Posture Status Differences Between Preschool Boys and Girls
Abstract
1. Introduction
2. Materials and Methods
2.1. The Sample of Participants
2.2. Testing Protocol
2.2.1. Anthropometry
2.2.2. Body Composition
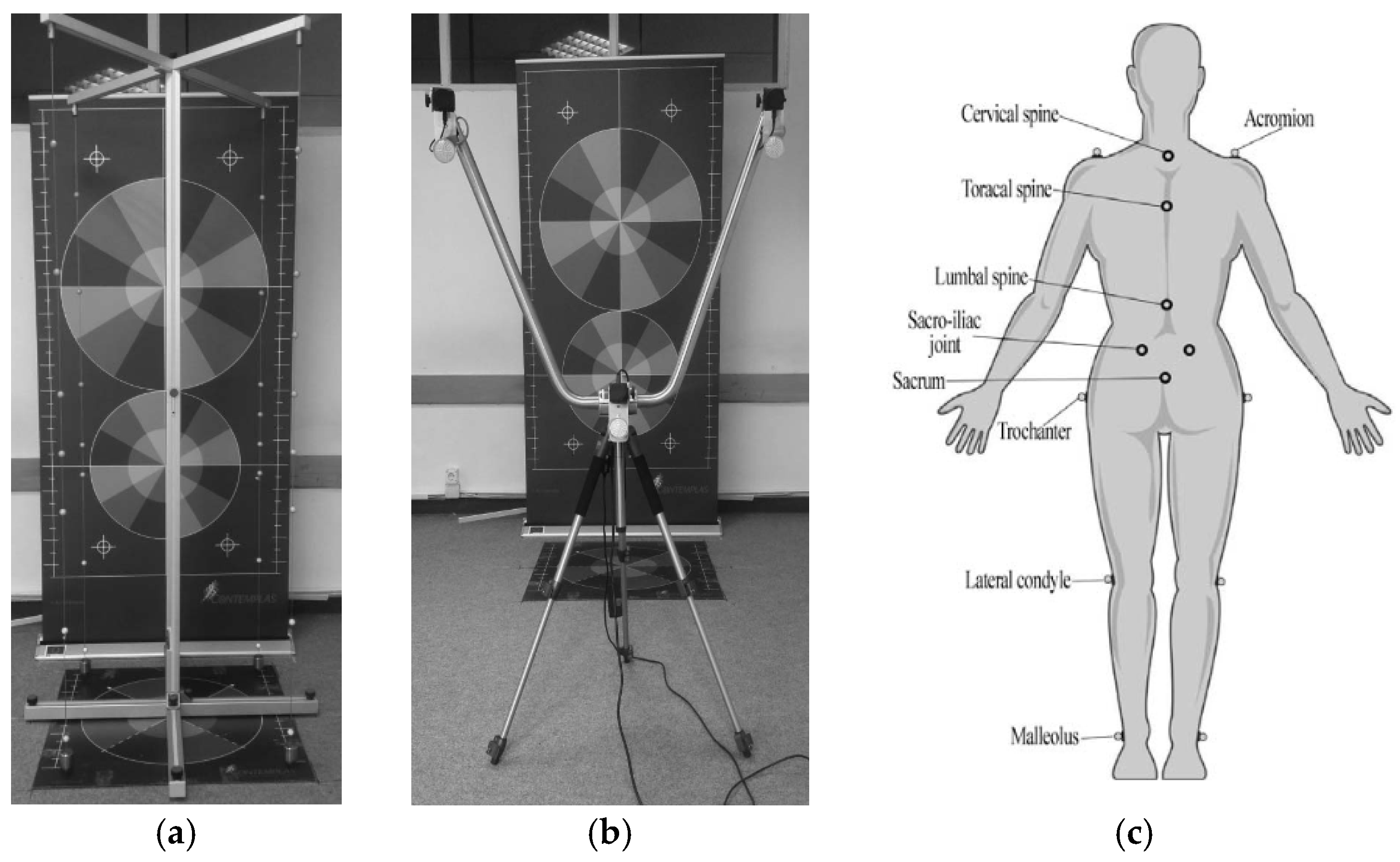
2.2.3. Posture Assessment
- Sample of variables
2.3. Statistical Analysis
3. Results
4. Discussion
- Conducting cross-cultural research that would enable the comparison of results among children from different environments and cultural contexts, which would determine eventual differences and specificities in the development of postural characteristics.
- Including a larger sample of participants in future research, including children from rural and urban areas, to ensure the representativeness and generalizability of the results.
- Conducting a longitudinal study that would follow the postural characteristics of children through different developmental stages, aiming to identify critical periods for intervention and determine more precisely developmental trends in the context of gender differences.
- Conducting research with a larger sample of subjects and by including factors of physical activity and lateralization could provide more detailed insights into these variables and enable a better understanding of their influence on postural status.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Skender, N.; Pistotnik, B.; Čolakhodžić, E. Basics of Movement in Sports; Faculty of Education, University of Bihać: Bihać, Bosnia and Herzegovina, 2007. [Google Scholar]
- Augustinović, I.; Halilović, S.; Dobrić, A.; Kovačevska, K.; Kovač, L.; Matošević, L.; Kosterović, A.; Begović, H.; Jakešević, B.; Barnjak, T.; et al. The Present Development Program of Pre-School Upbringing and Education of the Canton of Central Bosnia; Ministry of Education, Science, Culture and Sports of the Canton of Central Bosnia/Central Bosnia Canton: Travnik, Bosnia and Herzegovina, 2018.
- Baranowska, A.; Sierakowska, M.; Owczarczuk, A.; Olejnik, B.J.; Lankau, A.; Baranowski, P. An Analysis of the Risk Factors for Postural Defects among Early School-Aged Children. J. Clin. Med. 2023, 12, 4621. [Google Scholar] [CrossRef] [PubMed]
- Plandowska, M.; Lichota, M.; Górniak, K. Postural Stability of 5-Year-Old Girls and Boys with Different Body Heights. PLoS ONE 2019, 14, e0227119. [Google Scholar] [CrossRef] [PubMed]
- Peulić, J.; Katanić, B.; Jovanović, N.; Bjelica, D. Exploring Anthropometric Characteristics, Weight Status, and Posture among Preschool Children in Serbia. J. Anthr. Sport Phys. Educ. 2024, 8, 19–24. [Google Scholar] [CrossRef]
- Rusek, W.; Baran, J.; Leszczak, J.; Adamczyk, M.; Baran, R.; Weres, A.; Inglot, G.; Czenczek-Lewandowska, E.; Pop, T. Changes in Children’s Body Composition and Posture during Puberty Growth. Children 2021, 8, 288. [Google Scholar] [CrossRef] [PubMed]
- Vranešić-Hadžimehmedović, D.; Arapović, M.; Hodžić, A.; Mašić, S. Prevalence of spinal deformities in preschool children living in the SOS children’s village in Sarajevo. Homosporticus 2024, 26, 18–24. [Google Scholar] [CrossRef]
- Standring, S. Gray’s Anatomy: The Anatomical Basis of Clinical Practice; Elsevier Churchill Livingstone: Edinburgh, UK, 2005. [Google Scholar]
- Protić-Gava, B.; Šćepanović, T. Basis of Kinesitherapy and Applied Corrective Gymnastic; University of Novi Sad: Novi Sad, Serbia, 2016. [Google Scholar]
- Madić, D. (Ed.) Improving Testing Abilities on Postural and Spinal Column Status—Spinelab; Faculty of Sport and Physical Education: Novi Sad, Serbia, 2014. [Google Scholar]
- Čović, N. The Influence of a Program of Motor Control Exercises on Body Composition, Postural Status and Motor Skills in Young Athletes. Ph.D. Thesis, Faculty of Sports and Physical Education, University of Sarajevo, Sarajevo, Bosnia and Herzegovina, 2020. [Google Scholar]
- McEvoy, M.P.; Grimmer, K. Reliability of Upright Posture Measurements in Primary School Children. Biomed. Cent. Ser. Musculoskelet. Disord. 2005, 29, 6. [Google Scholar] [CrossRef]
- Romanov, R.; Stupar, D.; Međedović, B.; Brkin, D. Postural Status of Preschool Children in the Territory of Novi Sad. TIMS Acta 2014, 8, 129–135. [Google Scholar] [CrossRef]
- Sabo, E. Postural Status of Preschool Children in Novi Sad. Pedagog. Real. 2006, 54, 108–113. [Google Scholar]
- Džibrić, D. Differences in Morphological and Postural Status between Primary School Males and Females. Sport Sci. Pract. Asp. 2019, 16, 2. [Google Scholar] [CrossRef]
- Kolybacz, A.; Niewiem, M.; Buczyńska, A.; Woś, H. Health Status of 9-Year-Old Children in Katowice. Stand. With. Pediatr. 2019, 16, 537–554. (In Polish) [Google Scholar]
- Glavaš, J.; Rumboldt, M.; Karin, Ž.; Matković, R.; Kresina, S.; Dragaš-Zubalj, N.; Aljinović, J. The role of school medicine in the early detection and management of adolescent idiopathic scoliosis. Wien. Klin. Wochenschr. 2023, 135, 273–281. [Google Scholar] [CrossRef]
- Rusnák, R.; Kolarová, M.; Aštaryová, I.; Kutiš, P. Screening and Early Identification of Spinal Deformities and Posture in 311 Children: Results from 16 Districts in Slovakia. Rehabil. Res. Pract. 2019, 2019, 4758386. [Google Scholar] [CrossRef] [PubMed]
- Miletić, A.; Protić-Gava, B. Gender-Related Morphological Characteristics in Preschool Children of Kolubara District. EQOL J. 2017, 9, 31–36. [Google Scholar] [CrossRef]
- Kovač, S.; Kajmović, H.; Rađo, I.; Manić, G. Trend Projections of Body Deformities Occurrence between the Ages of 5 and 12, Metrically Objectified and Estimated by 3D Postural Status Screening. Sporty Man 2014, 16, 5–13. [Google Scholar]
- Kovač, S.; Kapo, S.; Alić, H.; Manić, G. Postural Quality Analyses for Children Recorded in Kinematic 2D and 3D Contemplas Method. Tech. Technol. Educ. Manag. 2015, 10, 99–106K. [Google Scholar]
- Kapo, S.; Rađo, I.; Smajlović, N.; Kovač, R.; Talović, M.; Doder, L.; Čović, N. Increasing Postural Deformity Trends and Body Mass Index Analysis in School-Age Children. Slov. J. Public Health 2018, 57, 1. [Google Scholar] [CrossRef]
- Bićanin, P.; Milenković, S.; Radovanović, D.; Gajević, A.; Ivanović, J. Postural Disorders in Preschool Children in Relation to Gender. Univ. Facts Phys. Educ. Sports 2017, 15, 1–10. [Google Scholar] [CrossRef]
- Mitova, S. Frequency and Prevalence of the Postural Disorders and Spinal Deformities in the Children of Primary School Age. Res. Kinesiol. 2015, 43, 21–24. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Tanita Corporation. BC-420MA Body Composition Monitor Instruction Manual; Tanita Corporation: Tokyo, Japan, 2015. [Google Scholar]
- Widhalm, K.; Durstberger, S.; Greisberger, A.; Wolf, B.; Putz, P. Validity of Assessing Level Walking with the 2D Motion Analysis Software TEMPLO and Reliability of 3D Marker Application. Sci. Rep. 2024, 14, 1427. [Google Scholar] [CrossRef]
- Šćepanović, T.; Marinković, D.; Korovljev, D.; Madić, D. The Status of the Spine in the Sagittal Plane in Girls. In Proceedings of the 5th International Scientific Conference Contemporary Kinesiology, Split, Croatia, 28–30 August 2015. [Google Scholar]
- Ćirić, A.; Čaušević, D.; Bejdić, A. Differences in Postural Status between Boys and Girls Aged 6–9 Years Recorded with the 3D Method of the Measuring Instrument Contemplas. Homosporticus 2015, 17, 15–20. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect Size Estimates: Current Use, Calculations, and Interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Tomczak, M.; Tomczak, E. The Need to Report Effect Size Estimates Revisited: An Overview of Some Recommended Measures of Effect Size. Trends Sport Sci. 2014, 21, 19–25. [Google Scholar]
- Dop, D.; Pădureanu, V.; Pădureanu, R.; Niculescu, S.-A.; Drăgoescu, A.N.; Moroșanu, A.; Mateescu, D.; Niculescu, C.E.; Marcu, I.R. Risk Factors Involved in Postural Disorders in Children and Adolescents. Life 2024, 14, 1463. [Google Scholar] [CrossRef]
- Yang, L.; Lu, X.; Yan, B.; Huang, Y. Prevalence of Incorrect Posture among Children and Adolescents: Finding from a Large Population-Based Study in China. iScience. 2020, 23, 101043. [Google Scholar] [CrossRef]
- Kolarova, M.; Kutiš, P.; Rusnak, R.; Hrčková, Z.; Hudáková, Z.; Lysá, L.; Luliak, M.; Babel’a, R. Analysis of Body Segments and Postural State in School Children. Neuroendocrinol. Lett. 2019, 40 (Suppl. S1), 17–23. [Google Scholar]
- Batistão, M.V.; Carreira Moreira, R.F.; Cote Gil Coury, H.J.; Salasar, L.E.B.; Sato, T.O. Prevalence of Postural Deviations and Associated Factors in Children and Adolescents: A Cross-Sectional Study. Fisioter. Mov. 2016, 29, 777–785. [Google Scholar] [CrossRef]
- Maciałczyk-Paprocka, K.; Stawińska-Witoszyńska, B.; Kotwicki, T.; Sowińska, A.; Krzyżaniak, A.; Walkowiak, J.; Krzywińska-Wiewiorowska, M. Prevalence of incorrect body posture in children and adolescents with overweight and obesity. Eur. J. Pediatr. 2017, 176, 563–572. [Google Scholar] [CrossRef]
- Bubanj, S.; Đorđević, S.; Milenković, S.; Stanković, R.; Vidojević, M.; Đokić, M. Postural Disorders and Muscle Power in Primary School Children. Acta Fac. Medicae Naissensis 2021, 38, 270–278. [Google Scholar]
- Penha, P.J.; Casarotto, R.A.; Sacco, I.C.N.; Marques, A.P.; João, S.M.A. Qualitative Postural Analysis among Boys and Girls of Seven to Ten Years of Age. Braz. J. Phys. Ther. 2008, 12, 386–391. [Google Scholar] [CrossRef]
- Coelho, J.J.; Graciosa, M.D.; de Medeiros, D.L.; Pacheco, S.C.; da Costa, L.M.; Ries, L.G. Influence of Flexibility and Gender on the Posture of School Children. Rev. Paul. Pediatr. 2014, 32, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Mizukoshi, R.; Yagi, M.; Yamada, Y.; Yokoyama, Y.; Yamada, M.; Watanabe, K.; Nakamura, M.; Nagura, T.; Jinzaki, M. Gender Differences in Spinal Mobility During Postural Changes: A Detailed Analysis Using Upright CT. Sci. Rep. 2024, 14, 9154. [Google Scholar] [CrossRef]
- Smith, A.W.; Ulmer, F.F.; Wong, D.P. Gender Differences in Postural Stability Among Children. J. Hum. Kinet. 2012, 33, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Gajić, D. Kinesitherapy in Spine Deformity. Master’s Thesis, Faculty of Health Care, Pan-European University, Banja Luka, Bosnia and Herzegovina, 2009. [Google Scholar]
- Đorđević, S.; Jorgić, B.; Milenković, S.; Stanković, R.; Stanković, M. The Incidence of Spinal Postural Disorders in First-Grade Elementary-School Students. Facta Univ. Ser. Phys. Educ. Sport 2020, 18, 381–390. [Google Scholar] [CrossRef]
- Đorđević, S.; Stanković, M.; Jorgić, B.; Milenković, S.; Smailović, S.; Katanić, B.; Jelaska, I.; Pezelj, L. The Association of Sagittal Spinal Posture among Elementary School Pupils with Sex and Grade. Children 2024, 11, 446. [Google Scholar] [CrossRef]
- Wojtków, M.; Szkoda-Poliszuk, K.; Szotek, S. Influence of Body Posture on Foot Load Distribution in Young School-Age Children. Acta Bioeng. Biomech. 2018, 20, 101–107. [Google Scholar]
- Poussa, M.S.; Heliövaara, M.M.; Seitsamo, J.T.; Könönen, M.H.; Hurmerinta, K.A.; Nissinen, M.J. Development of Spinal Posture in a Cohort of Children from the Age of 11 to 22 Years. Eur. Spine J. 2005, 14, 738–742. [Google Scholar] [CrossRef]
- Skender, N.; Kurtović, N.; Kovač, S.; Šabić, E.; Ćeleš, N. Two Different Methods Comparative Analysis of Determining Body Deformities in Students. Homosporticus 2023, 25, 18–23. [Google Scholar] [CrossRef]
- Kojić, M. Differences in Indicators of Postural Status between Boys and Girls from Srem. Exerc. Qual. Life 2014, 6, 17–22. [Google Scholar]
- Ng, S.Y.; Bettany-Saltikov, J. Imaging in the Diagnosis and Monitoring of Children with Idiopathic Scoliosis. Open Orthop. J. 2017, 11, 1500–1520. [Google Scholar] [CrossRef]
- Weigel, S.; Dullien, S.; Grifka, J.; Jansen, P. Comparison Between Rasterstereographic Scan and Orthopedic Examination for Posture Assessment: An Observational Study. Front. Surg. 2024, 11, 1461569. [Google Scholar] [CrossRef] [PubMed]
- Kutanzi, K.R.; Lumen, A.; Koturbash, I.; Miousse, I.R. Pediatric Exposures to Ionizing Radiation: Carcinogenic Considerations. Int. J. Environ. Res. Public Health 2016, 13, 1057. [Google Scholar] [CrossRef] [PubMed]
- Inoue, D.; Shigematsu, H.; Nakagawa, Y.; Takeshima, T.; Tanaka, Y. The Influence of Posture on Instability Evaluation Using Flexion-Extension X-Ray Imaging in Lumbar Spondylolisthesis. Asian Spine J. 2021, 15, 308–316. [Google Scholar] [CrossRef]
- Dorfman, A.L.; Fazel, R.; Einstein, A.J.; Applegate, K.E.; Krumholz, H.M.; Wang, Y.; Christodoulou, E.; Chen, J.; Sanchez, R.; Nallamothu, B.K. Use of Medical Imaging Procedures with Ionizing Radiation in Children: A Population-Based Study. Arch. Pediatr. Adolesc. Med. 2011, 165, 458–464. [Google Scholar] [CrossRef]
- Dreischarf, M.; Pries, E.; Bashkuev, M.; Putzier, M.; Schmidt, H. Differences Between Clinical “Snap-Shot” and “Real-Life” Assessments of Lumbar Spine Alignment and Motion—What Is the “Real” Lumbar Lordosis of a Human Being? J. Biomech. 2016, 49, 638–644. [Google Scholar] [CrossRef]
- Sugiyama, N.; Kai, Y.; Koda, H.; Morihara, T.; Kida, N. Agreement in the Postural Assessment of Older Adults by Physical Therapists Using Clinical and Imaging Methods. Geriatrics 2024, 9, 40. [Google Scholar] [CrossRef] [PubMed]
- Hébert-Losier, K.; Abd Rahman, F. Reliability of postural measures in elite badminton players using Posture Pro 8. Physiother. Theory Pract. 2017, 34, 483–494. [Google Scholar] [CrossRef]
- Van Niekerk, S.M.; Louw, Q.; Vaughan, C.; Grimmer-Somers, K.; Schreve, K. Photographic measurement of upper-body sitting posture of high school students: A reliability and validity study. BMC Musculoskelet. Disord. 2008, 9, 113. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I.; Vaz, J.R. Reliability and validity of angular measures through the software for postural assessment. Rehabilitación 2013, 47, 223–228. [Google Scholar]
- Ha, S.M.; Kwon, O.Y.; Weon, J.H.; Kim, M.H.; Kim, S.J. Reliability and validity of goniometric and photographic measurements of clavicular tilt angle. Man. Ther. 2013, 18, 367–371. [Google Scholar] [CrossRef]
- Alam, M.F.; Zaki, S.; Sharma, S.; Nuhmani, S. Establishing the Reliability of the GaitON Motion Analysis System: A Foundational Study for Gait and Posture Analysis in a Healthy Population. Sensors 2024, 24, 6884. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, O.; Hammes, A.; Kelm, J.; Schmitt, E. Assessment of the posture of adolescents in everyday clinical practice: Intra-rater and inter-rater reliability and validity of a posture index. J. Bodyw. Mov. Ther. 2016, 20, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Roggio, F.; Ravalli, S.; Maugeri, G.; Bianco, A.; Palma, A.; Di Rosa, M.; Musumeci, G. Technological Advancements in the Analysis of Human Motion and Posture Management through Digital Devices. World J. Orthop. 2021, 12, 467–484. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Thoracic and Lumbar Posture Behaviour in Sitting Tasks and Standing: Progressing the Biomechanics from Observations to Measurements. Appl. Ergon. 2016, 53, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Straker, L.M.; O’Sullivan, P.B.; Smith, A.; Perry, M. Computer Use and Habitual Spinal Posture in Australian Adolescents. Public Health Rep. 2007, 122, 634. [Google Scholar] [CrossRef]
- Simov, S.B.; Milinić, S.M.; Stojanović, D.O. Frequency of Poor Posture and Flat Feet in Preschool Children. Apollo Med. Aescul. 2011, 9, 5–8. [Google Scholar]
- Slováková, M.; Mandzáková, M. Effect of an exercise program on the body posture of young school-aged pupils. J. Phys. Educ. Sport 2024, 24, 747–753. [Google Scholar] [CrossRef]
- Araújo, C.L.; Moreira, A.; Carvalho, G.S. Postural Education Programmes with School Children: A Scoping Review. Sustainability 2023, 15, 10422. [Google Scholar] [CrossRef]
- Miñana-Signes, V.; Monfort-Pañego, M.; Valiente, J. Teaching Back Health in the School Setting: A Systematic Review of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2021, 18, 979. [Google Scholar] [CrossRef]
- Lopez-Fuenzalida, A.; Rodriguez Channels, C.; Reyes Ponce, A.; Contreras Molina, A.; Quezada, J.F.; Polanco, C.A. Association between Nutritional Status and Flat Foot Prevalence in Chilean Children from 6 to 10 Years of Age. Nutr. Hosp. 2016, 33, 249–254. [Google Scholar] [CrossRef]
- Fernandes, O.; Basilio, F. Tai Chi training can improve postural control. Rev. Artes Marciales Asiáticas 2016, 11, 42–43. [Google Scholar] [CrossRef]
- Wąsik, J.; Motow-Czyz, M. Comparative analysis of body posture in child and adolescent taekwon-do practitioners and non-practitioners. Ido Mov. Cult. J. Martial Arts Anthropol. 2015, 15, 35–40. [Google Scholar] [CrossRef]
- Kojić, F.; Arsenijević, R.; Grujić, G.; Toskić, L.; Šimenko, J. Effects of Structured Physical Activity on Motor Fitness in Preschool Children. Children 2024, 11, 433. [Google Scholar] [CrossRef] [PubMed]
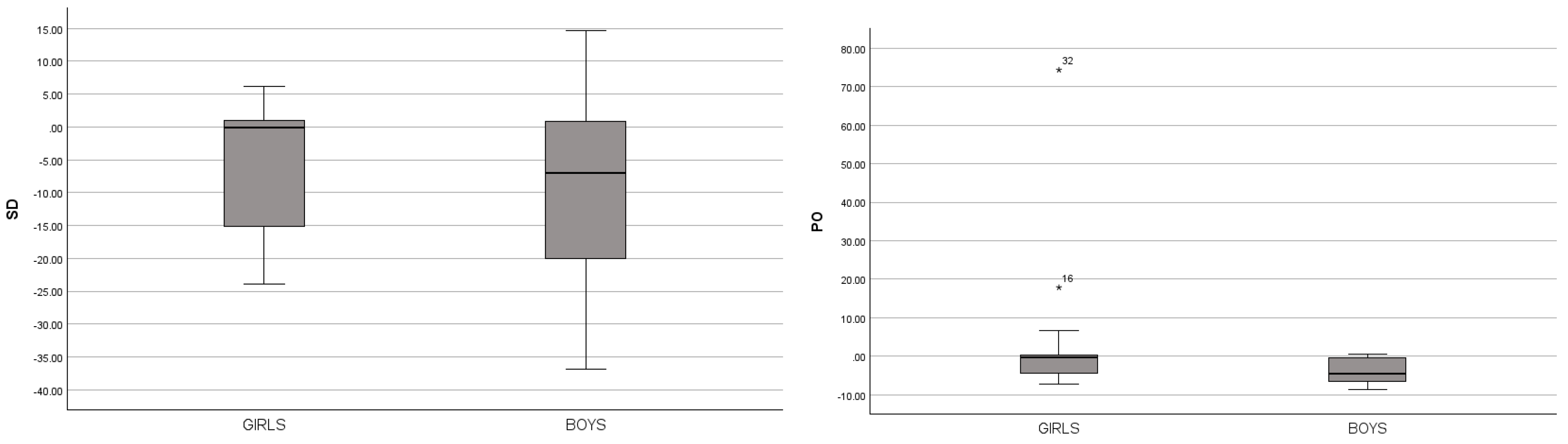
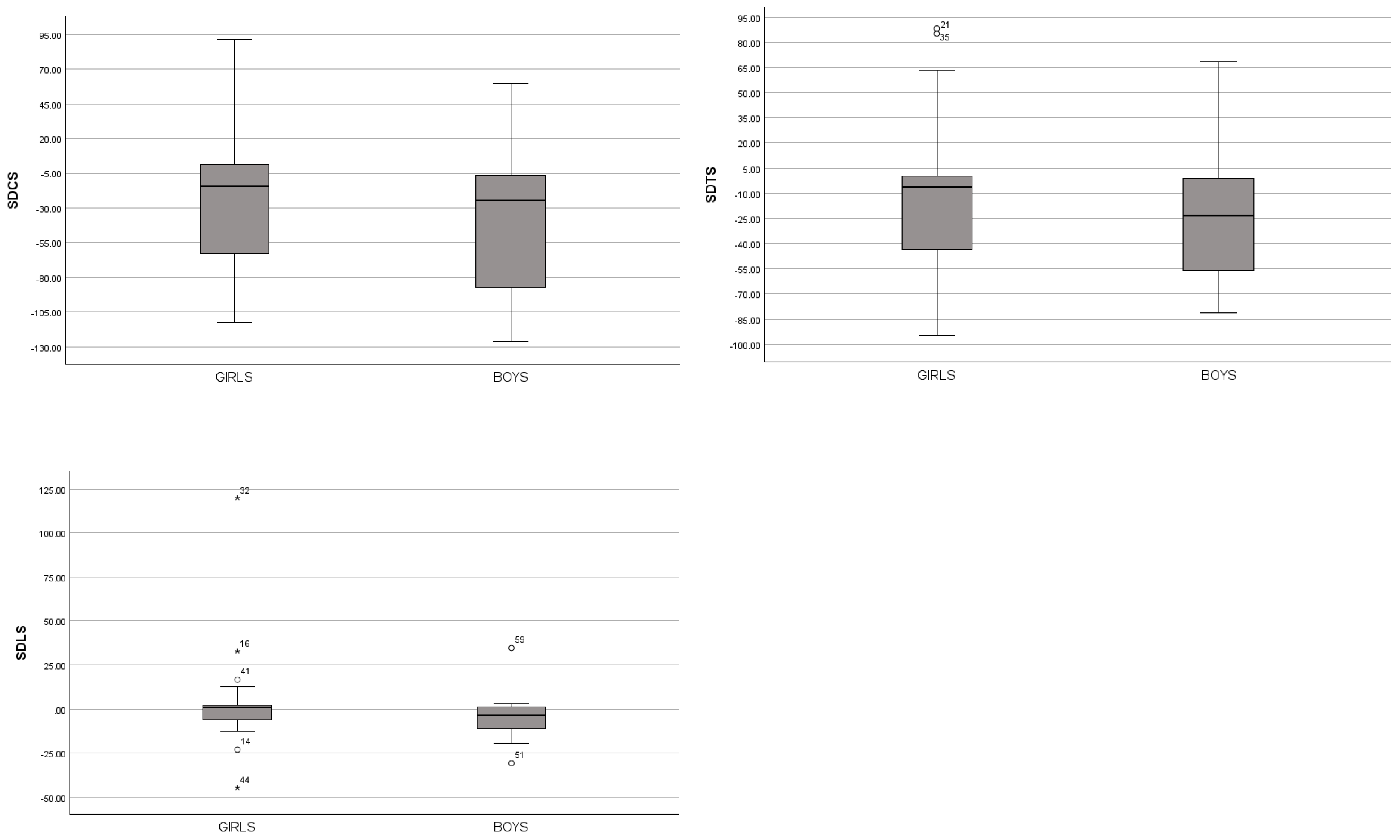
| Variables | Girls | Boys | Mean Rank | U | Z | p | r | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SDv | Mean | SDv | Girls | Boys | |||||
| SD (cm) | −4.7 | 8.78 | −9.94 | 12.32 | 52.0 | 41.0 | 803.5 | −1.99 | 0.047 * | 0.21 |
| PO (cm) | 0.49 | 11.8 | −3.62 | 3.06 | 56.4 | 36.6 | 603.5 | −3.55 | 0.000 * | 0.37 |
| SR (°) | 26.95 | 42.4 | 32.6 | 46.13 | 44.8 | 48.2 | 981.5 | −0.60 | 0.550 | 0.06 |
| PR (°) | 26.6 | 45.9 | 27.26 | 53.88 | 47.9 | 45.1 | 994.5 | −0.50 | 0.620 | 0.05 |
| TR (°) | 40.87 | 47.4 | 49.99 | 58.69 | 43.9 | 49.1 | 937.5 | −0.94 | 0.347 | 0.10 |
| CR (°) | 4.17 | 55.1 | 16.84 | 73.68 | 42.1 | 50.9 | 857.5 | −1.57 | 0.117 | 0.16 |
| SDCS (cm) | −18.1 | 45.7 | −44.7 | 48.98 | 52.6 | 40.4 | 778.5 | −2.18 | 0.029 * | 0.23 |
| SDTS (cm) | −8.67 | 37.9 | −27.8 | 33.21 | 53.2 | 39.8 | 748.5 | −2.42 | 0.016 * | 0.25 |
| SDLS (cm) | 1.75 | 20.7 | −4.85 | 9.69 | 54.3 | 38.7 | 699.5 | −2.80 | 0.005 * | 0.29 |
| VVL (°) | 10.47 | 84.3 | 22.12 | 62.22 | 41.9 | 51.1 | 848.5 | −1.64 | 0.102 | 0.17 |
| VVR (°) | −27.1 | 92 | −46.1 | 101.1 | 48.0 | 45.0 | 987.5 | −0.55 | 0.582 | 0.06 |
| FEL (°) | 5.34 | 74.1 | −14.8 | 68.07 | 47.5 | 45.5 | 1014 | −0.35 | 0.728 | 0.04 |
| FER (°) | −36.1 | 91.7 | −53.3 | 101.2 | 49.3 | 43.7 | 927.5 | −1.02 | 0.308 | 0.11 |
| CS (cm) | 0.22 | 14.7 | −0.59 | 27.89 | 48.3 | 44.7 | 975.5 | −0.64 | 0.519 | 0.07 |
| TS (cm) | 2.4 | 11.5 | 2.99 | 26.67 | 49.5 | 43.5 | 921.5 | −1.07 | 0.286 | 0.11 |
| LS (cm) | 1.14 | 7.13 | 2.97 | 14.62 | 49.4 | 43.6 | 926 | −1.03 | 0.303 | 0.11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kapo-Gurda, A.; Efendić, A.; Mahmutović, I.; Kovač, S.; Kajmović, H.; Kapo, S.; Šimenko, J. Posture Status Differences Between Preschool Boys and Girls. J. Funct. Morphol. Kinesiol. 2025, 10, 101. https://doi.org/10.3390/jfmk10020101
Kapo-Gurda A, Efendić A, Mahmutović I, Kovač S, Kajmović H, Kapo S, Šimenko J. Posture Status Differences Between Preschool Boys and Girls. Journal of Functional Morphology and Kinesiology. 2025; 10(2):101. https://doi.org/10.3390/jfmk10020101
Chicago/Turabian StyleKapo-Gurda, Anida, Amin Efendić, Indira Mahmutović, Siniša Kovač, Husnija Kajmović, Safet Kapo, and Jožef Šimenko. 2025. "Posture Status Differences Between Preschool Boys and Girls" Journal of Functional Morphology and Kinesiology 10, no. 2: 101. https://doi.org/10.3390/jfmk10020101
APA StyleKapo-Gurda, A., Efendić, A., Mahmutović, I., Kovač, S., Kajmović, H., Kapo, S., & Šimenko, J. (2025). Posture Status Differences Between Preschool Boys and Girls. Journal of Functional Morphology and Kinesiology, 10(2), 101. https://doi.org/10.3390/jfmk10020101









