Effects of a Multicomponent Periodized Program in Kinematic and Muscle Activity Characteristics Related to Anterior Cruciate Ligament Injury Mechanism in College Football Players—A Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
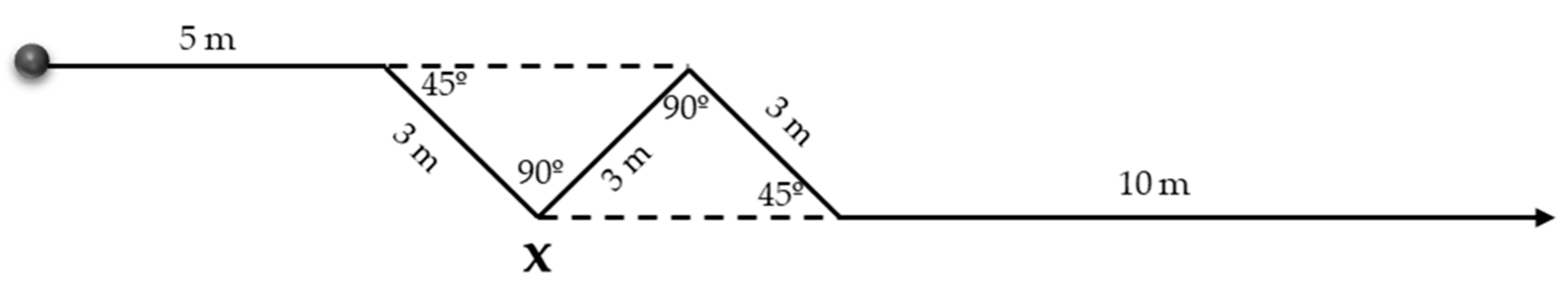
2.3. Procedure
2.4. Sensor Placement
2.5. Intervention Period—12-Week Multicomponent Periodized Program
2.6. Data Analysis
2.7. Sample Size
2.8. Statistical Analysis
3. Results
| Total (n = 35) | Intervention Group (n = 17) | Control Group (n = 18) | ||
|---|---|---|---|---|
| Age (years) | 15.50 ± 1.22 | 15.29 ± 1.16 | 15.70 ± 1.27 | |
| Height (cm) | 164.67 ± 6.47 | 165.96 ± 5.90 | 163.37 ± 7.05 | |
| Weight (Kg) | Pre | 58.83 ± 6.08 | 57.23 ± 4.59 | 60.43 ± 7.57 |
| Post | 58.46 ± 6.92 | 56.55 ± 5.90 | 60.38 ± 7.94 | |
| Limb Dominance (Right/Left) | 33/2 | 17/0 | 16/2 | |
| Football Experience (years) | 7.47 ± 1.15 | 7.31 ± 1.14 | 7.62 ± 1.15 | |
3.1. Kinematic Analysis Findings
| PRE—Intervention | POST—Intervention | p-Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||||||||
| DL | NDL | DL | NDL | DL | NDL | DL | NDL | ||||
| Mean ± Standard Deviation | Group * Time | Limb Dom * Time | Three-Way Interaction Effect | ||||||||
| Variables Angular Velocity (°/s) | |||||||||||
| Sagittal Plane | |||||||||||
| Thigh Extension | −411.48 ± 93.96 | −371.94 ± 108.07 | −372.98 ± 97.44 | −416.20 ± 66.06 | −343.09 ± 89.08 | −354.41 ± 58.25 | −370.26 ± 90.12 | −367.02 ± 79.94 | 0.563 | 0.021 * | 0.100 |
| ROM Thigh Sagittal | 619.19 ± 164.63 | 503.77 ± 136.82 | 640.71 ± 123.78 | 802.91 ± 241.33 | 554.06 ± 128.95 | 541.26 ± 140.35 | 651.36 ± 192.79 | 645.53 ± 241.23 | 0.320 | 0.585 | 0.025 * |
| Coronal Plane | |||||||||||
| Thigh Varus/Abd | 228.21 ± 136.64 | 178.56 ± 107.91 | 260.95 ± 129.68 | 270.16 ± 125.84 | 175.06 ± 87.90 | 190.29 ± 118.18 | 219.12 ± 102.56 | 200.84 ± 113.94 | 0.377 | 0.581 | 0.242 |
| ROM Thigh Coronal | 434.81 ± 202.76 | 371.52 ± 167.96 | 491.34 ± 196.53 | 486.34 ± 158.10 | 345.22 ± 114.74 | 315.97 ± 133.25 | 417.75 ± 195.54 | 416.66 ± 183.92 | 0.987 | 0.396 | 0.795 |
| Transverse Plane | |||||||||||
| Shank Internal Rotation | 519.46 ± 155.96 | 438.30 ± 197.74 | 512.17 ± 221.36 | 568.96 ± 271.85 | 441.06 ± 191.96 | 372.73 ± 151.55 | 632.78 ± 300.90 | 481.96 ± 223.89 | 0.235 | 0.460 | 0.141 |
3.2. Muscle Activity Analysis Findings
| PRE—Intervention | POST—Intervention | Wilcoxon p-Value (PRE—POST) | Effect Size d Cohen (PRE—POST) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Mann Whitney U | Effect Size d Cohen | Intervention | Control | Mann Whitney U | Effect Size d Cohen | |||||||||||||
| DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | |||||
| Median [Interquartile Range [Q1, Q3] | Intervention Related Samples Analyses | Control Related Samples Analyses | Intervention Related Samples Analyses | Control Related Samples Analyses | ||||||||||||||||
| Variables Angular Velocity (°/s) | ||||||||||||||||||||
| Sagittal Plane | ||||||||||||||||||||
| Thigh Flexion | 188.33 [90.69, 323.76] | 144.06 [67.54, 175.93] | 267.02 [170.31, 360.21] | 375.45 [191.97, 575.66] | 0.318 | 0.000 * | −1.62 † | 6.69 † | 222.17 [146.82, 274.83] | 173.98 [78.86, 303.44] | 286.35 [138.26, 412.08] | 213.20 [139.41, 430.26] | 0.173 | 0.273 | 2.13 † | 2.10 † | DL: 0.653 NDL: 0.124 | DL: 0.349 NDL: 0.085 | DL: 0.05 NDL: 2.38 † | DL: 0.38 NDL: 2.08 † |
| Shank Extension | −158.87 [−305.97, −45.26] | −140.63 [−248.83, 30.78] | −66.76 [−150.55, −23.09] | −53.84 [−108.92, 0.17] | 0.144 | 0.403 | −1.62 † | 1.57 † | −176.44 [−345.17, −102.29] | −153.94 [−304.39, −41.63] | −41.03 [−98.31, 36.92] | 3.73 [−129.90, 45.83] | 0.008 * | 0.019 * | 2.60 † | 1.42 † | DL: 0.469 NDL: 0.679 | DL: 0.396 NDL: 0.215 | DL: 0.92 NDL: 0.66 | DL: 0.28 NDL: 0.29 |
| Shank Flexion | 631.67 [552.42, 762.21] | 543.08 [463.61, 714.58] | 487.25 [404.33, 677.64] | 626.43 [483.73, 727.82] | 0.959 | 0.027 * | 3.14 † | 1.10 † | 617.69 [506.00, 898.83] | 666.72 [567.76, 929.40] | 512.74 [404.97, 636.21] | 483.38 [404.54, 602.36] | 0.027 * | 0.011 * | 3.90 † | 2.78 † | DL: 0.836 NDL: 0.017 * | DL: 0.647 NDL: 0.122 | DL: 0.42 NDL: 3.04 † | DL: 0.85 NDL: 1.20 † |
| ROM Shank Sagittal | 842.77 [612.61, 1141.90] | 698.16 [450.97, 956.79] | 546.81 [477.07, 784.80] | 643.83 [506.10, 786.20] | 0.187 | 0.695 | 2.84 † | 0.24 | 784.35 [625.18, 1118.16] | 820.66 [567.62, 1232.52] | 502.79 [406.37, 698.93] | 442.90 [366.29, 768.80] | 0.005 * | 0.019 * | 3.75 † | 2.19 † | DL: 0.535 NDL: 0.109 | DL: 0.557 NDL: 0.078 | DL: 0.76 NDL: 2.08 † | DL: 0.64 NDL: 0.50 |
| Coronal Plane | ||||||||||||||||||||
| Thigh Valgus | −162.31 [−292.84, −130.02] | −167.46 [−245.99, −135.90] | −202.07 [−266.43, −162.50] | −214.72 [−264.86, −162.22] | 0.303 | 0.258 | 1.03 † | 0.98 | −153.86 [−216.75, −129.09] | −124.80 [−163.15, −100.45] | −158.56 [−200.94, −115.53] | −197.91 [−259.17, −121.60] | 1.000 | 0.008 * | 1.07 † | 4.30 † | DL: 0.246 NDL: 0.025 * | DL: 0.122 NDL: 0.711 | DL: 1.65 † NDL: 3.81 † | DL: 1.10 † NDL: 0.02 |
| Shank Valgus | −387.44 [−466.28, −216.66] | −257.58 [−395.05, −180.16] | −254.53 [−391.80, −157.22] | −287.05 [−411.14, −201.79] | 0.022 * | 0.695 | 2.31 † | 0.68 | −266.01 [−406.42, −184.66] | −174.69 [−319.93, −145.55] | −216.89 [−293.05, −119.38] | −170.27 [−306.65, −91.40] | 0.245 | 0.568 | 1.25 † | 0.25 | DL: 0.501 NDL: 0.134 | DL: 0.306 NDL: 0.078 | DL: 0.94 NDL: 1.19 † | DL: 0.40 NDL: 1.93 † |
| Shank Varus | 389.33 [249.25, 697.08] | 245.07 [174.75, 307.50] | 256.33 [209.80, 308.46] | 255.11 [236.53, 391.75] | 0.020 * | 0.251 | 3.70 † | 1.64 † | 398.97 [273.07, 509.85] | 358.59 [230.03, 536.36] | 277.35 [144.60, 378.08] | 232.08 [180.34, 349.75] | 0.022 * | 0.096 | 3.00 † | 1.11 † | DL: 0.642 NDL: 0.013 * | DL: 0.913 NDL: 0.372 | DL: 0.83 NDL: 3.13 † | DL: 0.03 NDL: 0.32 |
| ROM Shank Coronal | 754.27 [468.27, 944.63] | 436.92 [374.21, 707.55] | 552.00 [390.02, 662.97] | 682.15 [456.80, 764.81] | 0.030 * | 0.211 | 3.46 † | 1.42 ◊ | 592.03 [527.55, 995.34] | 544.13 [371.76, 813.52] | 425.36 [268.73, 708.48] | 409.67 [290.07, 604.89] | 0.029 * | 0.110 | 2.26 † | 0.81 | DL: 0.469 NDL: 0.642 | DL: 0.500 NDL: 0.058 | DL: 1.01 † NDL: 1.32 † | DL: 0.24 NDL: 0.68 |
| Transverse Plane | ||||||||||||||||||||
| Thigh Int Rot | −483.39 [−729.41, −293.17] | −355.65 [−615.18, −262.08] | −360.49 [−509.59, −240.07] | −504.46 [−676.22, −396.81] | 0.232 | 0.195 | 2.29 † | 0.87 | −279.71 [−478.98, −171.26] | −257.63 [−499.43, −171.70] | −328.95 [−510.58, −234.47] | −385.81 [−527.98, −263.31] | 0.424 | 0.134 | 0.59 | 1.80 † | DL: 0.017 * NDL: 0.076 | DL: 0.647 NDL: 0.028 * | DL: 3.04 † NDL: 2.27 † | DL: 0.52 NDL: 2.36 † |
| Thigh Ext Rot | 524.72 [443.35, 799.60] | 399.39 [268.46, 524.53] | 358.95 [258.58, 506.70] | 564.44 [310.06, 614.90] | 0.014 * | 0.126 | 2.87 † | 1.88 † | 373.62 [229.22, 511.09] | 359.34 [269.68, 463.43] | 285.87 [185.29, 537.21] | 406.49 [315.98, 474.26] | 0.832 | 0.386 | 0.09 | 0.58 | DL: 0.010 * NDL: 0.619 | DL: 0.327 NDL: 0.122 | DL: 3.92 † NDL: 0.40 | DL: 0.93 NDL: 1.71 † |
| ROM Thigh Transverse | 1100.97 [781.14, 1373.19] | 853.41 [593.04, 1063.16] | 730.85 [525.73, 1121.73 | 1012.31 [702.57, 1233.77] | 0.959 | 0.211 | 2.86† | 1.68† | 711.71 [418.30, 946.61] | 619.00 [483.08, 909.21] | 668.46 [486.33, 981.02] | 842.64 [643.48, 971.74] | 0.961 | 0.184 | 0.35 | 1.42 † | DL: 0.002 * NDL: 0.014 * | DL: 0.327 NDL: 0.076 | DL: 3.85 † NDL: 1.65 † | DL: 0.87 NDL: 2.35 † |
| Shank Ext Rot | −382.95 [−673.24, −272.65] | −385.12 [−448.65, −216.54] | −440.65 [−707.45, −230.45] | −611.39 [−683.34, −363.50] | 0.959 | 0.027 * | 0.72 | 2.90 † | −320.57 [−617.07, −234.49] | −402.48 [−578.84, −261.21] | −485.96 [−959.60, −292.64] | −493.12 [−566.04, −273.31] | 0.303 | 0.483 | 1.76 † | 1.23 † | DL: 0.438 NDL: 0.438 | DL: 0.472 NDL: 0.420 | DL: 0.33 NDL: 0.93 | DL: 0.81 NDL: 0.75 |
| ROM Shank Transverse | 923.06 [688.65, 1223.11] | 900.56 [509.76, 1009.47] | 972.71 [605.50, 1323.60] | 1090.74 [765.62, 1423.79] | 0.959 | 0.042 * | 0.43 | 2.86 † | 803.81 [543.57, 1218.70] | 730.85 [650.87, 944.61] | 1095.36 [705.99, 1664.09] | 973.91 [693.96, 1146.79] | 0.096 | 0.126 | 2.69 † | 2.26 † | DL: 0.469 NDL: 1.000 | DL: 0.248 NDL: 0.157 | DL: 1.06 † NDL: 0.28 | DL: 1.44 † NDL: 1.34 † |
| PRE—Intervention | POST—Intervention | p-Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||||||||
| DL | NDL | DL | NDL | DL | NDL | DL | NDL | ||||
| Mean ± Standard Deviation | Group*Time | Limb Dom*Time | Three-Way Interaction Effect | ||||||||
| Variables Muscle Activity (% of Maximum) | |||||||||||
| Average Biceps Femoris | 0.12 ± 0.03 | 0.12 ± 0.05 | 0.10 ± 0.04 | 0.12 ± 0.04 | 0.10 ± 0.04 | 0.10 ± 0.07 | 0.10 ± 0.04 | 0.11 ± 0.04 | 0.569 | 0.624 | 0.981 |
| Peak Biceps Femoris | 0.58 ± 0.15 | 0.55 ± 0.18 | 0.48 ± 0.22 | 0.57 ± 0.17 | 0.50 ± 0.18 | 0.41 ± 0.22 | 0.44 ± 0.15 | 0.51 ± 0.15 | 0.389 | 0.528 | 0.699 |
| Average Semitendinosus | 0.13 ± 0.04 | 0.13 ± 0.04 | 0.13 ± 0.04 | 0.12 ± 0.05 | 0.10 ± 0.06 | 0.15 ± 0.06 | 0.11 ± 0.05 | 0.11 ± 0.05 | 0.540 | 0.080 | 0.334 |
| Peak Semitendinosus | 0.56 ± 0.17 | 0.50 ± 0.17 | 0.55 ± 0.16 | 0.55 ± 0.20 | 0.49 ± 0.28 | 0.55 ± 0.17 | 0.49 ± 0.15 | 0.50 ± 0.21 | 0.486 | 0.323 | 0.488 |
| Average Vastus Lateralis | 0.12 ± 0.04 | 0.12 ± 0.04 | 0.12 ± 0.06 | 0.11 ± 0.06 | 0.10 ± 0.04 | 0.11 ± 0.05 | 0.10 ± 0.05 | 0.08 ± 0.05 | 0.447 | 0.645 | 0.571 |
| Peak Vastus Lateralis | 0.50 ± 0.19 | 0.53 ± 0.13 | 0.51 ± 0.18 | 0.49 ± 0.22 | 0.45 ± 0.17 | 0.52 ± 0.24 | 0.47 ± 0.18 | 0.37 ± 0.20 | 0.505 | 0.823 | 0.353 |
| Average Vastus Medialis | 0.14 ± 0.04 | 0.13 ± 0.06 | 0.13 ± 0.04 | 0.12 ± 0.05 | 0.13 ± 0.04 | 0.13 ± 0.07 | 0.12 ± 0.05 | 0.09 ± 0.06 | 0.488 | 0.672 | 0.359 |
| Peak Vastus Medialis | 0.55 ± 0.12 | 0.49 ± 0.15 | 0.51 ± 0.14 | 0.53 ± 0.20 | 0.47 ± 0.18 | 0.44 ± 0.20 | 0.53 ± 0.18 | 0.38 ± 0.25 | 0.876 | 0.242 | 0.105 |
| PRE—Intervention | POST—Intervention | p-Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||||||||
| DL | NDL | DL | NDL | DL | NDL | DL | NDL | ||||
| Parametric Analysis | Mean ± Standard Deviation | Group*Time | Limb Dom*Time | Interaction Effect | |||||||
| Variables Muscle Activity (% of Maximum) | |||||||||||
| Peak Biceps Femoris | 0.53 ± 0.14 | 0.51 ± 0.13 | 0.48 ± 0.19 | 0.58 ± 0.15 | 0.51 ± 0.19 | 0.37 ± 0.24 | 0.56 ± 0.13 | 0.48 ± 0.18 | 0.212 | 0.013 * | 0.633 |
| Peak Semitendinosus | 0.51 ± 0.15 | 0.44 ± 0.14 | 0.45 ± 0.12 | 0.49 ± 0.21 | 0.30 ± 0.19 | 0.39 ± 0.14 | 0.47 ± 0.16 | 0.36 ± 0.15 | 0.173 | 0.945 | 0.006 * |
| PRE—Intervention | POST—Intervention | Wilcoxon p-Value (PRE—POST) | Effect Size d Cohen (PRE—POST) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Mann Whitney U | Effect Size d Cohen | Intervention | Control | Mann Whitney U | Effect Size d Cohen | |||||||||||||
| DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | DL | NDL | |||||
| Median [Interquartile range [Q1, Q3] | Intervention Related Samples Analyses | Control Related Samples Analyses | Intervention Related Samples Analyses | Control Related Samples Analyses | ||||||||||||||||
| Variables Muscle Activity (% of Maximum) | ||||||||||||||||||||
| Average Biceps Femoris | 0.10 [0.08, 0.12] | 0.10 [0.08, 0.12] | 0.10 [0.08, 0.13] | 0.12 [0.09, 0.15] | 0.883 | 0.163 | 0.00 | 2.00 † | 0.10 [0.07, 0.13] | 0.09 [0.03, 0.14] | 0.11 [0.09, 0.13] | 0.10 [0.07, 0.12] | 0.424 | 0.318 | 1.00 | 2.00 † | DL: 0.657 NDL: 0.156 | DL: 0.156 NDL: 0.420 | DL: 0.00 NDL: 2.00 † | DL: 1.00 NDL: 2.00 † |
| Average Semitendinosus | 0.09 [0.06, 0.12] | 0.09 [0.07, 0.11] | 0.09 [0.08, 0.11] | 0.11 [0.08, 0.13] | 0.883 | 0.118 | 0.00 | 2.00 † | 0.05 [0.02, 0.08] | 0.09 [0.05, 0.10] | 0.09 [0.07, 0.12] | 0.08 [0.06, 0.11] | 0.001 * | 0.782 | 5.00 † | 1.00 | DL: 0.004 * NDL: 0.652 | DL: 0.750 NDL: 0.117 | DL: 4.00 † NDL: 0.00 | DL: 1.00 NDL: 3.00 † |
| Average Vastus Lateralis | 0.15 [0.11, 0.17] | 0.13 [0.11, 0.16] | 0.12 [0.07, 0.17] | 0.13 [0.08, 0.16] | 0.303 | 0.335 | 2.00 † | 3.00 † | 0.14 [0.10, 0.16] | 0.14 [0.09, 0.17] | 0.13 [0.07, 0.16] | 0.08 [0.06, 0.11] | 0.351 | 0.173 | 2.00 † | 2.00 † | DL: 1.000 NDL: 0.089 | DL: 0.324 NDL: 0.128 | DL: 1.00 NDL: 2.00 † | DL: 1.00 NDL: 1.00 |
| Peak Vastus Lateralis | 0.66 [0.48, 0.74] | 0.64 [0.61, 0.71] | 0.59 [0.46, 0.68] | 0.65 [0.51, 0.72] | 0.219 | 0.660 | 1.11 † | 1.88 † | 0.68 [0.60, 0.74] | 0.68 [0.39, 0.77] | 0.58 [0.38, 0.68] | 0.43 [0.32, 0.61] | 0.083 | 0.207 | 1.99 † | 1.67 † | DL: 0.756 NDL: 0.121 | DL: 0.459 NDL: 0.124 | DL: 0.00 NDL: 1.90 † | DL: 1.00 NDL: 1.67 † |
| Average Vastus Medialis | 0.14 [0.11, 0.18] | 0.14 [0.09, 0.17] | 0.14 [0.10, 0.17] | 0.12 [0.09, 0.17] | 0.660 | 0.708 | 1.00 | 1.00 | 0.15 [0.11, 0.18] | 0.16 [0.07, 0.19] | 0.13 [0.09, 0.16] | 0.10 [0.06, 0.14] | 0.245 | 0.041 * | 2.00 † | 2.55 † | DL: 0.000 * NDL: 0.000 * | DL: 0.000 * NDL:0.000 * | DL: 1.10 † NDL: 1.26 † | DL: 1.10 † NDL: 3.00 † |
| Peak Vastus Medialis | 0.62 [0.51, 0.73] | 0.60 [0.41, 0.68] | 0.60 [0.53, 0.69] | 0.62 [0.48, 0.72] | 0.613 | 0.386 | 0.28 | 0.66 | 0.66 [0.53, 0.70] | 0.57 [0.43, 0.71] | 0.64 [0.57, 0.72] | 0.41 [0.29, 0.61] | 0.684 | 0.126 | 0.50 | 2.00 † | DL: 0.943 NDL: 0.538 | DL: 0.381 NDL: 0.026 * | DL: 0.00 NDL: 0.39 | DL: 0.85 NDL: 3.20 † |
| Mean Difference | p-Value | Effect Size d Cohen | 95% Confidence Intervals for Differences | |||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Variable—Kinematics | ||||||
| Thigh Extension Angular Velocity | DL_PRE and POST | −34.62 | 0.040 * | 2.20 † | −67.62 | −1.62 |
| NDL_PRE and POST | −33.81 | 0.053 | 2.48 † | −68.02 | 0.40 | |
| Variable—Muscle Activity EMG | ||||||
| Peak Biceps Femoris Load Phase | DL_PRE and POST | −0.03 | 0.432 | 1.00 | −0.10 | 0.05 |
| NDL_PRE and POST | 0.12 | 0.003 * | 3.79 † | 0.04 | 0.19 | |
| Mean Difference | p-Value | Effect Size d Cohen | 95% Confidence Intervals for Differences | ||||
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Variables—Kinematics ROM Thigh Sagittal Angular Velocity | |||||||
| Intervention | DL | PRE-POST | 65.14 | 0.137 | 0.44 | −23.07 | 153.34 |
| NDL | PRE-POST | −37.49 | 0.442 | 0.07 | −138.36 | 63.39 | |
| Control | DL | PRE-POST | −10.65 | 0.834 | 0.27 | −116.16 | 94.87 |
| NDL | PRE-POST | 157.38 | 0.015 * | 0.65 | 34.37 | 280.39 | |
| Variable—Muscle Activity EMG Peak Semitendinosus Load Phase | |||||||
| Intervention | DL | PRE-POST | 0.21 | 0.006 * | 1.23† | 0.07 | 0.34 |
| NDL | PRE-POST | 0.05 | 0.362 | 0.14 | −0.06 | 0.16 | |
| Control | DL | PRE-POST | −0.02 | 0.677 | 0.36 | −0.12 | 0.08 |
| NDL | PRE-POST | 0.13 | 0.103 | 0.71 | −0.03 | 0.28 | |
4. Discussion
4.1. Limitations
4.2. Clinical Contributions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACL | Anterior Cruciate Ligament |
| EMG | Electromyography |
| ST | Semitendinosus |
| BF | Biceps Femoris |
| VM | Vastus Medialis |
| VL | Vastus Lateralis |
| PREP | Preparation phase |
| LOAD | Load phase |
| ROM | Range of Motion |
| DL | Dominant Limb |
| NDL | Non-Dominant Limb |
| CODAT | Change of Direction and Acceleration Test |
| COD | Change of Direction |
| RPE | Rating of Perceived Exertion |
Appendix A. Multicomponent Periodized Program
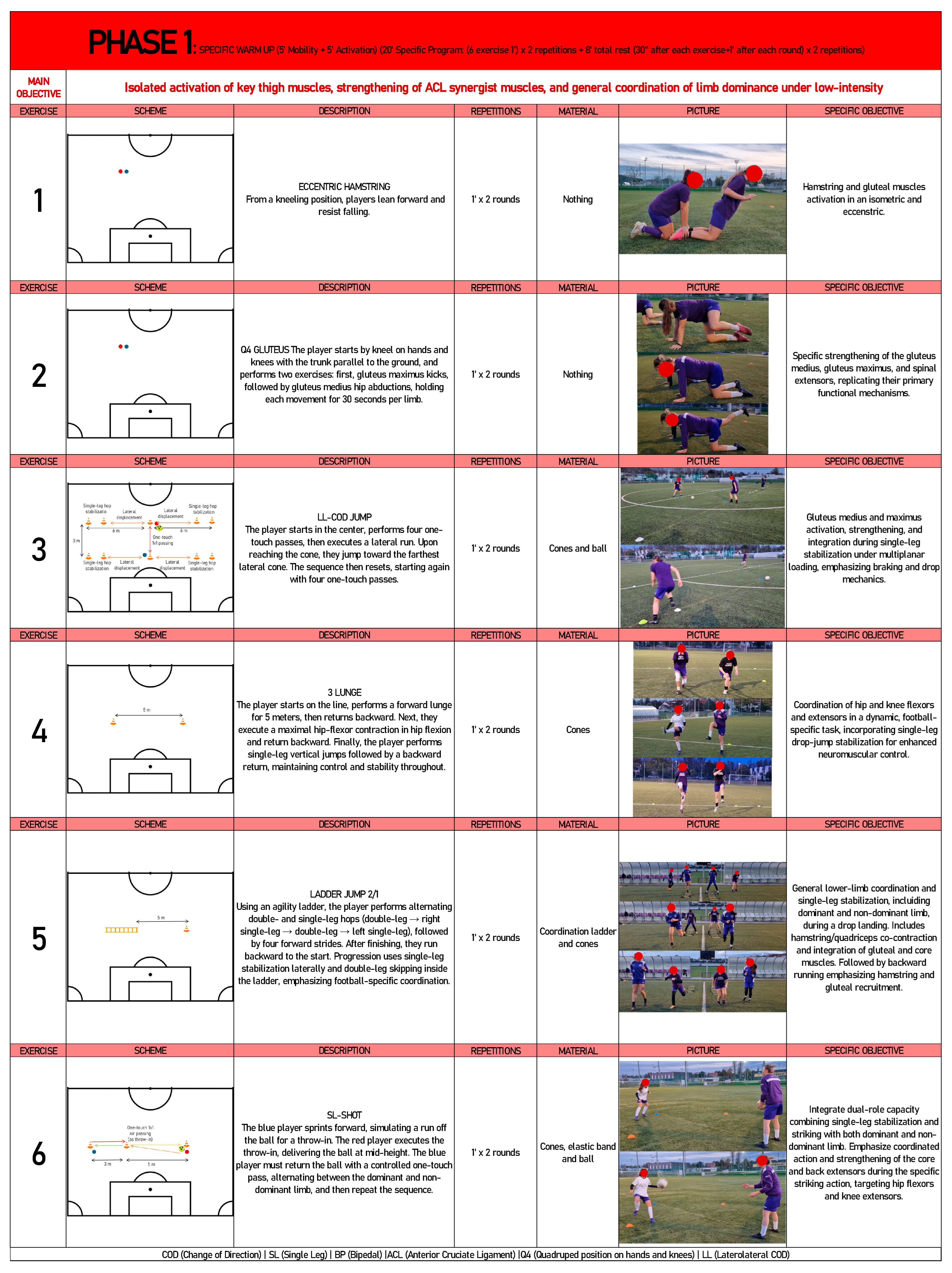
Appendix A.1. First Phase of Multicomponent Periodized Program
Appendix A.2. Second Phase of Multicomponent Periodized Program

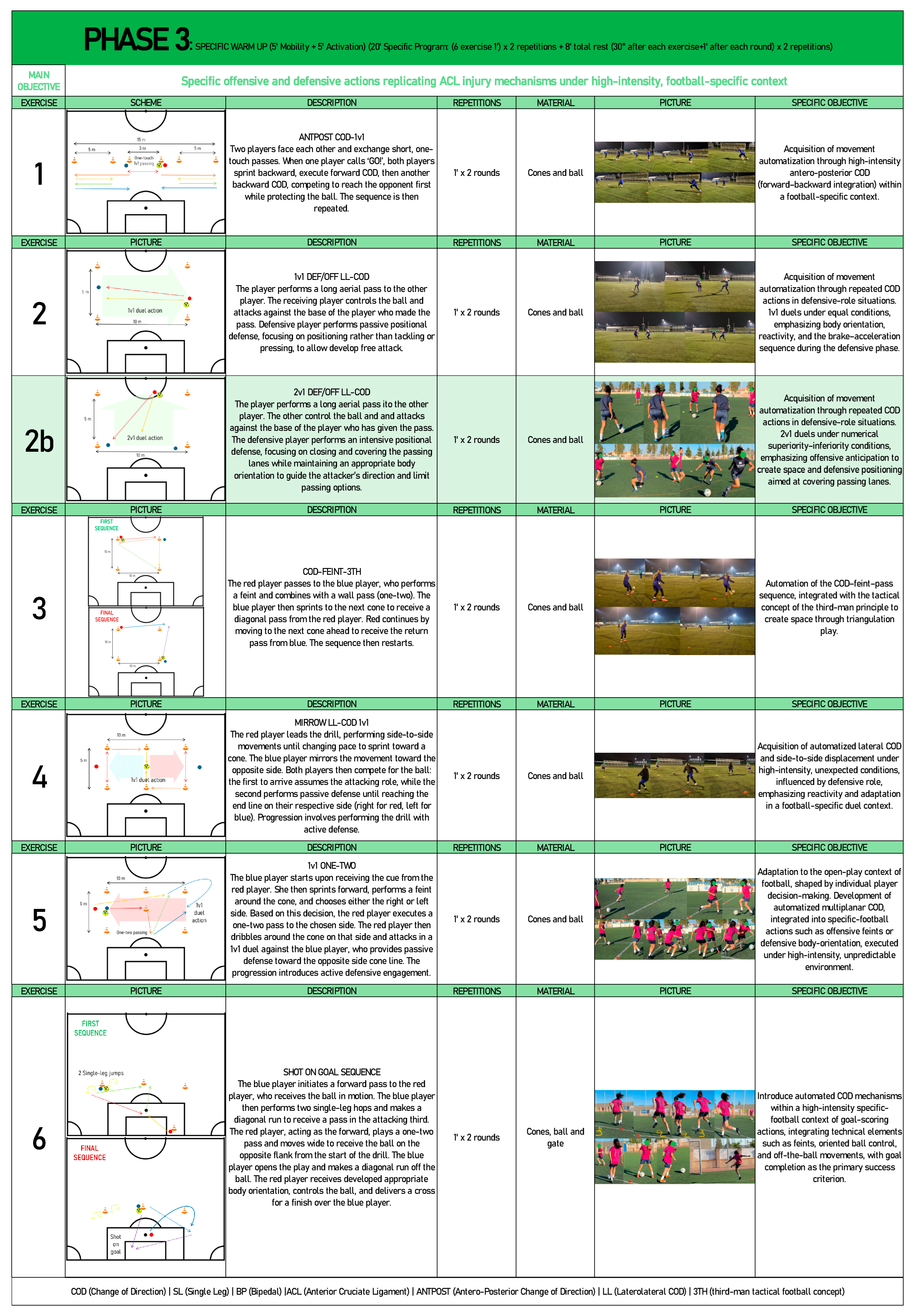
Appendix A.3. Third Phase of Multicomponent Periodized Program
References
- Hallén, A.; Tomás, R.; Ekstrand, J.; Bengtsson, H.; Van den Steen, E.; Hägglund, M.; Waldén, M. UEFA Women’s Elite Club Injury Study: A prospective study on 1527 injuries over four consecutive seasons 2018/2019 to 2021/2022 reveals thigh muscle injuries to be most common and ACL injuries most burdensome. Br. J. Sports Med. 2024, 58, 128–136. [Google Scholar] [CrossRef]
- Larruskain, J.; Lekue, J.A.; Angulo, P.; Santisteban, J.M.; Diaz-Beitia, G.; Martin-Garetxana, I.; Gil, S.M.; Bidaurrazaga-Letona, I.; Monasterio, X. An injury burden heat map of all men’s and women’s teams of a professional football club over a decade. Res. Sports Med. 2024, 32, 740–750. [Google Scholar] [CrossRef]
- Beech, J.; Jones, B.; King, R.; Bennett, P.; Young, S.; Williams, S.; Stokes, K.; Emmonds, S. The incidence and burden of injuries in elite English youth female soccer players. Sci. Med. Footb. 2022, 6, 605–615. [Google Scholar] [CrossRef]
- Union of European Football Associations (UEFA). Unstoppable. UEFA Women’s Football Strategy 2024–2030. A Six-Year Plan To-wards a Sustainable Ecosystem. 2024. Available online: https://editorial.uefa.com/resources/0292-1c3532529b72-3306578495fb-1000/unstoppable_uefa_women_s_football_strategy.pdf (accessed on 14 September 2025).
- Fédération Internationale de Football Association (FIFA). Women’s Football: Member Associations Survey Report. Documento Interno. 2023. Available online: https://digitalhub.fifa.com/m/6973d06842598476/original/Futbol-femenino-encuesta-a-las-federaciones-miembro-2023.pdf (accessed on 14 September 2025).
- Hilska, M.; Leppänen, M.; Vasankari, T.; Aaltonen, S.; Kannus, P.; Parkkari, J.; Steffen, K.; Kujala, U.M.; Konttinen, N.; Räisänen, A.M.; et al. Neuromuscular Training Warm-up Prevents Acute Noncontact Lower Extremity Injuries in Children’s Soccer: A Cluster Randomized Controlled Trial. Orthop. J. Sports Med. 2021, 9, 23259671211005769. [Google Scholar] [CrossRef]
- Nasseri, A.; Lloyd, D.G.; Minahan, C.; Sayer, T.A.; Paterson, K.; Vertullo, C.J.; Bryant, A.L.; Saxby, D.J. Effects of Pubertal Maturation on ACL Forces During a Landing Task in Females. Am. J. Sports Med. 2021, 49, 3322–3334. [Google Scholar] [CrossRef]
- Bolling, C.; Tomás, R.; Verhagen, E. ‘Considering the reality, I am very lucky’: How professional players and staff perceive injury prevention and performance protection in women’s football. Br. J. Sports Med. 2024, 58, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Lucarno, S.; Zago, M.; Buckthorpe, M.; Grassi, A.; Tosarelli, F.; Smith, R.; Della Villa, F. Systematic Video Analysis of Anterior Cruciate Ligament Injuries in Professional Female Soccer Players. Am. J. Sports Med. 2021, 49, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Logerstedt, D.S.; Scalzitti, D.; Risberg, M.A.; Engebretsen, L.; Webster, K.E.; Feller, J.; Snyder-Mackler, L.; Axe, M.J.; McDonough, C.M. Knee stability and movement coordination impairments: Knee ligament sprain revision. J. Orthop. Sports Phys. Ther. 2017, 47, A1–A47. [Google Scholar] [CrossRef]
- Beaulieu, M.L.; Ashton-Miller, J.A.; Wojtys, E.M. Loading mechanisms of the anterior cruciate ligament. Sports Biomech. 2023, 22, 1–29. [Google Scholar] [CrossRef]
- Dos’santos, T.; McBurnie, A.; Comfort, P.; Jones, P.A. The effects of six-weeks change of direction speed and technique modification training on cutting performance and movement quality in male youth soccer players. Sports 2019, 7, 205. [Google Scholar] [CrossRef]
- DeLang, M.D.; Salamh, P.A.; Farooq, A.; Tabben, M.; Whiteley, R.; van Dyk, N.; Chamari, K. The dominant leg is more likely to get injured in soccer players: Systematic review and meta-analysis. Biol. Sport 2021, 38, 397–435. [Google Scholar] [CrossRef]
- Hewett, T.E.; Ford, K.R.; Myer, G.D. Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuro-muscular interventions aimed at injury prevention. Am. J. Sports Med. 2006, 34, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Dos’sAntos, T.; Comfort, P.; Jones, P.A. Male and female soccer players exhibit different knee joint mechanics during pre-planned change of direction. Sports Biomech. 2024, 23, 118–131. [Google Scholar] [CrossRef]
- Brophy, R.H.; Stepan, J.G.; Silvers, H.J.; Mandelbaum, B.R. Defending Puts the Anterior Cruciate Ligament at Risk During Soccer: A Gender-Based Analysis. Sports Health. 2015, 7, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Arundale, A.J.H.; Bizzini, M.; Giordano, A.; Hewett, T.E.; Logerstedt, D.S.; Mandelbaum, B.; Scalzitti, D.A.; Silvers-Granelli, H.; Snyder-Mackler, L.; Altman, R.D.; et al. Exercise-Based Knee and Anterior Cruciate Ligament Injury Prevention. J. Orthop. Sports Phys. Ther. 2023, 48, A1–A42. [Google Scholar] [CrossRef]
- Petushek, E.J.; Sugimoto, D.; Stoolmiller, M.; Smith, G.; Myer, G.D. Evidence-Based Best-Practice Guidelines for Preventing Anterior Cruciate Ligament Injuries in Young Female Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2019, 47, 1744–1753. [Google Scholar] [CrossRef] [PubMed]
- Dos’Santos, T.; Thomas, C.; Comfort, P.; Jones, P.A. The Effect of Training Interventions on Change of Direction Biomechanics Associated with Increased Anterior Cruciate Ligament Loading: A Scoping Review. Sports Med. 2019, 49, 1837–1859. [Google Scholar] [CrossRef]
- Olivares-Jabalera, J.; Fílter-Ruger, A.; Dos’santos, T.; Afonso, J.; Della Villa, F.; Morente-Sánchez, J.; Soto-Hermoso, V.M.; Requena, B. Exercise-Based Training Strategies to Reduce the Incidence or Mitigate the Risk Factors of Anterior Cruciate Ligament Injury in Adult Football (Soccer) Players: A Systematic Review. Int. J. Environ. Res. Public Health. 2021, 18, 13351. [Google Scholar] [CrossRef]
- Wang, D.; Valtonen, A.M.; Thiel, T.; Stenroth, L.; Gao, Y.; Kulmala, J.-P. Effects of Exercise-Based ACL Injury Prevention Interventions on Knee Motion in Athletes: A Systematic Review and Bayesian Network Meta-Analysis. J. Orthop. Sports Phys. Ther. 2025, 55, 123–136. [Google Scholar] [CrossRef]
- Wang, D.; Wang, M.; Chu, V.W.-S.; Yung, P.S.-H.; Fong, D.T. Effects of Gluteus Medius and Biceps Femoris Stimulation on Reduction of Knee Abduction Moment During a Landing Task. J. Appl. Biomech. 2023, 39, 110–117. [Google Scholar] [CrossRef]
- Aoki, A.; Kubota, S.; Morinaga, K.; Zheng, N.N.; Wang, S.S.; Gamada, K. Detection of knee wobbling as a screen to identify athletes who may be at high risk for ACL injury. Int. Biomech. 2021, 8, 30–41. [Google Scholar] [CrossRef]
- Wakabayashi, K.; Ogasawara, I.; Suzuki, Y.; Nakata, K.; Nomura, T. Exploring pre-impact landing kinematics associated with increase and decrease in the anterior cruciate ligament injury risk. J. Biomech. 2022, 145, 111382. [Google Scholar] [CrossRef]
- Jeong, J.; Choi, D.-H.; Shin, C.S. Association Between the Medial-Lateral Quadriceps and Hamstring Muscle Thickness and the Knee Kinematics and Kinetics During Single-Leg Landing. Sports Health 2023, 15, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S.; Colosimo, A.J.; McLean, S.G.; Van Den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Dix, C.; Arundale, A.; Silvers-Granelli, H.; Marmon, A.; Zarzycki, R.; Snyder-Mackler, L. Biomechanical measures during two sport-specific tasks differentiate between soccer players who go on to anterior cruciate ligament injury and those who do not: A prospective cohort analysis. Int. J. Sports Phys. Ther. 2020, 15, 928–935. [Google Scholar] [CrossRef]
- Nasseri, A.; Akhundov, R.; Bryant, A.L.; Lloyd, D.G.; Saxby, D.J. Limiting the Use of Electromyography and Ground Reaction Force Data Changes the Magnitude and Ranking of Modelled Anterior Cruciate Ligament Forces. Bioengineering 2023, 10, 369. [Google Scholar] [CrossRef]
- Ebner, C.; Granacher, U.; Gehring, D. Effects of Anticipation and Dual-Tasking on Lower Limb Biomechanics While Performing Change-of-Direction Tasks in Physically Active Individuals: A Systematic Review with Meta-Analysis. Sports Med. 2025, 55, 857–876. [Google Scholar] [CrossRef] [PubMed]
- Boden, B.P.; Torg, J.S.; Knowles, S.B.; Hewett, T.E. Video analysis of anterior cruciate ligament injury: Abnormalities in hip and ankle kinematics. Am. J. Sports Med. 2009, 37, 252–259. [Google Scholar] [CrossRef]
- Dix, C.; Arundale, A.; Silvers-Granelli, H.; Marmon, A.; Zarzycki, R.; Arch, E.; Snyder-Mackler, L. Descriptive trunk kinematics in healthy collegiate women’s soccer players indicate trunk center of mass is laterally positioned prior to decelerating and cutting. J. ISAKOS 2022, 7, 10–16. [Google Scholar] [CrossRef]
- Quatman, C.E.; Hewett, T.E. The anterior cruciate ligament injury controversy: Is “valgus collapse” a sex-specific mechanism? Br. J. Sports Med. 2009, 43, 328–335. [Google Scholar] [CrossRef]
- Ueno, R.; Navacchia, A.; Schilaty, N.D.; Myer, G.D.; Hewett, T.E.; Bates, N.A. Anterior Cruciate Ligament Loading Increases With Pivot-Shift Mechanism During Asymmetrical Drop Vertical Jump in Female Athletes. Orthop. J. Sports Med. 2021, 9, 2325967121989095. [Google Scholar] [CrossRef]
- Steiner, M.; Baur, H.; Blasimann, A. Sex-specific differences in neuromuscular activation of the knee stabilizing muscles in adults—A systematic review. Arch. Physiother. 2023, 13, 4. [Google Scholar] [CrossRef]
- Bencke, J.; Zebis, M.K. The influence of gender on neuromuscular pre-activity during side-cutting. J. Electromyogr. Kinesiol. 2011, 21, 371–375. [Google Scholar] [CrossRef]
- Zebis, M.K.; Aagaard, P.; Andersen, L.L.; Hölmich, P.; Clausen, M.B.; Brandt, M.; Husted, R.S.; Lauridsen, H.B.; Curtis, D.J.; Bencke, J. First-time anterior cruciate ligament injury in adolescent female elite athletes: A prospective cohort study to identify modifiable risk factors. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1341–1351. [Google Scholar] [CrossRef]
- Husted, R.S.; Bencke, J.; Andersen, L.L.; Myklebust, G.; Kallemose, T.; Lauridsen, H.B.; Hölmich, P.; Aagaard, P.; Zebis, M.K. A comparison of hamstring muscle activity during different screening tests for non-contact ACL injury. Knee 2016, 23, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; Demeco, A.; de Scorpio, G.; Indino, A.; Iona, T.; Ammendolia, A. Late activation of the vastus medialis in determining the risk of anterior cruciate ligament injury in soccer players. J. Sport Rehabil. 2020, 29, 952–955. [Google Scholar] [CrossRef]
- Nasseri, A.; Lloyd, D.G.; Bryant, A.L.; Headrick, J.; Sayer, T.A.; Saxby, D.J. Mechanism of Anterior Cruciate Ligament Loading during Dynamic Motor Tasks. Med. Sci. Sports Exerc. 2021, 53, 1235–1244. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Ethical Principles for Medical Research Involving Human Subjects. Eur. J. Emerg. Med. 2001, 8, 221–223. [Google Scholar] [CrossRef]
- Poretti, K.; Ghoddosi, N.; Martin, J.; Eddo, O.; Cortes, N.; Clark, N.C. The Nature of Rehabilitation Programs to Improve Musculoskeletal, Biomechanical, Functional, and Patient-Reported Outcomes in Athletes With ACL Reconstruction: A Scoping Review. Sports Health. 2024, 16, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.; Choi, D.-H.; Shin, C.S. The Effect of Strength Training Targeting Medial Thigh Muscles on Neuromuscular and Biomechanical Risk Factors for Anterior Cruciate Ligament Injury: A Randomized Controlled Trial. Sports Med. Open 2025, 11, 5. [Google Scholar] [CrossRef]
- Ferrández-Laliena, L.; Vicente-Pina, L.; Sánchez-Rodríguez, R.; Chapman, G.J.; Heredia-Jimenez, J.; Hidalgo-García, C.; Tricás-Moreno, J.M.; Lucha-López, M.O. Differences in Kinematic and Muscle Activity Between ACL Injury Risk and Healthy Players in Female Football: Influence of Change of Direction Amplitude in a Cross-Sectional Case–Control Study. Medicina 2025, 61, 1259. [Google Scholar] [CrossRef]
- Markström, J.L.; Grinberg, Y.; Sole, G.; Häger, C.K. Strategies for knee stabilising and pivot-shift avoidance in a step-down and cross-over task observed sub-acutely after anterior cruciate ligament reconstruction. Clin. Biomech. 2024, 115, 106255. [Google Scholar] [CrossRef] [PubMed]
- Picot, B.; Lempereur, M.; Morel, B.; Forestier, N.; Rémy-Néris, O. Lack of Proprioceptive Strategy Modulation Leads to At-Risk Biomechanics for Anterior Cruciate Ligament in Healthy Athletes. Med. Sci. Sports Exerc. 2024, 56, 942–952. [Google Scholar] [CrossRef] [PubMed]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Budini, K.; Richards, J.; Cole, T.; Levine, D.; Trede, R.; George, L.S.; Selfe, J. An exploration of the use of Inertial Measurement Units in the assessment of dynamic postural control of the knee and the effect of bracing and taping. Physiother. Prac. Res. 2018, 39, 91–98. [Google Scholar] [CrossRef]
- Costello, K.E.; Eigenbrot, S.; Geronimo, A.; Guermazi, A.; Felson, D.T.; Richards, J.; Kumar, D. Quantifying varus thrust in knee osteoarthritis using wearable inertial sensors: A proof of concept. Clin. Biomech. 2020, 80, 105232. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.; Brito, J.P.; Fernandes, R.; Espada, M.C.; Santos, F.J.; Nalha, M.; Zmijewski, P.; Morgans, R. Comparison of external load during differing microcycle structures across two competitive seasons in elite female Portuguese soccer players. Front. Sports Act. Living 2025, 26, 1608382. [Google Scholar] [CrossRef]
- Hamoongard, M.; Letafatkar, A.; Thomas, A.C. The Effect of Neurocognitive Training on Biomechanical Risk Factors Related to Anterior Cruciate Ligament Injury in Athletes: A Narrative Review. J. Sport Rehabil. 2024, 33, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Boggenpoel, B.Y.; Nel, S.; Hanekom, S. The use of periodized exercise prescription in rehabilitation: A systematic scoping review of literature. Clin. Rehabil. 2018, 32, 1235–1248. [Google Scholar] [CrossRef]
- Swallow, W.E.; Skidmore, N.; Page, R.M.; Malone, J.J. An examination of in-season external training load in semi-professional soccer players: Considerations of one and two match weekly microcycles. Int. J. Sports Sci. Coach. 2021, 16, 192–199. [Google Scholar] [CrossRef]
- Vendrig, T.; Keizer, M.N.; Brouwer, R.W.; Houdijk, H. A Cognitive Dual Task Alters Dynamic Tibiofemoral Movements During Jump-Landing Assessments in Healthy Participants. Orthop. J. Sports Med. 2025, 13, 23259671251340996. [Google Scholar] [CrossRef]
- Martín-García, A.; Gómez-Díaz, A.; Bradley, P.S.; Morera, F.; Casamichana, D. Quantification of a professional football team’s external load using a microcycle structure. J. Strength Cond. Res. 2018, 32, 3511–3518. [Google Scholar] [CrossRef] [PubMed]
- Malone, J.J.; Di Michele, R.; Morgans, R.; Burgess, D.; Morton, J.P.; Drust, B. Seasonal training-load quantification in elite English Premier League soccer players. Int. J. Sports Physiol. Perform. 2015, 10, 489–497. [Google Scholar] [CrossRef]
- Miguel, M.; Cortez, A.; Romero, F.; Loureiro, N.; García-Rubio, J.; Ibáñez, S.J. Daily and weekly external loads in the microciclye: Characterization and comparison between playing positions on amateur soccer. Front. Sports Act. Living 2022, 4, 943367. [Google Scholar] [CrossRef] [PubMed]
- Romero-Moraleda, B.; González-García, J.; Morencos, E.; Giráldez-Costas, V.; Moya, J.M.; Ramirez-Campillo, R. Internal workload in elite female football players during the whole in-season: Starters vs non-starters. Biol. Sport 2023, 40, 1107. [Google Scholar] [CrossRef] [PubMed]
- Lathlean, T.J.H.; Gastin, P.B.; Newstead, S.V.; Finch, C.F. Human Kinetics (Soil A Prospective Cohort Study of Load and Wellness (Sleep, Fatigue, Soreness, Stress, and Mood) in Elite Junior Australian Football Players. Int. J. Sports Physiol. Perform. 2019, 14, 829–840. [Google Scholar] [CrossRef]
- Karacan, I.; Arslan, B.T.; Karaoglu, A.; Aydin, T.; Gray, S.; Ungan, P.; Türker, K.S. Estimating and minimizing movement artifacts in surface electromyogram. J. Electromyogr. Kinesiol. 2023, 70, 102778. [Google Scholar] [CrossRef]
- Ruan, M.; Zhang, Q.; Wu, X. Acute effects of static stretching of hamstring on performance and anterior cruciate ligament injury risk during stop-jump and cutting tasks in female athletes. J. Strength Cond. Res. 2017, 31, 1241–1250. [Google Scholar] [CrossRef]
- Universitat de Barcelona, Institut Municipal d’Investigació Mèdica (IMIM). GRANMO: Sample Size Calculator, Version 8.0; Universidad de Barcelona: Barcelona, Spain, 2012.
- McBurnie, A.J.; Dos’Santos, T.; Jones, P.A. Biomechanical Associates of Performance and Knee Joint Loads During A 70–90° Cutting90° Cutting Maneuver in Subelite Soccer Players. J. Strength Cond. Res. 2019, 35, 3190–3198. [Google Scholar] [CrossRef]
- Dos’Santos, T.; Thomas, C.; McBurnie, A.; Comfort, P.; Jones, P.A. Biomechanical Determinants of Performance and Injury Risk During Cutting: A Performance-Injury Conflict? Sports Med. 2021, 51, 1983–1998. [Google Scholar] [CrossRef]
- Bates, N.A.; Nesbitt, R.J.; Shearn, J.T.; Myer, G.D.; Hewett, T.E. The influence of internal and external tibial rotation offsets on knee joint and ligament biomechanics during simulated athletic tasks. Clin. Biomech. 2018, 52, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.; Landry, S.; Urquhart, N.; Coady, C.; Rutherford, D. Drop landing between subjects post anterior cruciate ligament reconstruction and uninjured controls: A biomechanical and neuromuscular analysis. Clin. Biomech. 2025, 124, 106504. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrández-Laliena, L.; Vicente-Pina, L.; Sánchez-Rodríguez, R.; Chapman, G.J.; Soussi, B.; Hidalgo-García, C.; Lucha-López, M.O.; Tricás-Moreno, J.M.; Ambrus, M. Effects of a Multicomponent Periodized Program in Kinematic and Muscle Activity Characteristics Related to Anterior Cruciate Ligament Injury Mechanism in College Football Players—A Controlled Trial. J. Funct. Morphol. Kinesiol. 2025, 10, 412. https://doi.org/10.3390/jfmk10040412
Ferrández-Laliena L, Vicente-Pina L, Sánchez-Rodríguez R, Chapman GJ, Soussi B, Hidalgo-García C, Lucha-López MO, Tricás-Moreno JM, Ambrus M. Effects of a Multicomponent Periodized Program in Kinematic and Muscle Activity Characteristics Related to Anterior Cruciate Ligament Injury Mechanism in College Football Players—A Controlled Trial. Journal of Functional Morphology and Kinesiology. 2025; 10(4):412. https://doi.org/10.3390/jfmk10040412
Chicago/Turabian StyleFerrández-Laliena, Loreto, Lucía Vicente-Pina, Rocío Sánchez-Rodríguez, Graham J. Chapman, Badis Soussi, César Hidalgo-García, María Orosia Lucha-López, José Miguel Tricás-Moreno, and Mira Ambrus. 2025. "Effects of a Multicomponent Periodized Program in Kinematic and Muscle Activity Characteristics Related to Anterior Cruciate Ligament Injury Mechanism in College Football Players—A Controlled Trial" Journal of Functional Morphology and Kinesiology 10, no. 4: 412. https://doi.org/10.3390/jfmk10040412
APA StyleFerrández-Laliena, L., Vicente-Pina, L., Sánchez-Rodríguez, R., Chapman, G. J., Soussi, B., Hidalgo-García, C., Lucha-López, M. O., Tricás-Moreno, J. M., & Ambrus, M. (2025). Effects of a Multicomponent Periodized Program in Kinematic and Muscle Activity Characteristics Related to Anterior Cruciate Ligament Injury Mechanism in College Football Players—A Controlled Trial. Journal of Functional Morphology and Kinesiology, 10(4), 412. https://doi.org/10.3390/jfmk10040412









