Mediating Effects of the COVID-19 Pandemic on the Associations between Physical Activity and Physical Fitness; Cross-Sectional Study among High School Adolescents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Variables and Measurements
2.3. Statistical Analysis
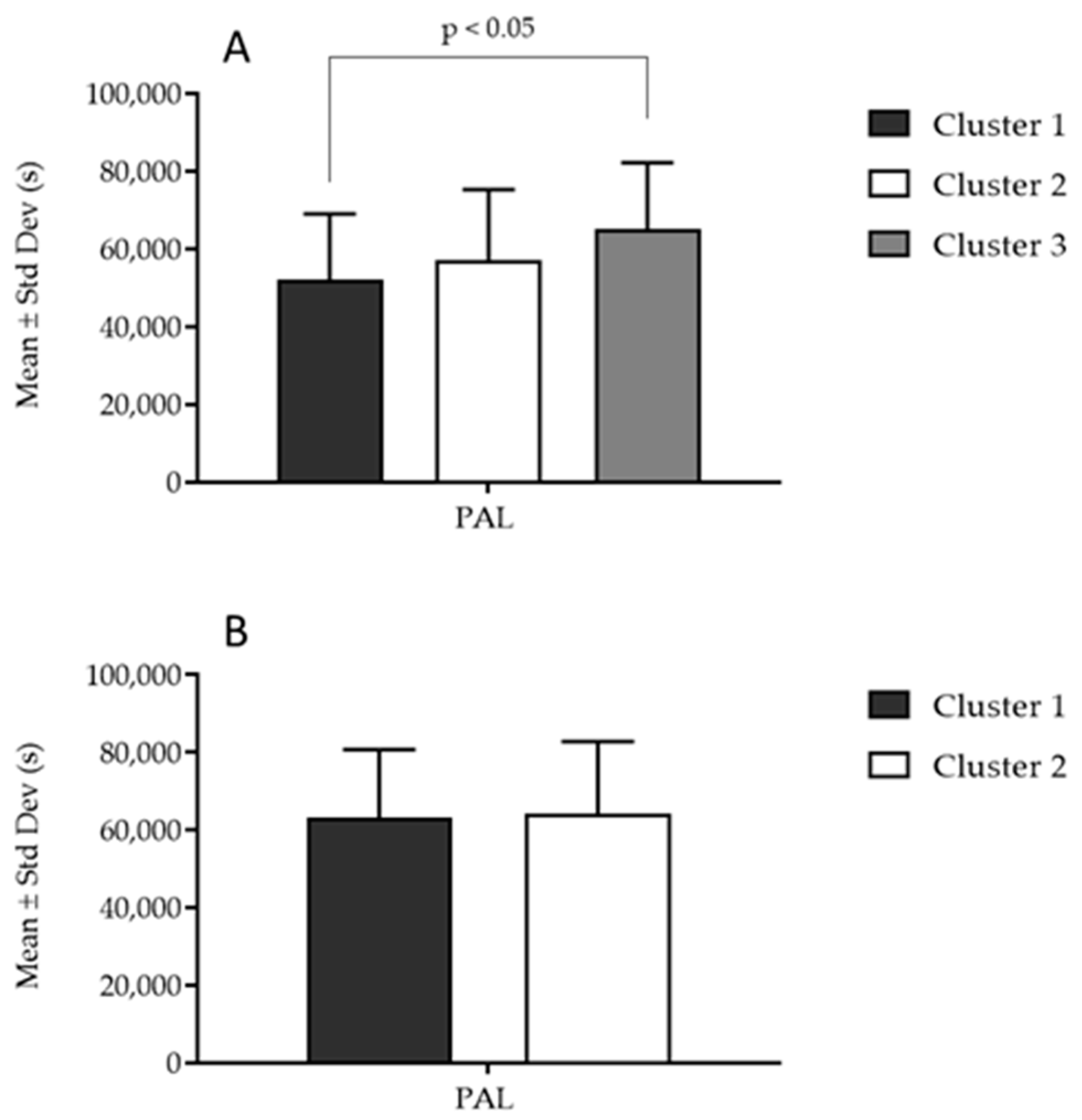
3. Results
4. Discussion
4.1. Physical Activity and Physical Fitness
4.2. Possible Mediating Effects of the COVID-19 Pandemic on the Association between Physical Activity Levels and Physical Fitness
4.3. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Muralidar, S.; Ambi, S.V.; Sekaran, S.; Krishnan, U.M. The emergence of COVID-19 as a global pandemic: Understanding the epidemiology, immune response and potential therapeutic targets of SARS-CoV-2. Biochimie 2020, 179, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G. Effects of COVID-19 syndemic on sport community. J. Funct. Morphol. Kinesiol. 2022, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Rossi, L.; Behme, N.; Breuer, C. Physical Activity of Children and Adolescents during the COVID-19 Pandemic-A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11440. [Google Scholar] [CrossRef] [PubMed]
- Geets Kesic, M.; Gilic, B.; Cerkez Zovko, I.; Drid, P.; Korovljev, D.; Sekulic, D. Differential impact of COVID-19 lockdown on physical activity in younger and older adolescents—Prospective study. Med. Pr. 2021, 72, 633–643. [Google Scholar] [CrossRef]
- Sekulic, D.; Blazevic, M.; Gilic, B.; Kvesic, I.; Zenic, N. Prospective Analysis of Levels and Correlates of Physical Activity during COVID-19 Pandemic and Imposed Rules of Social Distancing; Gender Specific Study among Adolescents from Southern Croatia. Sustainability 2020, 12, 4072. [Google Scholar] [CrossRef]
- Zenic, N.; Taiar, R.; Gilic, B.; Blazevic, M.; Maric, D.; Pojskic, H.; Sekulic, D. Levels and changes of physical activity in adolescents during the COVID-19 pandemic: Contextualizing urban vs. rural living environment. Appl. Sci. 2020, 10, 3997. [Google Scholar] [CrossRef]
- Gilic, B.; Ostojic, L.; Corluka, M.; Volaric, T.; Sekulic, D. Contextualizing Parental/Familial Influence on Physical Activity in Adolescents before and during COVID-19 Pandemic: A Prospective Analysis. Children 2020, 7, 125. [Google Scholar] [CrossRef]
- Sunda, M.; Gilic, B.; Peric, I.; Jurcev Savicevic, A.; Sekulic, D. Evidencing the Influence of the COVID-19 Pandemic and Imposed Lockdown Measures on Fitness Status in Adolescents: A Preliminary Report. Healthcare 2021, 9, 681. [Google Scholar] [CrossRef]
- Hallal, P.C.; Victora, C.G.; Azevedo, M.R.; Wells, J.C. Adolescent physical activity and health: A systematic review. Sports Med. 2006, 36, 1019–1030. [Google Scholar] [CrossRef]
- Young, J.; Bonnet, J.P.; Sokolof, J. Lifestyle Medicine: Physical Activity. J. Fam. Pract. 2022, 71, S17–S23. [Google Scholar] [CrossRef]
- Craggs, C.; Corder, K.; van Sluijs, E.M.; Griffin, S.J. Determinants of change in physical activity in children and adolescents: A systematic review. Am. J. Prev. Med. 2011, 40, 645–658. [Google Scholar] [CrossRef]
- Back, J.; Johnson, U.; Svedberg, P.; McCall, A.; Ivarsson, A. Drop-out from team sport among adolescents: A systematic review and meta-analysis of prospective studies. Psychol. Sport Exerc. 2022, 61, 102205. [Google Scholar] [CrossRef]
- Corder, K.; Sharp, S.J.; Atkin, A.J.; Griffin, S.J.; Jones, A.P.; Ekelund, U.; van Sluijs, E.M. Change in objectively measured physical activity during the transition to adolescence. Br. J. Sports Med. 2015, 49, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Breau, B.; Brandes, M.; Veidebaum, T.; Tornaritis, M.; Moreno, L.A.; Molnár, D.; Lissner, L.; Eiben, G.; Lauria, F.; Kaprio, J.; et al. Longitudinal association of childhood physical activity and physical fitness with physical activity in adolescence: Insights from the IDEFICS/I.Family study. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 147. [Google Scholar] [CrossRef] [PubMed]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Pedišić, Ž.; Strika, M.; Matolić, T.; Sorić, M.; Šalaj, S.; Dujić, I.; Rakovac, M.; Radičević, B.; Podnar, H.; Greblo Jurakić, Z.; et al. Physical Activity of Children and Adolescents in Croatia: A Global Matrix 4.0 Systematic Review of Its Prevalence and Associated Personal, Social, Environmental, and Policy Factors. J. Phys. Act. Health 2023, 20, 487–499. [Google Scholar] [CrossRef]
- Brás, R.; Esteves, D.; Rodrigues, R.G.; Duarte, P.; Gouveia, A.; O’Hara, K.; Pinheiro, P. Evaluation of risks and benefits of physical activity of hypertensives and normotensives: Fighting a societal burden. Montenegrin J. Sports Sci. Med. 2020, 9, 11. [Google Scholar] [CrossRef]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef]
- Rizzo, N.S.; Ruiz, J.R.; Hurtig-Wennlöf, A.; Ortega, F.B.; Sjöström, M. Relationship of Physical Activity, Fitness, and Fatness with Clustered Metabolic Risk in Children and Adolescents: The European Youth Heart Study. J. Pediatr. 2007, 150, 388–394. [Google Scholar] [CrossRef]
- Kumar, B.; Robinson, R.; Till, S. Physical activity and health in adolescence. Clin. Med. 2015, 15, 267. [Google Scholar] [CrossRef]
- Ornelas, R.T.; Silva, A.M.; Minderico, C.S.; Sardinha, L.B. Changes in cardiorespiratory fitness predict changes in body composition from childhood to adolescence: Findings from the European Youth Heart Study. Physician Sportsmed. 2011, 39, 78–86. [Google Scholar] [CrossRef]
- Béghin, L.; Thivel, D.; Baudelet, J.B.; Deschamps, T.; Ovigneur, H.; Vanhelst, J. Change in physical fitness due to the COVID-19 pandemic lockdown in French adolescents: A comparison between two independent large samples from Diagnoform battery. Eur. J. Pediatr. 2022, 181, 3955–3963. [Google Scholar] [CrossRef] [PubMed]
- Rúa-Alonso, M.; Rial-Vázquez, J.; Nine, I.; Lete-Lasa, J.R.; Clavel, I.; Giráldez-García, M.A.; Rodríguez-Corral, M.; Dopico-Calvo, X.; Iglesias-Soler, E. Comparison of Physical Fitness Profiles Obtained before and during COVID-19 Pandemic in Two Independent Large Samples of Children and Adolescents: DAFIS Project. Int. J. Environ. Res. Public Health 2022, 19, 3963. [Google Scholar] [CrossRef] [PubMed]
- Ascenso, A.; Palmeira, A.; Pedro, L.M.; Martins, S.; Fonseca, H. Physical activity and cardiorespiratory fitness, but not sedentary behavior, are associated with carotid intima-media thickness in obese adolescents. Eur. J. Pediatr. 2016, 175, 391–398. [Google Scholar] [CrossRef]
- Lohman, T.G.; Ring, K.; Pfeiffer, K.; Camhi, S.; Arredondo, E.; Pratt, C.; Pate, R.; Webber, L.S. Relationships among fitness, body composition, and physical activity. Med. Sci. Sports Exerc. 2008, 40, 1163–1170. [Google Scholar] [CrossRef] [PubMed]
- Hui, S.S.; Zhang, R.; Suzuki, K.; Naito, H.; Balasekaran, G.; Song, J.K.; Park, S.Y.; Liou, Y.M.; Lu, D.; Poh, B.K.; et al. Physical activity and health-related fitness in Asian adolescents: The Asia-fit study. J. Sports Sci. 2020, 38, 273–279. [Google Scholar] [CrossRef]
- Neil-Sztramko, S.E.; Caldwell, H.; Dobbins, M. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2021, 9, CD007651. [Google Scholar] [CrossRef]
- Chung, A.E.; Skinner, A.C.; Steiner, M.J.; Perrin, E.M. Physical activity and BMI in a nationally representative sample of children and adolescents. Clin. Pediatr. 2012, 51, 122–129. [Google Scholar] [CrossRef]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martinez-Vizcaino, V.; García-Hermoso, A.; Torres-Costoso, A.I.; Sánchez-López, M. Association between physical activity, sedentary behavior, and fitness with health related quality of life in healthy children and adolescents: A protocol for a systematic review and meta-analysis. Medicine 2017, 96, e6407. [Google Scholar] [CrossRef]
- Trost, S.G.; Pate, R.R.; Sallis, J.F.; Freedson, P.S.; Taylor, W.C.; Dowda, M.; Sirard, J. Age and gender differences in objectively measured physical activity in youth. Med. Sci. Sports Exerc. 2002, 34, 350–355. [Google Scholar] [CrossRef]
- Mraković, M.; Findak, V.; Metikoš, D.; Neljak, B. Developmental characteristics of motor and functional abilities in primary and secondary school pupils. Kinesiology 1996, 28, 57–65. [Google Scholar]
- McClain, J.J.; Welk, G.J.; Ihmels, M.; Schaben, J. Comparison of Two Versions of the PACER Aerobic Fitness Test. J. Phys. Act. Health 2006, 3, S47–S57. [Google Scholar] [CrossRef]
- Thomas, E.; Petrigna, L.; Tabacchi, G.; Teixeira, E.; Pajaujiene, S.; Sturm, D.J.; Sahin, F.N.; Gómez-López, M.; Pausic, J.; Paoli, A.; et al. Percentile values of the standing broad jump in children and adolescents aged 6-18 years old. Eur. J. Transl. Myol. 2020, 30, 9050. [Google Scholar] [CrossRef]
- Miyamoto, N.; Hirata, K.; Kimura, N.; Miyamoto-Mikami, E. Contributions of Hamstring Stiffness to Straight-Leg-Raise and Sit-and-Reach Test Scores. Int. J. Sports Med. 2018, 39, 110–114. [Google Scholar] [CrossRef]
- Chandana, A.; Xubo, W. The test battery: Evaluate muscular strength and endurance of the abdominals and hip-flexor muscles. In Proceedings of the General Sir John Kotelawala Defence University—14th International Research Conference, 9 September 2021; Volume 14, p. 23. [Google Scholar]
- Coffman, M.J.; Reeve, C.L.; Butler, S.; Keeling, M.; Talbot, L.A. Accuracy of the Yamax CW-701 Pedometer for measuring steps in controlled and free-living conditions. Digit. Health 2016, 2, 2055207616652526. [Google Scholar] [CrossRef]
- Dalmaijer, E.S.; Nord, C.L.; Astle, D.E. Statistical power for cluster analysis. BMC Bioinform. 2022, 23, 205. [Google Scholar] [CrossRef] [PubMed]
- Kesic, M.G.; Savicevic, A.J.; Peric, M.; Gilic, B.; Zenic, N. Specificity of the Associations between Indices of Cardiovascular Health with Health Literacy and Physical Literacy; A Cross-Sectional Study in Older Adolescents. Medicina 2022, 58, 1316. [Google Scholar] [CrossRef]
- Geets-Kesić, M.; Maras, N.; Gilić, B. Analysis of the Association Between Health Literacy, Physical Literacy, and Scholastic Achievement; A Preliminary Cross-Sectional Study Among High-School Students From Southern Croatia. Montenegrin J. Sports Sci. Med. 2023, 12, 3–9. [Google Scholar] [CrossRef]
- Júdice, P.B.; Silva, A.M.; Berria, J.; Petroski, E.L.; Ekelund, U.; Sardinha, L.B. Sedentary patterns, physical activity and health-related physical fitness in youth: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 25. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Eston, R.G. Comparison of Accelerometer and Pedometer Measures of Physical Activity in Boys and Girls, Ages 8–10 Years. Res. Q. Exerc. Sport 2005, 76, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, G.A.; Nordenfelt, A.M.; Ekelund, U.; Marcus, C. Physical activity patterns measured by accelerometry in 6- to 10-yr-old children. Med. Sci. Sports Exerc. 2009, 41, 1842–1848. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A.M.; Jebb, S.A. Beyond body mass index. Obes. Rev. 2001, 2, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Lakoski, S.G.; Barlow, C.E.; Farrell, S.W.; Berry, J.D.; Morrow, J.R., Jr.; Haskell, W.L. Impact of body mass index, physical activity, and other clinical factors on cardiorespiratory fitness (from the Cooper Center longitudinal study). Am. J. Cardiol. 2011, 108, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Gutin, B.; Yin, Z.; Humphries, M.C.; Barbeau, P. Relations of moderate and vigorous physical activity to fitness and fatness in adolescents. Am. J. Clin. Nutr. 2005, 81, 746–750. [Google Scholar] [CrossRef]
- Garrido-Chamorro, R.; Sirvent-Belando, J.; Gonzalez-Lorenzo, M.; Martin-Carratala, M.; Roche, E. Correlation between body mass index and body composition in elite athletes. J. Sports Med. Phys. Fit. 2009, 49, 278. [Google Scholar]
- Mielgo Ayuso, J.; Maroto Sanchez, B.; Luzardo Socorro, R.; Palacios Le Blé, G.; Palacios Gil Antuñano, N.; Gonzalez Gross, M.M. Evaluation of nutritional status and energy expenditure in athletes. Nutr. Hosp. 2015, 31, 227–236. [Google Scholar]
- Drenjak, J.L.; Pehar, M.; Užičanin, E.; Kontić, D.; Zenić, N. Physical activity, sport participation, and cigarette smoking in university students after COVID-19 pandemic; Cross sectional analysis of the associations in south-eastern Europe. Montenegrin J. Sports Sci. Med. 2023, 12, 61–68. [Google Scholar] [CrossRef]
- Gilic, B.; Zenic, N.; Separovic, V.; Jurcev Savicevic, A.; Sekulic, D. Evidencing the influence of pre-pandemic sports participation and substance misuse on physical activity during the COVID-19 lockdown: A prospective analysis among older adolescents. Int. J. Occup. Med. Environ. Health 2021, 34, 151–163. [Google Scholar] [CrossRef]
- Cudeck, R. Analysis of correlation matrices using covariance structure models. Psychol. Bull. 1989, 105, 317. [Google Scholar] [CrossRef]
- Karuc, J.; Sorić, M.; Radman, I.; Mišigoj-Duraković, M. Moderators of Change in Physical Activity Levels during Restrictions Due to COVID-19 Pandemic in Young Urban Adults. Sustainability 2020, 12, 6392. [Google Scholar] [CrossRef]
- Harangi-Rákos, M.; Pfau, C.; Bácsné Bába, É.; Bács, B.A.; Kőmíves, P.M. Lockdowns and physical activities: Sports in the time of COVID. Int. J. Environ. Res. Public Health 2022, 19, 2175. [Google Scholar] [CrossRef] [PubMed]
- Trott, M.; Driscoll, R.; Irlado, E.; Pardhan, S. Changes and correlates of screen time in adults and children during the COVID-19 pandemic: A systematic review and meta-analysis. EClinicalMedicine 2022, 48, 101452. [Google Scholar] [CrossRef] [PubMed]

| Boys (N = 49) | Girls (N = 101) | T-Test | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t-Value | p-Value | |
| Body height (cm) | 180.84 | 7.64 | 168.24 | 6.67 | 10.37 | 0.001 |
| Body mass (kg) | 74.44 | 13.11 | 59.35 | 10.04 | 7.38 | 0.001 |
| Body mass index | 22.70 | 3.49 | 20.92 | 2.94 | 3.72 | 0.01 |
| Broad jump (cm) | 215.51 | 30.22 | 166.58 | 24.23 | 10.66 | 0.001 |
| Sit-and-reach (cm) | 6.90 | 9.59 | 13.31 | 6.98 | 4.65 | 0.001 |
| Sit-ups (number) | 65.98 | 10.98 | 52.20 | 11.64 | 6.92 | 0.001 |
| Beep test (level) | 11.77 | 2.74 | 9.62 | 9.50 | 6.91 | 0.001 |
| Step count | 61,828.63 | 24,196.94 | 59,804.20 | 19,384.67 | 0.55 | 0.58 |
| Body Height | Body Mass | Body Mass Index | Broad Jump | Sit-and-Reach | Sit-Ups | Beep Test | ||
|---|---|---|---|---|---|---|---|---|
| Body mass | Total sample | 0.68 * | ||||||
| Girls | 0.53 * | |||||||
| Boys | 0.51 * | |||||||
| Body mass index | Total sample | 0.23 * | 0.87 * | |||||
| Girls | 0.09 | 0.89 * | ||||||
| Boys | 0.09 | 0.90 * | ||||||
| Broad jump | Total sample | 0.49 * | 0.20 * | −0.07 | ||||
| Girls | 0.02 | −0.25 * | −0.29 * | |||||
| Boys | 0.23 | −0.23 | −0.38 * | |||||
| Sit-and-reach | Total sample | −0.28 * | −0.16 * | −0.02 | −0.05 | |||
| Girls | −0.08 | 0.11 | 0.18 | 0.22 * | ||||
| Boys | −0.06 | −0.05 | −0.03 | 0.30 * | ||||
| Sit-ups | Total sample | 0.39 * | 0.25 * | 0.07 | 0.61 * | 0.06 | ||
| Girls | 0.12 | −0.01 | −0.08 | 0.40 * | 0.25 * | |||
| Boys | 0.07 | −0.03 | −0.05 | 0.49 * | 0.39 * | |||
| Beep test | Total sample | 0.35 * | 0.07 | −0.15 | 0.67 * | −0.08 | 0.49 * | |
| Girls | 0.02 | −0.23 * | −0.28 * | 0.49 * | 0.13 | 0.36 * | ||
| Boys | 0.08 | −0.32 * | −0.40 * | 0.59 * | 0.10 | 0.27 | ||
| PAL | Total sample | 0.01 | 0.00 | −0.01 | 0.02 | 0.06 | 0.07 | 0.25 * |
| Girls | 0.03 | −0.01 | −0.03 | 0.07 | 0.06 | 0.06 | 0.29 * | |
| Boys | −0.10 | −0.05 | −0.01 | 0.13 | 0.11 | 0.05 | 0.23 |
| Root 1 | Root 2 | |
|---|---|---|
| Beep test | 0.56 | 0.03 |
| Broad jump | 0.11 | −0.02 |
| Sit-ups | 0.51 | −0.09 |
| Sit-and-reach | −0.04 | 0.41 |
| Canonical R | 0.41 | 0.32 |
| Wilks’ lambda | 0.65 | 0.74 |
| p-value | 0.01 | 0.03 |
| Centroid: Cluster 1 | −0.54 | 0.55 |
| Centroid: Cluster 2 | −0.11 | −0.32 |
| Centroid: Cluster 3 | 0.87 | 0.05 |
| Root 1 | |
|---|---|
| Beep test | 0.41 |
| Broad jump | 0.32 |
| Sit-ups | 0.38 |
| Sit-and-reach | −0.09 |
| Canonical R | 0.37 |
| Wilks’ lambda | 0.79 |
| p-value | 0.01 |
| Centroid: Cluster 1 | 0.47 |
| Centroid: Cluster 2 | −0.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sunda, M.; Gilic, B.; Vuletic, P.R.; Pavlinovic, V.; Zenic, N. Mediating Effects of the COVID-19 Pandemic on the Associations between Physical Activity and Physical Fitness; Cross-Sectional Study among High School Adolescents. J. Funct. Morphol. Kinesiol. 2023, 8, 131. https://doi.org/10.3390/jfmk8030131
Sunda M, Gilic B, Vuletic PR, Pavlinovic V, Zenic N. Mediating Effects of the COVID-19 Pandemic on the Associations between Physical Activity and Physical Fitness; Cross-Sectional Study among High School Adolescents. Journal of Functional Morphology and Kinesiology. 2023; 8(3):131. https://doi.org/10.3390/jfmk8030131
Chicago/Turabian StyleSunda, Mirela, Barbara Gilic, Petra Rajkovic Vuletic, Vladimir Pavlinovic, and Natasa Zenic. 2023. "Mediating Effects of the COVID-19 Pandemic on the Associations between Physical Activity and Physical Fitness; Cross-Sectional Study among High School Adolescents" Journal of Functional Morphology and Kinesiology 8, no. 3: 131. https://doi.org/10.3390/jfmk8030131
APA StyleSunda, M., Gilic, B., Vuletic, P. R., Pavlinovic, V., & Zenic, N. (2023). Mediating Effects of the COVID-19 Pandemic on the Associations between Physical Activity and Physical Fitness; Cross-Sectional Study among High School Adolescents. Journal of Functional Morphology and Kinesiology, 8(3), 131. https://doi.org/10.3390/jfmk8030131







