Effect of Joint Mobilization in Individuals with Chronic Ankle Instability: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy and Selection of Studies
2.2.1. Inclusion Criteria
- Participants
- 2.
- Intervention
- 3.
- Comparisons
- 4.
- Outcomes
- 5.
- Types of studies
2.2.2. Exclusion Criteria
2.2.3. Literature Search Strategy
2.2.4. Study Selection and Data Extraction
2.2.5. Quality Assessment
2.3. Strategy for Data Synthesis
3. Results
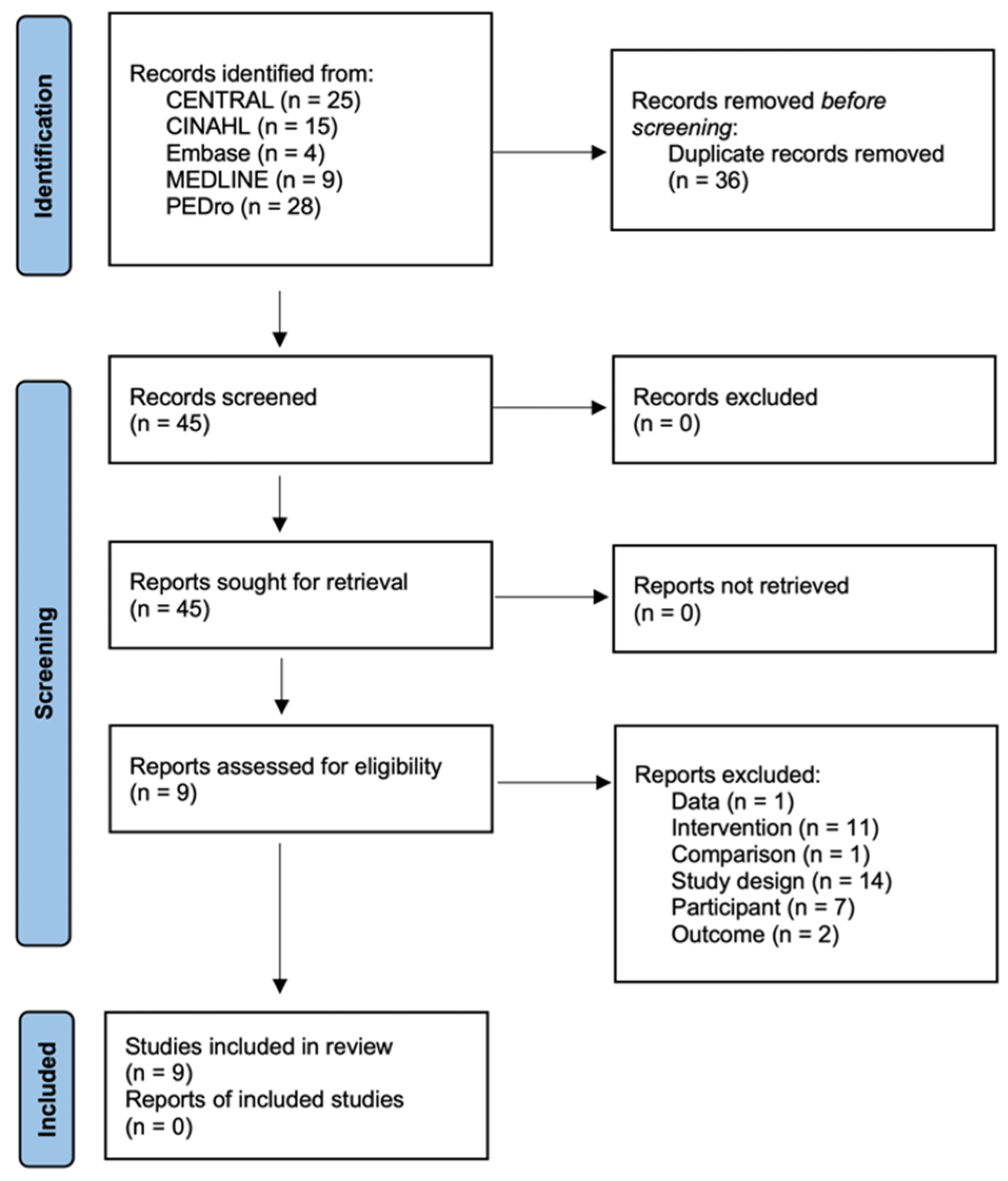
3.1. Literature Search and Characteristics of the Included Randomized Clinical Trials
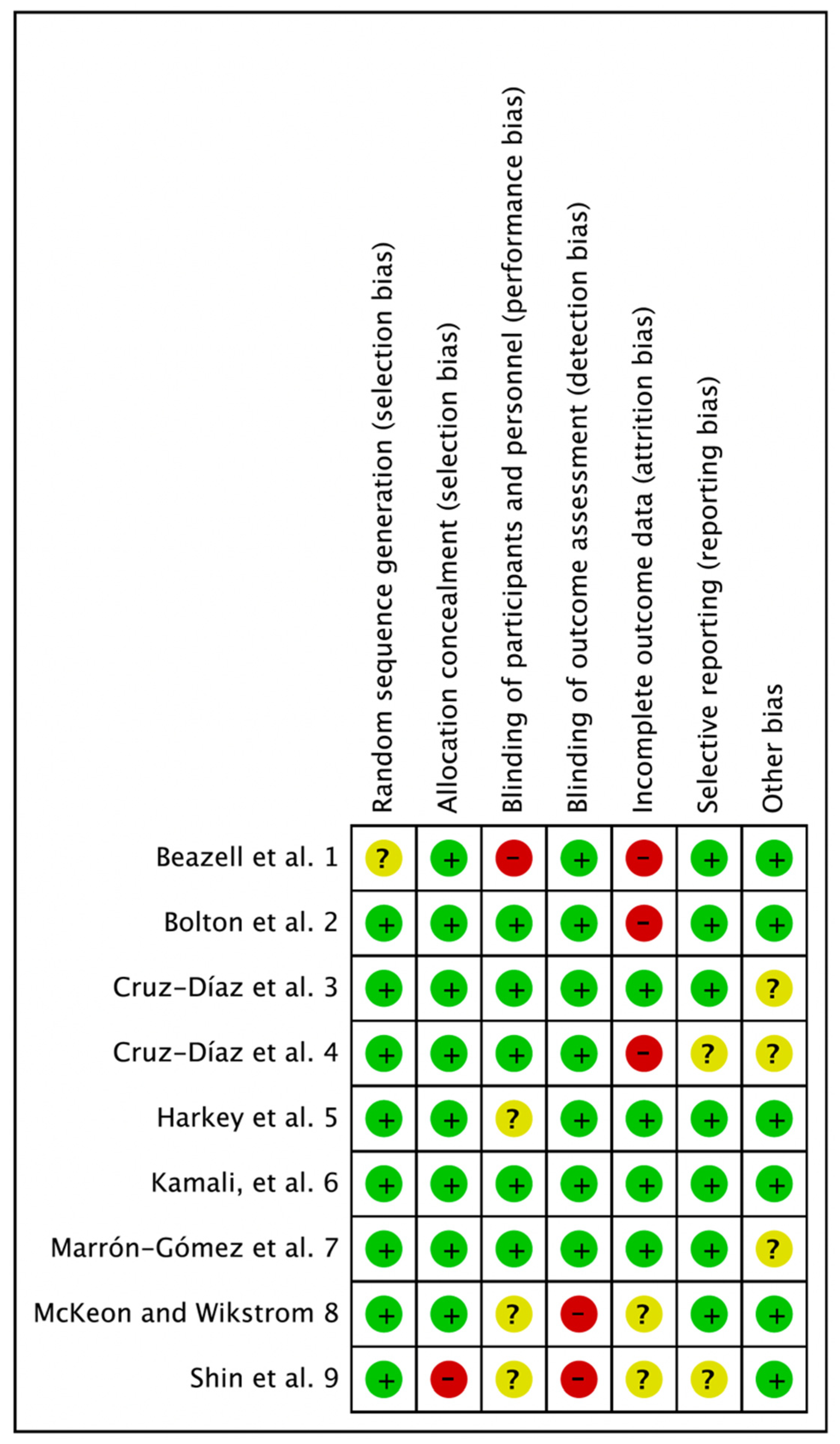
3.2. Methodological Quality Assessment
3.3. Joint Mobilization for Individuals with Chronic Ankle Instability
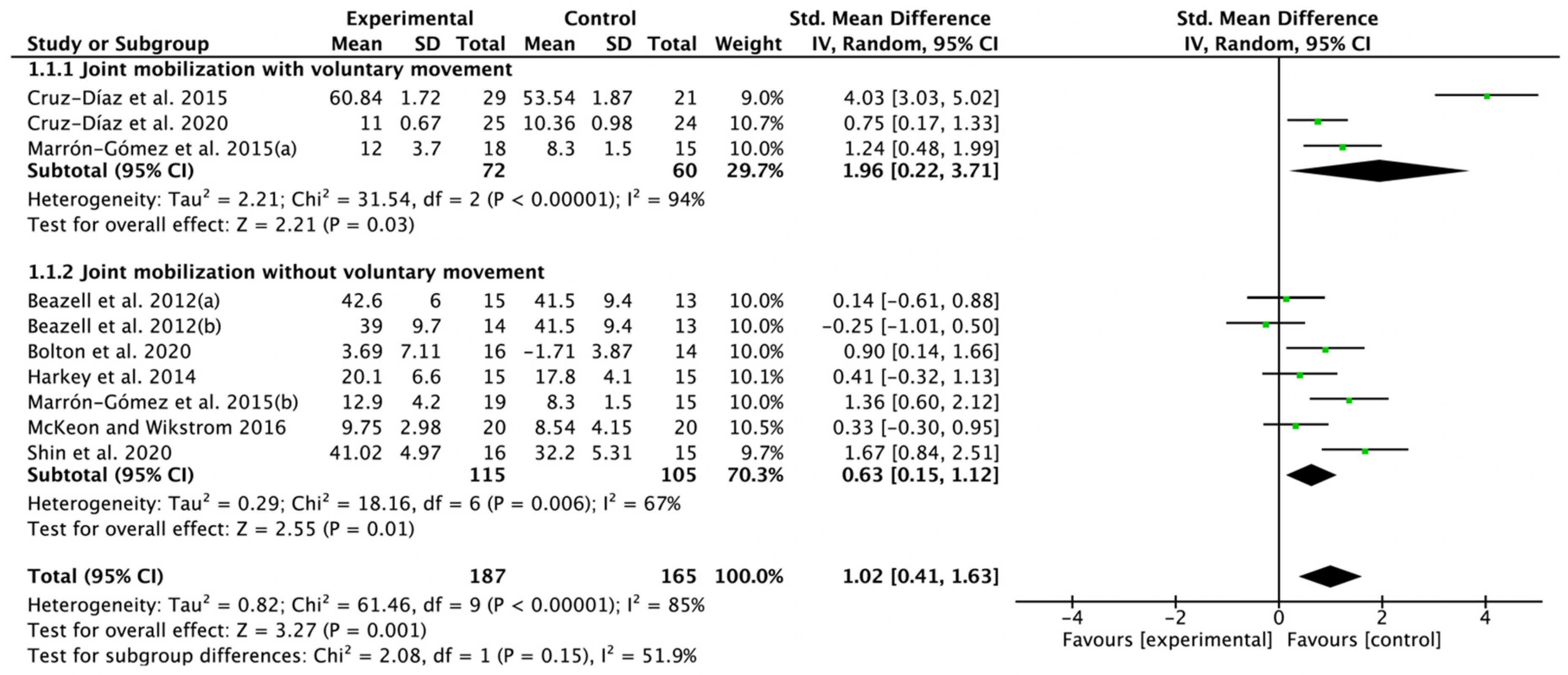
3.4. Effectiveness of Joint Mobilization on Ankle Dorsiflexion Range of Motion
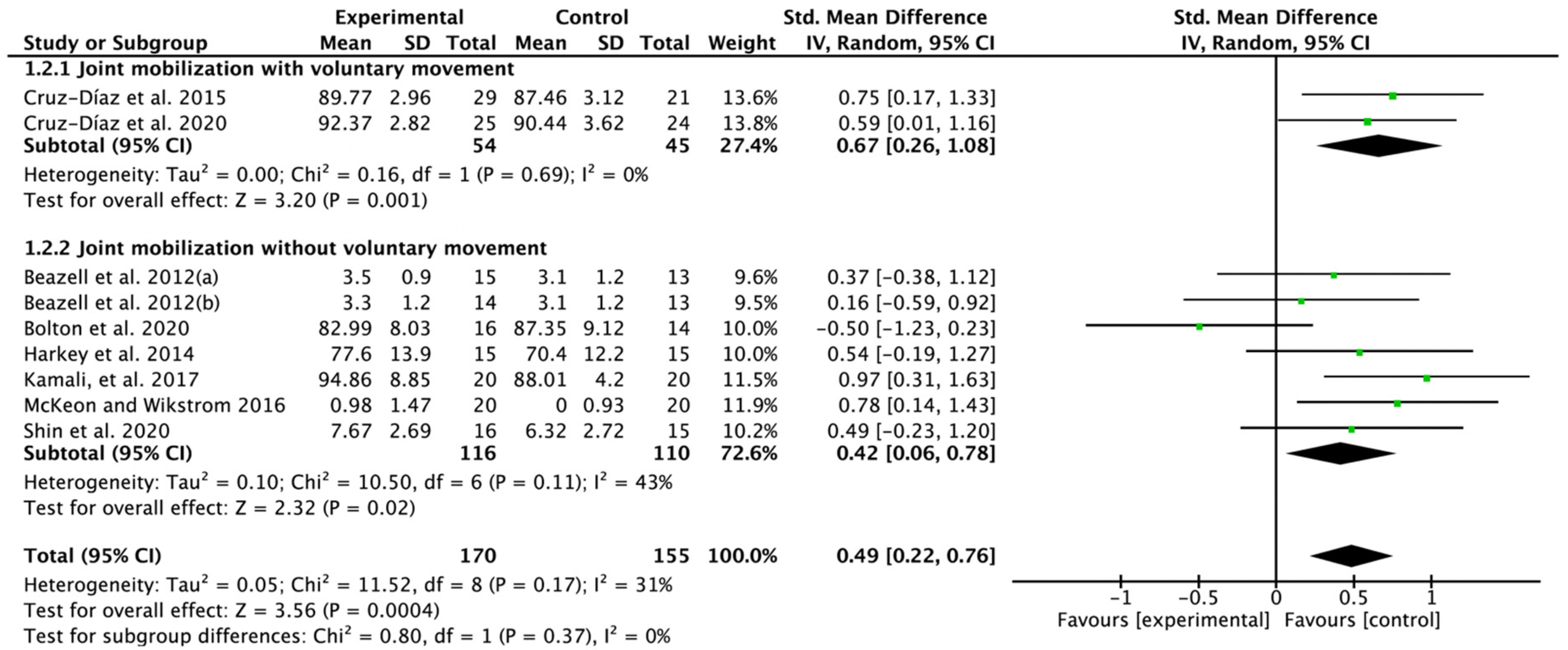
3.5. Effectiveness of Joint Mobilization on Dynamic Balance
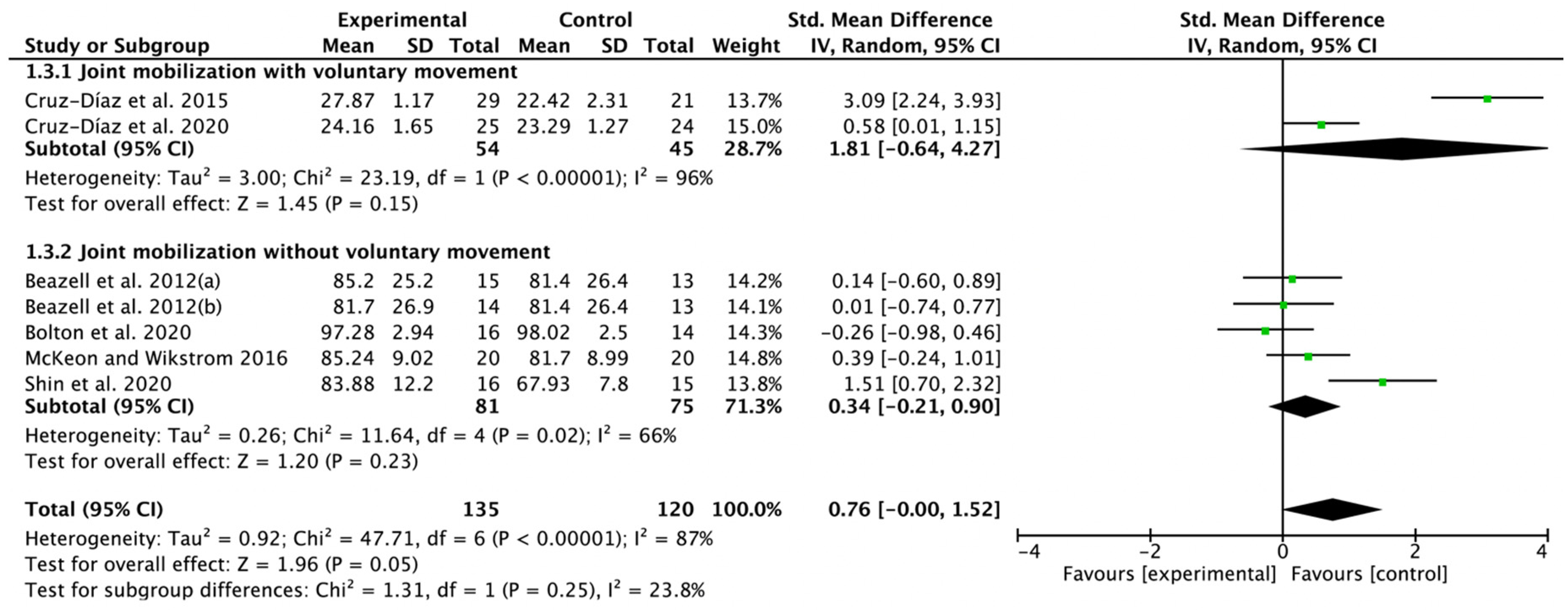
3.6. Effectiveness of Joint Mobilization on Function
3.7. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014, 44, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Roos, K.G.; Kerr, Z.Y.; Mauntel, T.C.; Djoko, A.; Dompier, T.P.; Wikstrom, E.A. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am. J. Sports Med. 2017, 45, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Al-Mohrej, O.A.; Al-Kenani, N.S. Chronic ankle instability: Current perspectives. Avicenna J. Med. 2016, 6, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar]
- Martin, R.L.; Davenport, T.E.; Fraser, J.J.; Sawdon-Bea, J.; Carcia, C.R.; Carroll, L.A.; Kivlan, B.R.; Carreira, D. Ankle Stability and Movement Coordination Impairments: Lateral Ankle Ligament Sprains Revision 2021: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health From the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2021, 51, CPG1–CPG80. [Google Scholar] [PubMed]
- Rosen, A.B.; Needle, A.R.; Ko, J. Ability of functional performance tests to identify individuals with chronic ankle instability: A systematic review with meta-analysis. Clin. J. Sport Med. 2019, 29, 509–522. [Google Scholar] [CrossRef]
- Zech, A.; Huebscher, M.; Vogt, L.; Banzer, W.; Hänsel, F.; Pfeifer, K. Neuromuscular training for rehabilitation of sports injuries: A systematic review. Med. Sci. Sports Exerc. 2009, 41, 1831–1841. [Google Scholar] [CrossRef]
- Nitz, A.J.; Dobner, J.J.; Kersey, D. Nerve injury and grades II and III ankle sprains. Am. J. Sports Med. 1985, 13, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Konradsen, L.; Magnusson, P. Increased inversion angle replication error in functional ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 246–251. [Google Scholar] [CrossRef]
- Kazemi, K.; Arab, A.M.; Abdollahi, I.; López-López, D.; Calvo-Lobo, C. Electromiography comparison of distal and proximal lower limb muscle activity patterns during external perturbation in subjects with and without functional ankle instability. Hum. Mov. Sci. 2017, 55, 211–220. [Google Scholar] [CrossRef]
- Ebig, M.; Lephart, S.M.; Burdett, R.C.; Miller, M.C.; Pincivero, D.M. The effect of sudden inversion stress on EMG activity of the peroneal and tibialis anterior muscles in the chronically unstable ankle. J. Orthop. Sports Phys. Ther. 1997, 26, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Vuurberg, G.; Hoorntje, A.; Wink, L.M.; Van Der Doelen, B.F.; Van Den Bekerom, M.P.; Dekker, R.; Van Dijk, C.N.; Krips, R.; Loogman, M.C.; Ridderikhof, M.L. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br. J. Sports Med. 2018, 52, 956. [Google Scholar] [CrossRef] [PubMed]
- Loudon, J.K.; Reiman, M.P.; Sylvain, J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: A systematic review. Br. J. Sports Med. 2014, 48, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.D.; Higgins, J.P.; Deeks, J.J. Interpretation of random effects meta-analyses. BMJ 2011, 342, d549. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G.; Cochrane Statistical Methods Group. Analysing Data and Undertaking Meta-Analyses. In Cochrane Handbook for Systematic Reviews of Interventions; The Cochrane Collaboration: Oxford, UK, 2008; pp. 243–296. [Google Scholar]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Hita-Contreras, F.; Martínez-Amat, A.; Aibar-Almazán, A.; Kim, K.-M. Ankle-joint self-mobilization and CrossFit training in patients with chronic ankle instability: A randomized controlled trial. J. Athl. Train. 2020, 55, 159–168. [Google Scholar] [CrossRef]
- Beazell, J.R.; Grindstaff, T.L.; Sauer, L.D.; Magrum, E.M.; Ingersoll, C.D.; Hertel, J. Effects of a proximal or distal tibiofibular joint manipulation on ankle range of motion and functional outcomes in individuals with chronic ankle instability. J. Orthop. Sports Phys. Ther. 2012, 42, 125–134. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Lomas Vega, R.; Osuna-Pérez, M.C.; Hita-Contreras, F.; Martínez-Amat, A. Effects of joint mobilization on chronic ankle instability: A randomized controlled trial. Disabil. Rehabil. 2015, 37, 601–610. [Google Scholar] [CrossRef]
- Shin, H.-J.; Kim, S.-H.; Jung, H.J.; Cho, H.-Y.; Hahm, S.-C. Manipulative Therapy Plus Ankle Therapeutic Exercises for Adolescent Baseball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 4997. [Google Scholar] [CrossRef]
- McKeon, P.O.; Wikstrom, E.A. Sensory-targeted ankle rehabilitation strategies for chronic ankle instability. Med. Sci. Sports Exerc. 2016, 48, 776–784. [Google Scholar] [CrossRef]
- Marrón-Gómez, D.; Rodríguez-Fernández, Á.L.; Martín-Urrialde, J.A. The effect of two mobilization techniques on dorsiflexion in people with chronic ankle instability. Phys. Ther. Sport 2015, 16, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Bolton, C.; Hale, S.; Telemeco, T. The effects of therapeutic exercise with and without mobilization in participants with chronic ankle instability: A randomized controlled trial. J. Sport Rehabil. 2020, 30, 206–213. [Google Scholar] [CrossRef]
- Kamali, F.; Sinaei, E.; Bahadorian, S. The immediate effect of talocrural joint manipulation on functional performance of 15–40 years old athletes with chronic ankle instability: A double-blind randomized clinical trial. J. Bodyw. Mov. Ther. 2017, 21, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Harkey, M.; McLeod, M.; Van Scoit, A.; Terada, M.; Tevald, M.; Gribble, P.; Pietrosimone, B. The immediate effects of an anterior-to-posterior talar mobilization on neural excitability, dorsiflexion range of motion, and dynamic balance in patients with chronic ankle instability. J. Sport Rehabil. 2014, 23, 351–359. [Google Scholar] [CrossRef]
- Babic, A.; Pijuk, A.; Brázdilová, L.; Georgieva, Y.; Raposo Pereira, M.A.; Poklepovic Pericic, T.; Puljak, L. The judgement of biases included in the category “other bias” in Cochrane systematic reviews of interventions: A systematic survey. BMC Med. Res. Methodol. 2019, 19, 77. [Google Scholar] [CrossRef]
- Page, M.J.; Higgins, J.P.; Sterne, J.A. Assessing Risk of Bias Due to Missing Results in a Synthesis. In Cochrane Handbook for Systematic Reviews of Interventions; The Cochrane Collaboration: Oxford, UK, 2008; pp. 349–374. [Google Scholar]
- McKeon, P.O.; Hertel, J. Systematic review of postural control and lateral ankle instability, part I: Can deficits be detected with instrumented testing? J. Athl. Train. 2008, 43, 293–304. [Google Scholar] [CrossRef]
- Tsikopoulos, K.; Sidiropoulos, K.; Kitridis, D.; Metaxiotis, D.; Ali, A. Do external supports improve dynamic balance in patients with chronic ankle instability? A network meta-analysis. Clin. Orthop. Relat. Res. 2020, 478, 359–377. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Delahunt, E.; Holden, S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br. J. Sports Med. 2017, 51, 113–125. [Google Scholar] [CrossRef]
- Kim, H.; Song, S.; Lee, S.; Lee, S. Short-term effects of joint mobilization with versus without voluntary movement in patients with chronic ankle instability: A single-blind randomized controlled trial. Phys. Ther. Rehabil. Sci. 2021, 10, 1–9. [Google Scholar] [CrossRef]
- Needle, A.R.; Palmer, J.A.; Kesar, T.M.; Binder-Macleod, S.A.; Swanik, C.B. Brain regulation of muscle tone in healthy and functionally unstable ankles. J. Sport Rehabil. 2013, 22, 202–211. [Google Scholar] [CrossRef]
- Rosen, A.B.; Yentes, J.M.; McGrath, M.L.; Maerlender, A.C.; Myers, S.A.; Mukherjee, M. Alterations in cortical activation among individuals with chronic ankle instability during single-limb postural control. J. Athl. Train. 2019, 54, 718–726. [Google Scholar] [CrossRef] [Green Version]
| Study | Sample Size | Duration | Intervention | Outcome | Author’s Conclusion |
|---|---|---|---|---|---|
| Beazell et al., 2012 [18] | EG1 = 15 EG2 = 14 CG = 13 | Three weeks | EG1 = proximal TFJM EG2 = distal TFJM CG = no intervention | DFROM SDT FAAM | The use of a proximal or distal tibiofibular joint manipulation in isolation did not enhance outcome effects beyond those of the control group. |
| Bolton et al., 2021 [23] | EG = 16 CG = 14 | Twice a week for six weeks | EG = TJM plus exercise CG = exercise | DFROM SEBT FAAM | The addition of MT to exercise may improve the improvement in ROM compared to exercise alone. |
| Cruz-Díaz et al., 2014 [19] | EG = 29 CG = 21 | Twice a week for three weeks | EG = WB_MWM CG = no intervention | DFROM SEBT CAIT | Joint mobilization techniques applied to subjects suffering from CAI were able to improve ankle DFROM, postural control, and self-reported instability. |
| Cruz-Díaz et al., 2020 [17] | EG = 25 CG = 24 | Twice a week for 12 weeks | EG = MWM plus CrossFit CG = CrossFit | DFROM SEBT CAIT | Ankle joint self-mobilization and CrossFit training were effective in improving ankle DFROM, dynamic postural control and self-reported instability in patients with CAI. |
| Harkey et al., 2014 [25] | EG = 15 CG = 15 | One day | EG = TJM CG = no intervention | DFROM SEBT | A single joint-mobilization treatment was efficacious at restoring DFROM in participants with CAI. |
| Kamali et al., 2017 [24] | EG = 20 CG = 20 | One day | EG = TJM CG = sham | SEBT | TJM can significantly increase the functional performance of athletes with CIA and can be an effective supplementary treatment for these subjects. |
| Marrón-Gómez et al., 2015 [22] | EG1 = 18 EG2 = 19 CG = 15 | 48 h | EG1 = WB_MWM EG2 = TJM CG = sham | DFROM | A single application of the WB-MWM or HVLA manual technique improves ankle dorsiflexion in people with CAI, and the effects persist for at least two days. |
| McKeon and Wikstrom 2015 [21] | EG = 20 CG = 20 | Six times in two weeks | EG = TJM CG = no intervention | WBLT SLBT FAAM | Both joint mobilization and plantar massage appear to demonstrate the greatest potential to improve sensorimotor function in those with CAI. |
| Shin et al., 2020 [20] | EG = 16 CG = 15 | Twice a week for four weeks | EG = TJM plus ATE CG = ATE | DFROM AMTI AccuSway AOFAS score | Adding HVLA to resistance exercises may be synergistically effective in improving the ankle status, pain intensity, ROM, and balance ability in ABP with CAI. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Moon, S. Effect of Joint Mobilization in Individuals with Chronic Ankle Instability: A Systematic Review and Meta-Analysis. J. Funct. Morphol. Kinesiol. 2022, 7, 66. https://doi.org/10.3390/jfmk7030066
Kim H, Moon S. Effect of Joint Mobilization in Individuals with Chronic Ankle Instability: A Systematic Review and Meta-Analysis. Journal of Functional Morphology and Kinesiology. 2022; 7(3):66. https://doi.org/10.3390/jfmk7030066
Chicago/Turabian StyleKim, Hyunjoong, and Seoyoung Moon. 2022. "Effect of Joint Mobilization in Individuals with Chronic Ankle Instability: A Systematic Review and Meta-Analysis" Journal of Functional Morphology and Kinesiology 7, no. 3: 66. https://doi.org/10.3390/jfmk7030066
APA StyleKim, H., & Moon, S. (2022). Effect of Joint Mobilization in Individuals with Chronic Ankle Instability: A Systematic Review and Meta-Analysis. Journal of Functional Morphology and Kinesiology, 7(3), 66. https://doi.org/10.3390/jfmk7030066







