Retraining in a Female Elite Rower with Persistent Symptoms Post-Arthroscopy for Femoroacetabular Impingement Syndrome: A Proof-of-Concept Case Report
Abstract
:1. Introduction
2. Case Description and Methods
2.1. Participant Details
2.2. Outcome Measures
2.2.1. Identifying Movement Impairments: The Foundation Matrix Test Battery
2.2.2. Retraining Programme
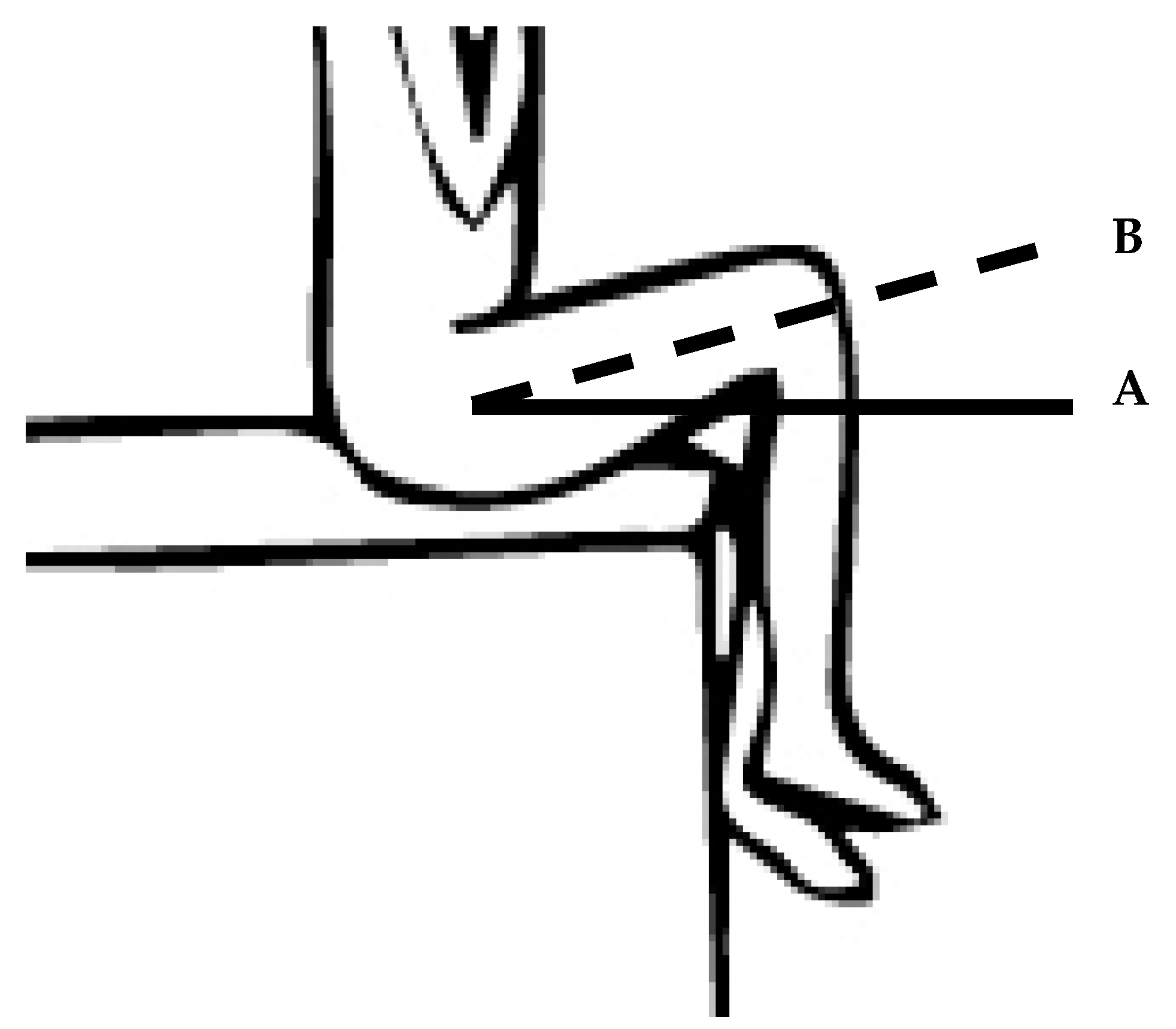
2.2.3. Identifying Movement Control Impairments: Movement Control Test with Motion Analysis during Seated Hip Flexion
3. Results
3.1. Clinical Assessment and Movement Control Assessment
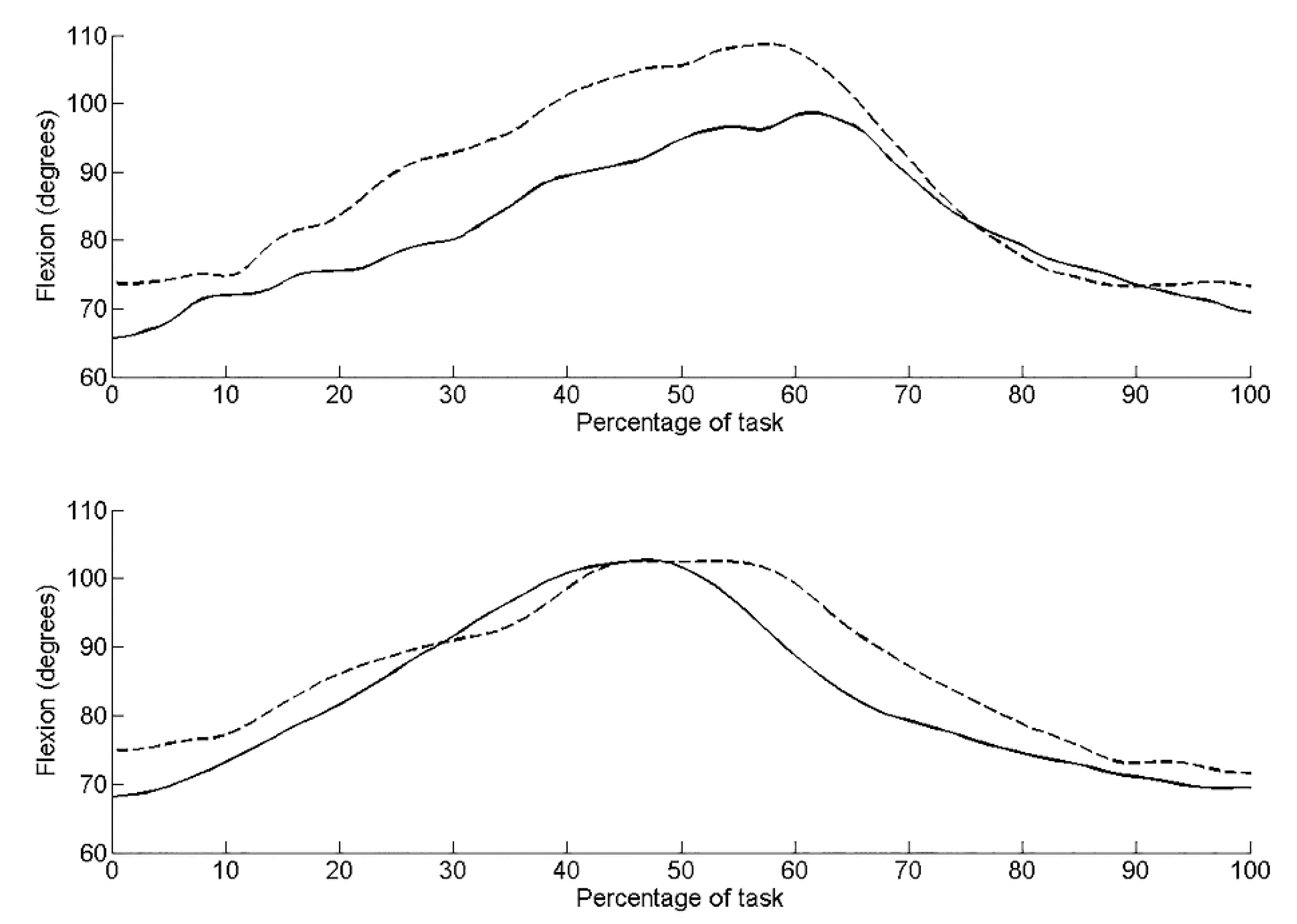
3.2. Kinematic Findings During Seated Hip Flexion Control Test
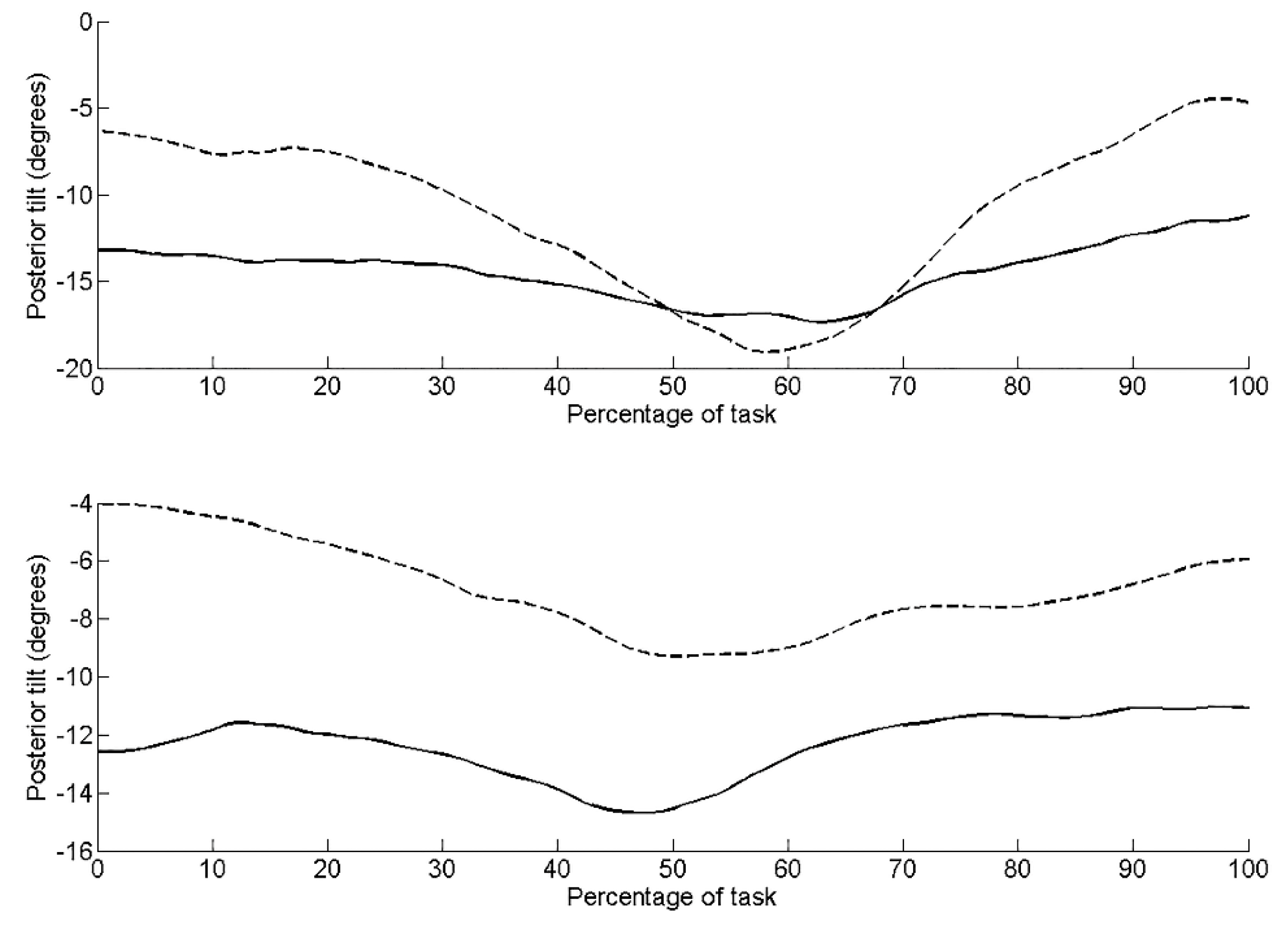
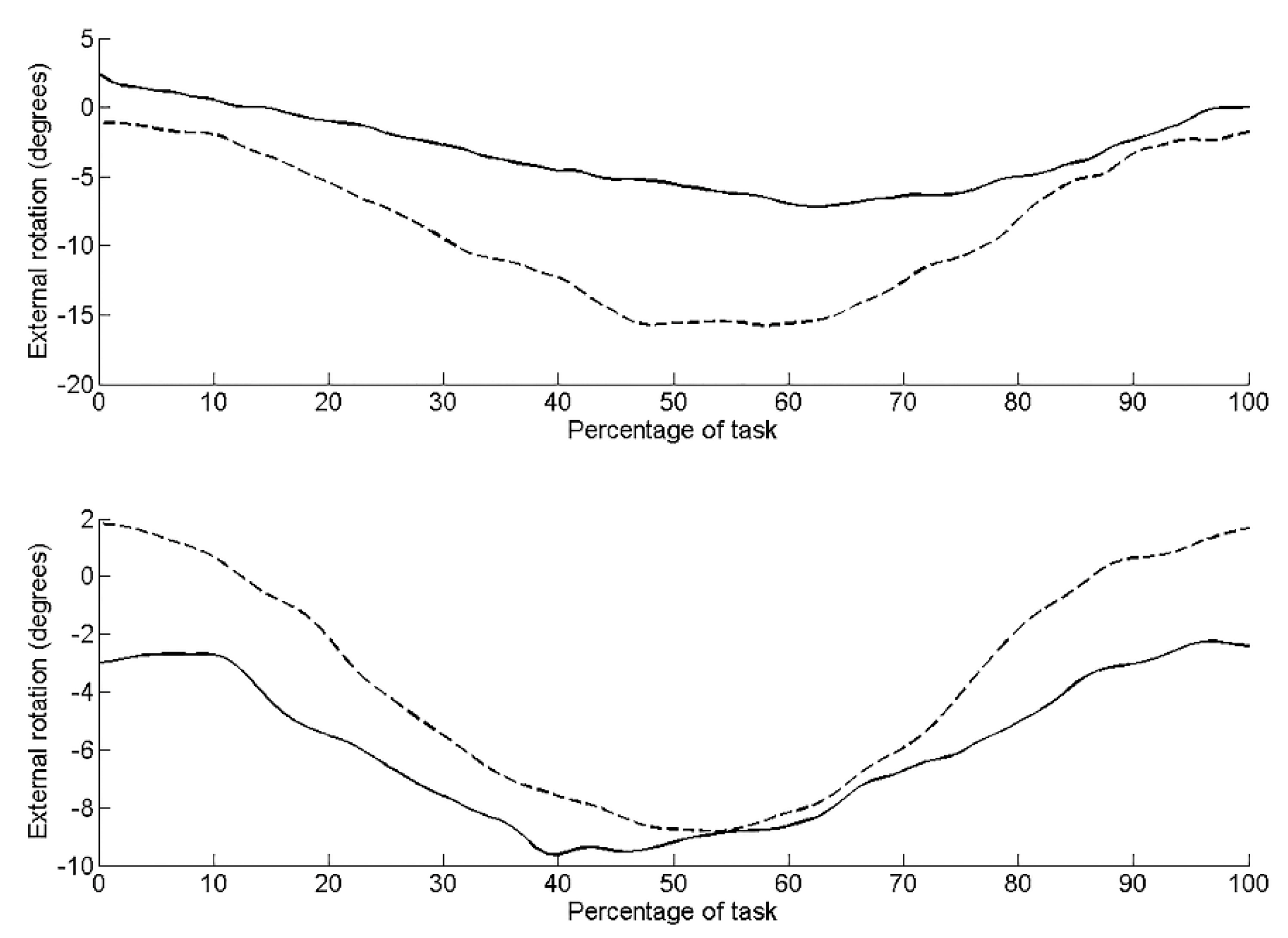
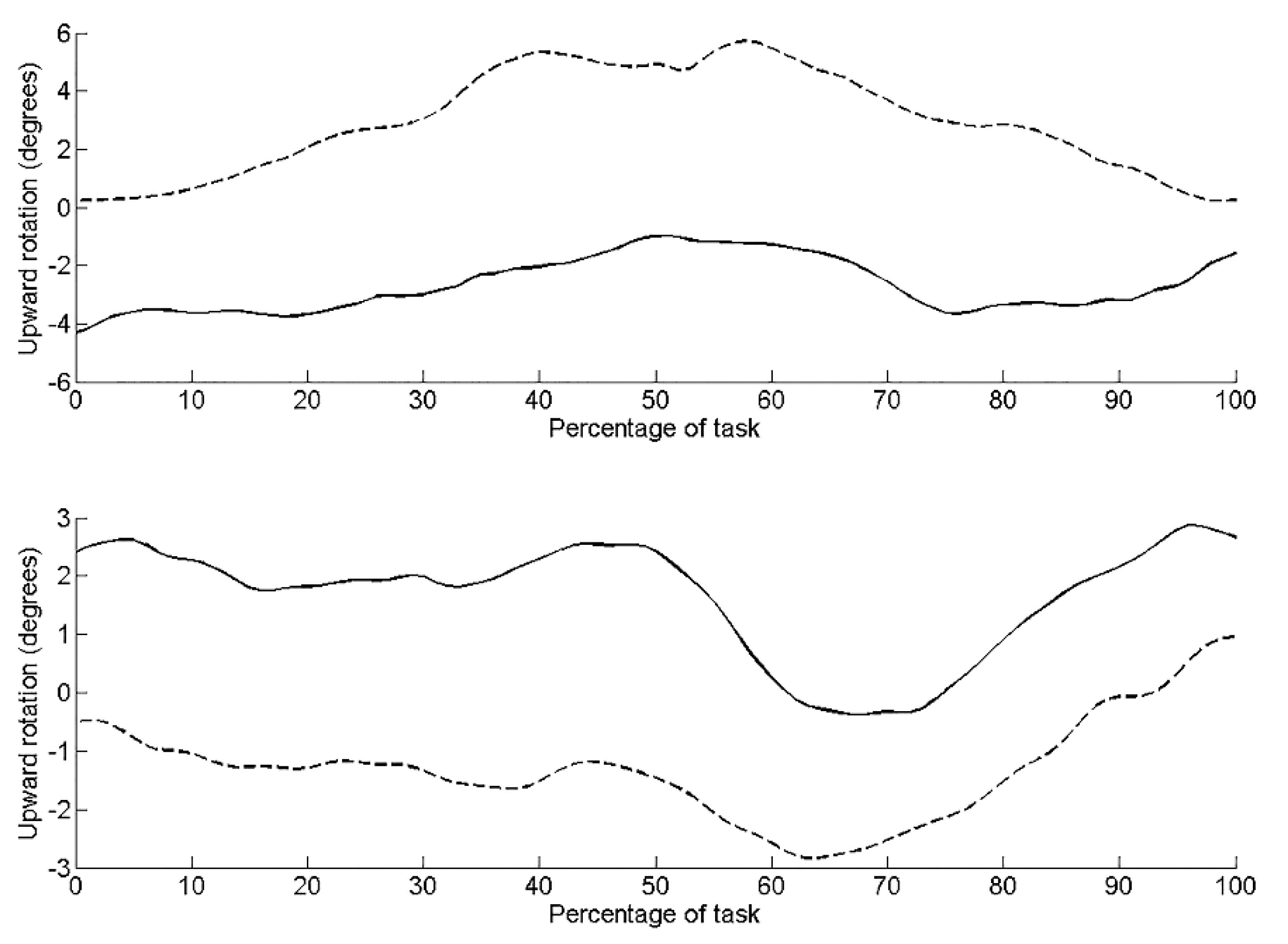
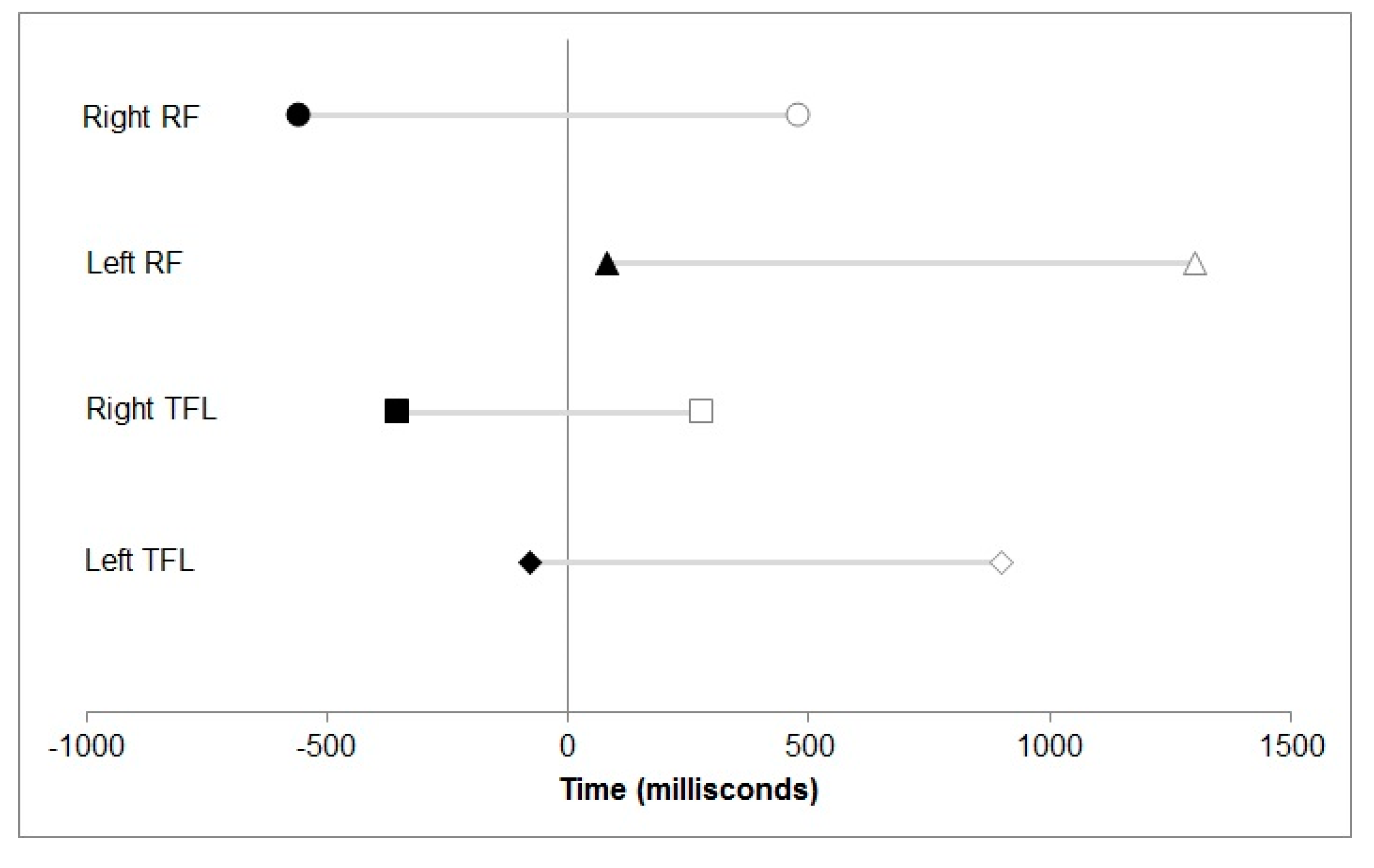
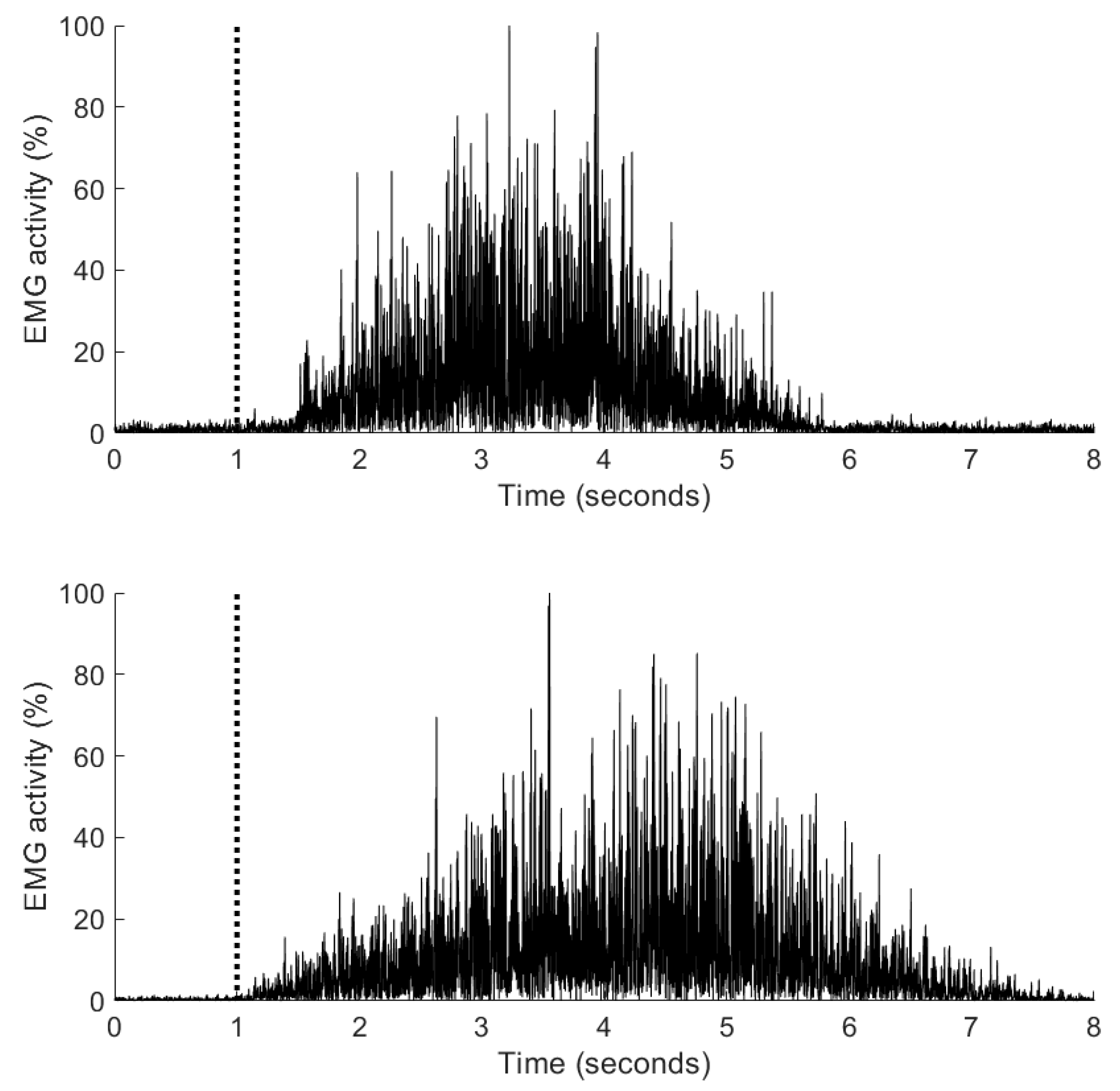
3.3. Muscle Activation Onset
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Higher Priority | Lower Priority | Assets: |
|---|---|---|
| Low threshold: alignment and coordination | ||
| Shoulder Anterior Tilt (Left) Shoulder Drop (Left) Shoulder Winging (Left–Right) Low Back/Pelvis Rotation (Left) Low Back/Pelvis Sidebend (Right) Hip Rotation Medial (Right) Hip Anterior Translation (Left) Foot Inversion (Right) Foot Pronation (Left–Right) | None | Upper Back Lower leg |
| High threshold: strength and speed | ||
| Shoulder Drop (Left–Right) Shoulder Forward Glide (Left–Right) Shoulder Hitch (Right) Shoulder Tilt (Left–Right) Low Back/Pelvis Extension Low Back/Pelvis Rotation (Right) Low Back/Pelvis Sidebend (Left–Right) Foot Inversion (Left–Right) Foot Pronation (Left–Right) | None | Upper Back Hip Lower Leg |
Appendix B
| Higher Priority | Lower Priority | Assets: |
|---|---|---|
| Low threshold: alignment and coordination | ||
| None | Shoulder Anterior Tilt (Left) Shoulder Winging (Left–Right) Foot Inversion (Right) | Upper Back Low Back/Pelvis Hip Lower Leg |
| High threshold: strength and speed | ||
| Upper Back Rotation (Right) | Shoulder Winging (Left–Right) Shoulder Anterior Tilt (Left–Right) Low Back/Pelvis Sidebend (Right) Hip Rotation-Medial (Left) | Lower Leg Foot |
References
- Griffin, D.R.; Dickenson, E.J.; O’Donnell, J.; Agricola, R.; Awan, T.; Beck, M.; Clohisy, J.C.; Dijkstra, H.P.; Falvey, E.; Gimpel, M.; et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): An international consensus statement. Br. J. Sports Med. 2016, 50, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.A.; Naze, G.S.; Kavchak, A.E.; Paul, D.; Kenison, B.; Hegedus, E.J. Radiological variables associated with progression of femoroacetabular impingement of the hip: A systematic review. J. Sci. Med. Sport 2015, 18, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Agricola, R.; Weinans, H. Femoroacetabular impingement: What is its link with osteoarthritis? Br. J. Sports Med. 2016, 50, 957–958. [Google Scholar] [CrossRef] [PubMed]
- Buckeridge, E.M.; Bull, A.M.; McGregor, A.H. Rowing technique and performance. Scand. J. Med. Sci. Sports 2015, 25, e176–e183. [Google Scholar] [CrossRef] [PubMed]
- Diamond, L.E.; Bennell, K.L.; Wrigley, T.V.; Hinman, R.S.; Hall, M.; O’Donnell, J.; Hodges, P.W. Trunk, pelvis and hip biomechanics in individuals with femoroacetabular impingement syndrome: Strategies for step ascent. Gait Posture 2018, 61, 176–182. [Google Scholar] [CrossRef] [PubMed]
- King, M.G.; Lawrenson, P.R.; Semciw, A.I.; Middleton, K.J.; Crossley, K.M. Lower limb biomechanics in femoroacetabular impingement syndrome: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 566–580. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.R.; Nepple, J.J.; Philippon, M.J.; Kelly, B.T.; Larson, C.M.; Bedi, A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am. J. Sports Med. 2014, 42, 2402–2409. [Google Scholar] [CrossRef]
- Van Houcke, J.; Pattyn, C.; Vanden Bossche, L.; Redant, C.; Maes, J.W.; Audenaert, E.A. The pelvifemoral rhythm in cam-type femoroacetabular impingement. Clin. Biomech. (Bristol. Avon) 2014, 29, 63–67. [Google Scholar] [CrossRef]
- Freke, M.D.; Kemp, J.; Svege, I.; Risberg, M.A.; Semciw, A.; Crossley, K.M. Physical impairments in symptomatic femoroacetabular impingement: A systematic review of the evidence. Br. J. Sports Med. 2016, 50, 1180. [Google Scholar] [CrossRef]
- Lawrenson, P.R.; Crossley, K.M.; Vicenzino, B.T.; Hodges, P.W.; James, G.; Croft, K.J.; King, M.G.; Semciw, A.I. Muscle size and composition in people with articular hip pathology: A systematic review with meta-analysis. Osteoarthr. Cartil. 2019, 27, 181–195. [Google Scholar] [CrossRef]
- Mendis, M.D.; Wilson, S.J.; Hayes, D.A.; Watts, M.C.; Hides, J.A. Hip flexor muscle size, strength and recruitment pattern in patients with acetabular labral tears compared to healthy controls. Man. Ther. 2014, 19, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Diamond, L.E.; Van den Hoorn, W.; Bennell, K.L.; Wrigley, T.V.; Hinman, R.S.; O’Donnell, J.; Hodges, P.W. Coordination of deep hip muscle activity is altered in symptomatic femoroacetabular impingement. J. Orthop. Res. 2017, 35, 1494–1504. [Google Scholar] [CrossRef] [PubMed]
- Liew, B.X.W.; Vecchio, A.D.; Falla, D. The influence of musculoskeletal pain disorders on muscle synergies—A systematic review. PLoS ONE 2018, 13, e0206885. [Google Scholar] [CrossRef] [PubMed]
- Wall, P.D.; Fernandez, M.; Griffin, D.R.; Foster, N.E. Nonoperative treatment for femoroacetabular impingement: A systematic review of the literature. PM R 2013, 5, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.R.; Dickenson, E.J.; Wall, P.D.H.; Achana, F.; Donovan, J.L.; Griffin, J.; Hobson, R.; Hutchinson, C.E.; Jepson, M.; Parsons, N.R.; et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): A multicentre randomised controlled trial. Lancet 2018, 391, 2225–2235. [Google Scholar] [CrossRef]
- Palmer, A.; Ayyar, G.; Fernquest, S.; Rombach, I.; Dutton, S.; Mansour, R.; Wood, S.; Khanduja, V.; Pollard, T.C.B.; McCaskie, A.W.; et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: Multicentre randomised controlled trial. BMJ 2019, 364, 1185. [Google Scholar] [CrossRef]
- Mansell, N.S.; Rhon, D.I.; Meyer, J.; Slevin, J.M.; Marchant, B.G. Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: A randomized controlled trial with 2-Year follow-up. Am. J. Sports Med. 2018, 46, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Wall, P.D.; Dickenson, E.J.; Robinson, D.; Hughes, I.; Realpe, A.; Hobson, R.; Griffin, D.R.; Foster, N.E. Personalised Hip Therapy: Development of a non-operative protocol to treat femoroacetabular impingement syndrome in the FASHIoN randomized controlled trial. Br. J. Sports Med. 2016, 50, 1217–1223. [Google Scholar] [CrossRef]
- Ford, K.R.; Nguyen, A.-D.; Dischiavi, S.L.; Hegedus, E.J.; Zuk, E.F.; Taylor, J.B. An evidence-based review of hip-focused neuromuscular exercise interventions to address dynamic lower extremity valgus. Open Access J. Sports Med. 2015, 6, 291–303. [Google Scholar] [CrossRef]
- Skou, S.T.; Roos, E.M. Good Life with osteoArthritis in Denmark (GLA:D™): Evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord. 2017, 18, 72. [Google Scholar] [CrossRef]
- Kemp, J.L.; King, M.G.; Barton, C.; Schache, A.G.; Thorborg, K.; Roos, E.M.; Scholes, M.; Grimaldi, A.; Semciw, A.I.; Freke, M.; et al. Is exercise therapy for femoroacetabular impingement in or out of FASHIoN? We need to talk about current best practice for the non-surgical management of FAI syndrome. Br. J. Sports Med. 2019. [Google Scholar] [CrossRef] [PubMed]
- Falla, D.; Hodges, P.W. Individualized Exercise Interventions for Spinal Pain. Exerc. Sport Sci. Rev. 2017, 45, 105–115. [Google Scholar] [CrossRef]
- Dingenen, B.; Blandford, L.; Comerford, M.; Staes, F.; Mottram, S. The assessment of movement health in clinical practice: A multidimensional perspective. Phys. Ther. Sport 2018, 32, 282–292. [Google Scholar] [CrossRef]
- Comerford, M.; Mottram, S. Kinetic Control: The Management of Uncontrolled Movement, 1st ed.; Elsevier: Churchill Livingstone, Australia, 2012. [Google Scholar]
- Comerford, M.; Mottram, S. Functional stability re-training: Principles and strategies for managing mechanical dysfunction. Man Ther. 2001, 6, 3–14. [Google Scholar] [CrossRef] [PubMed]
- McNeill, W.; Blandford, L. Movement Health. J. Bodyw. Mov. Ther. 2015, 19, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Mischiati, C.; Comerford, M.; Gosford, E.; Swart, J.; Ewings, S.; Botha, N.; Stokes, M.; Mottram, S. Intra and Inter-Rater Reliability of Screening for Movement Impairments: Movement Control Tests from the Foundation Matrix. J. Sports Sci. Med. 2015, 14, 427–440. [Google Scholar] [PubMed]
- Thorborg, K.; Roos, E.M.; Bartels, E.M.; Petersen, J.; Holmich, P. Validity, reliability and responsiveness of patient-reported outcome questionnaires when assessing hip and groin disability: A systematic review. Br. J. Sports Med. 2010, 44, 1186–1196. [Google Scholar] [CrossRef] [PubMed]
- Thorborg, K.; Holmich, P.; Christensen, R.; Petersen, J.; Roos, E.M. The Copenhagen Hip and Groin Outcome Score (HAGOS): Development and validation according to the COSMIN checklist. Br. J. Sports Med. 2011, 45, 478–491. [Google Scholar] [CrossRef]
- Croft, P.R.; Nahit, E.S.; Macfarlane, G.J.; Silman, A.J. Interobserver reliability in measuring flexion, internal rotation, and external rotation of the hip using a plurimeter. Ann. Rheum. Dis. 1996, 55, 320–323. [Google Scholar] [CrossRef]
- McNeill, W. The Double Knee Swing Test—a practical example of The Performance Matrix Movement Screen. J. Bodyw. Mov. Ther. 2014, 477–481. [Google Scholar] [CrossRef]
- Fitts, P.; Posner, M. Human Performance; Brooks/Cole: Belmont, TN, USA, 1967. [Google Scholar]
- Bernstein, N. The Coordination and Regulation of Movements; Pergamon Press: Oxford, UK, 1967. [Google Scholar]
- Van Ginneken, W.; Poolton, J.; Capio, C.; van der Kamp, J.; Choi, C.; Masters, R. Conscious control is associated with freezing of mechanical degrees of freedom during motor learning. J. Mot. Behav. 2018, 50, 436–456. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.B.; Ounpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Hodges, P.W.; Bui, B.H. A comparison of computer-based methods for the determination of onset of muscle contraction using electromyography. Electroencephalogr. Clin. Neurophysiol. 1996, 101, 511–519. [Google Scholar] [PubMed]
- Thorborg, K.; Kraemer, O.; Madsen, A.-D.; Hölmich, P. Patient-reported outcomes within the first year after hip arthroscopy and rehabilitation for femoroacetabular impingement and/or labral injury: The difference between getting better and getting back to normal. J. Sports Med. 2018, 46, 2607–2614. [Google Scholar] [CrossRef] [PubMed]
- Thorborg, K.; Branci, S.; Stensbirk, F.; Jensen, J.; Hölmich, P. Copenhagen hip and groin outcome score (HAGOS) in male soccer: Reference values for hip and groin injury-free players. Br. J. Sports Med. 2014, 48, 557–559. [Google Scholar] [CrossRef]
- Struyf, F.; Nijs, J.; Mollekens, S.; Jeurissen, I.; Truijen, S.; Mottram, S.; Meeusen, R. Scapular-focused treatment in patients with shoulder impingement syndrome: A randomized clinical trial. Clin. Rheumatol. 2013, 32, 73–85. [Google Scholar] [CrossRef]
- Worsley, P.; Warner, M.; Mottram, S.; Gadola, S.; Veeger, H.E.; Hermens, H.; Morrissey, D.; Little, P.; Cooper, C.; Carr, A.; et al. Motor control retraining exercises for shoulder impingement: Effects on function, muscle activation, and biomechanics in young adults. J. Shoulder Elb. Surg. 2013, 22, e11–e19. [Google Scholar] [CrossRef]
- Noyes, F.R.; Barber-Westin, S.D.; Smith, S.T.; Campbell, T.; Garrison, T.T. A training program to improve neuromuscular and performance indices in female high school basketball players. J. Strength Cond. Res. 2012, 26, 709–719. [Google Scholar] [CrossRef]
- Peck, K.Y.; DiStefano, L.J.; Marshall, S.W.; Padua, D.A.; Beutler, A.I.; de la Motte, S.J.; Frank, B.S.; Martinez, J.C.; Cameron, K.L. Effect of a Lower Extremity Preventive Training Program on Physical Performance Scores in Military Recruits. J. Strength Cond. Res. 2017, 31, 3146–3157. [Google Scholar] [CrossRef]
- Beck, M.; Leunig, M.; Parvizi, J.; Boutier, V.; Wyss, D.; Ganz, R. Anterior femoroacetabular impingement: Part II. Midterm results of surgical treatment. Clin. Orthop. Relat. Res. 2004, 67–73. [Google Scholar] [CrossRef]
- Wilson, D.A.; Booysen, N.; Dainese, P.; Hekker, M.O.; Stokes, M.; Warner, M.B. Accuracy of movement quality screening to document effects of neuromuscular control retraining exercise in a young ex-footballer with hip and groin symptoms: A proof of concept case study. Med. Hypotheses 2018, 120, 116–120. [Google Scholar] [CrossRef] [PubMed]
| Category | Pre-Intervention | Post-ntervention |
|---|---|---|
| Pain | 53 | 93 |
| Symptoms | 61 | 96 |
| Physical function, daily living | 65 | 100 |
| Function, sports and recreational activities | 56 | 100 |
| Participation in physical activities | 13 | 75 |
| Quality of life | 32 | 85 |
| Pre-intervention (left) | Pelvic tilt | 1.74 |
| Pelvic lat tilt | 0.87 | |
| Hip flexion | 2.65 | |
| Hip internal rotation | 1.66 | |
| Post-intervention (left) | Pelvic tilt | 1.57 |
| Pelvic lat tilt | 1.40 | |
| Hip flexion | 1.49 | |
| Hip internal rotation | 1.67 | |
| Pre-intervention (right) | Pelvic tilt | 1.43 |
| Pelvic lat tilt | 0.71 | |
| Hip flexion | 2.94 | |
| Hip internal rotation | 1.01 | |
| Post-intervention (right) | Pelvic tilt | 0.95 |
| Pelvic lat tilt | 0.87 | |
| Hip flexion | 3.64 | |
| Hip internal rotation | 1.06 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mottram, S.; Warner, M.; Booysen, N.; Bahain-Steenman, K.; Stokes, M. Retraining in a Female Elite Rower with Persistent Symptoms Post-Arthroscopy for Femoroacetabular Impingement Syndrome: A Proof-of-Concept Case Report. J. Funct. Morphol. Kinesiol. 2019, 4, 24. https://doi.org/10.3390/jfmk4020024
Mottram S, Warner M, Booysen N, Bahain-Steenman K, Stokes M. Retraining in a Female Elite Rower with Persistent Symptoms Post-Arthroscopy for Femoroacetabular Impingement Syndrome: A Proof-of-Concept Case Report. Journal of Functional Morphology and Kinesiology. 2019; 4(2):24. https://doi.org/10.3390/jfmk4020024
Chicago/Turabian StyleMottram, Sarah, Martin Warner, Nadine Booysen, Katie Bahain-Steenman, and Maria Stokes. 2019. "Retraining in a Female Elite Rower with Persistent Symptoms Post-Arthroscopy for Femoroacetabular Impingement Syndrome: A Proof-of-Concept Case Report" Journal of Functional Morphology and Kinesiology 4, no. 2: 24. https://doi.org/10.3390/jfmk4020024
APA StyleMottram, S., Warner, M., Booysen, N., Bahain-Steenman, K., & Stokes, M. (2019). Retraining in a Female Elite Rower with Persistent Symptoms Post-Arthroscopy for Femoroacetabular Impingement Syndrome: A Proof-of-Concept Case Report. Journal of Functional Morphology and Kinesiology, 4(2), 24. https://doi.org/10.3390/jfmk4020024





