]
- Németh, J.; Erdélyi, B.; Csákány, B. Corneal topography changes after a 15 s pause in blinking. J. Cataract Refract. Surg. 2001, 27, 589–592. [Google Scholar] [CrossRef]

| Lens | Material | Diameter (mm) | Base Curve (mm) | Centre Thickness (mm) | Water Content (%) | DK/t | Modulus (MPa) |
|---|---|---|---|---|---|---|---|
| Total1 | Delefilcon A | 14.1 | 8.5 | 0.09 | >80% at surface 33% at core | 156 | 0.7 |
| MyDay | Stenfilcon A | 14.2 | 8.4 | 0.08 | 54% | 100 | 0.4 |
| Parameter | Description |
|---|---|
| N | 20 |
| Gender | 13 F (65%) |
| 7 M (35%) | |
| Age (years) | 26.75 ± 6.28 |
| 26.92 ± 6.4 F | |
| 26.42 ± 6.6 Ma | |
| Habitual refraction (D) Mean ± SD | Pre-Delefilcon A Eye |
| −1.97 ± 1.14 DS | |
| −0.11 ± 0.27 DC | |
| Pre-Stenfilcon A Eye | |
| −1.88 ± 1.15 DS | |
| −0.16 ± 0.33 DC | |
| Keratometry Mean ± SD | Pre-Delefilcon A Eye: 7.71 ± 0.26 (D) |
| Pre-Stenfilcon A Eye: 7.79 ± 0.26 (D) | |
| Habitual correction | Glasses and sporadic CL wear: 5 |
| Sporadic CL wear only: 2 | |
| Daily disposable CL wear: 5 | |
| Monthly CL (daily wear): 8 | |
| NIBUT (seconds) Mean ± SD | Pre-Delefilcon A Eye: 7.73 ± 2.2 s |
| Pre-Stenfilcon A Eye: 8.3 ± 2.9 s | |
| OSDI Mean ± SD | 32.95 ± 9.82 (range: 16.67 to 56.25) |
| 33.36 ± 9.7 F | |
| 32.70 ± 10.9 Ma |
| HCVA | LCVA | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Mean p (a) | Day 1 | Day 2 | Day 3 | Mean p (a) | ||
| Delefilcon A | Morning | −0.05 ± 0.07 | −0.05 ± 0.10 | −0.07 ± 0.11 | −0.06 ± 0.08 0.821 * | 0.17 ± 0.10 | 0.16 ± 0.11 | 0.13 ± 0.12 | 0.16 ± 0.10 0.081 + |
| Afternoon | −0.03 ± 0.10 | −0.05 ± 0.10 | −0.08 ± 0.10 | −0.05 ± 0.09 0.021 + | 0.17 ± 0.12 | 0.14 ± 0.10 | 0.13 ± 0.12 | 0.15 ± 0.10 0.043 + | |
| Difference p (b) | −0.02 ± 0.06, 0.144 º | 0.00 ± 0.07, 0.984 × | 0.01 ± 0.06, 0.425 º | 0.00 ± 0.07 0.950 º | 0.02 ± 0.06, 0.079 º | 0.00 ± 0.06, 0.801 º | |||
| Stenfilcon A | Morning | −0.04 ± 0.09 | −0.04 ± 0.11 | −0.06 ± 0.11 | −0.04 ± 0.09 0.771 * | 0.17 ± 0.09 | 0.15 ± 0.12 | 0.12 ± 0.09 | 0.15 ± 0.08 0.196 * |
| Afternoon | −0.05 ± 0.10 | −0.05 ± 0.10 | −0.06 ± 0.09 | −0.05 ± 0.09 0.877 * | 0.14 ± 0.11 | 0.12 ± 0.08 | 0.12 ± 0.11 | 0.13 ± 0.09 0.766 * | |
| Difference p (b) | 0.01 ± 0.06 0.468 º | 0.01 ± 0.08 0.484 º | 0.00 ± 0.08 0.769 º | 0.04 ± 0.06 0.024 º | 0.04 ± 0.12 0.304 × | 0.00 ± 0.05 0.729 º | |||
| BINOCULAR | Morning | −0.15 ± 0.17 | −0.12 ± 0.07 | −0.14 ± 0.08 | −0.14 ± 0.09 0.513 + | 0.09 ± 0.06 | 0.06 ± 0.07 | 0.04 ± 0.05 | 0.06 ± 0.05 0.068 * |
| Afternoon | −0.12 ± 0.08 | −0.13 ± 0.06 | −0.12 ± 0.08 | −0.13 ± 0.07 0.921 * | 0.06 ± 0.06 | 0.05 ± 0.05 | 0.05 ± 0.06 | 0.05 ± 0.05 0.461 + | |
| Difference p (b) | −0.02 ± 0.16, 0.636 × | 0.01 ± 0.04, 0.280 º | −0.01 ± 0.07, 0.452 × | 0.03 ± 0.05, 0.029 º | 0.01 ± 0.05, 0.267 º | −0.01 ± 0.04, 0.391 º | |||
| Day 1 | Day 2 | Day 3 | Mean (s) p (a) | ||
|---|---|---|---|---|---|
| Delefilcon A | Morning | 5.94 ± 1.58 | 5.27 ± 1.33 | 5.57 ± 1.31 | 5.59 ± 1.05 0.387 + |
| Afternoon | 5.21 ± 0.82 | 4.80 ± 0.86 | 4.83 ± 1.17 | 4.95 ± 0.63 0.326 * | |
| Difference p (b) | 0.73 ± 1.63 0.102 × | 0.47 ± 1.22 0.101 º | 0.74 ± 1.58 0.048 × | ||
| Stenfilcon A | Morning | 5.97 ± 1.58 | 5.45 ± 1.15 | 5.66 ± 1.43 | 5.69 ± 1.21 0.165 + |
| Afternoon | 5.07 ± 0.79 | 4.87 ± 1.32 | 4.93 ± 1.95 | 4.96 ± 0.93 0.200 + | |
| Difference p (b) | 0.89 ± 1.29 0.006 º | 0.58 ± 0.99 0.017 º | 0.74 ± 1.90 0.007 × |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Macedo-de-Araújo, R.J.; Rico-del-Viejo, L.; Martin-Montañez, V.; Queirós, A.; González-Méijome, J.M. Daytime Changes in Tear Film Parameters and Visual Acuity with New-Generation Daily Disposable Silicone Hydrogel Contact Lenses—A Double-Masked Study in Symptomatic Subjects. Vision 2024, 8, 11. https://doi.org/10.3390/vision8010011
Macedo-de-Araújo RJ, Rico-del-Viejo L, Martin-Montañez V, Queirós A, González-Méijome JM. Daytime Changes in Tear Film Parameters and Visual Acuity with New-Generation Daily Disposable Silicone Hydrogel Contact Lenses—A Double-Masked Study in Symptomatic Subjects. Vision. 2024; 8(1):11. https://doi.org/10.3390/vision8010011
Chicago/Turabian StyleMacedo-de-Araújo, Rute J., Laura Rico-del-Viejo, Vicente Martin-Montañez, António Queirós, and José M. González-Méijome. 2024. "Daytime Changes in Tear Film Parameters and Visual Acuity with New-Generation Daily Disposable Silicone Hydrogel Contact Lenses—A Double-Masked Study in Symptomatic Subjects" Vision 8, no. 1: 11. https://doi.org/10.3390/vision8010011
APA StyleMacedo-de-Araújo, R. J., Rico-del-Viejo, L., Martin-Montañez, V., Queirós, A., & González-Méijome, J. M. (2024). Daytime Changes in Tear Film Parameters and Visual Acuity with New-Generation Daily Disposable Silicone Hydrogel Contact Lenses—A Double-Masked Study in Symptomatic Subjects. Vision, 8(1), 11. https://doi.org/10.3390/vision8010011






