Breathing Signature as Vitality Score Index Created by Exercises of Qigong: Implications of Artificial Intelligence Tools Used in Traditional Chinese Medicine
Abstract
:1. Background
2. Clinical Significance
3. Mechanism of Action for Practice of Breathing
4. Comprehensive Healthcare by Integrating Western Medicine with TCM
5. The Concept
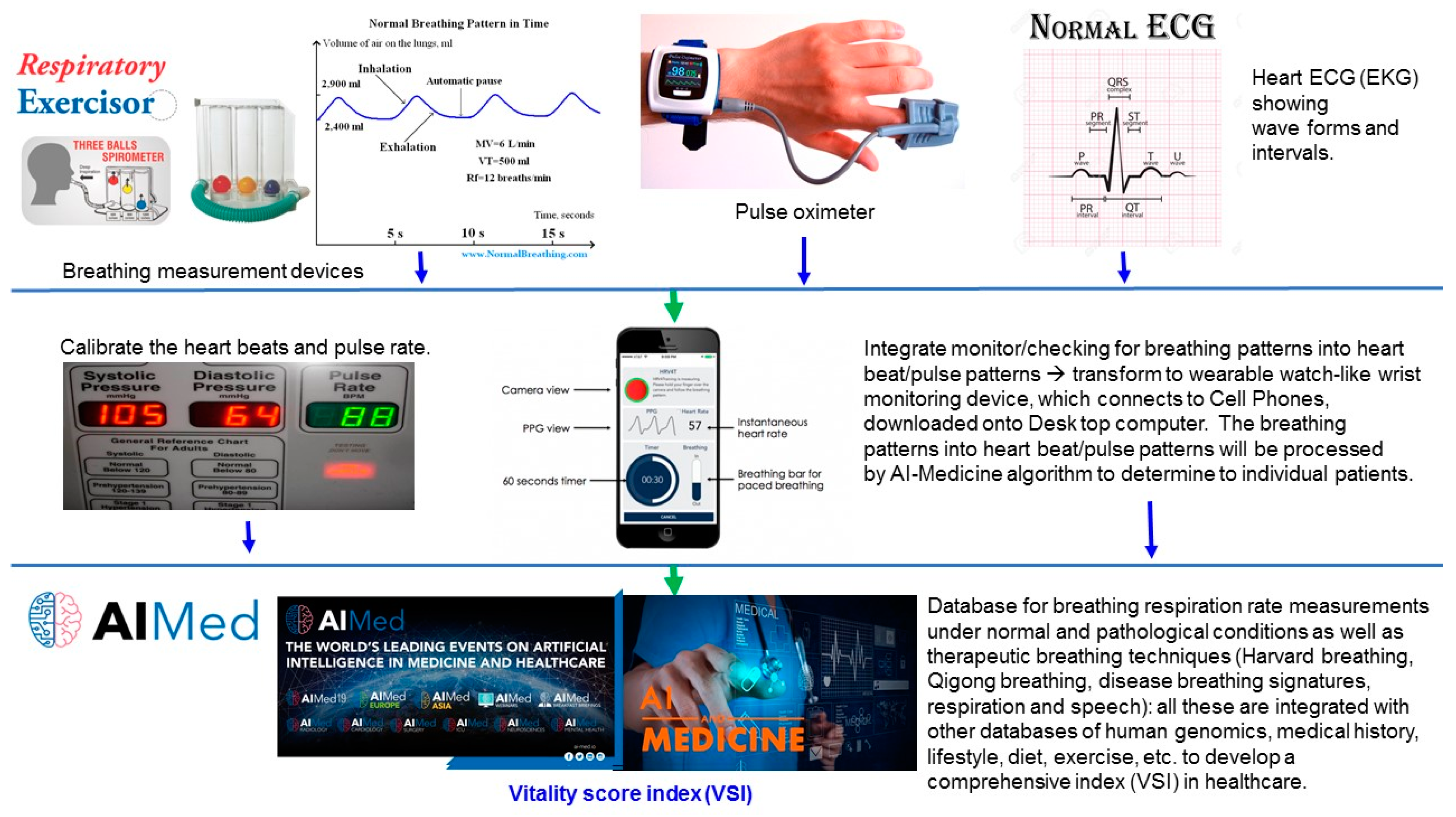
6. Technology and AI Medicine
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chakraborty, A.A.; Laukka, T.; Myllykoski, M.; Ringel, A.E.; Booker, M.A.; Tolstorukov, M.Y.; Meng, Y.J.; Meier, S.R.; Jennings, R.B.; Creech, A.L.; et al. Histone demethylase KDM6A directly senses oxygen to control chromatin and cell fate. Science 2019, 363, 1217–1222. [Google Scholar] [CrossRef] [Green Version]
- Schodel, J.; Ratcliffe, P.J. Mechanisms of hypoxia signalling: New implications for nephrology. Nat. Rev. Nephrol. 2019, 15, 641–659. [Google Scholar] [CrossRef]
- Xiang, L.; Semenza, G.L. Hypoxia-inducible factors promote breast cancer stem cell specification and maintenance in response to hypoxia or cytotoxic chemotherapy. Adv. Cancer Res. 2019, 141, 175–212. [Google Scholar] [PubMed]
- Adachi, M.; Watanabe, M.; Kurata, Y.; Inoue, Y.; Notsu, T.; Yamamoto, K.; Horie, H.; Tanno, S.; Morita, M.; Miake, J.; et al. Beta-Adrenergic Blocker, Carvedilol, Abolishes Ameliorating Actions of Adipose-Derived Stem Cell Sheets on Cardiac Dysfunction and Remodeling After Myocardial Infarction. Circ. J. 2019, 83, 2282–2291. [Google Scholar] [CrossRef] [PubMed]
- Sorg, A.L.; von Kries, R.; Klemme, M.; Gerstl, L.; Weinberger, R.; Beyerlein, A.; Lack, N.; Felderhoff-Muser, U.; Dzietko, M. Risk factors for perinatal arterial ischaemic stroke: A large case-control study. Dev. Med. Child Neurol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Kulikowicz, E.; Santos, P.T.; Koehler, R.C.; Martin, L.J.; Lee, J.K. Spatial T-maze identifies cognitive deficits in piglets 1 month after hypoxia-ischemia in a model of hippocampal pyramidal neuron loss and interneuron attrition. Behav. Brain. Res. 2019, 369, 111921. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.Y.; Tang, C.J.; Wu, J.; Zhou, J.S. Parkinson’s disease in China. Neurol. Sci. 2011, 32, 23–30. [Google Scholar] [CrossRef]
- Lin, C.Y.; Wei, T.T.; Wang, C.C.; Chen, W.C.; Wang, Y.M.; Tsai, S.Y. Acute Physiological and Psychological Effects of Qigong Exercise in Older Practitioners. Evid.-Based Complement. Altern. Med. 2018, 2018, 4960978. [Google Scholar] [CrossRef] [Green Version]
- Klein, P.; Picard, G.; Baumgarden, J.; Schneider, R. Meditative Movement, Energetic, and Physical Analyses of Three Qigong Exercises: Unification of Eastern and Western Mechanistic Exercise Theory. Medicines 2017, 4, 69. [Google Scholar] [CrossRef] [Green Version]
- Tang, N.; Chang, J.; Zeng, Y.; Zheng, J. Tanshinone IIA protects hypoxia-induced injury by preventing microRNA-28 up-regulation in PC-12 cells. Eur. J. Pharmacol. 2019, 854, 265–271. [Google Scholar] [CrossRef]
- Devi, U.; Singh, M.; Roy, S.; Gupta, P.S.; Ansari, M.N.; Saeedan, A.S.; Kaithwas, G. Activation of prolyl hydroxylase-2 for stabilization of mitochondrial stress along with simultaneous downregulation of HIF-1alpha/FASN in ER + breast cancer subtype. Cell Biochem. Funct. 2019, 37, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Udjus, C.; Cero, F.T.; Halvorsen, B.; Behmen, D.; Carlson, C.R.; Bendiksen, B.A.; Espe, E.K.; Sjaastad, I.; Loberg, E.M.; Yndestad, A.; et al. Caspase-1 induces smooth muscle cell growth in hypoxia-induced pulmonary hypertension. Am. J. Physiol.-Lung Cell Mol. Physiol. 2019, 316, L999–L1012. [Google Scholar] [CrossRef] [PubMed]
- Perdrizet, G.A. Chronic Diseases as Barriers to Oxygen Delivery: A Unifying Hypothesis of Tissue Reoxygenation Therapy. Adv. Exp. Med. Biol. 2017, 977, 15–20. [Google Scholar] [PubMed]
- Polrola, P.; Wilk-Franczuk, M.; Wilczynski, J.; Nowak-Starz, G.; Goral-Polrola, J.; Chruscinski, G.; Bonislawska, I.; Pedrycz, A.; Zychowska, M. Anti-inflammatory effect on genes expression after four days of Qigong training in peripheral mononuclear blood cells in healthy women. Ann. Agric. Environ. Med. 2018, 25, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Hida, T.; Yamada, Y.; Ueyama, M.; Araki, T.; Nishino, M.; Kurosaki, A.; Jinzaki, M.; Honda, H.; Hatabu, H.; Kudoh, S. Time-resolved quantitative evaluation of diaphragmatic motion during forced breathing in a health screening cohort in a standing position: Dynamic chest phrenicography. Eur. J. Radiol. 2019, 113, 59–65. [Google Scholar] [CrossRef] [Green Version]
- Putiri, A.L.; Close, J.R.; Lilly, H.R.; Guillaume, N.; Sun, G.C. Qigong Exercises for the Management of Type 2 Diabetes Mellitus. Medicines 2017, 4, 59. [Google Scholar] [CrossRef] [Green Version]
- Chu, M.; Nguyen, T.; Pandey, V.; Zhou, Y.; Pham, H.N.; Bar-Yoseph, R.; Radom-Aizik, S.; Jain, R.; Cooper, D.M.; Khine, M. Respiration rate and volume measurements using wearable strain sensors. NPJ Digit. Med. 2019, 2, 8. [Google Scholar] [CrossRef]
- Zheng, Z. What have we learnt from acupuncture research of fibromyalgia? Longhua Chin. Med. 2018, 19, 1862–1871. [Google Scholar] [CrossRef]
- Yeo, E.J. Hypoxia and aging. Exp. Mol. Med. 2019, 51, 67. [Google Scholar] [CrossRef]
- Lee, M.S.; Kim, M.K.; Ryu, H. Qi-training (qigong) enhanced immune functions: What is the underlying mechanism? Int. J. Neurosci. 2005, 115, 1099–1104. [Google Scholar] [CrossRef]
- Wang, C.X.; Xu, D.H. The beneficial effect of qigong on the ventricular function and microcirculation in deficiency of heart-energy hypertensive patients. Zhong Xi Yi Jie He Za Zhi 1991, 11, 659–660. [Google Scholar] [PubMed]
- Ohnishi, S.T.; Ohnishi, A.T. How Far Can Ki-energy Reach?—A Hypothetical Mechanism for the Generation and Transmission of Ki-energy. Evid.-Based Complement Altern. Med. 2009, 6, 379–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohnishi, S.T.; Ohnishi, A.T. Philosophy, psychology, physics, and practice of ki. Evid.-Based Complement Altern. Med. 2009, 6, 175–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiwari, A.; Chan, C.L.; Ho, R.T.; Tsao, G.S.; Deng, W.; Hong, A.W.; Fong, D.Y.; Fung, H.Y.; Pang, E.P.; Cheung, D.S.; et al. Effect of a qigong intervention program on telomerase activity and psychological stress in abused Chinese women: A randomized, wait-list controlled trial. BMC Complement. Altern. Med. 2014, 14, 300. [Google Scholar] [CrossRef]
- Ho, R.T.; Chan, J.S.; Wang, C.W.; Lau, B.W.; So, K.F.; Yuen, L.P.; Sham, J.S.; Chan, C.L. A randomized controlled trial of qigong exercise on fatigue symptoms, functioning, and telomerase activity in persons with chronic fatigue or chronic fatigue syndrome. Ann. Behav. Med. 2012, 44, 160–170. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Couet, J.; Lisanti, M.P. Src tyrosine kinases, Galpha subunits, and H-Ras share a common membrane-anchored scaffolding protein, caveolin. Caveolin binding negatively regulates the auto-activation of Src tyrosine kinases. J. Biol. Chem. 1996, 271, 29182–29190. [Google Scholar] [CrossRef] [Green Version]
- Pagnozzi, L.A.; Butcher, J.T. Mechanotransduction Mechanisms in Mitral Valve Physiology and Disease Pathogenesis. Front. Cardiovasc. Med. 2017, 4, 83. [Google Scholar] [CrossRef] [Green Version]
- Leong, P.K.; Ko, K.M. Shengmai San: A modern medicine perspective on its remedial effects on Qi and Yin deficiency syndrome in Chinese medicine. Longhua Chin. Med. 2018, 1, 4731. [Google Scholar] [CrossRef]
- Sisa, C.; Kholia, S.; Naylor, J.; Sanchez, M.B.H.; Bruno, S.; Deregibus, M.C.; Camussi, G.; Inal, J.M.; Lange, S.; Hristova, M. Mesenchymal Stromal Cell Derived Extracellular Vesicles Reduce Hypoxia-Ischaemia Induced Perinatal Brain Injury. Front. Physiol. 2019, 10, 282. [Google Scholar] [CrossRef] [Green Version]
- Guo, F.; Tang, S.; Guo, T.; Bartell, S.; Detrano, R. Revised threshold values for neonatal oxygen saturation at mild and moderate altitudes. Acta Paediatr. 2019. [Google Scholar] [CrossRef]
- Li, S.C.; Han, Y.P.; Dethlefs, B.A.; Loudon, W.G. Therapeutic Window, a Critical Developmental Stage for Stem Cell Therapies. Curr. Stem Cell Res. Ther. 2010, 5, 297–303. [Google Scholar] [PubMed]
- Al-Halhouli, A.; Al-Ghussain, L.; el Bouri, S.; Liu, H.; Zheng, D. Fabrication and Evaluation of a Novel Non-Invasive Stretchable and Wearable Respiratory Rate Sensor Based on Silver Nanoparticles Using Inkjet Printing Technology. Polymers 2019, 11, 1518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nayan, N.A.; Risman, N.S.; Jaafar, R. A portable respiratory rate estimation system with a passive single-lead electrocardiogram acquisition module. Technol. Health Care. 2016, 24, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Park, C.A.; Lee, Y.B.; Kim, H.K.; Kang, C.K. EEG signals during mouth breathing in a working memory task. Int. J. Neurosci. 2019, 1–10. [Google Scholar] [CrossRef]
- Krug, B.; Kugel, H.; Harnischmacher, U.; Heindel, W.; Schmidt, R.; Krings, F. MR pulsatility measurements in peripheral arteries: Preliminary results. Magn. Reson. Med. 1995, 34, 698–705. [Google Scholar] [CrossRef]
- Cloete, E.; Gentles, T.L.; Dixon, L.A.; Webster, D.R.; Agnew, J.D.; Davidkova, S.; Alsweiler, J.M.; Rogers, J.; Bloomfield, F.H. Feasibility study assessing equitable delivery of newborn pulse oximetry screening in New Zealand’s midwifery-led maternity setting. BMJ Open 2019, 9, e030506. [Google Scholar] [CrossRef] [Green Version]
- Naschitz, J.E.; Bezobchuk, S.; Mussafia-Priselac, R.; Sundick, S.; Dreyfuss, D.; Khorshidi, I.; Karidis, A.; Manor, H.; Nagar, M.; Peck, E.R.; et al. Pulse transit time by R-wave-gated infrared photoplethysmography: Review of the literature and personal experience. J. Clin. Monit. Comput. 2004, 18, 333–342. [Google Scholar] [CrossRef]
- Oddie, S.; McGuire, A.W. Response to the Letter “RE: Commentary on ‘Pulse Oximetry Screening for Critical Congenital Heart Defects’”. Neonatology 2019, 116, 1–4. [Google Scholar] [CrossRef]
- Kodituwakku, S.; Lazar, S.W.; Indic, P.; Chen, Z.; Brown, E.N.; Barbieri, R. Point process time-frequency analysis of dynamic respiratory patterns during meditation practice. Med. Biol. Eng. Comput. 2012, 50, 261–275. [Google Scholar] [CrossRef] [Green Version]
- Kodituwakku, S.; Lazar, S.W.; Indic, P.; Brown, E.N.; Barbieri, R. Point process time-frequency analysis of respiratory sinus arrhythmia under altered respiration dynamics. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2010, 2010, 1622–1625. [Google Scholar]
- Ye, C.; Murano, E.; Stone, M.; Prince, J.L. A Bayesian approach to distinguishing interdigitated tongue muscles from limited diffusion magnetic resonance imaging. Comput. Med. Imaging Graph. 2015, 45, 63–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmar, C.R.; Brown, A.D.; Qian, M.; Laska, E.; Siegel, C.; Li, M.; Abu-Amara, D.; Tsiartas, A.; Richey, C.; Smith, J.; et al. Speech-based markers for posttraumatic stress disorder in US veterans. Depress Anxiety 2019, 36, 607–616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Wen, T.; Liao, W. Neurally adjusted ventilatory assist versus pressure support ventilation in patient-ventilator interaction and clinical outcomes: A meta-analysis of clinical trials. Ann. Transl. Med. 2019, 7, 382. [Google Scholar] [CrossRef] [PubMed]
- Zoladz, P.R.; Diamond, D.M. Current status on behavioral and biological markers of PTSD: A search for clarity in a conflicting literature. Neurosci. Biobehav. Rev. 2013, 37, 860–895. [Google Scholar] [CrossRef]
- Li, S.C.; Tachiki, L.M.; Kabeer, M.H.; Dethlefs, B.A.; Anthony, M.J.; Loudon, W.G. Cancer genomic research at the crossroads: Realizing the changing genetic landscape as intratumoral spatial and temporal heterogeneity becomes a confounding factor. Cancer Cell Int. 2014, 14, 111–116. [Google Scholar] [CrossRef] [Green Version]
- Lehrner, A.; Yehuda, A.R. Biomarkers of PTSD: Military applications and considerations. Eur. J. Psychotraumatol. 2014, 5. [Google Scholar] [CrossRef] [Green Version]
- Shalev, A.; Liberzon, I.; Marmar, C. Post-Traumatic Stress Disorder. N. Engl. J. Med. 2017, 376, 2459–2469. [Google Scholar] [CrossRef]
- Manchester, W. The Last Lion: Winston Spencer Churchill Is a Trilogy of Biographies Covering the Life of Winston Churchill; Little, Brown and Company: Boston, MA, USA, 1983; p. 983. [Google Scholar]
- Mehta, S.; Grabowski, T.J.; Razavi, M.; Eaton, B.; Bolinger, L. Analysis of speech-related variance in rapid event-related fMRI using a time-aware acquisition system. Neuroimage 2006, 29, 1278–1293. [Google Scholar] [CrossRef]
- Espinoza-Cuadros, F.; Fernandez-Pozo, R.; Toledano, D.T.; Alcazar-Ramirez, J.D.; Lopez-Gonzalo, E.; Hernandez-Gomez, L.A. Reviewing the connection between speech and obstructive sleep apnea. Biomed. Eng. Online 2016, 15, 20. [Google Scholar] [CrossRef] [Green Version]
- Sazonov, E.S.; Makeyev, O.; Schuckers, S.; Lopez-Meyer, P.; Melanson, E.L.; Neuman, M.R. Automatic detection of swallowing events by acoustical means for applications of monitoring of ingestive behavior. IEEE Trans. Biomed. Eng. 2010, 57, 626–633. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Andre, A.E. Emotion recognition based on physiological changes in music listening. IEEE Trans. Pattern Anal. Mach. Intell. 2008, 30, 2067–2083. [Google Scholar] [CrossRef] [PubMed]
- Reinhardt, B.; Leistritz, L.; Faenger, B.; Hansen, E.; Scholle, H.C.; Muller, A. EMG analysis of the thenar muscles as a model for EMG-triggered larynx stimulation. Biomed. Technol. 2007, 52, 122–125. [Google Scholar] [CrossRef] [PubMed]
- Zhong, T.; Kindem, J.M.; Rochman, J.; Faraon, A. Interfacing broadband photonic qubits to on-chip cavity-protected rare-earth ensembles. Nat. Commun. 2017, 8, 14107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minges, K.E.; Herrin, J.; Fiorilli, P.N.; Curtis, J.P. Development and validation of a simple risk score to predict 30-day readmission after percutaneous coronary intervention in a cohort of medicare patients. Catheter. Cardiovasc. Interv. 2017, 89, 955–963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuzniewicz, M.W.; Puopolo, K.M.; Fischer, A.; Walsh, E.M.; Li, S.; Newman, T.B.; Kipnis, P.; Escobar, G.J. A Quantitative, Risk-Based Approach to the Management of Neonatal Early-Onset Sepsis. JAMA Pediatr. 2017, 171, 365–371. [Google Scholar] [CrossRef]
- Li, S.; Kabeer, A.M. Designer Immunotherapy Specific for Cancer. J. Cell Sci. Ther. 2013, 4, e116. [Google Scholar] [CrossRef]
- Li, S.C.; Tachiki, L.M.; Luo, J.; Dethlefs, B.A.; Chen, Z.; Loudon, W.G. A biological global positioning system: Considerations for tracking stem cell behaviors in the whole body. Stem Cell Rev. 2010, 6, 317–333. [Google Scholar] [CrossRef] [Green Version]
- Li, S.C.; Kabeer, M.H. Spatiotemporal switching signals for cancer stem cell activation in pediatric origins of adulthood cancer: Towards a watch-and-wait lifetime strategy for cancer treatment. World J. Stem Cells 2018, 10, 15–22. [Google Scholar] [CrossRef]
| Technology of Medical Measurement | Evidence-Based Wellness and Maintenance | Disease-Centric Parameters of Personalized Strategies | References |
|---|---|---|---|
| Hypoxia | hypoxia-inducible factors (HIFs). | hypoxia-ischemia | [19] |
| Local/regional hypoxia | Hippocampus | CA3 pyramidal neurons | [6] |
| Whole-body hypoxia | Heart functions | myocardial infarction | [4] |
| Breathing patterns | Non-Invasive Stretchable and Wearable Respiratory Rate Sensor for respiration rate | [32] | |
| e-Health nasal sensor (consists of a passive and non-invasive single-lead electrocardiogram (ECG) acquisition module and an ECG-derived respiratory (EDR) algorithm in the working prototype of a mobile application) | [33] | ||
| Nose breathing vs. mouth breathing (correlations between mouth breathing and cognition show that decreased oxygen saturation during mouth breathing results not only in morphological deformations but also in poor learning outcomes) | [34] | ||
| Heartbeat/pulse patterns | Flattening of the flow velocity (pulse) patterns correlates with the local severity of arteriosclerotic disease | [35] | |
| Preventive medicine using pulse oximetry screening | [36] | ||
| Pulse transit time (PTT) is the time it takes a pulse wave to travel between two arterial sites (R-wave-gated photo-plethysmography (RWPP) as of measurement of PTT as a surrogate for intra-thoracic pressure changes in obstructive sleep apnea) | [37] | ||
| Pulse Oximetry Screening for Critical Congenital Heart Defects | [38] | ||
| AI-Medicine algorithm | |||
| Algorithm to track changes in cardiorespiratory interactions (heartbeat intervals and respiratory recordings under dynamic breathing patterns) | [39] | ||
| Respiratory sinus arrhythmia (RSA) with algorithm for quantifying instantaneous RSA as applied to heartbeat interval and respiratory recordings in order to track changes in cardiorespiratory interactions elicited during meditation, otherwise not evidenced in control resting states) | [40] | ||
| Tongue is a critical organ for respiration and speech | [41] | ||
| 18 voice features with posttraumatic stress disorder | [42] | ||
| Breathing pattern parameters: Peak airway pressure (Pawpeek), mean airway pressure (Pawmean), tidal volume (VT, mL/kg), minute volume (MV), respiratory muscle unloading (peak electricity of diaphragm (EAdipeak), P 0.1, VT/EAdi), clinical outcomes (ICU mortality, duration of ventilation days, ICU stay time, hospital stay time | [43] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Su, Q.; Loudon, W.G.; Lee, K.L.; Luo, J.; Dethlefs, B.A.; Li, S.C. Breathing Signature as Vitality Score Index Created by Exercises of Qigong: Implications of Artificial Intelligence Tools Used in Traditional Chinese Medicine. J. Funct. Morphol. Kinesiol. 2019, 4, 71. https://doi.org/10.3390/jfmk4040071
Zhang J, Su Q, Loudon WG, Lee KL, Luo J, Dethlefs BA, Li SC. Breathing Signature as Vitality Score Index Created by Exercises of Qigong: Implications of Artificial Intelligence Tools Used in Traditional Chinese Medicine. Journal of Functional Morphology and Kinesiology. 2019; 4(4):71. https://doi.org/10.3390/jfmk4040071
Chicago/Turabian StyleZhang, Junjie, Qingning Su, William G. Loudon, Katherine L. Lee, Jane Luo, Brent A. Dethlefs, and Shengwen Calvin Li. 2019. "Breathing Signature as Vitality Score Index Created by Exercises of Qigong: Implications of Artificial Intelligence Tools Used in Traditional Chinese Medicine" Journal of Functional Morphology and Kinesiology 4, no. 4: 71. https://doi.org/10.3390/jfmk4040071
APA StyleZhang, J., Su, Q., Loudon, W. G., Lee, K. L., Luo, J., Dethlefs, B. A., & Li, S. C. (2019). Breathing Signature as Vitality Score Index Created by Exercises of Qigong: Implications of Artificial Intelligence Tools Used in Traditional Chinese Medicine. Journal of Functional Morphology and Kinesiology, 4(4), 71. https://doi.org/10.3390/jfmk4040071






