Lifestyle as a Modulator of the Effects on Fitness of an Integrated Neuromuscular Training in Primary Education
Abstract
1. Introduction
2. Materials and Methods
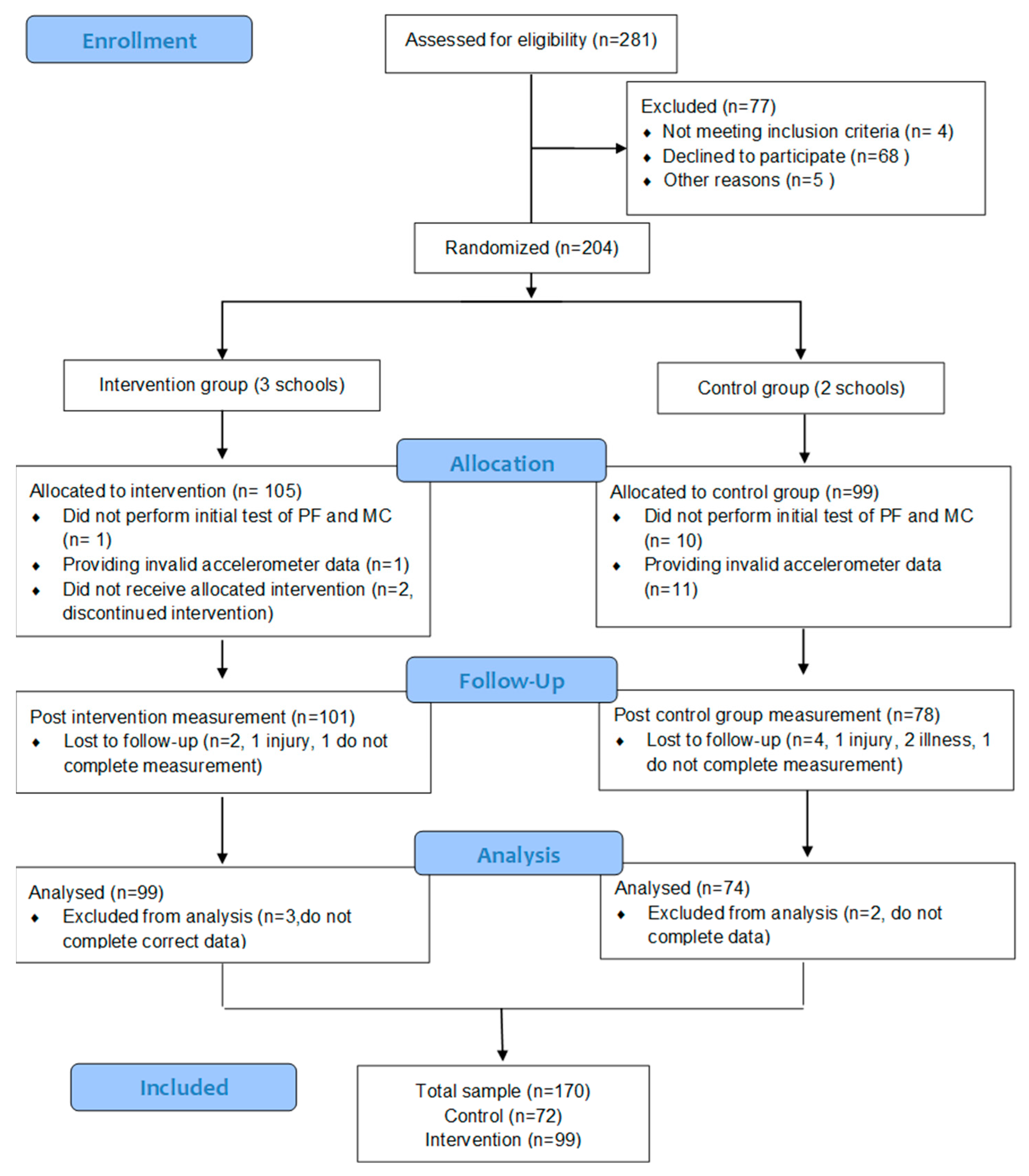
2.1. Subjects
2.2. Measurements
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef]
- Malina, R.M. Physical activity and fitness: Pathways from childhood to adulthood. Am. J. Hum. Biol. 2001, 13, 162–172. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Alonso-Martínez, A.M.; Ramírez-Vélez, R.; Pérez-Sousa, M.Á.; Ramírez-Campillo, R.; Izquierdo, M. Association of Physical Education with Improvement of Health-Related Physical Fitness Outcomes and Fundamental Motor Skills Among Youths: A Systematic Review and Meta-analysis. JAMA Pediatr. 2020, 174, e200223. [Google Scholar] [CrossRef]
- Mintjens, S.; Menting, M.D.; Daams, J.G.; van Poppel, M.N.M.; Roseboom, T.J.; Gemke, R.J.B.J. Cardiorespiratory Fitness in Childhood and Adolescence Affects Future Cardiovascular Risk Factors: A Systematic Review of Longitudinal Studies. Sports Med. 2018, 48, 2577–2605. [Google Scholar] [CrossRef]
- Fühner, T.; Kliegl, R.; Arntz, F.; Kriemler, S.; Granacher, U. An Update on Secular Trends in Physical Fitness of Children and Adolescents from 1972 to 2015: A Systematic Review. Sports Med. 2021, 51, 303–320. [Google Scholar] [CrossRef]
- Smith, L.; Fisher, A.; Hamer, M. Prospective association between objective measures of childhood motor coordination and sedentary behaviour in adolescence and adulthood. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 75. [Google Scholar] [CrossRef]
- Zaqout, M.; Vyncke, K.; Moreno, L.A.; De Miguel-Etayo, P.; Lauria, F.; Molnar, D.; Lissner, L.; Hunsberger, M.; Veidebaum, T.; Tornaritis, M.; et al. Determinant factors of physical fitness in European children. Int. J. Public Health 2016, 61, 573–582. [Google Scholar] [CrossRef]
- Silventoinen, K.; Maia, J.; Jelenkovic, A.; Pereira, S.; Gouveia, É.; Antunes, A.; Thomis, M.; Lefevre, J.; Kaprio, J.; Freitas, D. Genetics of somatotype and physical fitness in children and adolescents. Am. J. Hum. Biol. 2021, 33, e23470. [Google Scholar] [CrossRef]
- Stodden, D.F.; Langendorfer, S.J.; Roberton, M.A.; Kelbley, L. Association between motor skill competence and health-related physical fitness. J. Sport Exerc. Psychol. 2007, 29, S45–S46. [Google Scholar]
- Barnett, L.M.; Webster, E.K.; Hulteen, R.M.; De Meester, A.; Valentini, N.C.; Lenoir, M.; Pesce, C.; Getchell, N.; Lopes, V.P.; Robinson, L.E.; et al. Through the Looking Glass: A Systematic Review of Longitudinal Evidence, Providing New Insight for Motor Competence and Health. Sports Med. 2022, 52, 875–920. [Google Scholar] [CrossRef]
- MacNamara, Á.; Collins, D.; Giblin, S. Just let them play? Deliberate preparation as the most appropriate foundation for lifelong physical activity. Front. Psychol. 2015, 6, 1548. [Google Scholar] [CrossRef]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor Competence and its Effect on Positive Developmental Trajectories of Health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef] [PubMed]
- Bel-Serrat, S.; Ojeda-Rodríguez, A.; Heinen, M.M.; Buoncristiano, M.; Abdrakhmanova, S.; Duleva, V.; Sant’Angelo, V.F.; Fijałkowska, A.; Hejgaard, T.; Huidumac, C.; et al. Clustering of Multiple Energy Balance-Related Behaviors in School Children and its Association with Overweight and Obesity-WHO European Childhood Obesity Surveillance Initiative (COSI 2015⁻2017). Nutrients 2019, 11, 511. [Google Scholar] [CrossRef] [PubMed]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Association of cardiorespiratory fitness levels with dietary habits and lifestyle factors in schoolchildren. Appl. Physiol. Nutr. Metab. 2019, 44, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Deci, E.L.; Ryan, R.M. Handbook of Self-Determination Research; University of Rochester Press: Rochester, New York, USA, 2002. [Google Scholar]
- Hagger, M.S.; Chatzisarantis, N.L. The Trans-Contextual Model of Autonomous Motivation in Education: Conceptual and Empirical Issues and Meta-Analysis. Rev. Educ. Res. 2016, 86, 360–407. [Google Scholar] [CrossRef]
- UNESCO Quality Physical Education (QPE) Guidelines for Policy-Makers; United Nations Educational, Scientific and Cultural Organization: Paris, France, 2015; Available online: http://unesdoc.unesco.org/images/0023/002311/231101E.pdf (accessed on 3 January 2023).
- Hollis, J.L.; Williams, A.J.; Sutherland, R.; Campbell, E.; Nathan, N.; Wolfenden, L.; Morgan, P.J.; Lubans, D.R.; Wiggers, J. A systematic review and meta-analysis of moderate-to-vigorous physical activity levels in elementary school physical education lessons. Prev. Med. 2016, 86, 34–54. [Google Scholar] [CrossRef]
- Kalajas-Tilga, H.; Hein, V.; Koka, A.; Tilga, H.; Raudsepp, L.; Hagger, M.S. Trans-Contextual Model Predicting Change in Out-of-School Physical Activity: A One-Year Longitudinal Study. Eur. Phys. Educ. Rev. 2022, 28, 463–481. [Google Scholar] [CrossRef]
- Errisuriz, V.L.; Golaszewski, N.M.; Born, K.; Bartholomew, J.B. Systematic Review of Physical Education-Based Physical Activity Interventions Among Elementary School Children. J. Prim. Prev. 2018, 39, 303–327. [Google Scholar] [CrossRef]
- Myer, G.D.; Faigenbaum, A.D.; Chu, D.A.; Falkel, J.; Ford, K.R.; Best, T.M.; Hewett, T.E. Integrative training for children and adolescents: Techniques and practices for reducing sports-related injuries and enhancing athletic performance. Phys. Sportsmed. 2011, 39, 74–84. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; Myer, G.D.; Farrell, A.; Radler, T.; Fabiano, M.; Kang, J.; Ratamess, N.; Khoury, J.; Hewett, T.E. Integrative neuromuscular training and sex-specific fitness performance in 7-year-old children: An exploratory investigation. J. Athl. Train. 2014, 49, 145–153. [Google Scholar] [CrossRef]
- Font-Lladó, R.; López-Ros, V.; Montalvo, A.M.; Sinclair, G.; Prats-Puig, A.; Fort-Vanmeerhaeghe, A. Pedagogical Approach to Integrative Neuromuscular Training to Improve Motor Competence in Children: A Randomized Controlled Trail. J. Strength Cond. Res. 2020, 34, 3078–3085. [Google Scholar] [CrossRef]
- Sinđić, M.; Mačak, D.; Todorović, N.; Purda, B.; Batez, M. Effect of Integrated Neuromuscular Exercise in Physical Education Class on Health-Related Fitness in Female Children. Healthcare 2021, 9, 312. [Google Scholar] [CrossRef] [PubMed]
- Zeng, N.; Johnson, S.L.; Boles, R.E.; Bellows, L.L. Social-ecological correlates of fundamental movement skills in young children. J. Sport Health Sci. 2019, 8, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Galiano, I.M.; Connor, J.D.; Gómez-Ruano, M.A.; Torres-Luque, G. Students’ Physical Activity Profiles According to Children’s Age and Parental Educational Level. Children 2021, 8, 516. [Google Scholar] [CrossRef]
- Álvarez, C.; Guzmán-Guzmán, I.P.; Latorre-Román, P.Á.; Párraga-Montilla, J.; Palomino-Devia, C.; Reyes-Oyola, F.A.; Paredes-Arévalo, L.; Leal-Oyarzún, M.; Obando-Calderón, I.; Cresp-Barria, M.; et al. Association between the Sociodemographic Characteristics of Parents with Health-Related and Lifestyle Markers of Children in Three Different Spanish-Speaking Countries: An Inter-Continental Study at OECD Country Level. Nutrients 2021, 13, 2672. [Google Scholar] [CrossRef]
- de la Puente, M.L.; Canela, J.; Alvarez, J.; Salleras, L.; Vicens-Calvet, E. Cross-sectional growth study of the child and adolescent population of Catalonia (Spain). Ann. Hum. Biol. 1997, 24, 435–452. [Google Scholar] [CrossRef] [PubMed]
- Adam, C.; Klissouras, V.; Ravazzolo, M.; Renson, R.; Tuxworth, W.; Kemper, H.C.G.; van Mechelen, W.; Hlobil, H.; Beunen, G.; Levarlet-Joye, H. EUROFIT—European Test of Physical Fitness, 2nd ed.; Committee for the development of sport. (2 ed.); Council of Europe: London, UK, 1993. [Google Scholar]
- Castro-Piñero, J.; González-Montesinos, J.L.; Mora, J.; Keating, X.D.; Girela-Rejón, M.J.; Sjöström, M.; Ruiz, J.R. Percentile values for muscular strength field tests in children aged 6 to 17 years: Influence of weight status. J. Strength Cond. Res. 2009, 23, 2295–2310. [Google Scholar] [CrossRef]
- Castro-Piñero, J.; Ortega, F.B.; Artero, E.G.; Girela-Rejón, M.J.; Mora, J.; Sjöström, M.; Ruiz, J.R. Assessing muscular strength in youth: Usefulness of standing long jump as a general index of muscular fitness. J. Strength Cond. Res. 2010, 24, 1810–1817. [Google Scholar] [CrossRef] [PubMed]
- Hänggi, J.M.; Phillips, L.R.S.; Rowlands, A.V. Validation of the GT3X ActiGraph in children and comparison with the GT1M ActiGraph. J. Sci. Med. Sport 2013, 16, 40–44. [Google Scholar] [CrossRef]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef]
- Chaput, J.P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: Summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A. Mediterranean diet as intangible heritage of humanity: 10 years on. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1943–1948. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Duncan, M.J.; Eyre, E.; Oxford, S.W. The Effects of 10-week Integrated Neuromuscular Training on Fundamental Movement Skills and Physical Self-efficacy in 6–7-Year-Old Children. J. Strength Cond. Res. 2018, 32, 3348–3356. [Google Scholar] [CrossRef] [PubMed]
- Faigenbaum, A.D.; Farrell, A.; Fabiano, M.; Radler, T.; Naclerio, F.; Ratamess, N.A.; Kang, J.; Myer, G.D. Effects of integrative neuromuscular training on fitness performance in children. Pediatr. Exerc. Sci. 2011, 23, 573–584. [Google Scholar] [CrossRef]
- Boyle-Holmes, T.; Grost, L.; Russell, L.; Laris, B.A.; Robin, L.; Haller, E.; Potter, S.; Lee, S. Promoting elementary physical education: Results of a school-based evaluation study. Health Educ. Behav. 2010, 37, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, T.B.; Sanders, T.; Vasconcellos, D.; Noetel, M.; Parker, P.D.; Lubans, D.R.; Andrade, S.; Ávila-García, M.; Bartholomew, J.; Belton, S.; et al. School-based interventions modestly increase physical activity and cardiorespiratory fitness but are least effective for youth who need them most: An individual participant pooled analysis of 20 controlled trials. Br. J. Sports Med. 2021, 55, 721–729. [Google Scholar] [CrossRef] [PubMed]
- Castro-Piñero, J.; González-Montesinos, J.L.; Mora, J.; Keating, X.D.; Girela-Rejón, M.J.; Sjöström, M.; Ruiz, J.R. Percentile values for aerobic performance running/walking field tests in children aged 6 to 17 years: Influence of weight status. Nutr. Hosp. 2011, 26, 572–578. [Google Scholar] [CrossRef]
- Marrodán Serrano, M.D.; Romero Collazos, J.F.; Moreno Romero, S.; Mesa Santurino, M.S.; Cabañas Armesilla, M.D.; Pacheco Del Cerro, J.L.; González-Montero de Espinosa, M. Dinamometría en niños y jóvenes de entre 6 y 18 años: Valores de referencia, asociación con tamaño y composición corporal [Handgrip strength in children and teenagers aged from 6 to 18 years: Reference values and relationship with size and body composition]. An. Pediatr. 2009, 70, 340–348. [Google Scholar] [CrossRef]
- Cameron, N.; Humbert, L. ‘Strong Girls’ in physical education: Opportunities for social justice education. Sport Educ. Soc. 2020, 25, 249–250. [Google Scholar] [CrossRef]
- White, R.L.; Bennie, A.; Vasconcellos, D.; Cinelli, R.; Hilland, T.; Owen, K.B.; Lonsdale, C. Self-determination theory in physical education: A systematic review of qualitative studies. Teach. Teach. Educ. 2021, 99, 103247. [Google Scholar] [CrossRef]
- Herrera-Ramos, E.; Tomaino, L.; Sánchez-Villegas, A.; Ribas-Barba, L.; Gómez, S.F.; Wärnberg, J.; Osés, M.; González-Gross, M.; Gusi, N.; Aznar, S.; et al. Trends in Adherence to the Mediterranean Diet in Spanish Children and Adolescents across Two Decades. Nutrients 2023, 15, 2348. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Román-Viñas, B.; Sanchez-Villegas, A.; Guasch-Ferré, M.; Corella, D.; La Vecchia, C. Benefits of the Mediterranean diet: Epidemiological and molecular aspects. Mol. Aspects Med. 2019, 67, 1–55. [Google Scholar] [CrossRef] [PubMed]
- Posadzki, P.; Pieper, D.; Bajpai, R.; Makaruk, H.; Könsgen, N.; Neuhaus, A.L.; Semwal, M. Exercise/physical activity and health outcomes: An overview of Cochrane systematic reviews. BMC Public Health 2020, 20, 1724. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Ramirez Varela, A.; Bauman, A.E.; Ekelund, U.; Lee, I.M.; Heath, G.; Katzmarzyk, P.T.; Reis, R.; Pratt, M. Towards better evidence-informed global action: Lessons learnt from the Lancet series and recent developments in physical activity and public health. Br. J. Sports Med. 2020, 54, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Elsenburg, L.K.; Corpeleijn, E.; van Sluijs, E.M.; Atkin, A.J. Clustering and correlates of multiple health behaviours in 9–10 year old children. PLoS ONE 2014, 9, e99498. [Google Scholar] [CrossRef]
- Warburton, D.; Bredin, S. Health Benefits of Physical Activity: A Strengths-Based Approach. J. Clin. Med. 2019, 8, 2044. [Google Scholar] [CrossRef]
| All (n = 170) | Boys (n = 82) | Girls (n = 88) | p-Value | |
|---|---|---|---|---|
| Clinical Variables | ||||
| Age (y) | 7.45 ± 0.34 | 7.43 ± 0.32 | 7.47 ± 0.35 | 0.529 |
| Weight (kg) | 25.95 ± 4.2 | 25.68 ± 3.74 | 26.23 ± 4.77 | 0.409 |
| Height (cm) | 124.5 ± 14.89 | 124.7± 15.03 | 124.4 ± 14.76 | 0.869 |
| BMI (kg/m2) | 16.18 ± 2.27 | 16.08 ± 1.72 | 16.29 ± 2.83 | 0.566 |
| BMI SDS | −0.29 ± 0.75 | −0.38 ± 0.68 | −0.21 ± 0.83 | 0.154 |
| Fat Mass (%) | 20.38 ± 6.07 | 18.74 ± 4.97 | 21.72 ± 6.57 | 0.001 |
| Caucasian (%) | 73.9 | 76.9 | 71.1 | -- |
| High Parental Education (%) | 41.63 | 33.58 | 40.28 | -- |
| Physical Fitness | ||||
| Speed-agility (s) | 25.02 ± 2.81 | 23.99 ± 2.58 | 26.05 ± 3.04 | <0.0001 |
| Cardiorespiratory fitness (min) | 5.22 ± 0.69 | 4.93 ± 0.61 | 5.52 ± 0.78 | <0.0001 |
| Lower-limb muscular strength (cm) | 96.20 ± 14.37 | 103.54 ± 16.09 | 88.87 ± 12.65 | <0.0001 |
| Upper-limb muscular strength (kg) | 10.5 ± 2.47 | 10.69 ± 2.37 | 10.31 ± 2.58 | 0.348 |
| Physical Activity | ||||
| Sedentary (min/d) | 450.69 ± 75.69 | 441.85 ± 81.43 | 459.54 ± 69.96 | 0.130 |
| Light (min/d) | 293.05 ± 48.13 | 290.87 ± 56.74 | 295.24 ± 39.53 | 0.560 |
| MVPA (min/d) | 66.01 ± 21.87 | 73.69 ± 24.95 | 58.34 ± 18.79 | <0.0001 |
| Lifestyle behaviors | ||||
| Mediterranean Diet (points) | 6.29 ± 2.10 | 6.29 ± 1.93 | 6.29 ± 2.25 | 0.993 |
| Sleep Time (h) | 9.54 ± 1.07 | 9.35 ± 1.15 | 9.73 ± 0.99 | 0.022 |
| Adherence to lifestyle recommendations (%) | ||||
| Physical Activity (%) | 55.3 | 70.7 | 40.9 | <0.0001 |
| Mediterranean Diet (%) | 31.2 | 28.0 | 34.1 | 0.395 |
| Sleep Time (%) | 29.4 | 23.2 | 35.2 | 0.086 |
| Boys | Girls | ||||||
|---|---|---|---|---|---|---|---|
| Δ (Post-Pre) | p-Value | Cohen’s Effect Size | Δ (Post-Pre) | p-Value | Cohen’s Effect Size | ||
| Speed-agility (s) * | Control | −0.46 ± 1.43 | 0.111 | 0.24 | −0.28 ± 1.45 | 0.319 | 0.15 |
| Intervention | −1.73 ± 1.11 | <0.0001 | 0.7 | −1.40 ± 1.38 | <0.0001 | 0.51 | |
| p-value | 0.002 | 0.004 | |||||
| CRF (min) * | Control | −0.12 ± 0.47 | 0.241 | 0.2 | −0.039 ± 0.58 | 0.765 | 0.07 |
| Intervention | −0.14 ± 0.56 | 0.220 | 0.36 | −0.11 ± 0.51 | 0.245 | 0.16 | |
| p-value | 0.87 | 0.637 | |||||
| LLMS (cm) | Control | 0.99 ± 10.76 | 0.645 | 0.06 | 2.07 ± 8.28 | 0.189 | 0.18 |
| Intervention | 5.24 ± 9.35 | 0.012 | 0.32 | 5.79 ± 9.72 | 0.004 | 0.51 | |
| p-value | 0.144 | 0.124 | |||||
| ULMS (kg) | Control | 0.21 ± 1.10 | 0.369 | 0.1 | −0.10 ± 1.24 | 0.723 | 0.04 |
| Intervention | 0.26 ± 1.05 | 0.144 | 0.1 | 0.76 ± 1.21 | <0.0001 | 0.3 | |
| p-value | 0.870 | 0.011 | |||||
| BMI SDS * (kg/m2) | Control | −0.02 ± 0.43 | 0.452 | 0.05 | −0.03 ± 0.45 | 0.157 | 0.05 |
| Intervention | 0.03 ± 0.19 | 0.211 | 0.07 | −0.11 ± 0.42 | <0.0001 | 0.12 | |
| p-value | 0.159 | 0.055 | |||||
| Fat Mass (%) | Control | −0.02 ± 1.47 | 0.896 | 0.01 | −0.14 ± 1.73 | 0.568 | 0.03 |
| Intervention | 0.35 ± 3.26 | 0.367 | 0.07 | 0.89 ± 2.40 | 0.001 | 0.13 | |
| p-value | 0.506 | 0.037 | |||||
| Physical Activity Recommendations | Parental Education | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Compliant | Compliant | Low | High | ||||||
| Δ (Post-Pre) | Cohen’s Effect Size | Δ (Post-Pre) | Cohen’s Effect Size | Δ (Post-Pre) | Cohen’s Effect Size | Δ (Post-Pre) | Cohen’s Effect Size | ||
| Speed-agility (s) * | Cont | −0.42 ± 1.57 | 0.2 | −0.32 ± 1.33 | 0.16 | −0.50 ± 1.56 † | 0.021 | −0.34 ± 1.51 | 0.161 |
| Int | −1.24 ± 1.19 ‡ | 0.53 | −1.84 ± 1.35 ‡ | 0.73 | −1.43 ± 1.64 ‡ | 0.59 | −1.62 ± 1.21 ‡ | 0.72 | |
| p-value | 0.039 | <0.0001 | 0.006 | <0.001 | |||||
| CRF (min) * | Cont | −0.13 ± 0.56 | 0.23 | −0.04 ± 0.50 | 0.07 | −0.16 ± 0.52 | 0.228 | −0.06 ± 0.50 | 0.097 |
| Int | −0.05 ± 0.51 | 0.07 | −0.20 ± 0.56 | 0.28 | −0.11 ± 0.70 | 0.14 | −0.28 ± 0.63 ‡ | 0.34 | |
| p-value | 0.622 | 0.286 | 0.741 | 0.137 | |||||
| LLMS (cm) | Cont | −0.26 ± 9.05 | 0.02 | 2.96 ± 9.67 | 0.19 | 2.98 ± 9.41 † | 0.187 | 1.60 ± 11.04 | 0.097 |
| Int | 5.64 ± 7.67 ‡ | 0.37 | 5.44 ± 11.12 † | 0.32 | 5.76 ± 12.54 ‡ | 0.34 | 2.62 ± 16.10 | 0.015 | |
| p-value | 0.016 | 0.372 | 0.229 | 0.758 | |||||
| ULMS (kg) | Cont | 0.25 ± 1.21 | 0.11 | 0.30 ± 1.10 | 0.14 | −0.09 ± 1.28 | 0.04 | 0.13 ± 1.18 | 0.053 |
| Int | 0.61 ± 1.28 ‡ | 0.27 | 0.48 ± 1.06 ‡ | 0.22 | 0.45 ± 1.49 | 0.17 | 1.04 ± 1.25 ‡ | 0.4 | |
| p-value | 0.023 | 0.525 | 0.125 | 0.003 | |||||
| BMI SDS *(kg/m2) | Cont | −0.05 ± 0.19 | 0.07 | 0.01 ± 0.16 | 0.04 | −0.03 ± 0.27 | 0.01 | −0.07 ± 0.15 ‡ | 0.37 |
| Int | −0.69 ± 0.19 † | 0.09 | 0.01 ± 0.29 | 0.04 | −0.05 ± 0.21 † | 0.01 | −0.05 ± 0.20 | 0.44 | |
| p-value | 0.764 | 0.928 | 0.554 | 0.527 | |||||
| Fat Mass (%) | Cont | −0.10 ± 1.77 | 0.01 | 0.01 ± 1.44 | 0.01 | 0.28 ± 1.50 | 0.05 | −0.30 ± 1.60 | 0.05 |
| Int | −0.85 ± 2.72 † | 0.14 | −0.59 ± 3.04 | 0.09 | −0.83 ± 3.49 † | 0.12 | −0.51 ± 1.77 † | 0.08 | |
| p-value | 0.114 | 0.208 | 0.012 | 0.561 | |||||
| All ChildrenM OR (95% CI) | Non-Compliant (PA) OR (95% CI) | Compliant (PA) OR (95% CI) | Low PEL OR (95% CI) | High PEL OR (95% CI) | |
|---|---|---|---|---|---|
| Speed-agility | |||||
| Basal | 2.51 (1.84–3.42) *** | 3.03 (1.77–5.20) *** | 2.48 (1.54–3.99) *** | 3.22 (1.91–5.43) *** | 2.22 (1.39–3.53) *** |
| Intervention | 2.50 (0.92–6.79) | 2.93 (0.61–14.10) | 1.60 (0.36–7.11) | 2.90 (0.70–11.99) | 1.92 (0.37–9.96) |
| Cardiorespiratory fitness | |||||
| Basal | 6.16 (3.06–12.40) *** | 8.62 (2.71–27.37) *** | 6.02 (1.94–18.66) *** | 5.91 (2.72–16.04) *** | 7.64 (2.36–24.79) ** |
| Intervention | 0.81 (0.37–1.80) | 0.46 (0.13–1.55) | 1.27 (0.37–4.36) | 0.51 (0.16–1.58) | 1.94 (0.52–7.29) |
| Lower-limb muscular strength | |||||
| Basal | 1.14 (1.09–1.18) *** | 1.19 (1.07–1.32) *** | 1.13 (1.06–1.21) *** | 1.17 (1.10–1.26) *** | 1.09 (1.03–1.14) ** |
| Intervention | 1.19 (0.54–2.62) | 0.61 (0.12–3.10) | 4.64 (1.10–19.54) * | 1.23 (0.39–3.85) | 1.28 (0.38–4.26) |
| Upper-limb muscular strength | |||||
| Basal | 1.67 (1.45–1.92) *** | 1.87 (1.41–2.48) *** | 1.65 (1.35–2.01) *** | 2.87 (1.86–4.42) *** | 4.40 (2.21–8.79) *** |
| Intervention | 0.62 (0.25–1.53) | 0.63 (0.13–3.09) | 0.38 (0.10–1.43) | 1.16 (0.30–4.49) | 0.08 (0.01–0.60) * |
| Body mass index | |||||
| Basal | 24.19 (8.89–65.82) *** | 13.89 (3.99–48.35) *** | 175 (11.00–2684) *** | 12.81 (4.34 –37.82) *** | 86.44 (8.31–899.06) *** |
| Intervention | 0.18 (0.05–0.58) ** | 0.14 (0.03–0.80) * | 0.20 (0.03–1.20) | 0.52 (0.14–1.96) | 0.07 (0.00–1.00) * |
| Fat mass (%) | |||||
| Basal | 2.66 (2.03–3.48) *** | 2.70 (1.75–4.18) *** | 3.14 (2.02–4.89) *** | 9.42 (4.17–21.28) *** | 9.38 (3.41–25.80) *** |
| Intervention | 1.28 (0.48–3.41) | 4.75 (0.83–27.27) | 1.93 (0.40–9.44) | 2.70 (0.67–10.88) | 0.91 (0.22–3.82) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roman-Viñas, B.; Vasileva, F.; Font-Lladó, R.; Aznar-Laín, S.; Jiménez-Zazo, F.; Lopez-Bermejo, A.; López-Ros, V.; Prats-Puig, A. Lifestyle as a Modulator of the Effects on Fitness of an Integrated Neuromuscular Training in Primary Education. J. Funct. Morphol. Kinesiol. 2024, 9, 117. https://doi.org/10.3390/jfmk9030117
Roman-Viñas B, Vasileva F, Font-Lladó R, Aznar-Laín S, Jiménez-Zazo F, Lopez-Bermejo A, López-Ros V, Prats-Puig A. Lifestyle as a Modulator of the Effects on Fitness of an Integrated Neuromuscular Training in Primary Education. Journal of Functional Morphology and Kinesiology. 2024; 9(3):117. https://doi.org/10.3390/jfmk9030117
Chicago/Turabian StyleRoman-Viñas, Blanca, Fidanka Vasileva, Raquel Font-Lladó, Susana Aznar-Laín, Fabio Jiménez-Zazo, Abel Lopez-Bermejo, Victor López-Ros, and Anna Prats-Puig. 2024. "Lifestyle as a Modulator of the Effects on Fitness of an Integrated Neuromuscular Training in Primary Education" Journal of Functional Morphology and Kinesiology 9, no. 3: 117. https://doi.org/10.3390/jfmk9030117
APA StyleRoman-Viñas, B., Vasileva, F., Font-Lladó, R., Aznar-Laín, S., Jiménez-Zazo, F., Lopez-Bermejo, A., López-Ros, V., & Prats-Puig, A. (2024). Lifestyle as a Modulator of the Effects on Fitness of an Integrated Neuromuscular Training in Primary Education. Journal of Functional Morphology and Kinesiology, 9(3), 117. https://doi.org/10.3390/jfmk9030117









