More than Just Type 1 or Type 2: Radiologically and Anatomically Refined Lunate Classification Correlating Ulnar Carpal Alignment and Hamate-Lunate Osteoarthrosis
Abstract
1. Introduction
2. Materials and Methods
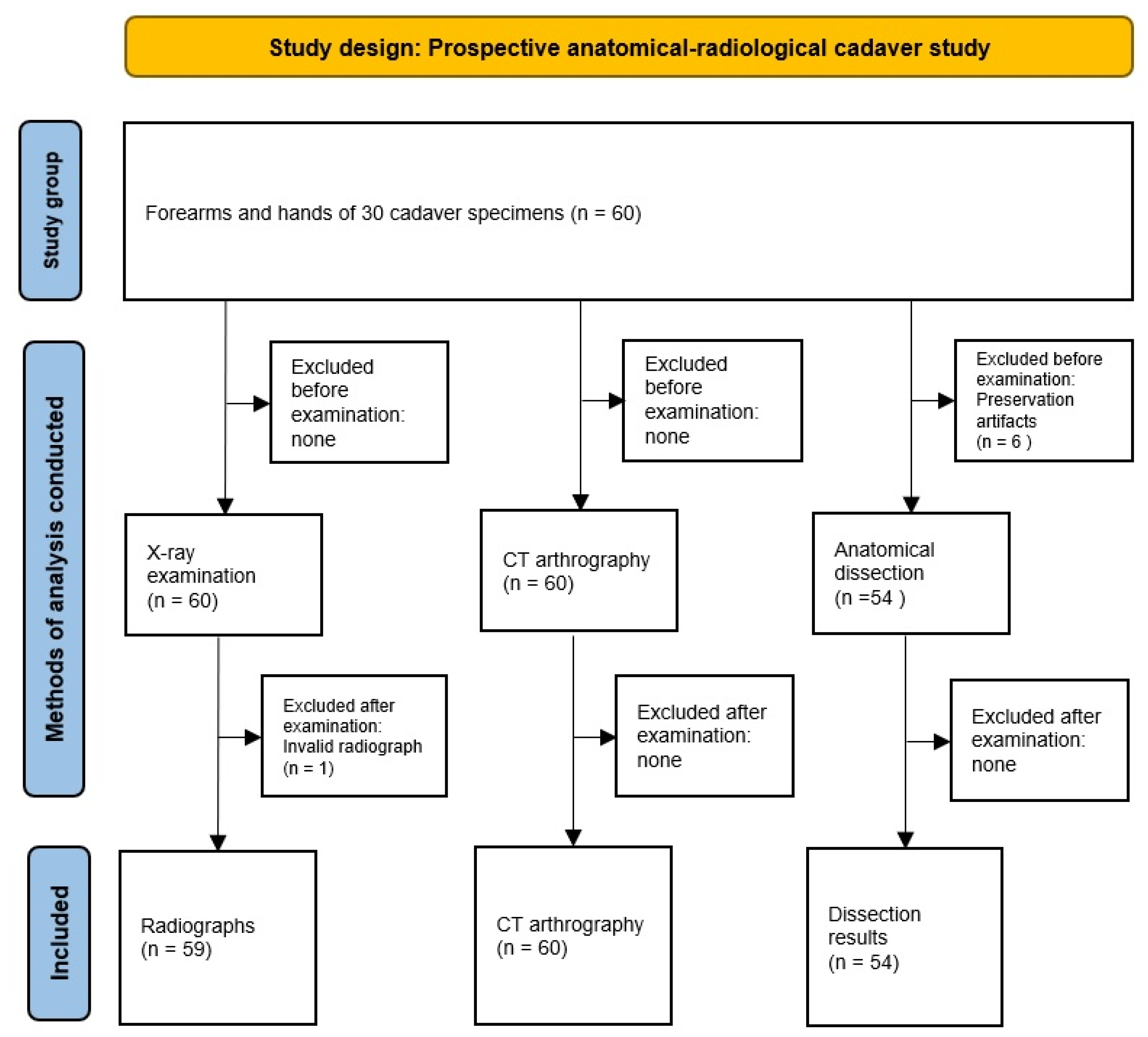
2.1. Study Design and Data Collection
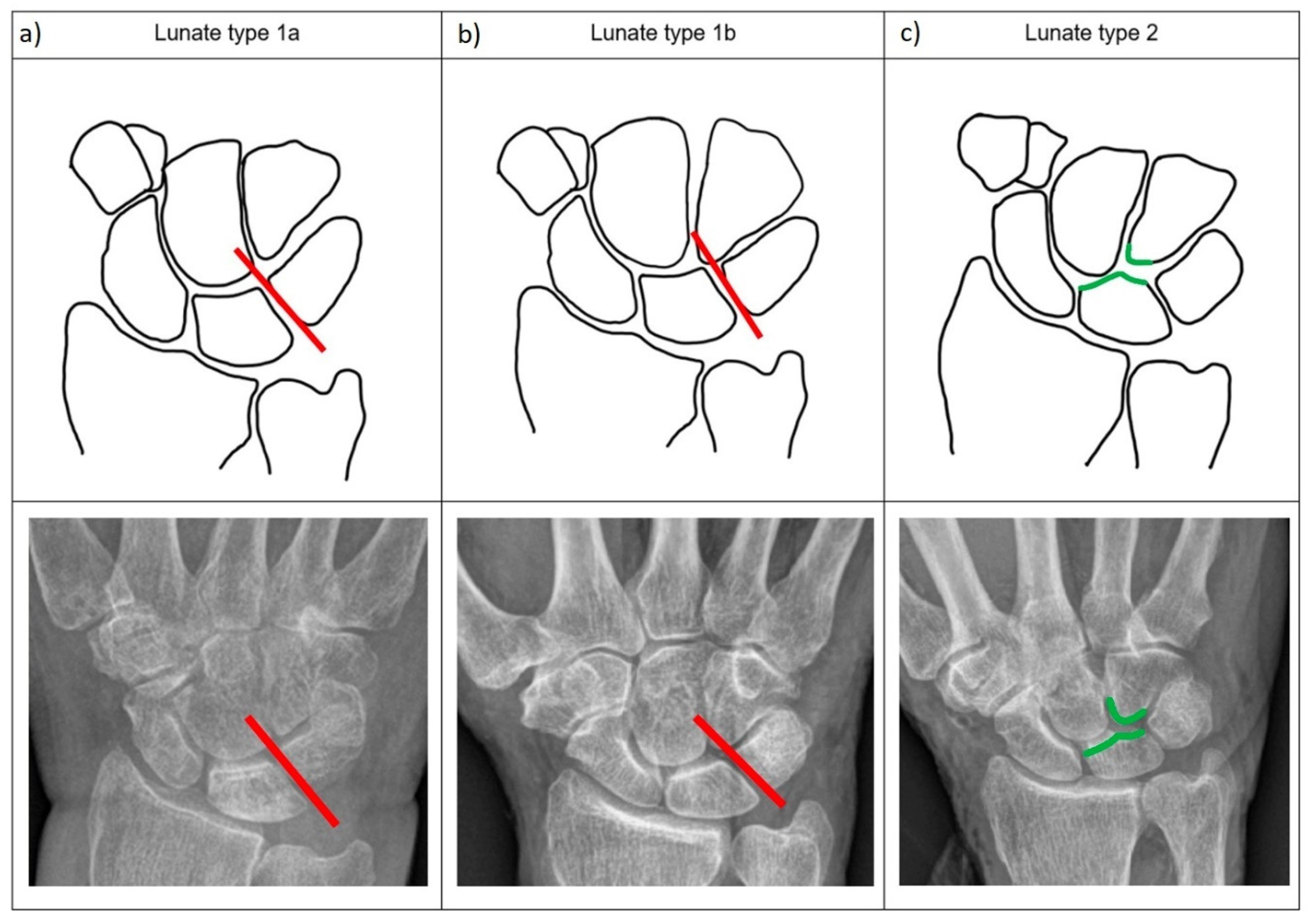
2.2. Radiological Examinations
2.3. Anatomical Examinations
2.4. Statistical Analysis
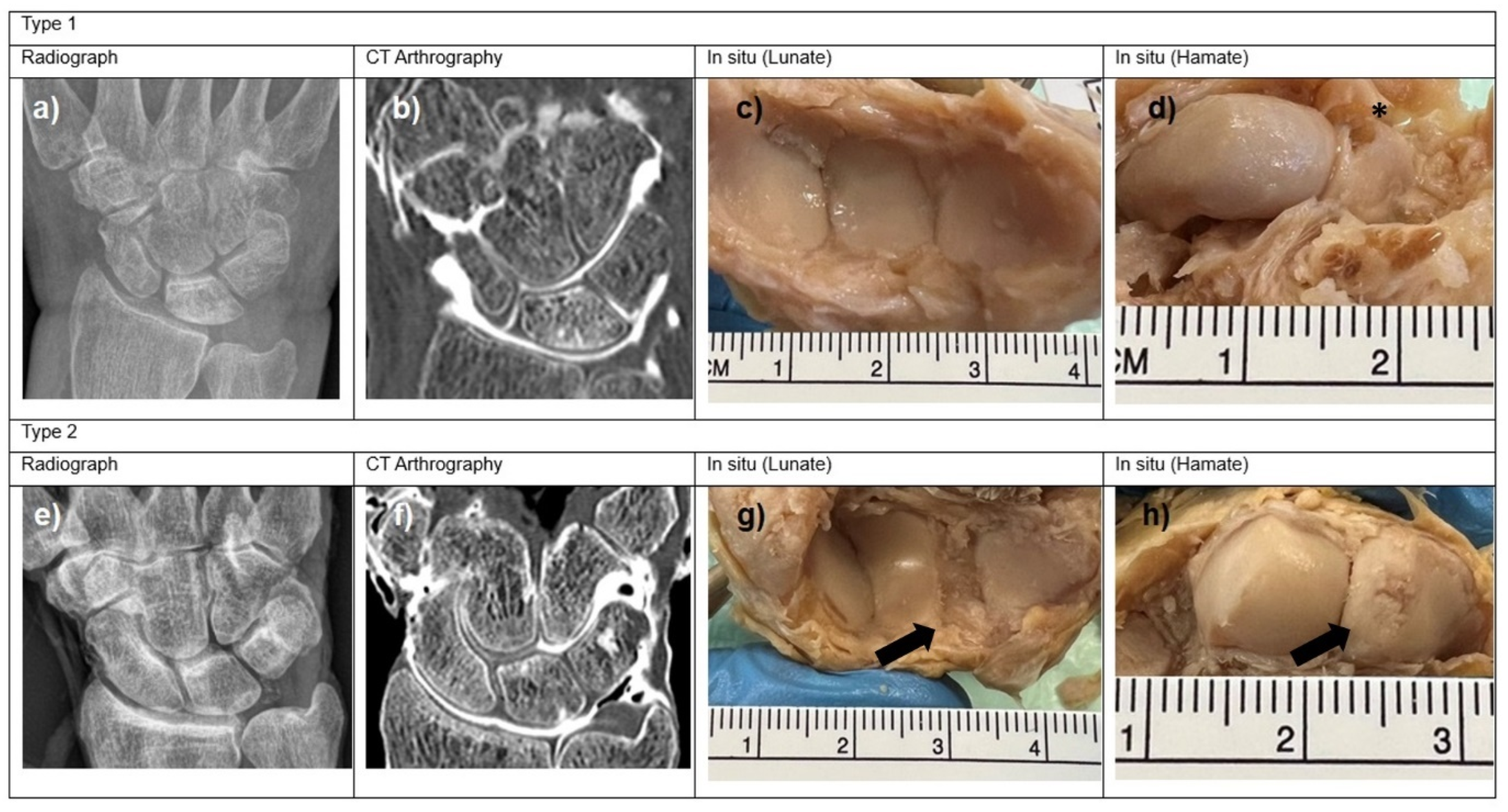
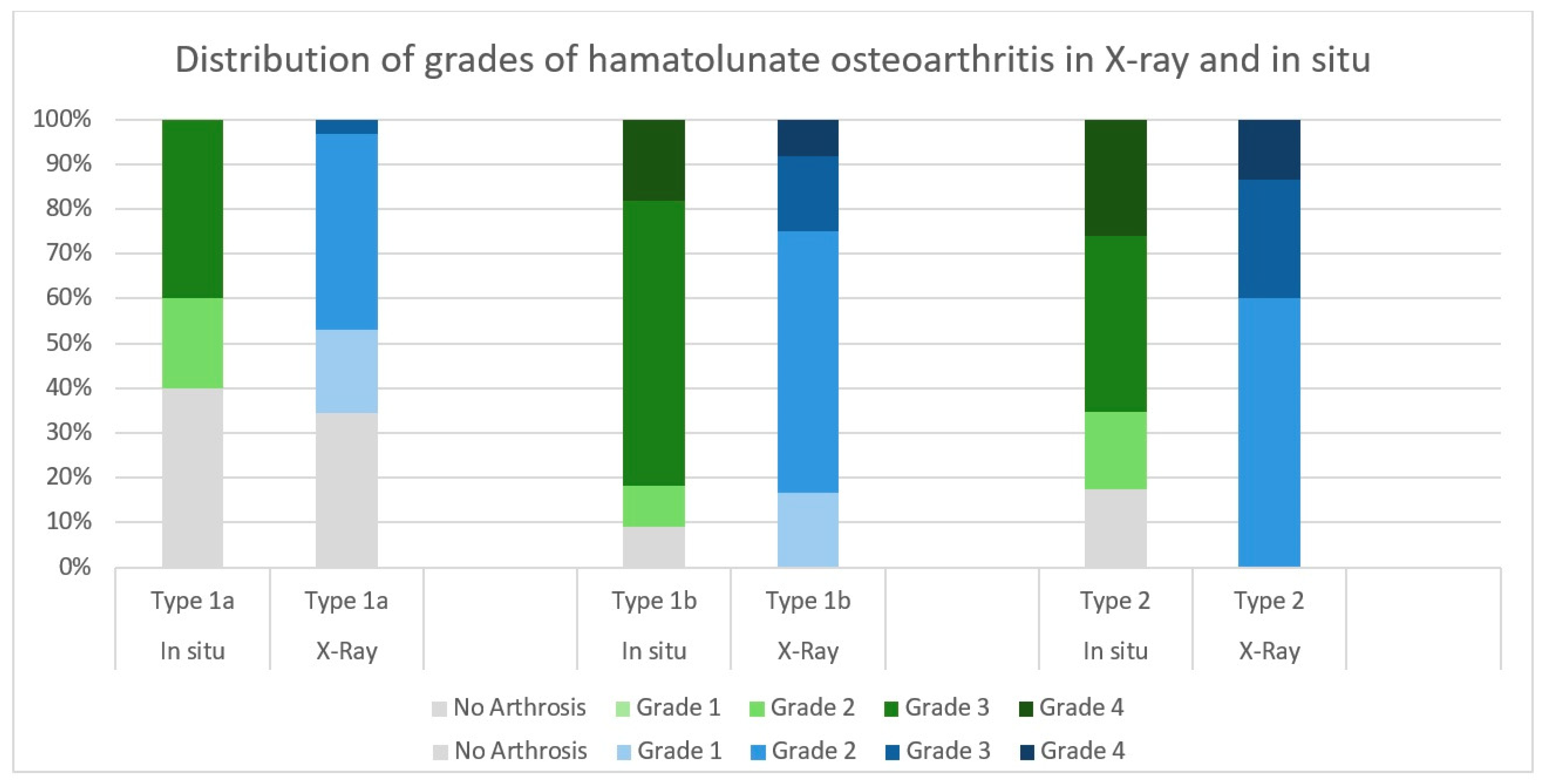
3. Results
- In situ:
- Radiological imaging:
4. Discussion
- Limitations of this study:
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ko, E.H.; Viegas, S.F. Chronic wrist pain. Curr. Opin. Rheumatol. 1997, 9, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Thurston, A.J.; Stanley, J.K. Hamato-lunate impingement: An uncommon cause of ulnar-sided wrist pain. Arthroscopy 2000, 16, 540–544. [Google Scholar]
- Viegas, S.F.; Wagner, K.; Patterson, R.; Peterson, P. Medial (hamate) facet of the lunate. J. Hand Surg. Am. 1990, 15, 564–571. [Google Scholar] [PubMed]
- DaSilva, M.F.; Goodman, A.D.; Gil, J.A.; Akelman, E. Evaluation of Ulnar-sided Wrist Pain. JAAOS J. Am. Acad. Orthop. Surg. 2017, 25, e150–e156. [Google Scholar]
- Sachar, K. Ulnar-sided wrist pain: Evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J. Hand Surg. Am. 2012, 37, 1489–1500. [Google Scholar] [PubMed]
- Artuso, M.; Picard, K.; Manoukov, Y.; Fontes, D. Hamatolunate impingement syndrome in golfers: Results of arthroscopic burring of the apex of the hamate. Hand Surg. Rehabil. 2022, 41, 452–456. [Google Scholar]
- Pirolo, J.M.; Yao, J. Minimally invasive approaches to ulnar-sided wrist disorders. Hand Clin. 2014, 30, 77–89. [Google Scholar] [CrossRef]
- Ali, B.; Ozyurekoglu, T. Arthroscopic Management of the Hamate Proximal Pole Arthrosis. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4672. [Google Scholar]
- Meaike, J.; Meaike, J.; Kakar, S. Outcomes Following Surgical Treatment of Hamate Arthrosis Lunotriquetral Ligament Injuries. Hand 2023, 18, 582–588. [Google Scholar]
- Nakamoto, J.C.; Althoff, B.F.; Abarca Herrera, A.K.; Escudero, R.B. Hamatolunate impingement, a differential diagnosis of ulnar-sided wrist pain. J. Hand Microsurg. 2024, 16, 100049. [Google Scholar]
- Arai, T. Roentgenographical and anatomical study of the midcarpal joint--morphology and degenerative change of ulnar side. Nihon Seikeigeka Gakkai Zasshi 1993, 67, 1114–1121. [Google Scholar]
- Nakamura, K.; Patterson, R.M.; Moritomo, H.; Viegas, S.F. Type I versus type II lunates: Ligament anatomy and presence of arthrosis. J. Hand Surg. Am. 2001, 26, 428–436. [Google Scholar] [CrossRef]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [PubMed]
- Outerbridge, R.E. The etiology of chondromalacia patellae. J. Bone Joint Surg. Br. 1961, 43, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Slattery, C.; Kweon, C.Y. Classifications in Brief: Outerbridge Classification of Chondral Lesions. Clin. Orthop. Relat. Res. 2018, 476, 2101–2104. [Google Scholar]
- Bin Abd Razak, H.R.; Heng, H.Y.; Cheng, K.Y.; Mitra, A.K. Correlation between radiographic and arthroscopic findings in Asian osteoarthritic knees. J. Orthop. Surg. 2014, 22, 155–157. [Google Scholar]
- Newman, S.; Ahmed, H.; Rehmatullah, N. Radiographic vs. MRI vs. arthroscopic assessment and grading of knee osteoarthritis-are we using appropriate imaging? J. Exp. Orthop. 2022, 9, 2. [Google Scholar]
- AlOmran, A.S. Osteoarthritis of knee: Correlation between radiographic and arthroscopic findings. Int. Surg. 2009, 94, 269–272. [Google Scholar]
- Lysholm, J.; Hamberg, P.; Gillquist, J. The correlation between osteoarthrosis as seen on radiographs and on arthroscopy. Arthroscopy 1987, 3, 161–165. [Google Scholar] [CrossRef]
- Pal, A.; Bhanarkar, U.; Ray, B. Embalming with Formalin—Benefits and Pitfalls. Sch. Int. J. Anat. Physiol. 2022, 5, 70–77. [Google Scholar]
- Waldt, S.; Eiber, M.; Wörtler, K. Messverfahren und Klassifikationen in der Muskuloskettalen Radiologie; Thieme: Stuttgart, Deutschland, 2011. [Google Scholar]
- Felson, D.T.; Naimark, A.; Anderson, J.; Kazis, L.; Castelli, W.; Meenan, R.F. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1987, 30, 914–918. [Google Scholar] [CrossRef] [PubMed]
- Gietzen, C.H.; Kunz, A.S.; Luetkens, K.S.; Huflage, H.; Christopoulos, G.; van Schoonhoven, J.; Bley, T.A.; Schmitt, R.; Grunz, J.P. Evaluation of prestyloid recess morphology and ulnar-sided contrast leakage in CT arthrography of the wrist. BMC Musculoskelet. Disord. 2022, 23, 284. [Google Scholar] [CrossRef]
- Cerezal, L.; de Dios Berná-Mestre, J.; Canga, A.; Llopis, E.; Rolon, A.; Martín-Oliva, X.; del Piñal, F. MR and CT arthrography of the wrist. Semin. Musculoskelet Radiol. 2012, 16, 27–41. [Google Scholar] [CrossRef]
- Thienpont, E.; Schwab, P.E.; Omoumi, P. Wear patterns in anteromedial osteoarthritis of the knee evaluated with CT-arthrography. Knee 2014, 21, S15–S19. [Google Scholar] [CrossRef]
- Cohen, M.M.; Vela, N.D.; Levine, J.E.; Barnoy, E.A. Validating a new computed tomography atlas for grading ankle osteoarthritis. J. Foot Ankle Surg. 2015, 54, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Qin, J.; Zhong, W.; Tang, K.; Quan, Z. The CT assessment of uncovertebral joints degeneration in a healthy population. Eur. J. Med. Res. 2021, 26, 145. [Google Scholar] [CrossRef]
- Henning, S.; Weston, M.; David, M. Surgical approaches and applied anatomy of the wrist. Orthop. Trauma 2021, 35, 174–179. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 1988. [Google Scholar]
- Ryan, T.P. Sample Size Determination and Power; Wiley: Hoboken, NJ, USA, 2013. [Google Scholar]
- Penteado, F.T.; Dos Santos, J.B.; Caporrino, F.A.; de Moraes, V.Y.; Belloti, J.C.; Faloppa, F. Scaphoid nonunion advanced collapse classifications: A reliability study. J. Hand Microsurg. 2012, 4, 12–15. [Google Scholar] [CrossRef]
- Watson, H.K.; Ballet, F.L. The SLAC wrist: Scapholunate advanced collapse pattern of degenerative arthritis. J. Hand Surg. Am. 1984, 9, 358–365. [Google Scholar] [CrossRef]
- Shin, E.K. Impaction Syndromes About the Wrist. Curr. Rev. Musculoskelet. Med. 2023, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mirza, A.; Mirza, J.B.; Zappia, L.C.; Thomas, T.L. Ulnar-Sided Wrist Pain: A Diagnostic Evaluation Guide From 30-Plus Years of Experience. Cureus 2024, 16, e53332. [Google Scholar] [CrossRef]
- Morway, G.R.; Miller, A. Clinical and Radiographic Evaluation of Ulnar-Sided Wrist Pain. Curr. Rev. Musculoskelet. Med. 2022, 15, 590–596. [Google Scholar] [CrossRef]
- Dharap, A.S.; Al-Hashimi, H.; Kassab, S.; Abu-Hijleh, M.F. The hamate facet of the lunate: A radiographic study in an Arab population from Bahrain. Surg. Radiol. Anat. 2006, 28, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Etli, I.; Kozaci, N.; Avci, M.; Karakoyun, O.F. Comparison of the diagnostic accuracy of X-ray and computed tomography in patients with wrist injury. Injury 2020, 51, 651–655. [Google Scholar] [CrossRef] [PubMed]
- Klose-Jensen, R.; Therkildsen, J.; Blavnsfeldt, A.G.; Langdahl, B.L.; Zejden, A.; Thygesen, J.; Keller, K.K.; Hauge, E.M. Diagnostic accuracy of high-resolution peripheral quantitative computed tomography and X-ray for classifying erosive rheumatoid arthritis. Rheumatology 2022, 61, 963–973. [Google Scholar] [CrossRef]
- Cámara Arrigunaga FEA-S, F.B.; Murillo Villarino, A.; Bobadilla Lescano, J.G.; Martínez Escalante, F.A.; Balam May, A. Correlation of the Kellgren-Lawrence Scale with the Outerbridge Classification in Patients with Chronic Gonalgia. Rev. Columbiana De Ortop. Y Traumatol. 2020, 34, 160–166. [Google Scholar]
- Galley, I.; Bain, G.I.; McLean, J.M. Influence of lunate type on scaphoid kinematics. J. Hand Surg. Am. 2007, 32, 842–847. [Google Scholar] [CrossRef]
- Rachunek, K.; Springer, F.; Barczak, M.; Wahler, T.; Daigeler, A.; Medved, F. Lunate morphology: Association with the severity of scapholunate ligament injuries and carpal instability patterns. J. Plast. Surg. Hand Surg. 2022, 56, 151–159. [Google Scholar] [CrossRef]
- Harley, B.J.; Werner, F.W.; Boles, S.D.; Palmer, A.K. Arthroscopic resection of arthrosis of the proximal hamate: A clinical and biomechanical study. J. Hand Surg. Am. 2004, 29, 661–667. [Google Scholar] [CrossRef]
- Zhang, G.; Wang, S.; Xu, S.; Guan, F.; Bai, Z.; Mao, H. The Effect of Formalin Preservation Time and Temperature on the Material Properties of Bovine Femoral Cortical Bone Tissue. Ann. Biomed. Eng. 2019, 47, 937–952. [Google Scholar] [CrossRef] [PubMed]
- Nowakowski, A.M.; Deyhle, H.; Zander, S.; Leumann, A.; Muller-Gerbl, M. Micro CT analysis of the subarticular bone structure in the area of the talar trochlea. Surg. Radiol. Anat. 2013, 35, 283–293. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Willett, T.L.; Kandel, R.; De Croos, J.N.; Avery, N.C.; Grynpas, M.D. Enhanced levels of non-enzymatic glycation and pentosidine crosslinking in spontaneous osteoarthritis progression. Osteoarthr. Cartil. 2012, 20, 736–744. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cerezal, L.; del Pinal, F.; Abascal, F.; Garcia-Valtuille, R.; Pereda, T.; Canga, A. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics 2002, 22, 105–121. [Google Scholar] [CrossRef]

| Grade of Osteoarthritis | Radiographic Evidence of Osteoarthritis |
|---|---|
| 0 | none |
| 1 | doubtful |
| 2 | minimal |
| 3 | moderate |
| 4 | severe |
| Grade of Osteoarthritis | Surface Description of Articular Cartilage and Diameter of Lesion |
|---|---|
| 0 | normal cartilage |
| 1 | chondral lesions characterized by softening and swelling |
| 2 | partial-thickness defect with fissures not exceeding 1.3 cm in diameter and not reaching the subchondral bone |
| 3 | Fissures of the cartilage >1.3 cm in diameter reaching the subchondral bone |
| 4 | erosion of the articular cartilage that exposes subchondral bone |
| Type 1 | Type 2 | |
|---|---|---|
| X-ray | 44 (74.6%) | 15 (25.4%) |
| CT arthrography | 43 (71.7%) | 17 (28.3%) |
| In situ | 23 (42.6%) | 31 (57.4%) |
| Luntate Type | Total | Overall Percentage of Osteoarthritis | Arthrosis Grade | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||
| In situ | 1 | 42.6% (n = 23) | 60.9% | 0.0% (n = 0) 1 | 17.4% (n = 4) 1 | 39.1% (n = 9) 1 | 4.3% (n = 1) 1 |
| 2 | 57.4% (n = 31) | 87.1% | 0.0% (n = 0) 1 | 16.1% (n = 5) 1 | 48.4% (n = 15) 1 | 22.6% (n = 7) 1 | |
| X-Ray | 1a | 54.3% (n = 32) | 65.6% | 18.8% (n = 6) 2 | 43.8% (n = 14) 2 | 3.1% (n = 1) 2 | 0% (n = 0) 2 |
| 1b | 20.3% (n = 12) | 100% | 16.7% (n = 2) 2 | 58.3% (n = 7) 2 | 16.7% (n = 2) 2 | 8.3% (n = 1) 2 | |
| 2 | 25.4% (n = 15) | 100% | 0% (n = 0) 2 | 60% (n = 9) 2 | 26.7% (n = 4) 2 | 13.3% (n = 2) 2 | |
| CT | 1a | 53.3% (n = 32) | 65.6% | 31.3% (n = 10) 2 | 31.3% (n = 10) 2 | 3.1% (n = 1) 2 | 0.0% (n = 0) 2 |
| 1b | 18.3% (n = 11) | 100% | 18.2% (n = 2) 2 | 54.5% (n = 6) 2 | 18.2% (n = 2) 2 | 9.1% (n = 1) 2 | |
| 2 | 28.3% (n = 17) | 100% | 0.0% (n = 0) 2 | 64.7% (n = 11) 2 | 23.5% (n = 4) 2 | 11.8% (n = 2) 2 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demmer, W.; Fialka, L.K.; Waschke, J.; Mesas Aranda, I.; Haas-Lützenberger, E.; Giunta, R.; Reidler, P. More than Just Type 1 or Type 2: Radiologically and Anatomically Refined Lunate Classification Correlating Ulnar Carpal Alignment and Hamate-Lunate Osteoarthrosis. J. Funct. Morphol. Kinesiol. 2025, 10, 141. https://doi.org/10.3390/jfmk10020141
Demmer W, Fialka LK, Waschke J, Mesas Aranda I, Haas-Lützenberger E, Giunta R, Reidler P. More than Just Type 1 or Type 2: Radiologically and Anatomically Refined Lunate Classification Correlating Ulnar Carpal Alignment and Hamate-Lunate Osteoarthrosis. Journal of Functional Morphology and Kinesiology. 2025; 10(2):141. https://doi.org/10.3390/jfmk10020141
Chicago/Turabian StyleDemmer, Wolfram, Lia K. Fialka, Jens Waschke, Irene Mesas Aranda, Elisabeth Haas-Lützenberger, Riccardo Giunta, and Paul Reidler. 2025. "More than Just Type 1 or Type 2: Radiologically and Anatomically Refined Lunate Classification Correlating Ulnar Carpal Alignment and Hamate-Lunate Osteoarthrosis" Journal of Functional Morphology and Kinesiology 10, no. 2: 141. https://doi.org/10.3390/jfmk10020141
APA StyleDemmer, W., Fialka, L. K., Waschke, J., Mesas Aranda, I., Haas-Lützenberger, E., Giunta, R., & Reidler, P. (2025). More than Just Type 1 or Type 2: Radiologically and Anatomically Refined Lunate Classification Correlating Ulnar Carpal Alignment and Hamate-Lunate Osteoarthrosis. Journal of Functional Morphology and Kinesiology, 10(2), 141. https://doi.org/10.3390/jfmk10020141






