Abstract
Kinetic chains (KCs) are primarily affected by the load of different activities that recruit muscles from different regions. We explored the effects of strengthening exercises on KCs through muscle activation. Four databases were searched from 1990 to 2019. The muscles of each KC, their surface electromyography (sEMG), and the exercises conducted were reported. We found 36 studies that presented muscle activation using the percent (%) maximal voluntary isometric contraction (MVIC) or average sEMG for nine KCs in different regions. The % MVIC is presented as the following four categories: low (≤20%), moderate (21~40%), high (41~60%), and very high (>60%). Only four studies mentioned muscle activation in more than three KCs, while the remaining studies reported inconsistent sEMG processing, lacked normalization, and muscle activation in one or two KCs. The roles of stabilizers and the base of support in overhead throwing mobility using balance exercises were examined, and the concentric phase of chin-up and lat pull-down activated the entire KC by recruiting multiple muscles. Also, deep-water running was shown to prevent the risk of falls and enhance balance and stability. In addition, low-load trunk rotations improved the muscles of the back and external oblique activation. Based on this study’s findings, closed-chain exercises activate more groups of muscles in a kinetic chain than open-chain exercises. However, no closed or open chain exercise can activate optimal KCs.
1. Introduction
Kinetic chains (KCs) in rehabilitation are defined [1] as “a combination of several successively arranged joints constituting a complex motor unit.” Each bony part of the lower limb, like the foot, leg, thigh, and pelvis, can be seen as a solid link, with the subtalar, ankle, knee, and hip joints serving as connections [2]. In a KC, if two ends of the rigid-link system are fixed so that no movement can occur at either end, applied external forces allow each segment to collect and transfer force to the neighboring segment, creating a chain reaction. Therefore, movement at any joint in the chain causes a consistent movement pattern with all of the other joints [3].
KCs are classified as open or closed based on the weight exerted on the terminal segment. Hence, an open KC (OKC) is “a combination of successively arranged joints in which the distal segment can move freely”, whereas a closed KC (CKC) is “a condition in which the distal segment meets considerable external resistance that restrains its free motion” [1]. It is understood that the type of KC utilized affects muscle recruitment and joint movement patterns [4]. The type and physiology of muscle contractions that underlie joint motion are intimately related. In many daily activities and sports, a common activation sequence uses a CKC, in which the action is initiated from a firm base of support, and the generated force is subsequently transferred to more mobile, distal segments through the links.
The concept of KCs provides a basis for comprehending and successively examining human movement patterns. It is also a helpful tool for executing challenging multi-joint exercises that target an entire KC of the body as a part of conditioning and rehabilitation programs [5,6]. Due to the interlinking of segments, KCs affect the proximal and distal segments’ movements [7,8] by offering several degrees of freedom and different segment positions and motions during sport-specific movements [5,6]. Sometimes, it can be challenging to differentiate between the CKC and OKC. For instance, OKC activities like swimming and cycling place a strain on the distal segment, but that segment is neither stable nor restricted from movement [9].
Myofascial chains (MCs) [10] have recently arisen, which contrasts the KC idea [11,12,13]. MCs describe anatomical and neurophysiological observations that suggest the fascia, a soft tissue with viscoelasticity, features as a functional envelopment linking muscles throughout the entire body, enabling rich sensorimotor communication between body segments [11,12,13]. This notion of neural and musculoskeletal systems acting as interconnected neuromuscular chains goes beyond the current paradigm of understanding musculoskeletal functioning as several isolated single-joint muscular origins and insertions [14]. This myofascial force transmission theory has been supported by several investigations, which contend that intermuscular chains transmit forces to the surrounding tissues through connective tissue envelopes of tendinous attachments between muscles rather than only working as isolated units [15,16].
Recent research on KCs and myofascial principles separately covers these two concepts [6,11,17,18]. These two ideas, however, might be viewed as two sides of the same coin, according to recent studies [8,11]. A study by Licen et al. [19] linked the KC approach with myofascial training in tennis players to maximize rehabilitation and prevention programs, which are primarily intended to reduce the incidence of injuries and positively influence biomechanical patterns of movement, muscle coordination, and muscle force production.
One study explored the effect of muscle activation during isometric movements (active plantar flexion) and found a strong correlation among the muscle activation of the entire kinematic chain, superficial backline (SBL) muscles at the right T12, posterior superior iliac spine (PSIS), and hamstrings. Hence, they reported that muscles do not work independently, so dysfunction in any muscle along any kinematic chain may alter activation patterns and increase myofascial pain (MFP) [20]. Another study presented the effect of changes in the trunk and lower-body position on trapezius activation and observed increased activation during unimodal squats on the contralateral leg compared to traditional seated exercises [21].
Comprehending how muscle activation in various joints interacts to produce biomechanically powerful but also safe movements could enable us to use customized conditioning and rehabilitation strategies to correct poor biomechanics. Because the malfunctioning of a KC indicates a significant injury risk, it is crucial to be aware of the frequent occurrence of pain or injury caused by inefficient biomechanics that result in changed force distributions and power outputs [19].
Strengthening exercises can be performed in a variety of ways, and each of them has an effect. Among them, resistance-band exercises are used for rotator cuff musculature training [22]. A sling exercise with eight variations in scapular retraction in overhead athletes activates the upper and lower trapezius muscles [21]. Body weight exercises like the bench press activate pectoralis major, triceps brachii, biceps brachii, deltoid, and supraspinatus muscles more than push-ups [23]. A modified closed kinetic chain knee extension activates the quadriceps more than an open kinetic chain knee extension [24].
Hence, our current study attempted to identify the evidence from existing research on training the entire KC of the human body through muscle activation. Much of the literature published on the existence of human KCs theoretically and anatomically [13,14] reports the effects of OKC or CKC exercises in a single muscle in a variety of pathological and normal conditions [6,9] including pain, disability, and muscle strength [21,25], but very few studies explore the effects of strengthening exercises on entire KC activation. Likewise, to the best of our knowledge, very little research was found to describe the suspension, sling, or three-degree-of-freedom exercise interventions [26,27,28] needed to train an entire KC and enhance physical or exercise performance. That is why we conducted a systematic review in which KCs of different regions were included, and we hypothesized that the type of exercise would affect kinetic chain activation during strengthening exercises in various regions of the body. So, the main goal of this study was to explore the effects of therapeutic exercises on the entire KCs of the upper limbs, trunk, and lower limbs, and the secondary goal was to highlight which exercises activated the entire KC in better ways to enhance physical performance compared to the single muscle activation of a KC.
2. Materials and Methods
2.1. Reporting and Registration
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement was fulfilled [29,30]. This review was registered before the initiation of the study with PROSPERO (registration no.: CRD42020142495).
2.2. The Literature Search Strategy
A search of the literature was performed from 1 January 1990 to 21 July 2019 and the first evidence of the effect of exercises on the functioning and performance of the kinetic chain was found in 1990. (Figure 1) We searched the four databases of Scopus, PubMed, Web of Science, and ScienceDirect using the following key terms: (1) ((“myofascial chain” OR “kinetic chain” OR “muscular sling” OR “anatomy train”) AND (exercise AND therapy OR strength AND training)), (2) ((“myofascial chain” OR “kinetic chain” OR “muscular sling” OR “anatomy train”) AND (“exercise therapy” OR “strength training”)), and (3) ((“myofascial chain” OR “kinetic chain” OR “muscular sling” OR “anatomy train”) AND (“exercise therapy” OR “strength training” OR ‘‘open chain’’ OR ‘‘close chain’’)).
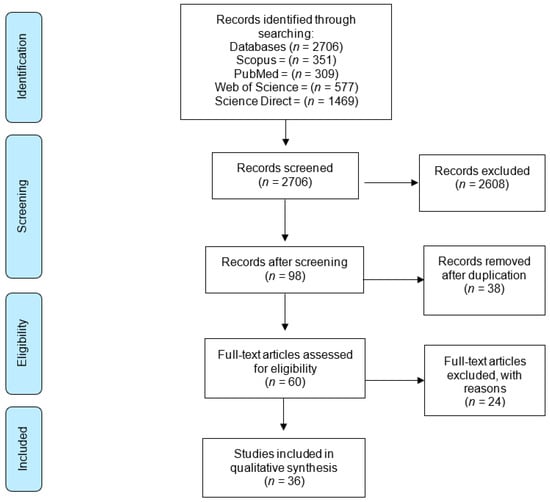
Figure 1.
PRISMA diagram.
2.3. Study Selection
The articles were selected if they (1) were written in English, (2) had healthy participants of both genders aged 15~50 years, (3) had participants with no history of a previous systemic illness, surgery, or musculoskeletal impairment, (4) were experimental studies including observational, case–control, cross-sectional, case report, quasi-experimental, and randomized controlled trials (RCTs), (5) were studies that included KCs of different regions like the upper limbs, trunk, or lower limbs, (6) were studies that mentioned the muscles included for exercise therapy, (7) examined a KC that included more than two muscles and fascia, (8) included exercise interventions in strength training that included suspension or sling and three degrees of freedom exercises [26,27,28], with such exercises being performed with some exercise gadgets like bands, cords, or exercise machines, and (9) were studies that specifically focused on outcomes related to body functions (weight maintenance and movement-related functions and activities) and participation (such as motor skills, carrying out tasks, or mobility and walking indices). Studies were excluded if they (1) reported only intervention effects (exercise therapy effects without considering human KCs, groups of muscles or describing biomechanical performance through kinematic or kinetic variables), (2) mentioned the exercise effect on muscle activity without mentioning the included muscles, (3) were anatomical studies confirming myofascial connections, (4) were studies other than those with experimental designs like qualitative surveys or theoretical studies, and (5) included exercises performed using assistive gadgets like orthosis or exercise therapy that focused on the effects of posture.
2.4. Risk of Bias Assessment
A modified version of the Quality Assessment Tool for Quantitative Studies [31] was employed to assess the quality of the articles. Two reviewers independently assessed the methodological quality of the articles according to the criteria established earlier [32]. If independent quality scores were within a 10% difference of each other, the average score of the two reviewers was used. If the scores differed by more than 10% between the reviewers, quality scoring was discussed, and if required, a third independent reviewer was consulted [33].
2.5. Quality of Reporting Assessment
The Effective Public Health Practice Project Quality Assessment Tool (EPHPP) was used to assess study designs like RCTs, before-and-after, and case–control studies. It is an effective tool for use in systematic reviews of effectiveness [34] with content and construct validities [35,36]. The EPHPP evaluates the following six domains: (1) selection bias, (2) study design, (3) confounders, (4) blinding, (5) data collection method, and (6) withdrawals/dropouts (Table 2). Each domain was scored as strong (3 points), moderate (2 points), or weak (1 point), and scores were averaged to obtain a total score or overall quality. Depending on the overall score, studies were given a quality rating of weak (1.00–1.50), moderate (1.51–2.50), or strong (2.51–3.00) [31].
2.6. Data Extraction and Analysis
The characteristics of participants (the number of participants, age, gender, weight, and height) [32], characteristics of the involved KCs (region, muscle, joints), outcome measurements (muscle activation, muscle strength, physical functioning, activity performance), exercise interventions (exercise type, intensity, load, and gadgets), and an improvement in performance through peak muscle activation (surface electromyography (sEMG)) or percent (%) maximal voluntary isometric contraction (MVIC) were extracted. The normalized % MVIC was used to report muscle activation (sEMG) as low (≤20% MVIC), moderate (21~40%), high (41~60%), and very high (>60%) [37,38,39,40,41]. The data of some studies were extracted from figures (if not available in tabulated form) using WebPlotDigitizer (accessed at https://automeris.io/WebPlotDigitizer/) (accessed on 5 May 2023). One reviewer extracted the data, which were then verified independently by a second reviewer. Data were tabulated in Microsoft® Office Excel (LTSC MSO (16.0.14332.20611)), and descriptive statistics were presented, including the means and SDs. Study outcome measures were (1) muscle strength through a repetition maximum (RM), manual muscle testing (MMT), and sEMG, and (2) physical functioning or activity performance through the change in activity levels after exercises assessed using a subjective tool.
3. Results
3.1. Quality of Reporting Assessment
Out of 36 studies, 6 showed moderate quality, while the remaining studies were rated as weak. Almost all studies had strong selection bias and data collection methods, but study design and blinding were weak because of smaller sample sizes, a lack of study groups, and a lack of a randomized controlled design. None of them reported confounders, and this category was rated as moderate. In addition, withdrawals and dropouts were also in the moderate category (Table 1).

Table 1.
Quality Assessment Tool for Quantitative Studies (EPHPP) (N = 36).
3.2. Participant Characteristics
The sample sizes of the included studies ranged from 5 to 47 participants of both genders. Out of 36 studies, 19 recruited both genders, 11 had only males, 4 had only females, and 2 studies did not mention gender. Ages ranged from 11 to 43 years, body weights ranged from 36 to 107 kg, and heights ranged from 143 to 185 cm (Table 2).

Table 2.
Basic demographics of participants (N = 36).
3.3. Studies Features
Out of the 36 studies, 17 were related to an upper extremity (UE), 11 to a lower extremity (LE), 2 to the trunk (Tr), 3 to UE and LE, 1 to UE and Tr, and 2 to LE and Tr.
3.3.1. Muscles
The UE included shoulder and scapular muscles, the LE included hip and knee muscles, and the Tr included abdominal and back muscles.
3.3.2. Exercises
In total, 21 out of the 36 studies tested CKC exercises with a stable or unstable base of support, isometric or isotonic muscle contractions, and only 5 studies researched OKC exercises. The remaining 10 studies did not mention whether they employed CKC or OKC exercises despite their included exercises focusing on a range of motion (ROM), balance, mobility, and isometrics.
3.4. Effects of Exercise Therapy on Human KCs
Overall, nine KCs were considered, which were the elbow, shoulder, scapula, abdomen, back of spine, pelvis, hip, knee, and ankle, based on muscle involvement. Different types of OKC, CKC, ROM, and balance exercises affected the muscle activation of a specific KC of the UE, LE, Tr, or a combination except for [22,52,59,63], which reported more than three KCs of different regions. The region-specific KCs are reported in Table 3.

Table 3.
The region and kinetic chains of the included studies (N = 36).
3.5. Exercise Type and Muscle Activation (sEMG)
The muscle activity reported through sEMG or integrated EMG (iEMG) in % MVIC normalized values is considered to present the effect of exercise therapy on KC muscles in this review. Of the 36 studies included, we did not compare the muscle activation of some studies due to the lack of a normalization process and presentation of average sEMG in microvolts (µV) or iEMG in volts (V) by (1) [44], (2) [47], (3) [69], and (4) [73]. DeCarlo et al. [73] did not report muscle activation, but rather, they interpreted outcomes based on ROM and angular velocity. There was an exception for this paper [44] because it was retracted by the journal. Therefore, we described the muscle activation of 32 studies according to the reported KCs. (Table 4).

Table 4.
Study features and outcome measures (N = 36).
3.6. Kinetic Chain Muscle Activation (sEMG)
Of the 32 studies, only 4 of them [22,52,59,63] included more than three KCs of different regions. Therefore, we describe and discuss the KC muscle activation of these studies in detail in the Discussion section.
4. Discussion
The current review is the first study to summarize the available literature on KC activation by exploring the effects of strengthening exercises. Based on these studies, the roles of stabilizers and the base of support in overhead throwing mobility using balance exercises were examined, and the concentric phase of chin-up and lat pull-down exercises were found to activate the entire KC by recruiting multiple muscles of the body. Also, deep-water running prevents the risk of falls and enhances balance and stability in elderly people. In addition, low-load trunk rotations can improve the muscles of the back and external oblique activation in athletes and healthy populations after an injury.
In all 36 studies, serratus anterior (SA), upper trapezius (UT), anterior deltoid (AD), lower trapezius (LT), and pectoralis major (PM) from the upper extremity, biceps femoris (BF), rectus femoris (RF), vastus lateralis (VL), gluteus maximus (GMax), and gluteus medius (GMed) from the lower extremity, and erector spinae (ES), rectus abdominus (RA), and external oblique (EO) from the trunk were the most often studied muscles. Muscles in a KC are sequentially activated, some of which are highly active, while others are less active. Hence, this research area can help determine the best exercise intervention to challenge or train an entire KC. Applied research on this topic is limited, which may pose greater benefits to prevent injuries and enhance physical performance through optimal muscle activation in a KC.
A study [22] reported on muscle activation in exercises with the following involved muscles: (1) airplane internal rotation: UT, LT, and BF; (2) airplane external rotation: LT, GMed, and BF; (3) lunge: UT, LT, SA, and LD; (4) get-up exercise: SA; (5) single-leg balance: UT; (6) I-band: UT, LT, and SA; (7) T-band: UT and LT; and (8) Y-band: LT was moderately active. This study included dominant-side UT, LT, SA, and LD and bilateral GMed and BF muscles with a focus on the posterior chain. In overhead throwing, stabilizers transfer kinetic energy from the lower extremity through the pelvis, trunk, and scapula onto the shoulder [74]. Therefore, stabilizers should be included in rehabilitation to prevent injury and maximize the throwing performance [22]. KC exercises (airplane ER and IR) moderately activate pelvic muscles along with the scapular musculature compared to band exercises due to the greater challenge of these muscles for single-leg balance and lumbopelvic stability. Another KC exercise, the lunge, also greatly activates scapular stabilizers (UT, LT, SA, and LD) [74]. Thus, challenging the entire KC can target not only the prime movers but also stabilizers for efficient movement performance.
Another study [52] reported that during the concentric phase, the muscle activation of the biceps brachii, latissimus dorsi, and ES were high during chin-ups, while those of LD and RA appeared high during the lat pull-down. During the eccentric phase, the activation of LD and BB was high during chin-ups, while lat pull-down showed higher activation for LD. The greater activation of BB and ES during chin-ups was due to an unstable position compared to lat pull-down, which was performed in a stable position [52]. In chin-ups, the LE can move freely in a horizontal plane, resulting in the displacement of the body’s center of gravity from the vertical alignment of holding the bar [75]. The PM, TB, and RA muscles were not affected by differences in the stability condition, as the same results were shown by previous studies [62,76,77,78]. The extent of the instability experienced by each muscle was proposed to be due to the anatomical orientation of the muscles [77]. Due to greater stability and movement demands at the glenohumeral and elbow joints, BB is highly active during chin-ups and also a biarticular muscle compared to the LD, which is a prime mover but a monoarticular muscle [77]. The higher activation of the ES during concentric chin-ups and the RA during eccentric lat pull-downs implied the engagement of core muscles to stabilize the body to a greater extent during these exercises, as mentioned by other studies [79,80,81]. However, this study performed only a sagittal plane analysis of chin-ups and lat pull-downs, but these exercises can be utilized for strengthening the upper back and arm muscles and are performed by gymnasts and rock climbers, which require the greater stability of the body while hanging from their hands [52].
One study [59] reported that the GMax, GMed, and ES had higher activation during deep water running (DWR) at slow, moderate, and fast speeds, while the AL, EO, and RA muscle activation levels were lower. The increased muscle activity during DWR and fast-speed water walking (WW) was due to an increased hip ROM, trunk forward inclination, and an unstable floating condition. Due to the large hip joint ROM, pelvic stabilization in an unstable condition was more challenging for the GMed and AL during DWR [59]. An increased hip extension caused the higher activation of the GMax and BF during DWR than land walking (LW). Also, fast-speed DWR reduces the cycle time and results in higher GMax activity to overcome water propulsion resistance, which increases as the second power of the speed [82]. To control hip extension movement and backward pelvic rotation, the RA and EO are highly active, while the ES tends to overcome water resistance [59]. This study involved trunk and hip adductor and abductor muscles to control the pelvic and trunk stability and balance in the elderly rather than the young [83,84]. In rehabilitation, water exercises prevent the risk of falls, unlike walking on land. So, DWR can be applied for coxarthropathy and lower-extremity rehabilitation after injury [59].
A study by Stevens et al. [63] mentioned that all of the included muscles reach a strength level at a 30% load except for the RA and IO, which may be trained in the flexion position rather than in the rotation. This intensity poses minimal tissue loads due to low resistance and a controlled neutral lumbar spine position [85]. The IO, EO, and LD are connected by the thoracolumbar fascia (TLF), and the MF and ICLT have hydraulic amplifier effects on layers of the TLF [86]. Due to these connections, the TLF maintains tension in these local and global trunk muscles [87]. Hence, a low-load-seated rotation can train the back muscles and EO during early rehabilitation after an injury [63].
The limitations include the following: (1) Only a few research studies were found with experimental designs to study therapeutic exercise effects on entire KCs. (2) There is a lack of focus on a single movement or family of movements to identify which muscles are involved in that specific kinetic chain and to what extent each one is involved in the movement. (3) There is a lack of movement-specific and particular body area analyses of the entire kinetic chain. (4) Due to inconsistent muscle activation data methods, a different group of involved muscles and varying kinds of exercises, such as a meta-analysis, were unable to be conducted.
Future work may include the following: (1) A good experimental design, particularly a randomized controlled trial for future research. (2) The same kind of studies should be conducted on older adults and people with diseases for an individualized exercise program. (3) Most of the research was focused on one or two muscle groups. So, in the future, studies should focus on the entire kinetic chain of different regions to examine the response during exercise regimens to recruit upper extremity, lower extremity, and trunk muscles. (4) About 60% of the included studies reported closed kinetic chain exercises, and only 14% of them reported open kinetic chain exercises. So, well-designed studies with mixed types of exercises that have better implications for athletes, healthy populations, and patients are required. (5) Overall, by increasing the load, muscle activation increases, but how it affects the entire kinetic chain is a missing area of research. (6) Most of these studies worked on UE and LE muscles like the SA, UT, ADelt, LT, PM, BF, RF, VL, GMax, and GT, but much less work was found on the LD, TB, BB, ES, GMed, TA, SOL, and peronei, etc., which should be considered in future research. (7) The search string should be tested with a simpler term to refer to kinetic or myofascial chains as “muscle chains” or “intermuscular coordination” in future research.
5. Conclusions
Kinetic chain exercises activate single or multiple groups of muscles. Based on the study findings, closed-chain exercises activate more groups of muscles in a kinetic chain than open-chain exercises. However, no closed or open-chain exercise can activate the optimal muscles of different regions simultaneously. However, a mixed approach using closed and open-chain exercises together can target more groups of muscles in an entire kinetic chain.
Author Contributions
Conceptualization, M.A., B.-S.L. and M.A.C.; methodology, M.A. and B.-S.L.; software, M.A.C. and C.-W.P.; validation, H.-C.C. and C.-W.P.; formal analysis, M.A. and B.-S.L.; investigation, C.-W.P.; resources, B.-S.L. and C.-W.P.; data curation, M.A. and M.A.C.; writing—original draft preparation, M.A., B.-S.L. and C.-W.P.; writing—review and editing, M.A., B.-S.L. and C.-W.P.; visualization, M.A.; supervision, B.-S.L., H.-C.C. and C.-W.P.; project administration, M.A. and H.-C.C.; funding acquisition, B.-S.L. and C.-W.P. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by grants from the National Science and Technology Council [112-2221-E-038-004-MY3, 112-2221-E-305-001-MY3, and 112-2811-E-038-002] and the Higher Education Sprout Project by the Ministry of Education [DP2-TMU-112-N-02] in Taiwan and by the TMU/CWRU (CTSC) Pilot Program [112-3805-003-400].
Institutional Review Board Statement
Not applicable.
Data Availability Statement
All data are presented in the manuscript.
Acknowledgments
We would like to acknowledge Usman Iqbal from the Global Health & Health Security Department, College of Public Health, Taipei Medical University, Taiwan, for his guidance and support in the completion of this review study. And Muhammad Salman Bashir School of Health Sciences, University of Management and Technology, Pakistan, for some investigation and project administration for this work.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
UE: upper extremity, LE; lower extremity, Tr; trunk, BB; biceps brachii, TB: triceps brachii: ADelt: anterior deltoid, MDelt; middle deltoid, PDelt; posterior deltoid, SS; supraspinatus, IF; infraspinatus, UT; upper trapezius, MT; middle trapezius, LT; lower trapezius, TMaj; teres major, SA; serratus anterior, LD; latissimus dorsi, USSS; upper subscapularis, PM; pectoralis major, GMax; gluteus maximus, GMed; gluteus medius, RF; rectus femoris, VL; vastus lateralis, VM; vastus medialis, AL; adductor longus, TFL; tensor fascia latae, BF; biceps femoris, SM; semimembranous, ST; semitendinous, TA; tibialis anterior, PL; peroneus longus, MGT; medial gastrocnemius, LGT; lateral gastrocnemius, SOL; soleus, RA; rectus abdominus, EO; external oblique, IO; internal oblique, TrA; transverses abdominus, ES; erector spinae, MF; multifidus, ICLT; iliocostalis lumborum pars thoracic, LTh; longissimus thoracic.
References
- Steindler, A. Kinesiology of the Human Body; Charles C Thomas: Springfield, IL, USA, 1955; pp. 646–651. [Google Scholar]
- Lefever, S. Closed kinetic chain training. In Therapeutic Exercise: Moving toward Function; Hall, C.M., Brody, L.T., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005. [Google Scholar]
- Reuleaux, F. Kinematics of Machinery: Outlines of a Theory of Machines; Nabu Press: Charleston, SC, USA, 2010. [Google Scholar]
- Voight, M.L.; Cook, G. Clinical application of closed kinetic chain exercise. J. Sport Rehabil. 1996, 5, 25–44. [Google Scholar] [CrossRef]
- Kibler, W.B.; Kuhn, J.E.; Wilk, K.; Sciascia, A.; Moore, S.; Laudner, K.; Ellenbecker, T.; Thigpen, C.; Uhl, T. The disabled throwing shoulder: Spectrum of pathology-10-year update. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 141–161.e126. [Google Scholar] [CrossRef]
- Sciascia, A.; Thigpen, C.; Namdari, S.; Baldwin, K. Kinetic chain abnormalities in the athletic shoulder. Sports Med. Arthrosc. Rev. 2012, 20, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Ellenbecker, T.S.; Aoki, R. Step by Step Guide to Understanding the Kinetic Chain Concept in the Overhead Athlete. Curr. Rev. Musculoskelet. Med. 2020, 13, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Dischiavi, S.L.; Wright, A.A.; Hegedus, E.J.; Bleakley, C.M. Biotensegrity and myofascial chains: A global approach to an integrated kinetic chain. Med. Hypotheses 2018, 110, 90–96. [Google Scholar] [CrossRef]
- Karandikar, N.; Vargas, O.O. Kinetic chains: A review of the concept and its clinical applications. Phys. Med. Rehabil. 2011, 3, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Frank, C.; Page, P.; Lardner, R. Assessment and Treatment of Muscle Imbalance: The Janda Approach; Human Kinetics: Champaign, IL, USA, 2009. [Google Scholar]
- Wilk, K.E.; Arrigo, C.A.; Hooks, T.R.; Andrews, J.R. Rehabilitation of the Overhead Throwing Athlete: There Is More to It Than Just External Rotation/Internal Rotation Strengthening. Phys. Med. Rehabil. 2016, 8, S78–S90. [Google Scholar] [CrossRef]
- Krause, F.; Wilke, J.; Vogt, L.; Banzer, W. Intermuscular force transmission along myofascial chains: A systematic review. J. Anat. 2016, 228, 910–918. [Google Scholar] [CrossRef]
- Myers, T.W. Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists; Elsevier Health Sciences: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Wilke, J.; Krause, F.; Vogt, L.; Banzer, W. What Is Evidence-Based About Myofascial Chains: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 454–461. [Google Scholar] [CrossRef]
- Yucesoy, C.A.; Koopman, B.H.; Baan, G.C.; Grootenboer, H.J.; Huijing, P.A. Effects of inter- and extramuscular myofascial force transmission on adjacent synergistic muscles: Assessment by experiments and finite-element modeling. J. Biomech. 2003, 36, 1797–1811. [Google Scholar] [CrossRef]
- Huijing, P.A.; Baan, G.C. Myofascial force transmission: Muscle relative position and length determine agonist and synergist muscle force. J. Appl. Physiol. 2003, 94, 1092–1107. [Google Scholar] [CrossRef]
- Kibler, W.B.; Sciascia, A.; Wilkes, T. Scapular dyskinesis and its relation to shoulder injury. J. Am. Acad. Orthop. Surg. 2012, 20, 364–372. [Google Scholar] [CrossRef]
- Kibler, W.B.; Uhl, T.L.; Maddux, J.W.; Brooks, P.V.; Zeller, B.; McMullen, J. Qualitative clinical evaluation of scapular dysfunction: A reliability study. J. Shoulder Elbow Surg. 2002, 11, 550–556. [Google Scholar] [CrossRef]
- Ličen, T.; Kalc, M.; Vogrin, M.; Bojnec, V. Injury Prevention in Tennis Players, Linking the Kinetic Chain Approach With Myofascial Lines: A Narrative Review With Practical Implications. Strength. Cond. J. 2022, 44, 104–114. [Google Scholar] [CrossRef]
- Weisman, M.H.S.; Haddad, M.; Lavi, N.; Vulfsons, S. Surface electromyographic recordings after passive and active motion along the posterior myofascial kinematic chain in healthy male subjects. J. Bodyw. Mov. Ther. 2014, 18, 452–461. [Google Scholar] [CrossRef] [PubMed]
- De Mey, K.; Danneels, L.; Cagnie, B.; Van den Bosch, L.; Flier, J.; Cools, A.M. Kinetic chain influences on upper and lower trapezius muscle activation during eight variations of a scapular retraction exercise in overhead athletes. J. Sci. Med. Sport. 2013, 16, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Oliver, G.D.; Plummer, H.A.; Gascon, S.S. Electromyographic Analysis of Traditional and Kinetic Chain Exercises for Dynamic Shoulder Movements. J. Strength. Cond. Res. 2016, 30, 3146–3154. [Google Scholar] [CrossRef]
- Chou, P.H.; Lou, S.Z.; Chen, S.K.; Chen, H.C.; Hsu, H.H.; Chou, Y.L. Comparative analysis of elbow joint loading in push-up and bench-press. Biomed. Eng. Appl. Basis Commun. 2011, 23, 21–28. [Google Scholar] [CrossRef]
- Brindle, T.J.; Nyland, J.; Ford, K.; Coppola, A.; Shapiro, R. Electromyographic comparison of standard and modified closed-chain isometric knee extension exercises. J. Strength. Cond. Res. 2002, 16, 129–134. [Google Scholar]
- Karabay, D.; Emük, Y.; Özer Kaya, D. Muscle Activity Ratios of Scapular Stabilizers During Closed Kinetic Chain Exercises in Healthy Shoulders: A Systematic Review. J. Sport. Rehabil. 2020, 29, 1001–1018. [Google Scholar] [CrossRef]
- McGill, S.; Andersen, J.; Cannon, J. Muscle activity and spine load during anterior chain whole body linkage exercises: The body saw, hanging leg raise and walkout from a push-up. J. Sports Sci. 2015, 33, 419–426. [Google Scholar] [CrossRef] [PubMed]
- McGill, S. Ultimate Back Fitness and Performance, 5th ed.; Backfitpro Incorporated: Ontario, Canada, 2014. [Google Scholar]
- Beach, T.A.; Howarth, S.J.; Callaghan, J.P. Muscular contribution to low-back loading and stiffness during standard and suspended push-ups. Hum. Mov. Sci. 2008, 27, 457–472. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef]
- Ruiz-González, L.; Lucena-Antón, D.; Salazar, A.; Martín-Valero, R.; Moral-Munoz, J. Physical therapy in Down syndrome: Systematic review and meta-analysis. J. Intellect. Disabil. Res. 2019, 63, 1041–1067. [Google Scholar] [CrossRef]
- Hébert-Losier, K.; Newsham-West, R.J.; Schneiders, A.G.; Sullivan, S.J. Raising the standards of the calf-raise test: A systematic review. J. Sci. Med. Sport 2009, 12, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Dinnes, J.; D’Amico, R.; Sowden, A.J.; Sakarovitch, C.; Song, F.; Petticrew, M.; Altman, D.G. Evaluating non-randomised intervention studies. Health Technol. Assess. 2003, 7, iii–173. [Google Scholar] [CrossRef]
- Jackson, N.; Waters, E. Criteria for the systematic review of health promotion and public health interventions. Health Promot. Int. 2005, 20, 367–374. [Google Scholar] [CrossRef]
- Thomas, B.H.; Ciliska, D.; Dobbins, M.; Micucci, S. A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 2004, 1, 176–184. [Google Scholar] [CrossRef]
- Smith, J.; Dahm, D.L.; Kaufman, K.R.; Boon, A.J.; Laskowski, E.R.; Kotajarvi, B.R.; Jacofsky, D.J. Electromyographic Activity in the Immobilized Shoulder Girdle Musculature During Ipsilateral Kinetic Chain Exercises. Arch. Phys. Med. Rehabil. 2007, 88, 1377–1383. [Google Scholar] [CrossRef]
- Dockery, M.L.; Wright, T.W.; LaStayo, P.C. Electromyography of the shoulder: An analysis of passive modes of exercise. Orthopedics 1998, 21, 1181–1184. [Google Scholar] [CrossRef] [PubMed]
- McCann, P.D.; Wootten, M.E.; Kadaba, M.P.; Bigliani, L.U. A kinematic and electromyographic study of shoulder rehabilitation exercises. Clin. Orthop. Relat. Res. 1993, 288, 179–188. [Google Scholar] [CrossRef]
- Townsend, H.; Jobe, F.W.; Pink, M.; Perry, J. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am. J. Sports Med. 1991, 19, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Jobe, F.W.; Moynes, D.R.; Tibone, J.E.; Perry, J. An EMG analysis of the shoulder in pitching. A second report. Am. J. Sports Med. 1984, 12, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Tsuruike, M.; Ellenbecker, T.S. Electromyographic Activity of Scapular Muscle Control in Free-Motion Exercise. J. Athl. Train. 2016, 51, 195–204. [Google Scholar] [CrossRef]
- Oliver, G.D.; Weimar, W.H.; Plummer, H.A. Gluteus medius and scapula muscle activations in youth baseball pitchers. J. Strength. Cond. Res. 2015, 29, 1494–1499. [Google Scholar] [CrossRef] [PubMed]
- Nanba, Y.; Miyamoto, S.; Takemasa, S.; Uesugi, M.; Inoue, Y.; Ootani, Y.; Fujii, S.; Hirotsu, T.; Tanaka, H. RETRACTED: Effect of exercise at light loads with manipulative resistance on infraspinatus, trapezius (upper fiber) and deltoid (middle fiber) muscle activities in shoulder joint elevation (Retracted article. See vol. 27, pg. R1, 2015). J. Phys. Ther. Sci. 2015, 27, 627–629. [Google Scholar] [CrossRef][Green Version]
- Herrington, L.; Waterman, R.; Smith, L. Electromyographic analysis of shoulder muscles during press-up variations and progressions. J. Electromyogr. Kinesiol. 2015, 25, 100–106. [Google Scholar] [CrossRef]
- Contreras, B.; Vigotsky, A.D.; Schoenfeld, B.J.; Beardsley, C.; Cronin, J. A Comparison of Gluteus Maximus, Biceps Femoris, and Vastus Lateralis Electromyographic Activity in the Back Squat and Barbell Hip Thrust Exercises. J. Appl. Biomech. 2015, 31, 452–458. [Google Scholar] [CrossRef]
- Cochrane, D.J.; Harnett, M.C. Muscle activation pattern and onset times during a semi-orthostatic, unilateral closed-kinetic hip extension exercise in adolescent males. Physiother. Theory Pract. 2015, 31, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Khademi Kalantari, K.; Berenji Ardestani, S. The effect of base of support stability on shoulder muscle activity during closed kinematic chain exercises. J. Bodyw. Mov. Ther. 2014, 18, 233–238. [Google Scholar] [CrossRef] [PubMed]
- De Mey, K.; Danneels, L.; Cagnie, B.; Borms, D.; T’Jonck, Z.; Van Damme, E.; Cools, A.M. Shoulder muscle activation levels during four closed kinetic chain exercises with and without redcord slings. J. Strength. Cond. Res. 2014, 28, 1626–1635. [Google Scholar] [CrossRef]
- Oliver, G.D.; Sola, M.; Dougherty, C.; Huddleston, S. Quantitative examination of upper and lower extremity muscle activation during common shoulder rehabilitation exercises using the bodyblade. J. Strength. Cond. Res. 2013, 27, 2509–2517. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, M.D.; Sundstrup, E.; Andersen, C.H.; Aagaard, P.; Andersen, L.L. Muscle activity during leg strengthening exercise using free weights and elastic resistance: Effects of ballistic vs controlled contractions. Hum. Mov. Sci. 2013, 32, 65–78. [Google Scholar] [CrossRef] [PubMed]
- Doma, K.; Deakin, G.B.; Ness, K.F. Kinematic and electromyographic comparisons between chin-ups and lat-pull down exercises. Sports Biomech. 2013, 12, 302–313. [Google Scholar] [CrossRef]
- Tucker, W.S.; Bruenger, A.J.; Doster, C.M.; Hoffmeyer, D.R. Scapular Muscle Activity in Overhead and Nonoverhead Athletes During Closed Chain Exercises. Clin. J. Sport Med. 2011, 21, 405–410. [Google Scholar] [CrossRef]
- Tucci, H.T.; Ciol, M.A.; De Araujo, R.C.; de Andrade, R.; Martins, J.; McQuade, K.J.; Oliveira, A.S. Activation of Selected Shoulder Muscles During Unilateral Wall and Bench Press Tasks Under Submaximal Isometric Effort. J. Orthop. Sports Phys. Ther. 2011, 41, 520–525. [Google Scholar] [CrossRef]
- Kim, S.J.; Kwon, O.Y.; Yi, C.H.; Jeon, H.S.; Oh, J.S.; Cynn, H.S.; Weon, J.H. Comparison of abdominal muscle activity during a single-legged hold in the hook-lying position on the floor and on a round foam roll. J. Athl. Train. 2011, 46, 403–408. [Google Scholar] [CrossRef]
- Uhl, T.L.; Muir, T.A.; Lawson, L. Electromyographical Assessment of Passive, Active Assistive, and Active Shoulder Rehabilitation Exercises. Phys. Med. Rehabil. 2010, 2, 132–141. [Google Scholar] [CrossRef]
- Schachter, A.K.; McHugh, M.P.; Tyler, T.F.; Kreminic, I.J.; Orishimo, K.F.; Johnson, C.; Ben-Avi, S.; Nicholas, S.J. Electromyographic activity of selected scapular stabilizers during glenohumeral internal and external rotation contractions. J. Shoulder Elb. Surg. 2010, 19, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Maenhout, A.; Van Praet, K.; Pizzi, L.; Van Herzeele, M.; Cools, A. Electromyographic analysis of knee push up plus variations: What is the influence of the kinetic chain on scapular muscle activity? Br. J. Sports Med. 2010, 44, 1010–1015. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, K.; Sato, D.; Wakabayashi, H.; Nomura, T. EMG activity of hip and trunk muscles during deep-water running. J. Electromyogr. Kinesiol. 2009, 19, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Ebben, W.P.; Feldmann, C.R.; Dayne, A.; Mitsche, D.; Alexander, P.; Knetzger, K.J. Muscle Activation during Lower Body Resistance Training. Int. J. Sports Med. 2009, 30, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tucker, W.S.; Campbell, B.M.; Swartz, E.E.; Armstrong, C.W. Electromyography of 3 scapular muscles: A comparative analysis of the Cuff Link device and a standard push-up. J. Athl. Train. 2008, 43, 464–469. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, A.S.; de Morais Carvalho, M.; de Brum, D.P.C. Activation of the shoulder and arm muscles during axial load exercises on a stable base of support and on a medicine ball. J. Electromyogr. Kinesiol. 2008, 18, 472–479. [Google Scholar] [CrossRef]
- Stevens, V.; Witvrouw, E.; Vanderstraeten, G.; Parlevliet, T.; Bouche, K.; Mahieu, N.; Danneels, L. The relevance of increasing resistance on trunk muscle activity during seated axial rotation. Phys. Ther. Sport 2007, 8, 7–13. [Google Scholar] [CrossRef]
- Azegami, M.; Yanagihash, R.; Miyoshi, K.; Akahane, K.; Ohira, M.; Sadoyama, T. Effects of multi-joint angle changes on EMG activity and force of lower extremity muscles during maximum isometric leg press exercises. J. Phys. Ther. Sci. 2007, 19, 65–72. [Google Scholar] [CrossRef]
- Smith, J.; Dahm, D.L.; Kaufman, K.R.; Boon, A.J.; Laskowski, E.R.; Kotajarvi, B.R.; Jacofsky, D.J. Electromyographic Activity in the Immobilized Shoulder Girdle Musculature During Scapulothoracic Exercises. Arch. Phys. Med. Rehabil. 2006, 87, 923–927. [Google Scholar] [CrossRef]
- Urabe, Y.; Kobayashi, R.; Sumida, S.; Tanaka, K.; Yoshida, N.; Nishiwaki, G.A.; Tsutsumi, E.; Ochi, M. Electromyographic analysis of the knee during jump landing in male and female athletes. Knee 2005, 12, 129–134. [Google Scholar] [CrossRef]
- Tucker, W.S.; Armstrong, C.W.; Swartz, E.E.; Campbell, B.M.; Rankin, J.M. An electromyographic analysis of the cuff link rehabilitation device. J. Sport Rehabil. 2005, 14, 124–136. [Google Scholar] [CrossRef]
- Wise, M.B.; Uhl, T.L.; Mattacola, C.G.; Nitz, A.J.; Kibler, W.B. The effect of limb support on muscle activation during shoulder exercises. J. Shoulder Elb. Surg. 2004, 13, 614–620. [Google Scholar] [CrossRef]
- Blackburn, J.T.; Hirth, C.J.; Guskiewicz, K.M. Exercise sandals increase lower extremity electromyographic activity during functional activities. J. Athl. Train. 2003, 38, 198–203. [Google Scholar]
- Blanpied, P.R. Changes in muscle activation during wall slides and squat-machine exercise. J. Sport Rehabil. 1999, 8, 123–134. [Google Scholar] [CrossRef]
- Isear, J.A.; Erickson, J.C.; Worrell, T.W. EMG analysis of lower extremity muscle recruitment patterns during an unloaded squat. Med. Sci. Sports Exerc. 1997, 29, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Wilk, K.E.; Escamilla, R.F.; Fleisig, G.S.; Barrentine, S.W.; Andrews, J.R.; Boyd, M.L. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am. J. Sports Med. 1996, 24, 518–527. [Google Scholar] [CrossRef]
- DeCarlo, M.; Porter, D.A.; Gehlsen, G.; Bahamonde, R. Electromyographic and cinematographic analysis of the lower extremity during closed and open kinetic chain exercise. Isokinet. Exerc. Sci. 1992, 2, 24–29. [Google Scholar] [CrossRef]
- Kibler, W.B.; Wilkes, T.; Sciascia, A. Mechanics and pathomechanics in the overhead athlete. Clin. Sports Med. 2013, 32, 637–651. [Google Scholar] [CrossRef]
- Antinori, F.; Felici, F.; Figura, F.; Marchetti, M.; Ricci, B. Joint moments and work in pull-ups. J. Sports Med. Phys. Fit. 1988, 28, 132–137. [Google Scholar]
- Marshall, P.W.; Murphy, B.A. Increased deltoid and abdominal muscle activity during Swiss ball bench press. J. Strength. Cond. Res. 2006, 20, 745–750. [Google Scholar] [CrossRef][Green Version]
- Lehman, G.J.; MacMillan, B.; MacIntyre, I.; Chivers, M.; Fluter, M. Shoulder muscle EMG activity during push up variations on and off a Swiss ball. Dyn. Med. 2006, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Lehman, G.J.; Gilas, D.; Patel, U. An unstable support surface does not increase scapulothoracic stabilizing muscle activity during push up and push up plus exercises. Man. Ther. 2008, 13, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Gardner-Morse, M.; Stokes, I.A.; Laible, J.P. Role of muscles in lumbar spine stability in maximum extension efforts. J. Orthop. Res. 1995, 13, 802–808. [Google Scholar] [CrossRef]
- Arokoski, J.P.; Valta, T.; Airaksinen, O.; Kankaanpää, M. Back and abdominal muscle function during stabilization exercises. Arch. Phys. Med. Rehabil. 2001, 82, 1089–1098. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.G.; Behm, D.G. Maintenance of EMG activity and loss of force output with instability. J. Strength. Cond. Res. 2004, 18, 637–640. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, K.; Wakabayashi, H.; Sato, D.; Uekusa, T.; Nomura, T. Lower extremity muscle activity during deep-water running on self-determined pace. J. Electromyogr. Kinesiol. 2008, 18, 965–972. [Google Scholar] [CrossRef]
- Panzer, V.P.; Bandinelli, S.; Hallett, M. Biomechanical assessment of quiet standing and changes associated with aging. Arch. Phys. Med. Rehabil. 1995, 76, 151–157. [Google Scholar] [CrossRef]
- Amiridis, I.G.; Hatzitaki, V.; Arabatzi, F. Age-induced modifications of static postural control in humans. Neurosci. Lett. 2003, 350, 137–140. [Google Scholar] [CrossRef]
- McGill, S.M. Lumbar Spine Stability: Mechanism of Injury and Restabilization; Lippincott, Williams & Wilkins: Philadelphia, PA, USA, 2007. [Google Scholar]
- Vleeming, A.; Pool-Goudzwaard, A.L.; Stoeckart, R.; van Wingerden, J.P.; Snijders, C.J. The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs. Spine 1995, 20, 753–758. [Google Scholar] [CrossRef]
- Barker, P.J.; Briggs, C.A. Attachments of the posterior layer of lumbar fascia. Spine 1999, 24, 1757–1764. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).