The Relationship between Inspiratory Muscle Strength and Cycling Performance: Insights from Hypoxia and Inspiratory Muscle Warm-Up
Abstract
1. Introduction
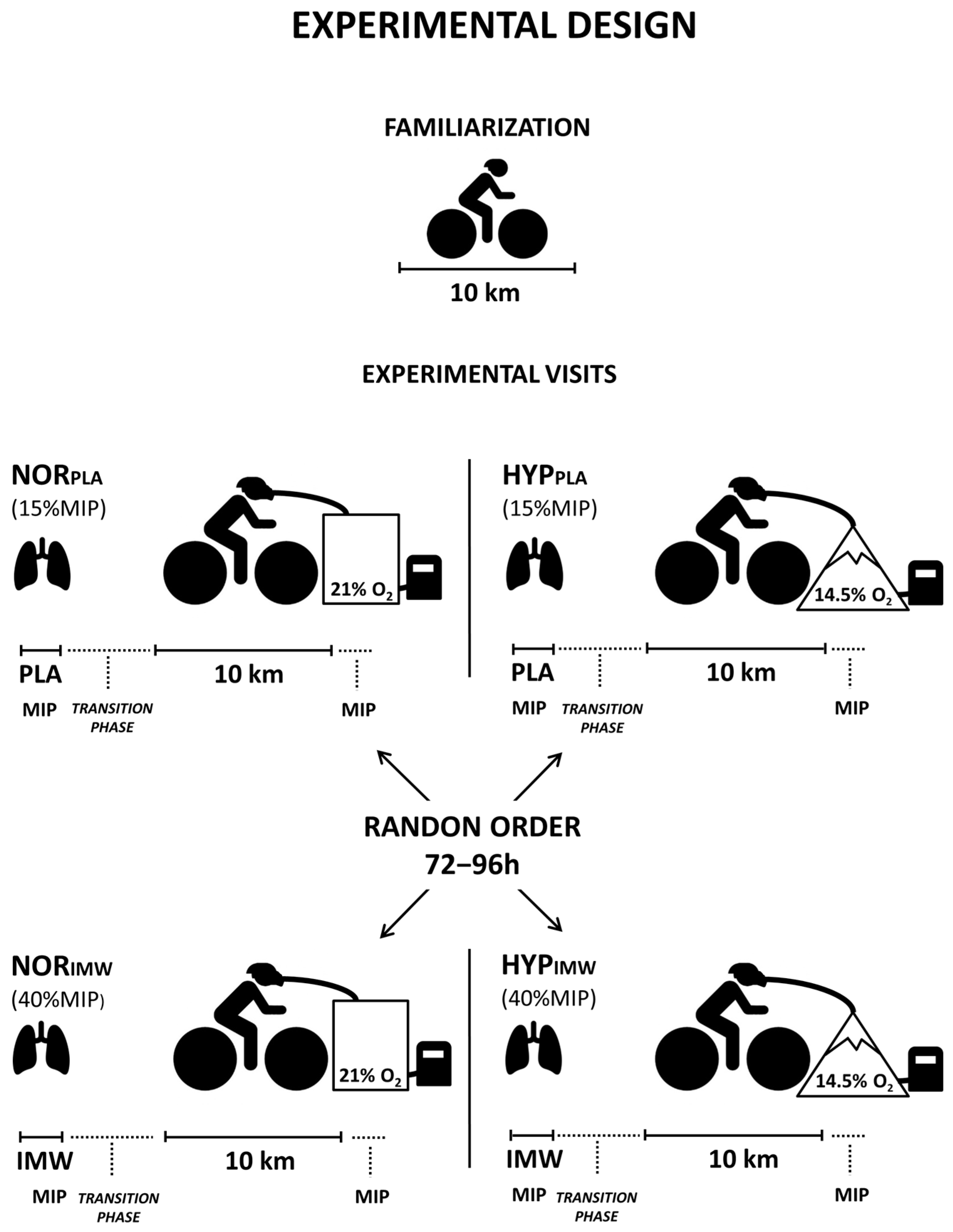
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Materials
2.4. Familiarization with Time Trial and IMW
2.5. Time Trial Tests
2.6. Inspiratory Muscle Pressure
2.7. Inspiratory Muscle Warm-Up and Placebo
2.8. Statistical Analysis
3. Results
3.1. Time Trial Performance
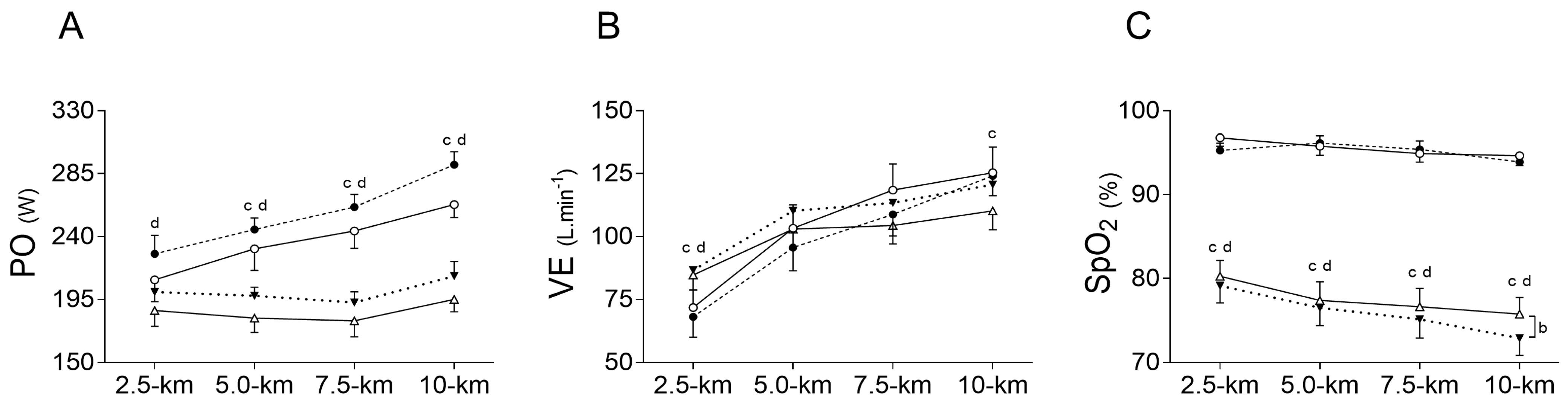
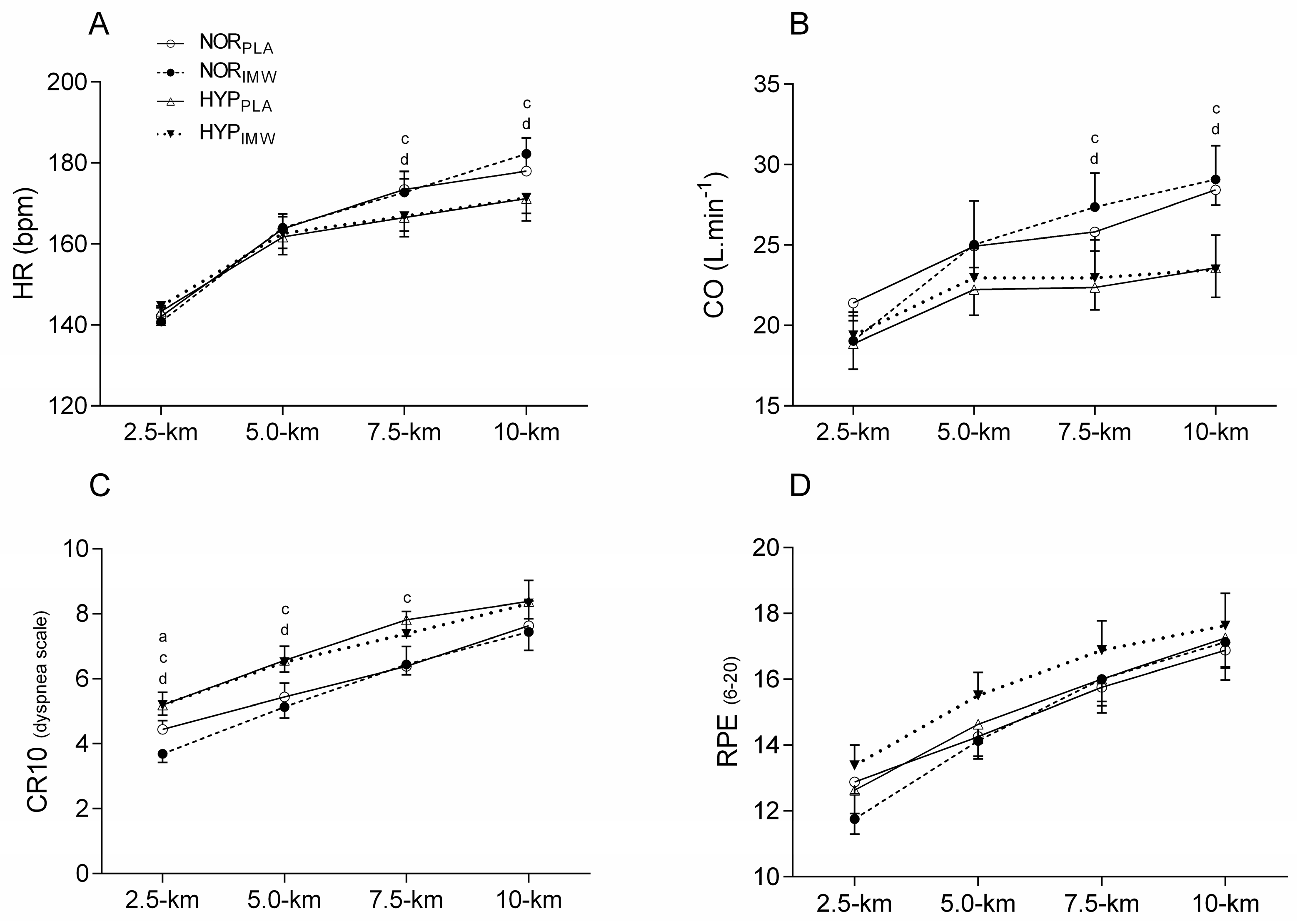
3.2. Physiological Responses
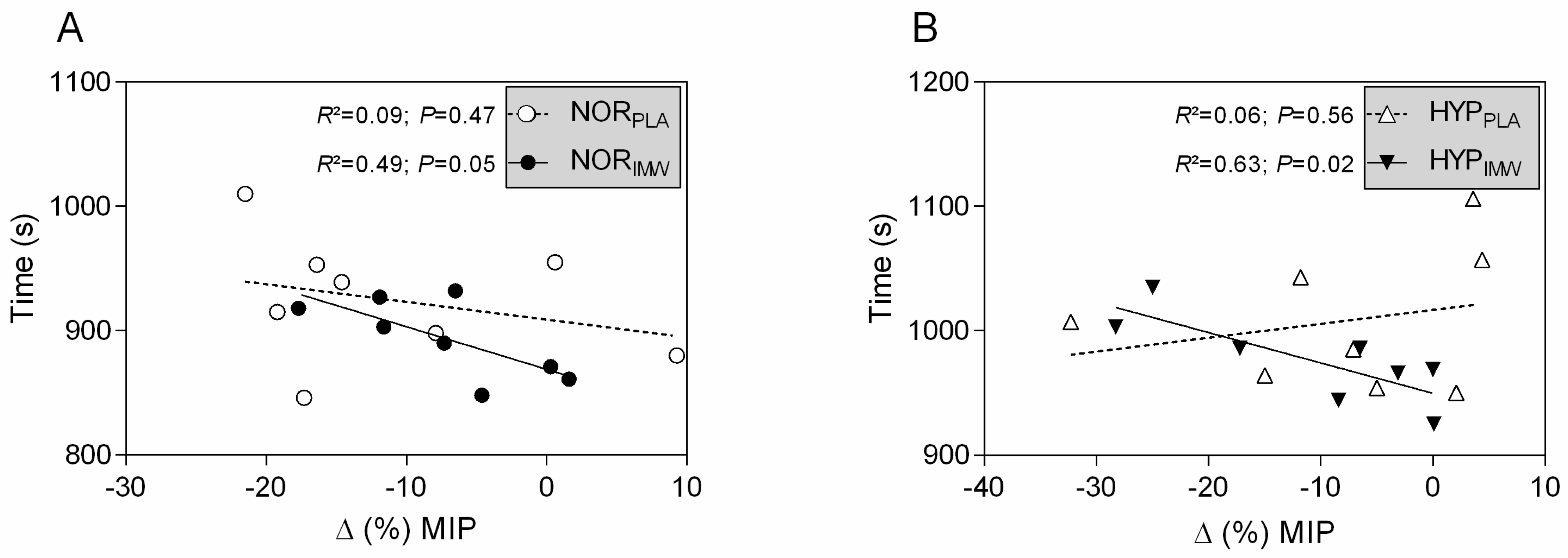
3.3. Inspiratory Strength and Exercise Time Relationships
4. Discussion
4.1. Effects of IMW in Normoxic Exercise
4.2. Effects of IMW in Hypoxic Exercise
4.3. Time Trial Performance and the Post-Exercise Inspiratory Muscle Strength Decline
4.4. Future Directions
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wüthrich, T.U.; Eberle, E.C.; Spengler, C.M. Locomotor and diaphragm muscle fatigue in endurance athletes performing time trials of different durations. Eur. J. Appl. Physiol. 2014, 114, 1619–1633. [Google Scholar] [CrossRef]
- Dempsey, J.A.; Romer, L.; Rodman, J.; Miller, J.; Smith, C. Consequences of exercise-induced respiratory muscle work. Respir. Physiol. Neurobiol. 2006, 151, 242–250. [Google Scholar] [CrossRef]
- Amann, M.; Pegelow, D.F.; Jacques, A.J.; Dempsey, J.A. Inspiratory muscle work in acute hypoxia influences locomotor muscle fatigue and exercise performance of healthy humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 293, R2036–R2045. [Google Scholar] [CrossRef]
- Babcock, M.A.; Johnson, B.D.; Pegelow, D.F.; Suman, O.E.; Griffin, D.; Dempsey, J.A. Hypoxic effects on exercise-induced diaphragmatic fatigue in normal healthy humans. J. Appl. Physiol. 1995, 78, 82–92. [Google Scholar] [CrossRef]
- Vogiatzis, I.; Georgiadou, O.; Koskolou, M.; Athanasopoulos, D.; Kostikas, K.; Golemati, S.; Wagner, H.; Roussos, C.; Wagner, P.D.; Zakynthinos, S. Effects of hypoxia on diaphragmatic fatigue in highly trained athletes. J. Physiol. 2007, 581, 299–308. [Google Scholar] [CrossRef]
- Downey, A.E.; Chenoweth, L.M.; Townsend, D.K.; Ranum, J.D.; Ferguson, C.S.; Harms, C.A. Effects of inspiratory muscle training on exercise responses in normoxia and hypoxia. Respir. Physiol. Neurobiol. 2007, 156, 137–146. [Google Scholar] [CrossRef]
- Salazar-Martínez, E.; Gatterer, H.; Burtscher, M.; Orellana, J.N.; Santalla, A. Influence of Inspiratory Muscle Training on Ventilatory Efficiency and Cycling Performance in Normoxia and Hypoxia. Front. Physiol. 2017, 8, 133. [Google Scholar] [CrossRef]
- Hursh, D.G.; Baranauskas, M.N.; Wiggins, C.C.; Bielko, S.; Mickleborough, T.D.; Chapman, R.F. Inspiratory Muscle Training: Improvement of Exercise Performance With Acute Hypoxic Exposure. Int. J. Sports Physiol. Perform. 2019, 31, 1124–1131. [Google Scholar] [CrossRef]
- Volianitis, S.; McConnell, A.K.; Koutedakis, Y.; Jones, D.A. Specific respiratory warm-up improves rowing performance and exertional dyspnea. Med. Sci. Sports Exerc. 2001, 33, 1189–1193. [Google Scholar] [CrossRef]
- Tong, T.K.; Fu, F.H. Effect of specific inspiratory muscle warm-up on intense intermittent run to exhaustion. Eur. J. Appl. Physiol. 2006, 97, 673–680. [Google Scholar] [CrossRef]
- Lin, H.; Kwokkeung, T.T.; Huang, C.; Nie, J.; Lu, K.; Quach, B. Specific inspiratory muscle warm-up enhances badminton footwork performance. Appl. Physiol. Nutr. Metab. 2007, 32, 1082–1088. [Google Scholar] [CrossRef]
- Özdal, M.; Bostanci, O.; Dağlioğlu, O.; Ağaoğlu, S.A.; Kabadayi, M. Effect of respiratory warm-up on anaerobic power. J. Phys. Ther. Sci. 2016, 28, 2097–2098. [Google Scholar] [CrossRef]
- Cirino, C.; Marostegan, A.B.; Hartz, C.S.; Moreno, M.A.; Gobatto, C.A.; Manchado-Gobatto, F.B. Effects of Inspiratory Muscle Warm-Up on Physical Exercise: A Systematic Review. Biology 2023, 12, 333. [Google Scholar] [CrossRef]
- Cheng, C.; Tong, T.K.; Kuo, Y.; Chen, P.; Huang, H.; Lee, C. Inspiratory muscle warm-up attenuates muscle deoxygenation during cycling exercise in women athletes. Respir. Physiol. Neurobiol. 2013, 186, 296–302. [Google Scholar] [CrossRef]
- Ohya, T.; Hagiwara, M.; Suzuki, Y. Inspiratory muscle warm-up has no impact on performance or locomotor muscle oxygenation during high intensity intermittent sprint cycling exercise. SpringerPlus 2015, 4, 556. [Google Scholar] [CrossRef]
- Johnson, M.A.; Gregson, I.R.; Mills, D.E.; Gonzalez, J.T.; Sharpe, G.R. Inspiratory muscle warm-up does not improve cycling time trial perfomance. Eur. J. Appl. Physiol. 2014, 114, 1821–1830. [Google Scholar] [CrossRef]
- Hawkes, E.Z.; Nowicky, A.V.; McConnell, A.K. Diaphragm and intercostal surface EMG and muscle performance after acute inspiratory muscle loading. Respir. Physiol. Neurobiol. 2007, 155, 213–219. [Google Scholar] [CrossRef]
- Lomax, M.; Grant, I.; Corbett, J. Inspiratory muscle warm-up and inspiratory muscle training: Separate and combined effects on intermittent running to exhaustion. J. Sports Sci. 2011, 29, 563–569. [Google Scholar] [CrossRef]
- Stone, M.R.; Thomas, K.; Wilkinson, M.; Gibson, A.S.C.; Thompson, K.G. Consistency of perceptual and metabolic responses to a laboratory-based simulated 4000-m cycling time trial. Eur. J. Appl. Physiol. 2011, 111, 1807–1813. [Google Scholar] [CrossRef]
- Borg, G. Borg’s Perceived Exertion and Pain Scales, 1st ed.; Human Kinetics: Champaign, IL, USA, 1998; pp. 29–43. [Google Scholar]
- Wen, A.; Marlyn, M.; Woo, S.; Keens, T. How many maneuvers are required to measure maximal inspiratory pressure accurately? Chest 1997, 111, 807. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef]
- Faghy, M.A.; Brown, P.I. Whole body active warm up and inspiratory muscle warm up do not improve running performance when carrying thoracic loads. Appl. Physiol. Nutr. Metab. 2017, 42, 810–815. [Google Scholar] [CrossRef]
- Callegaro, C.C.; Ribeiro, J.P.; Tan, C.O.; Taylor, J.A. Attenuated inspiratory muscle metaboreflex in endurance-trained individuals. Respir. Physiol. Neurobiol. 2011, 177, 24–29. [Google Scholar] [CrossRef]
- Lomax, M.; Massey, H.C.; House, J.R. Inspiratory Muscle Training Effects on Cycling During Acute Hypoxic Exposure. Aerosp. Med. Hum. Perform. 2017, 88, 544–549. [Google Scholar] [CrossRef]
- Siebenmann, C.; Lundby, C. Regulation of cardiac output in hypoxia. Scand. J. Med. Sci. Sports 2015, 25, 53–59. [Google Scholar] [CrossRef]
- Gonçalves, T.R.; Soares, P.P.D.S. Positive Pressure Ventilation Improves Exercise Performance and Attenuates the Fall of Postexercise Inspiratory Muscular Strength in Rower Athletes. J. Strength Cond. Res. 2021, 35, 253–259. [Google Scholar] [CrossRef]
| IMW Indexes | NORPLA | NORIMW | HYPPLA | HYPIMW | es NORIMW | es HYPIMW |
|---|---|---|---|---|---|---|
| Pressure (cmH2O) | 15.16 ± 3.18 | 39.84 ± 7.96 * | 15.76 ± 4.16 | 40.09 ± 8.65 # | (5.04) | (4.54) |
| Power (W) | 3.86 ± 1.91 | 11.09 ± 5.62 * | 4.47 ± 3.78 | 12.27 ± 5.42 # | (1.83) | (2.97) |
| Volume (L) | 2.92 ± 0.56 | 3.27 ± 0.78 | 2.90 ± 0.79 | 2.94 ± 0.80 | (0.44) | (0.05) |
| Flow (L/s) | 2.32 ± 0.66 | 2.48 ± 0.76 | 2.50 ± 1.34 | 2.80 ± 0.68 | (0.27) | (0.31) |
| NORPLA | NORIMW | HYPPLA | HYPIMW | |
|---|---|---|---|---|
| MIP values | ||||
| MIPPRE (cmH2O) | 135 ± 34 | 149 ± 34 | 146 ± 37 | 149 ± 36 |
| MIPPOST-EXER (cmH2O) | 120 ± 30 * (1.06) | 138 ± 35 * (1.00) | 134 ± 34 (0.56) | 132 ± 36 * (0.89) |
| MIP changes | ||||
| ∆MIPPOST-PRE (%) | −11 ± 11 | −7 ± 6 | −8 ± 12 | −11 ± 11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, A.L.M.B.; Rodrigues, G.D.; Rohan, P.d.A.; Gonçalves, T.R.; Soares, P.P.d.S. The Relationship between Inspiratory Muscle Strength and Cycling Performance: Insights from Hypoxia and Inspiratory Muscle Warm-Up. J. Funct. Morphol. Kinesiol. 2024, 9, 97. https://doi.org/10.3390/jfmk9020097
Oliveira ALMB, Rodrigues GD, Rohan PdA, Gonçalves TR, Soares PPdS. The Relationship between Inspiratory Muscle Strength and Cycling Performance: Insights from Hypoxia and Inspiratory Muscle Warm-Up. Journal of Functional Morphology and Kinesiology. 2024; 9(2):97. https://doi.org/10.3390/jfmk9020097
Chicago/Turabian StyleOliveira, André Luiz Musmanno Branco, Gabriel Dias Rodrigues, Philippe de Azeredo Rohan, Thiago Rodrigues Gonçalves, and Pedro Paulo da Silva Soares. 2024. "The Relationship between Inspiratory Muscle Strength and Cycling Performance: Insights from Hypoxia and Inspiratory Muscle Warm-Up" Journal of Functional Morphology and Kinesiology 9, no. 2: 97. https://doi.org/10.3390/jfmk9020097
APA StyleOliveira, A. L. M. B., Rodrigues, G. D., Rohan, P. d. A., Gonçalves, T. R., & Soares, P. P. d. S. (2024). The Relationship between Inspiratory Muscle Strength and Cycling Performance: Insights from Hypoxia and Inspiratory Muscle Warm-Up. Journal of Functional Morphology and Kinesiology, 9(2), 97. https://doi.org/10.3390/jfmk9020097









