Anatomy, Morphology and Function of the Tensor of Vastus Intermedius: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Criteria for Study Selection
2.2. Search Strategy
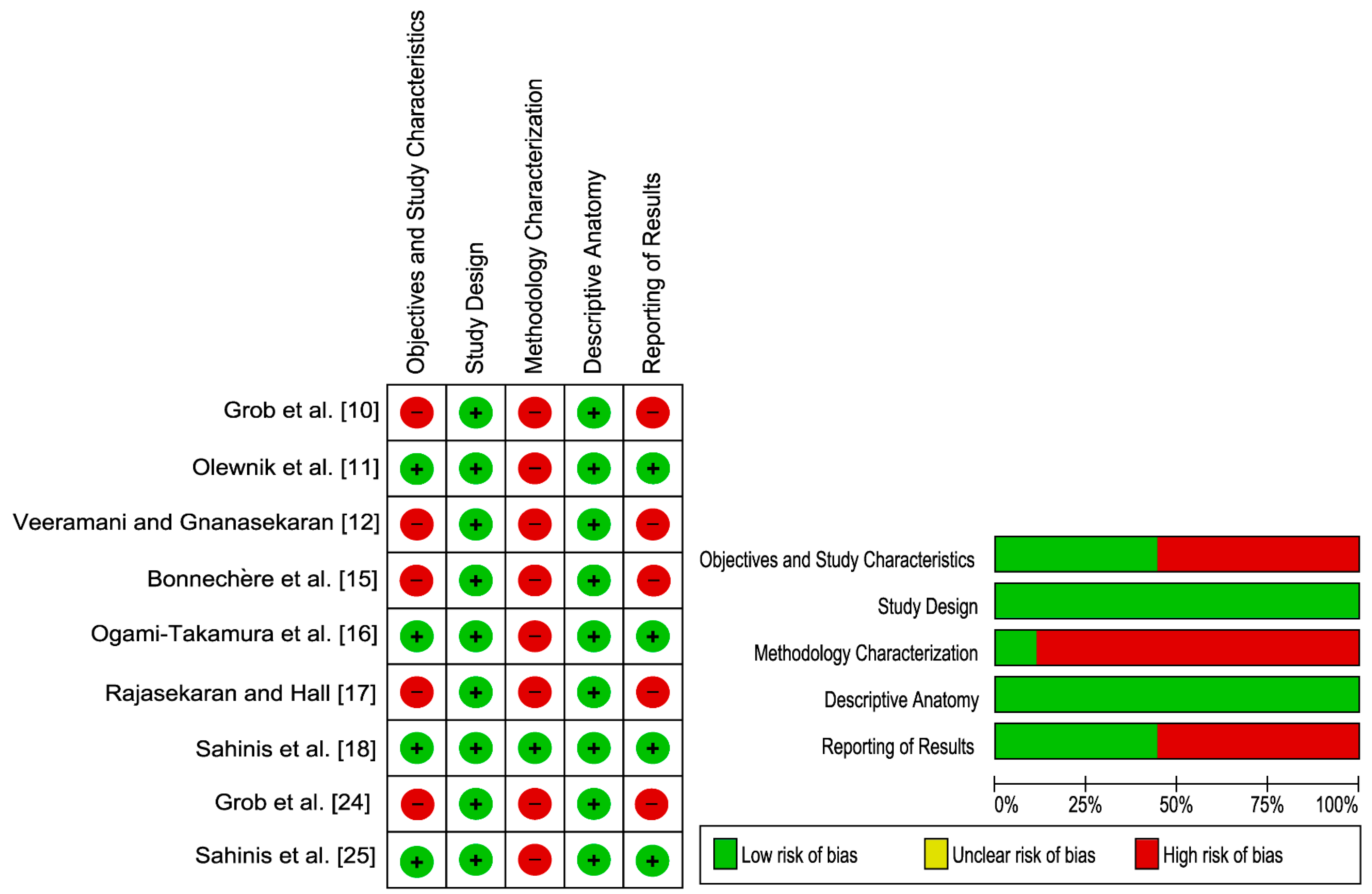
2.3. Risk of Bias Assessment
2.4. Data Extraction
3. Results
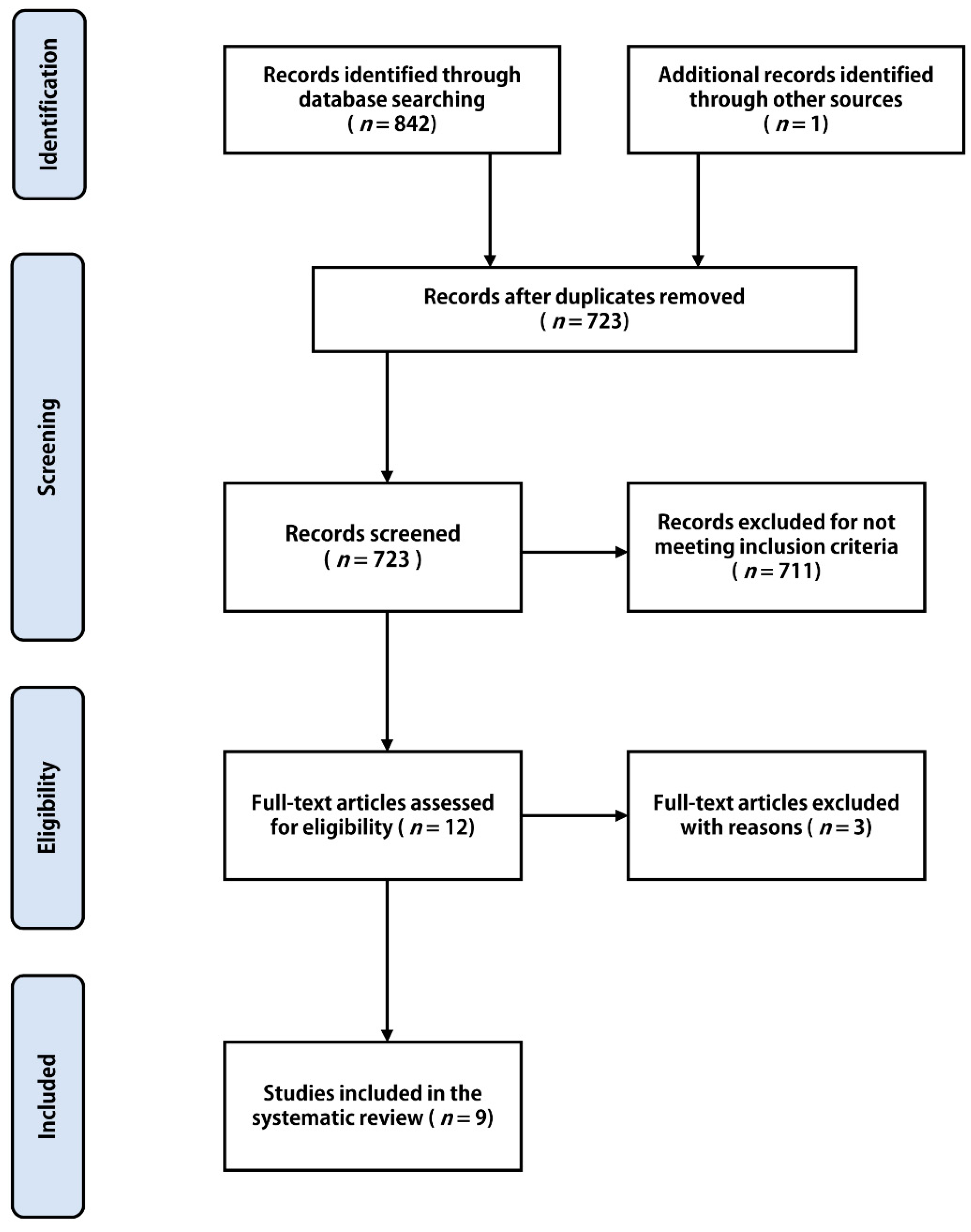
3.1. Study Selection
3.2. Criteria for Study Selection
3.3. Characteristics of the Included Studies
3.4. Prevalence
3.5. Anatomy
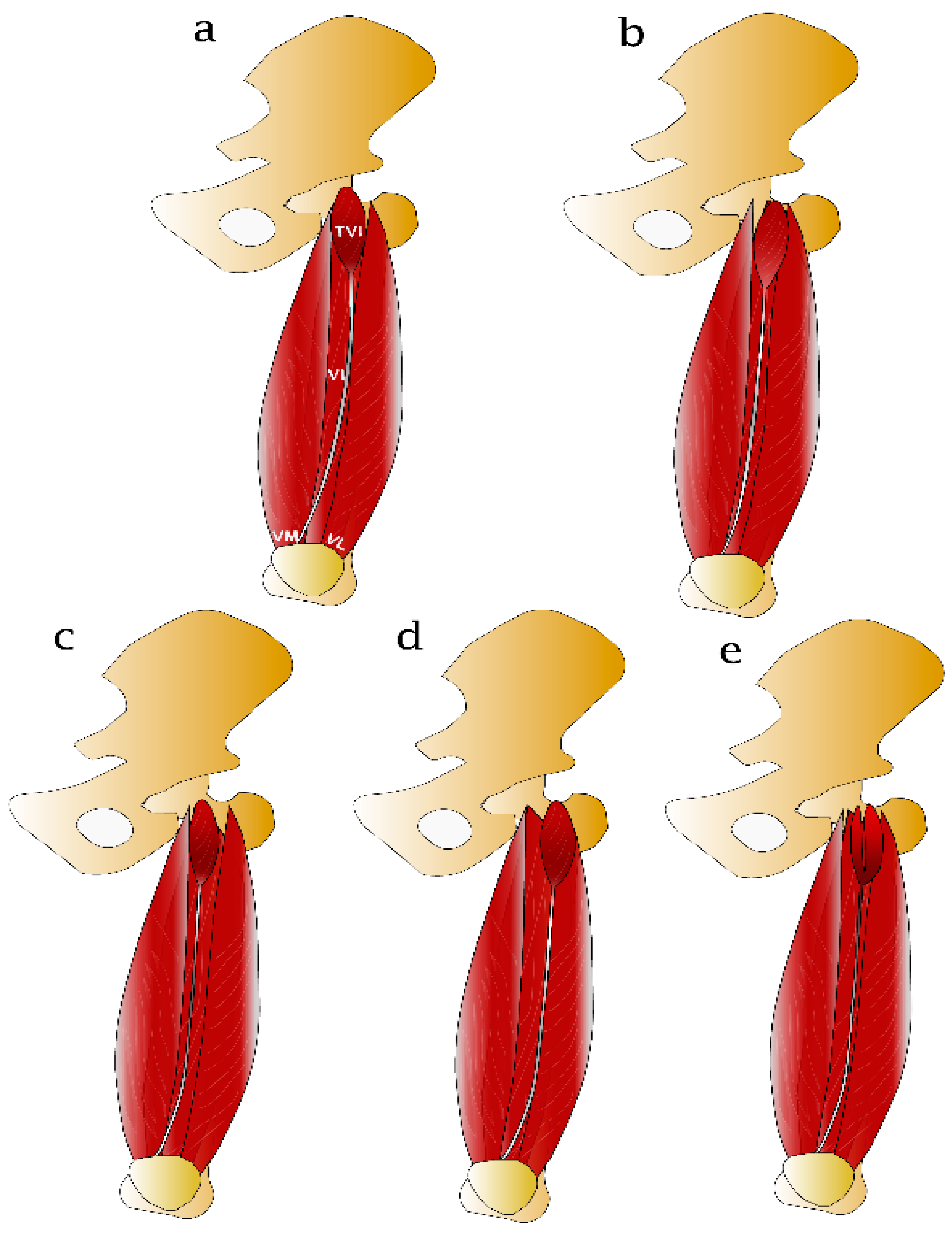
3.6. Variations
3.7. Morphological Characteristics
3.8. Neurovascular Supply
3.9. Functional Anatomy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheung, Y. Normal Variants: Accessory Muscles About the Ankle. Magn. Reson. Imaging Clin. N. Am. 2017, 25, 11–26. [Google Scholar] [CrossRef]
- Filip, V.; Philippe, D.; Maximiliaan, M. The Accessory muscles of the Axilla. Acta Orthop. Belg. 2019, 85, 421–428. [Google Scholar]
- Labbé, J.L.; Peres, O.; Leclair, O.; Goulon, R.; Scemama, P.; Jourdel, F.; Duparc, B. Progressive limitation of knee flexion secondary to an accessory quinticeps femoris muscle in a child: A case report and literature review. J. Bone Jt. Surg. Ser. B 2011, 93, 1568–1570. [Google Scholar] [CrossRef][Green Version]
- Mendes Da Costa, T.; Leveille, L.A.; Rosenbaum, D.G. Quads or quins? Atraumatic restricted knee flexion due to accessory quadriceps bands in children. Pediatr. Radiol. 2020, 435–440. [Google Scholar] [CrossRef]
- Andrikoula, S.; Tokis, A.; Vasiliadis, H.S.; Georgoulis, A. The extensor mechanism of the knee joint: An anatomical study. Knee Surgery, Sport. Traumatol. Arthrosc. 2006, 14, 214–220. [Google Scholar] [CrossRef]
- Iriuchishima, T.; Shirakura, K.; Yorifuji, H.; Fu, F.H. Anatomical evaluation of the rectus femoris tendon and its related structures. Arch. Orthop. Trauma Surg. 2012, 132, 1665–1668. [Google Scholar] [CrossRef] [PubMed]
- Yablon, C.M.; Pai, D.; Dong, Q.; Jacobson, J.A. Magnetic Resonance Imaging of the Extensor Mechanism. Magn. Reson. Imaging Clin. N. Am. 2014, 22, 601–620. [Google Scholar] [CrossRef] [PubMed]
- Zeiss, J.; Saddemi, S.R.; Ebraheim, N.A. MR imaging of the quadriceps tendon: Normal layered configuration and its importance in cases of tendon rupture. Am. J. Roentgenol. 1992, 159, 1031–1034. [Google Scholar] [CrossRef]
- Lieb, F.J.; Perry, J. Quadriceps function. An anatomical and mechanical study using amputated limbs. J. Bone Joint Surg. Am. 1968, 50, 1535–1548. [Google Scholar] [CrossRef]
- Grob, K.; Ackland, T.; Kuster, M.S.; Manestar, M.; Filgueira, L. A newly discovered muscle: The tensor of the vastus intermedius. Clin. Anat. 2016, 29, 256–263. [Google Scholar] [CrossRef]
- Olewnik, Ł.; Tubbs, R.S.; Ruzik, K.; Podgórski, M.; Aragonés, P.; Waśniewska, A.; Karauda, P.; Szewczyk, B.; Sanudo, J.R.; Polguj, M. Quadriceps or multiceps femoris?—Cadaveric study. Clin. Anat. 2020, 34, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Veeramani, R.; Gnanasekaran, D. Morphometric study of tensor of vastus intermedius in South Indian population. Anat. Cell Biol. 2017, 50, 7. [Google Scholar] [CrossRef][Green Version]
- Golland, J.A.; Mahon, M.W.P. Anatomical variations in human quadriceps femoris muscles. J. Anat. 1986, 263–264. [Google Scholar]
- Willan, P.L.; Mahon, M.; Golland, J.A. Morphological variations of the human vastus lateralis muscle. J. Anat. 1990, 168, 235–239. [Google Scholar] [PubMed]
- Bonnechère, B.; Louryan, S.; Feipel, V. Triceps, quadriceps or pentaceps femoris? Need for proper muscle definition. Morphologie 2020, 104, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Ogami-Takamura, K.; Saiki, K.; Endo, D.; Murai, K.; Nishi, K.; Okamoto, K.; Murata, H.; Hara, T.; Tsurumoto, T. Gross anatomical investigation of the muscular head between the vastus lateralis and intermedius in the Japanese population: A cadaver study. Anat. Sci. Int. 2020, 1, 3. [Google Scholar] [CrossRef]
- Rajasekaran, S.; Hall, M.M. Sonographic Appearance of the Tensor of the Vastus Intermedius. PM R 2016, 8, 1020–1023. [Google Scholar] [CrossRef] [PubMed]
- Sahinis, C.; Kellis, E.; Ellinoudis, A.; Dafkou, K. In Vivo Assessment of the Tensor Vastus Intermedius Cross-sectional Area Using Ultrasonography. Muscle Ligaments Tendons J. 2020, 10, 416. [Google Scholar] [CrossRef]
- Sahinis, C.; Kellis, E.; Dafkou, K.; Ellinoudis, A. Reliability of Distal Hamstring Tendon Length and Cross-sectional Area Using 3-D Freehand Ultrasound. Ultrasound Med. Biol. 2021, 47, 2579–2588. [Google Scholar] [CrossRef]
- Lund, B.; Nielsen, T.; Faunø, P.; Christiansen, S.E.; Lind, M. Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 593–598. [Google Scholar] [CrossRef]
- Ramseier, L.E.; Werner, C.M.L.; Heinzelmann, M. Quadriceps and patellar tendon rupture. Injury 2006, 37, 516–519. [Google Scholar] [CrossRef] [PubMed]
- Franchi, T. Tensor vastus intermedius: A review of its discovery, morphology and clinical importance. Folia Morphol. (Warsz). 2020. [Google Scholar] [CrossRef]
- Henry, B.M.; Tomaszewski, K.A.; Ramakrishnan, P.K.; Roy, J.; Vikse, J.; Loukas, M.; Tubbs, R.S.; Walocha, J.A. Development of the anatomical quality assessment (AQUA) tool for the quality assessment of anatomical studies included in meta-analyses and systematic reviews. Clin. Anat. 2017, 30, 6–13. [Google Scholar] [CrossRef]
- Grob, K.; Manestar, M.; Gascho, D.; Ackland, T.; Gilbey, H.; Fretz, C.; Kuster, M.S. Magnetic resonance imaging of the tensor vastus intermedius: A topographic study based on anatomical dissections. Clin. Anat. 2017, 30, 1096–1102. [Google Scholar] [CrossRef] [PubMed]
- Sahinis, C.; Kellis, E.; Galanis, N.; Dafkou, K.; Ellinoudis, A. Intra- and inter-muscular differences in the cross-sectional area of the quadriceps muscles assessed by extended field-of-view ultrasonography. Med. Ultrason. 2020, 22, 152–158. [Google Scholar] [CrossRef]
- Yoshida, S.; Ichimura, K.; Sakai, T. Structural diversity of the vastus intermedius origin revealed by analysis of isolated muscle specimens. Clin. Anat. 2017, 30, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Willan, P.L.T.; Ransome, J.A.; Mahon, M. Variability in human quadriceps muscles: Quantitative study and review of clinical literature. Clin. Anat. 2002, 15, 116–128. [Google Scholar] [CrossRef]
- Grob, K.; Manestar, M.; Filgueira, L.; Ackland, T.; Gilbey, H.; Kuster, M.S. New insight in the architecture of the quadriceps tendon. J. Exp. Orthop. 2016, 32, 3734. [Google Scholar] [CrossRef]
- Kellis, E.; Sahinis, C.; Dafkou, K.; Ellinoudis, A.; Galanis, N. Hamstring to quadriceps strength ratio and cross-sectional area of the quadriceps and hamstrings muscles assessed using extended field-of-view ultrasonography. Res. Sports Med. 2020, 25–42. [Google Scholar] [CrossRef] [PubMed]

| Study | Bonnechère et al. [15] | Grob et al. [10] | Grob et al. [24] | Ogami-Takamura et al. [16] | |
|---|---|---|---|---|---|
| Subject/Specimen characteristics | 20 limbs, 4 M and 6F Age N/R | 26 limbs, 9 M and 7 F, Age N/R | 1 lower limb | 35 lower limbs, 19 M and 16 F, Age 61–98 years | |
| Pathology | N/R | N/R | N/R | Without any injury | |
| Dissection technique | From the supine position, three skin incisions were performed: from the anterior superior iliac spine to the pubic tubercle, a horizontal incision below the tibial tuberosity and a vertical incision between these two incisions. Different muscle bellies were identified manually, and different parts were noted only if it was possible to separate the different heads without scalpel. * | From supine position, the anterior aspect of the hip joint was approached. Primarily, the ascending branch of the LCFA was recognized and traced medially. TVI identification was traced from their origin to their insertion. * | Dissection of all lower limb muscles. Muscle bellies of the extensor apparatus were traced from their origins to their insertion into the quadriceps tendon, and their affiliation was assessed. * | Line connecting the center of the inguinal ligament to the patella was incised. VL, VM and VI the TVI were described. * | |
| Imaging technique | N/R | N/R | MRI | 15 lower limbs, using computed tomography | |
| Measurement recorded | Lateral extensor apparatus with emphasis on TVI identification, origin, insertion and innervation. | Observation and tracing of neurovascular supply of TVI to determine its relationship with the VL and VI. Examination of TVI anatomy with respect to its location, origin and insertion. No quantification of TVI dimension was reported. | Description οf lateral knee extensor apparatus and TVI with focus on conjunction between the TVI, VI, and VL. No quantification of TVI dimensions. | TVI belly and aponeurosis length using a vernier caliper. Descriptions of TVI location, origin, insertion and innervation | |
| Investigators | N/R | N/R | N/R | N/R | |
| Subject/Specimen characteristics | 106 lower limbs 34 M and 19 F, Mean Age 68.4 years | 20 subjects (40 lower limbs), 10 M and 10 F | 21 subjects, (21 lower limbs), 17 M and 4 F, Mean Age 21.72 ± 1.83 years | 10 subjects (10 lower limbs), 10 M and F, Mean age 21.6 ± 2.41 years | 36 lower limbs, 27 M and 9 F |
| Pathology | Any lower limbs with evidence of surgical intervention in the dissected area were excluded | N/R | No lower limb injury | No lower limb injury | No lower limb injury |
| Dissection technique | From the supine position, the hip joint capsule was resected and the inguinal ligament identified. Muscle belly’s origin and insertion were identified. * | N/R | N/R | N/R | A longitudinal incision from mid-inguinal point to the patella. Muscle components were defined by blunt dissection. * |
| Imaging technique | N/R | Ultrasound | Ultrasound | Extended field of view ultrasound | N/R |
| Measurement recorded | Length, width, thickness of belly and muscle-tendon unit junction using an electronic digital caliber. | Descriptions of TVI belly and tendon relationship with adjacent structures. Dimensions not reported. | CSA along TVI belly and tendon | TVI CSA at two sites | TVI belly and aponeurosis length and distance of fusion of TVI from the patella to VL or VI using a digital vernier caliper. Description of TVI location, origin, insertion and neurovascular supply |
| Investigators | N/R | N/R | Experienced investigator | Experienced investigator | N/R |
| Study | TVI/n Lower Limbs | % Prevalence of TVI |
|---|---|---|
| Cadaveric studies | ||
| Bonnechère et al. [15] | 7/20 | 35 |
| Grob et al. [10] | 26/26 | 100 |
| Ogami-Takamura et al. [16] | 35/35 | 100 |
| Olewnik et al. [11] | 68/106 | 64.1 |
| Veeramani and Gnanasekaran [12] | 36/36 | 100 |
| Imaging Studies | ||
| Grob et al. [24] | 1/1 | 100 |
| Rajasekaran and Hall [17] | 40/40 | 100 |
| Sahinis et al. [18] | 21/21 | 100 |
| Sahinis et al. [25] | 10/10 | 100 |
| Total | 244/295 | 82.7 |
| Studies | n Lower Limbs that TVI Identified | Independent Type (%) | VI Type (%) | VL Type (%) | GM Type (%) | Common Type (%) | Multiple Heads of TVI |
|---|---|---|---|---|---|---|---|
| Bonnechère et al. [15] | 7 | 14 | - | 86 | - | - | - |
| Grob et al. [10] | 26 | 42.31 | 23.08 | 19.23 | - | 15.38 | 5 cases |
| Ogami-Takamura et al. [16] | 35 | 11 | 23 | 37 | - | 29 | - |
| Olewnik et al. [11] * | 68 | 44.1 | 4.5 | 23.5 | 2.9 | - | 25% |
| Veeramani and Gnanasekaran [12] | 36 | 33.33 | 8.33 | 30.56 | - | 27.78 | 3 cases |
| Muscle Cross-Sectional Area (cm2) | |||||
|---|---|---|---|---|---|
| Study | Muscle Length (mm) | Muscle Width (mm) | Muscle Thickness (mm) | Proximal Site | Distal Site |
| Ogami-Takamura et al. [16] | 102.36 ± 34.05 | - | - | - | - |
| Olewnik et al. [11] | 101.863 ± 16.96 | 16.76 ± 5.55 | 4.19 ± 1.44 | - | - |
| Sahinis et al. [18] | - | - | - | 1.32 ± 0.16 | 1.22 ± 0.14 |
| Sahinis et al. [25] | 1.31 ± 0.09 | 1.21 ± 0.10 | |||
| Veeramani and Gnanasekaran [12] | 145.40 ± 37.55 | - | - | - | - |
| Muscle-Tendon Junction | Tendon Cross-Sectional Area (cm2) | |||||
|---|---|---|---|---|---|---|
| Study | Tendon Length (mm) | Tendon Width (mm) | Tendon Thickness (mm) | Proximal Site | Middle Site | Distal Site |
| Ogami-Takamura et al. [16] | 208.50 ± 36.03 | - | - | - | - | - |
| Olewnik et al. [11] | 213.91 ± 34.93 | 14.21 ± 5.92 | 1.70 ± 1.08 | - | - | - |
| Sahinis et al. [18] | - | - | - | 0.21 ± 0.01 | 0.19 ± 0.01 | 0.19 ± 0.01 |
| Veeramani and Gnanasekaran [12] | 193.55 ± 42.32 | - | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sahinis, C.; Kellis, E. Anatomy, Morphology and Function of the Tensor of Vastus Intermedius: A Systematic Review. J. Funct. Morphol. Kinesiol. 2021, 6, 77. https://doi.org/10.3390/jfmk6030077
Sahinis C, Kellis E. Anatomy, Morphology and Function of the Tensor of Vastus Intermedius: A Systematic Review. Journal of Functional Morphology and Kinesiology. 2021; 6(3):77. https://doi.org/10.3390/jfmk6030077
Chicago/Turabian StyleSahinis, Chrysostomos, and Eleftherios Kellis. 2021. "Anatomy, Morphology and Function of the Tensor of Vastus Intermedius: A Systematic Review" Journal of Functional Morphology and Kinesiology 6, no. 3: 77. https://doi.org/10.3390/jfmk6030077
APA StyleSahinis, C., & Kellis, E. (2021). Anatomy, Morphology and Function of the Tensor of Vastus Intermedius: A Systematic Review. Journal of Functional Morphology and Kinesiology, 6(3), 77. https://doi.org/10.3390/jfmk6030077