The Impact of Rotational Malalignment Following Intramedullary Nailing for Intertrochanteric Fractures on Patients’ Functional Outcomes: A Prospective Study
Abstract
1. Introduction
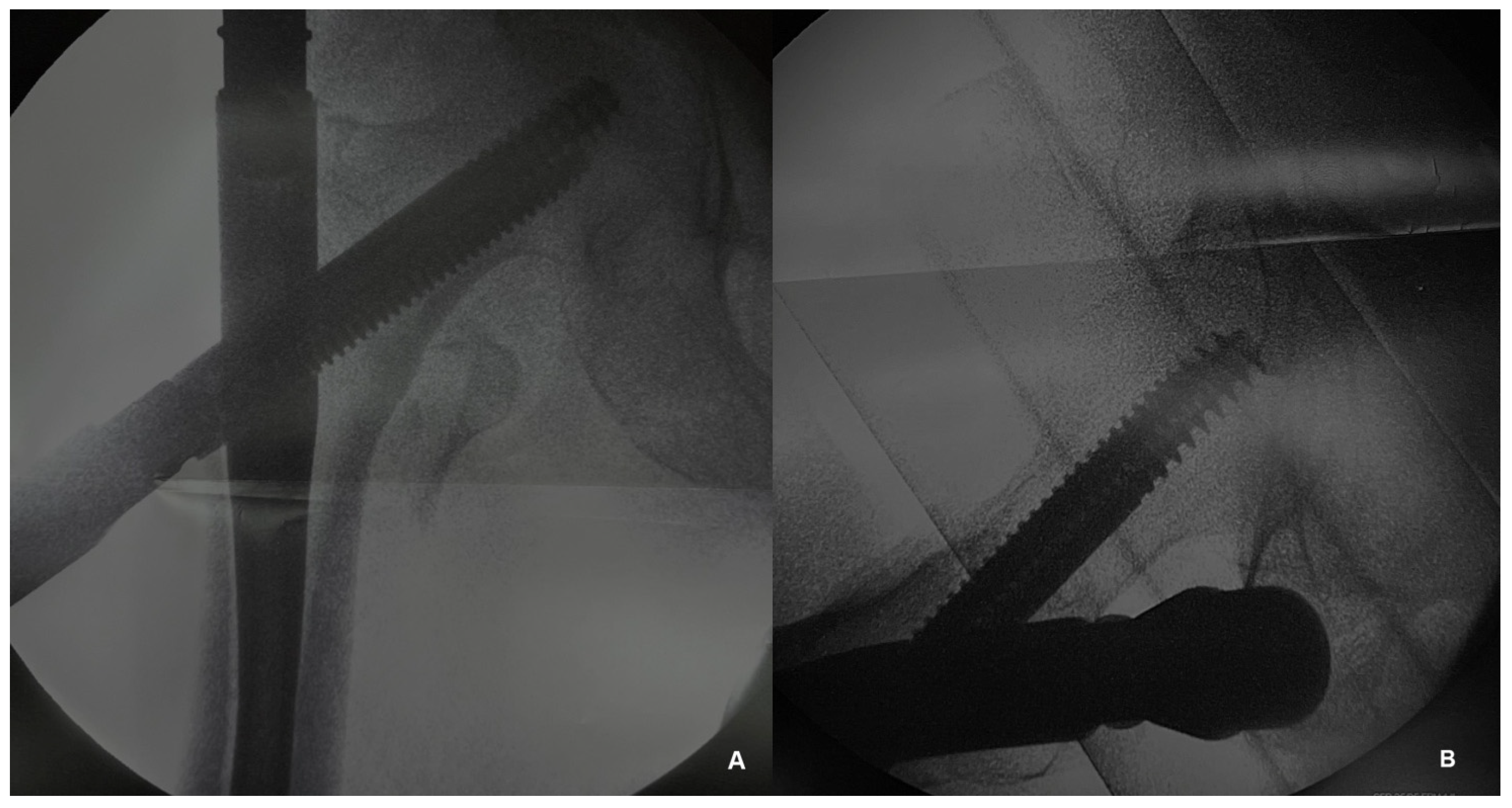
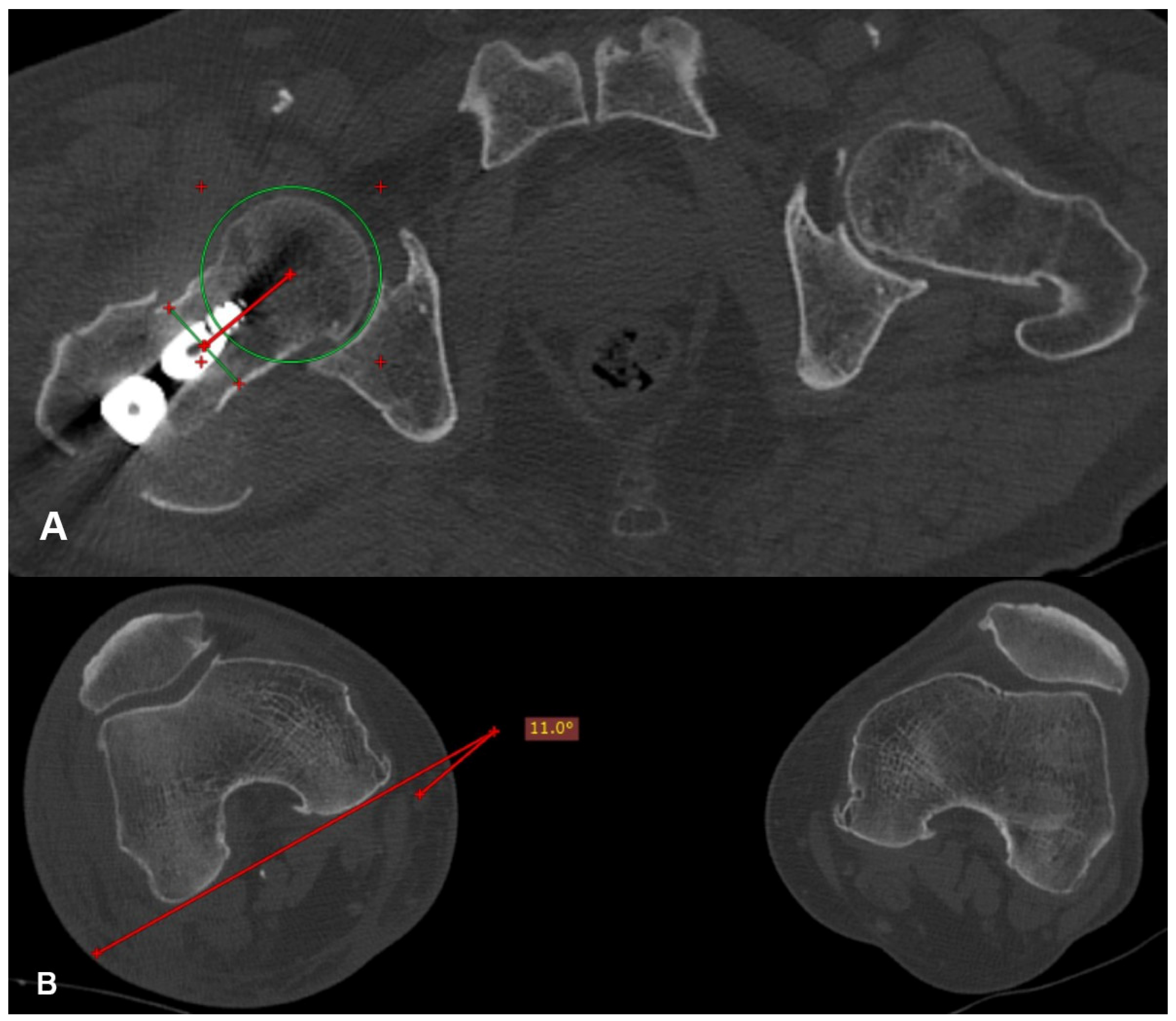
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Williamson, S.; Landeiro, F.; McConnell, T.; Fulford-Smith, L.; Javaid, M.K.; Judge, A.; Leal, J. Costs of fragility hip fractures globally: A systematic review and meta-regression analysis. Osteoporos. Int. 2017, 28, 2791–2800. [Google Scholar] [CrossRef]
- Mattisson, L.; Bojan, A.; Enocson, A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: Data from the Swedish fracture register. BMC Musculoskelet. Disord. 2018, 19, 369. [Google Scholar] [CrossRef]
- Vieira, E.R.; Palmer, R.C.; Chaves, P.H. Prevention of falls in older people living in the community. BMJ 2016, 353, i1419. [Google Scholar] [CrossRef]
- Alpantaki, K.; Papadaki, C.; Raptis, K.; Dretakis, K.; Samonis, G.; Koutserimpas, C. Gender and Age Differences in Hip Fracture Types among Elderly: A Retrospective Cohort Study. Maedica 2020, 15, 185–190. [Google Scholar] [CrossRef]
- Noh, J.; Lee, K.H.; Jung, S.; Hwang, S. The Frequency of Occult Intertrochanteric Fractures among Individuals with Isolated Greater Trochanteric Fractures. Hip Pelvis. 2019, 31, 23–32. [Google Scholar] [CrossRef]
- González-Zabaleta, J.; Pita-Fernandez, S.; Seoane-Pillado, T.; López-Calviño, B.; Gonzalez-Zabaleta, J.L. Dependence for basic and instrumental activities of daily living after hip fractures. Arch. Gerontol. Geriatr. 2015, 60, 66–70. [Google Scholar] [CrossRef]
- Tang, V.L.; Sudore, R.; Cenzer, I.S.; Boscardin, W.J.; Smith, A.; Ritchie, C.; Wallhagen, M.; Finlayson, E.; Petrillo, L.; Covinsky, K. Rates of Recovery to Pre-Fracture Function in Older Persons with Hip Fracture: An Observational Study. J. Gen. Intern. Med. 2017, 32, 153–158. [Google Scholar] [CrossRef]
- Popp, D.; Nia, A.; Biedermann, G.; Schmoelz, L.; Silvaieh, S.; Tiefenboeck, T.M.; Hajdu, S.; Widhalm, H.K. Predictive Validity of Mortality after Surgically Treated Proximal Femur Fractures Based on Four Nutrition Scores-A Retrospective Data Analysis. Nutrients 2023, 15, 3357. [Google Scholar] [CrossRef]
- Outerbridge, R.E. Perosseous venography in the diagnosis of viability in subcapital fractures of the femur. Clin. Orthop. Relat. Res. 1978, 137, 132–139. [Google Scholar] [CrossRef]
- Vavourakis, M.; Zachariou, D.; Galanis, A.; Karampinas, P.; Rozis, M.; Sakellariou, E.; Vlachos, C.; Varsamos, I.; Vlamis, J.; Vasiliadis, E.; et al. Incidence of Rotational Malalignment after Intertrochanteric Fracture Intramedullary Nailing: A CT-Based Prospective Study. Medicina 2024, 60, 1535. [Google Scholar] [CrossRef]
- Jeanmart, L.B.A.; Wackenkeim, A. Computer Tomography of Neck, Chest, Spine, and Limbs. In Atlas of Pathological Computer Tomography; Springer: Berlin/Heidelberg, Germany, 1983; Volume 3. [Google Scholar]
- Citak, M.; Gardner, M.J.; Krettek, C.; Hüfner, T.; Kendoff, D. Navigated femoral anteversion measurements: A new intraoperativetechnique. Injury 2008, 39, 467–471. [Google Scholar] [CrossRef]
- Ettinger, M.; Maslaris, A.; Kenawey, M.; Petri, M.; Krettek, C.; Jagodzinski, M.; Liodakis, E. A preliminary clinical evaluationof the “greater trochanter-headcontact point” method for the intraoperative torsional control of femoral fractures. J. Orthop. Sci. 2012, 17, 717–721. [Google Scholar] [CrossRef]
- Kenawey, M.; Krettek, C.; Ettinger, M.; Hankemeier, S.; Breitmeier, D.; Liodakis, E. The greater trochanter-head contact method: A cadaveric study with a new technique for the intraoperative control of rotation of femoral fractures. J. Orthop. Trauma 2011, 25, 549–555. [Google Scholar] [CrossRef]
- Kendoff, D.; Citak, M.; Gardner, M.J.; Gösling, T.; Krettek, C.; Hüfner, T. Navigated femoral nailing using noninvasive registration of the contralateral intact femur to restore anteversion. Technique and clinical use. J. Orthop. Trauma 2007, 21, 725–730. [Google Scholar] [CrossRef]
- Stübig, T.; Min, W.; Arvani, M.; Hawi, N.; Krettek, C.; Citak, M. Accuracy of measurement of femoral anteversion in femoral shaft fractures using a computer imaging software: A cadaveric study. Arch. Orthop. Trauma Surg. 2012, 132, 613–616. [Google Scholar] [CrossRef]
- Ramanoudjame, M.; Guillon, P.; Dauzac, C.; Meunier, C.; Carcopino, J.M. CT evaluation of torsional malalignment after intertrochanteric fracture fixation. Orthop. Traumatol. Surg. Res. 2010, 96, 844–848. [Google Scholar] [CrossRef]
- Kim, T.Y.; Lee, Y.B.; Chang, J.D.; Lee, S.S.; Yoo, J.H.; Chung, K.J.; Hwang, J.H. Torsional malalignment, how much significant in the trochanteric fractures? Injury 2015, 46, 2196–2200. [Google Scholar] [CrossRef]
- Annappa, R.; Mittal, H.; Kamath, S.; Rai, S.; Suresh, P.; Mohammed, N. Rotational Malalignment after Intramedullary Fixation of Trochanteric Fractures. J. Clin. Diagn. Res. 2018, 12, RC05–RC08. [Google Scholar] [CrossRef]
- Kaiser, P.; Attal, R.; Kammerer, M.; Thauerer, M.; Hamberger, L.; Mayr, R.; Schmoelz, W. Significant differences in femoral torsion values depending on the CT measurement technique. Arch. Orthop. Trauma Surg. 2016, 136, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Shultz, J.S.; Nguyen, A.D. Bilateral asymmetries in clinical measures of lower-extremity anatomic characteristics. Clin. J. Sport Med. 2007, 17, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Vanhove, F.; Noppe, N.; Fragomen, A.T.; Hoekstra, H.; Vanderschueren, G.; Metsemakers, W.J. Standardization of torsional CT measurements of the lower limbs with threshold values for corrective osteotomy. Arch. Orthop. Trauma Surg. 2019, 139, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Jaarsma, R.L.; Pakvis, D.F.; Verdonschot, N.; Biert, J.; van Kampen, A. Rotational malalignment after intramedullary nailing of femoral fractures. J. Orthop. Trauma 2004, 18, 403–409. [Google Scholar] [CrossRef]
- Bråten, M.; Terjesen, T.; Rossvoll, I. Torsional deformity after intramedullary nailing of femoral shaft fractures. Measurement of anteversion angles in 110 patients. J. Bone Jt. Surg. Br. 1993, 75, 799–803. [Google Scholar] [CrossRef]
- Johnson, K.D.; Greenberg, M. Comminuted femoral shaft fractures. Orthop. Clin. N. Am. 1987, 18, 133–147. [Google Scholar] [CrossRef]
- Tornetta, P.; Ritz, G.; Kantor, A. Femoral torsion after interlocked nailing of unstable femoral fractures. J. Trauma 1995, 38, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, D.; Lucas, J.; Klaue, K. Retroversion of the acetabulum. A cause of hip pain. J. Bone Jt. Surg. Br. 1999, 81, 281–288. [Google Scholar] [CrossRef]
- Tönnis, D.; Heinecke, A. Diminished femoral antetorsion syndrome: A cause of pain and osteoarthritis. J. Pediatr. Orthop. 1991, 11, 419–431. [Google Scholar] [CrossRef]

| N | % | ||
|---|---|---|---|
| Gender | Male | 27 | 36.5% |
| Female | 47 | 63.5% | |
| Injury mechanism | Low-energy | 68 | 91.9% |
| High-energy | 6 | 8.1% | |
| Affected hip | Right | 34 | 45.9% |
| Left | 40 | 54.1% |
| Femoral Anteversion | Minimum Value | Mean Value | Standard Deviation | Range | Maximum Value |
|---|---|---|---|---|---|
| Healthy hip | 2.2° | 13.3° | 7.2° | 34.5° | 36.7° |
| Operated hip | 1.2° | 23.2° | 13.3° | 61.2° | 62.4° |
| Difference | 0.9° | 12.3° | 10.3° | 47.6° | 48.5° |
| D Angle | Group | N | % |
|---|---|---|---|
| <15° | A | 51 | 68.9% |
| ≥15° | B | 23 | 31.1% |
| Group | Total | ||||
|---|---|---|---|---|---|
| A | B | ||||
| 6-month mortality | Yes | N | 2 | 5 | 7 |
| % | 4% | 21.7% | 9.5% | ||
| No | N | 49 | 18 | 67 | |
| % | 96% | 78.3% | 90.5% | ||
| Total | N | 51 | 23 | 74 | |
| % | 100% | 100% | 100% | ||
| Value | Degrees of Freedom | Asymptotic Significance (2-Sided) | |
|---|---|---|---|
| Pearson Chi-Square | 6.072 | 2 | 0.048 |
| Group | Total | ||||
|---|---|---|---|---|---|
| A | B | ||||
| 1-year mortality | Yes | N | 4 | 7 | 11 |
| % | 7.8% | 30.4% | 14.9% | ||
| No | N | 47 | 16 | 63 | |
| % | 92.2% | 69.6% | 85.1% | ||
| Total | N | 51 | 23 | 74 | |
| % | 100% | 100% | 100% | ||
| Value | Degrees of Freedom | Asymptotic Significance (2-Sided) | |
|---|---|---|---|
| Pearson Chi-Square | 6.924 | 2 | 0.031 |
| N | Minimum Value | Mean Value | Standard Deviation | Maximum Value | |
|---|---|---|---|---|---|
| Pre-fracture mHHS | 74 | 50.6 | 86.7 | 11.8 | 100 |
| 6-month postoperative mHHS | 67 | 20.9 | 77.9 | 13.3 | 100 |
| 1-year postoperative mHHS | 63 | 20.9 | 83.2 | 14.3 | 100 |
| Group (D Angle) | N of Surviving Patients | Mean Value | Standard Deviation | t | Degrees of Freedom | Significance (2-Tailed) | |
|---|---|---|---|---|---|---|---|
| Difference between pre-fracture and six-month postoperative mHHS | A (<15°) | 49 | −8.7 | 6,1 | −2.536 | 65 | 0.014 |
| B (≥15°) | 18 | −14.5 | 12,4 | −1881 | 20.055 | 0.075 |
| Group (D Angle) | N of Surviving Patients | Mean Value | Standard Deviation | t | Degrees of Freedom | Significance (2-Tailed) | |
|---|---|---|---|---|---|---|---|
| Difference between pre-fracture and one-year postoperative mHHS | A (<15°) | 47 | −4.9 | 7.8 | −1.266 | 61 | 0.210 |
| B (≥15°) | 16 | −8.3 | 13.0 | −0.995 | 18.820 | 0.332 |
| Group | Total | ||||
|---|---|---|---|---|---|
| A | B | ||||
| Fracture union | Yes | N | 48 | 17 | 65 |
| % | 98% | 94.4% | 97% | ||
| No | N | 1 | 1 | 2 | |
| % | 2% | 5.6% | 3% | ||
| Total | N | 49 | 18 | 67 | |
| % | 100% | 100% | 100% | ||
| Value | Degrees of Freedom | Asymptotic Significance (2-Sided) | |
|---|---|---|---|
| Pearson Chi-Square | 0.720 | 2 | 0.698 |
| Study | Evaluation Score | Group (D Angle) | N | Pre-Fracture Functional Level Recovery | Significance (p-Value) |
|---|---|---|---|---|---|
| Kim et al. [18] | Koval | A (<15°) | 81 | 61 (75.3%) | 0.458 |
| B (≥15°) | 28 | 23 (82.1%) | |||
| Present study | Modified Harris Hip | A (<15°) | 47 | 35 (74.5%) | 0.210 |
| B (≥15°) | 16 | 12 (75%) | 0.332 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vavourakis, M.; Galanis, A.; Zachariou, D.; Sakellariou, E.; Patilas, C.; Karampinas, P.; Kaspiris, A.; Rozis, M.; Vlamis, J.; Vasiliadis, E.; et al. The Impact of Rotational Malalignment Following Intramedullary Nailing for Intertrochanteric Fractures on Patients’ Functional Outcomes: A Prospective Study. J. Funct. Morphol. Kinesiol. 2024, 9, 247. https://doi.org/10.3390/jfmk9040247
Vavourakis M, Galanis A, Zachariou D, Sakellariou E, Patilas C, Karampinas P, Kaspiris A, Rozis M, Vlamis J, Vasiliadis E, et al. The Impact of Rotational Malalignment Following Intramedullary Nailing for Intertrochanteric Fractures on Patients’ Functional Outcomes: A Prospective Study. Journal of Functional Morphology and Kinesiology. 2024; 9(4):247. https://doi.org/10.3390/jfmk9040247
Chicago/Turabian StyleVavourakis, Michail, Athanasios Galanis, Dimitrios Zachariou, Evangelos Sakellariou, Christos Patilas, Panagiotis Karampinas, Angelos Kaspiris, Meletis Rozis, John Vlamis, Elias Vasiliadis, and et al. 2024. "The Impact of Rotational Malalignment Following Intramedullary Nailing for Intertrochanteric Fractures on Patients’ Functional Outcomes: A Prospective Study" Journal of Functional Morphology and Kinesiology 9, no. 4: 247. https://doi.org/10.3390/jfmk9040247
APA StyleVavourakis, M., Galanis, A., Zachariou, D., Sakellariou, E., Patilas, C., Karampinas, P., Kaspiris, A., Rozis, M., Vlamis, J., Vasiliadis, E., & Pneumaticos, S. (2024). The Impact of Rotational Malalignment Following Intramedullary Nailing for Intertrochanteric Fractures on Patients’ Functional Outcomes: A Prospective Study. Journal of Functional Morphology and Kinesiology, 9(4), 247. https://doi.org/10.3390/jfmk9040247








