Optimizing Running Mechanics, Effects of Cadence, Footwear, and Orthoses on Force Distribution: A Quasi-Experimental Study
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Design
- C0 (Reference Condition): Rearfoot-to-toe drop of 10 mm, no cadence adjustment, no orthotics.
- C1 (Cadence only): 10 mm rearfoot-to-toe drop, 10% increase in cadence, no orthotics.
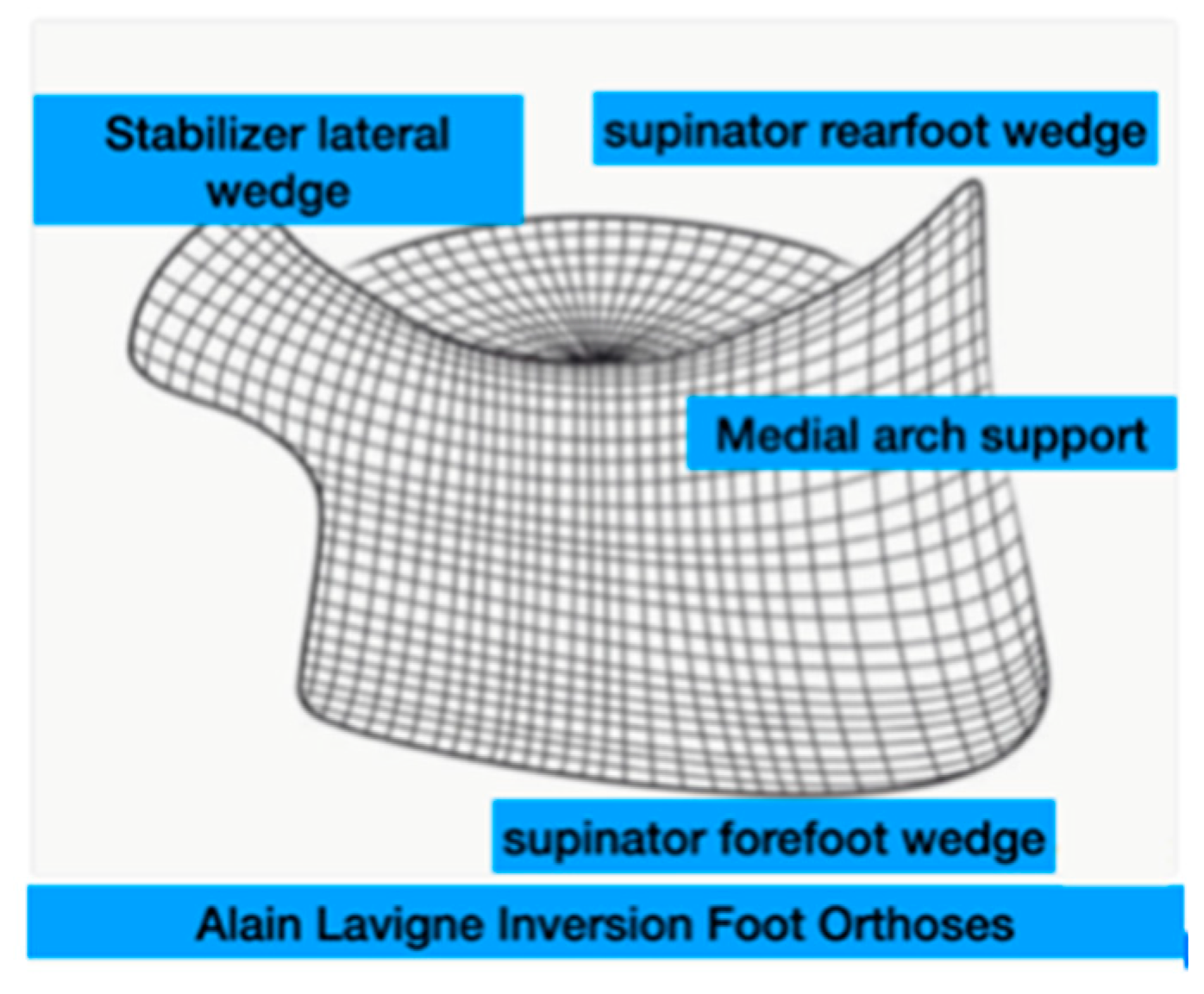
- C2 (Plantar orthoses): 10 mm rearfoot-to-toe drop and Alain Lavigne Inversion Foot Orthoses (ALIFOrthoses) [31].
- C3 (Asics Noosa shoe): 5 mm rearfoot-to-toe drop, no orthotics. The low drop favors a plantar attack on the forefoot or midfoot, which can modify the forces exerted on the rearfoot compared to high-drop shoes [32].
- C4 (Cross-interventions): 10% increase in cadence, ALIFOrthoses, 5-mm rearfoot-to-toe drop.
2.3. Participants
- Age ≥ 18 years.
- Recreational running activity of at least 2 sessions per week (running 5 km in under 25 min).
- Habitual use of running shoes with a 10 mm drop.
- Willingness and ability to adhere to the study protocol.
- Degenerative diseases of the bones and joints (diagnosed based on medical history).
- Surgery of the lower limbs.
- Recent knee or ankle injuries or serious foot injuries that may have left morphological changes.
- Painful skin conditions (e.g., calluses, plantar warts).
- Lower-limb injuries in the past 6 months (verified by self-report).
2.4. Procedure
2.5. Experimental Conditions
2.6. Sample Size
2.7. Statistical Analysis
3. Results
3.1. Overview of Key Findings
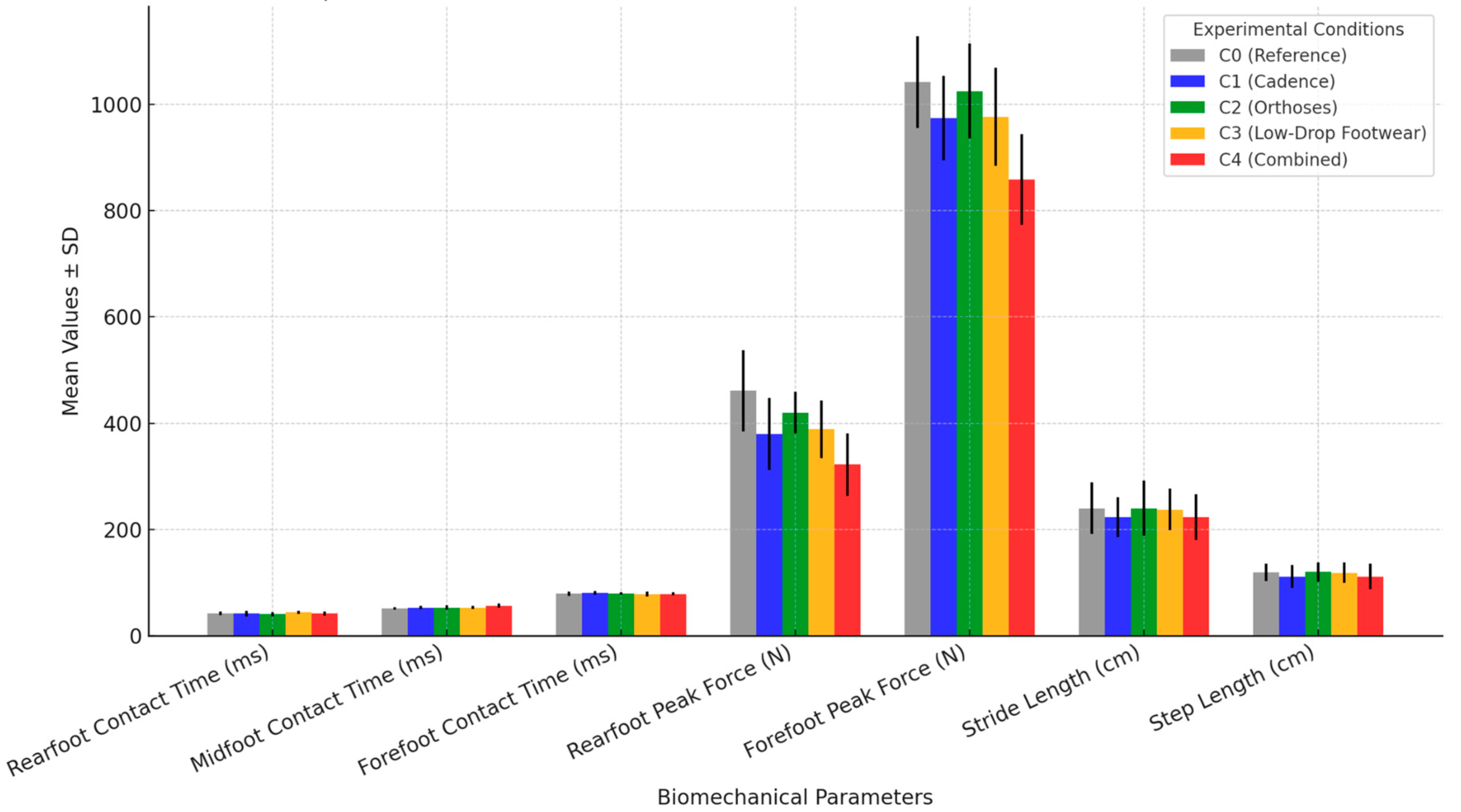
- Cadence adjustment (C1) and the combined intervention (C4) showed the most pronounced reductions in rearfoot peak force, while footwear changes primarily influenced midfoot contact time.
- The combined intervention (C4) produced the largest reduction in rearfoot impact (−139.09 N, p < 0.001), suggesting it may be the most effective strategy for minimizing joint stress in runners.
- Footwear modification (C3) led to an increase in midfoot contact time (+1.98 ms), while orthoses (C2) redistributed plantar pressure with a moderate effect on rearfoot force.
- Stride length and step length were significantly reduced under conditions C1 and C4, suggesting a more compact and controlled gait pattern.
3.2. Spatiotemporal and Force Distribution Comparisons
3.3. Key Observations
4. Discussion
- Cadence adjustment (+10%) may be particularly beneficial for runners at high risk of overuse injuries (e.g., patellofemoral pain syndrome (PFPS) or iliotibial band syndrome (ITBS)), as it helps reduce knee-joint loading [38].
- Inversion foot orthoses (C2) could be useful for runners with excessive pronation or flat feet, as they aid in redistributing plantar pressures and reducing stress on the medial tibia and Achilles tendon.
- Low-drop footwear (C3) may help runners transition to a midfoot strike, potentially benefiting those with high-impact running mechanics but requiring careful adaptation to avoid excessive forefoot loading.
- Combined interventions (C4) could be recommended for runners needing comprehensive biomechanical optimization, particularly in rehabilitation settings or performance training programs.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The State of Trail Running 2022. RunRepeat—Athletic Shoe Reviews. Available online: https://runrepeat.com/the-state-of-trail-running-2022 (accessed on 26 February 2025).
- Hebdo N°1760-61-62—Pourquoi Court-On? Courrier International. Available online: https://www.courrierinternational.com/magazine/2024/1760-61-62-magazine (accessed on 26 December 2024).
- Correia, C.K.; Machado, J.M.; Dominski, F.H.; de Castro, M.P.; de Brito Fontana, H.; Ruschel, C. Risk factors for running-related injuries: An umbrella systematic review. J. Sport Health Sci. 2024, 13, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Aicale, R.; Tarantino, D.; Maffulli, N. Overuse injuries in sport: A comprehensive overview. J. Orthop. Surg. Res. 2018, 13, 309. [Google Scholar] [CrossRef]
- Edwards, W.B. Modeling Overuse Injuries in Sport as a Mechanical Fatigue Phenomenon. Exerc. Sport Sci. Rev. 2018, 46, 224–231. [Google Scholar] [CrossRef]
- Taunton, J.E.; Ryan, M.B.; Clement, D.B.; McKenzie, D.C.; Lloyd-Smith, D.R.; Zumbo, B.D. A retrospective case-control analysis of 2002 running injuries. Br. J. Sports Med. 2002, 36, 95–101. [Google Scholar] [CrossRef]
- Nielsen, R.O.; Cederholm, P.; Buist, I.; Sørensen, H.; Lind, M.; Rasmussen, S. Can GPS be used to detect deleterious progression in training volume among runners? J. Strength Cond. Res. 2013, 27, 1471–1478. [Google Scholar] [CrossRef]
- Lopes, A.D.; Hespanhol Júnior, L.C.; Yeung, S.S.; Costa, L.O.P. What are the main running-related musculoskeletal injuries? A Systematic Review. Sports Med. 2012, 42, 891–905. [Google Scholar] [CrossRef] [PubMed]
- Ferber, R.; Hreljac, A.; Kendall, K.D. Suspected Mechanisms in the Cause of Overuse Running Injuries. Sports Health 2009, 1, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Hreljac, A. Impact and overuse injuries in runners. Med. Sci. Sports Exerc. 2004, 36, 845–849. [Google Scholar] [CrossRef]
- Hespanhol Junior, L.C.; Pena Costa, L.O.; Lopes, A.D. Previous injuries and some training characteristics predict running-related injuries in recreational runners: A prospective cohort study. J. Physiother. 2013, 59, 263–269. [Google Scholar] [CrossRef]
- Napier, C.; Willy, R.W. The Prevention and Treatment of Running Injuries: A State of the Art. Int. J. Sports Phys. Ther. 2021, 16, 968–970. [Google Scholar] [CrossRef]
- van der Worp, M.P.; ten Haaf, D.S.M.; van Cingel, R.; de Wijer, A.; Nijhuis-van der Sanden, M.W.G.; Staal, J.B. Injuries in runners; a systematic review on risk factors and sex differences. PLoS ONE 2015, 10, e0114937. [Google Scholar] [CrossRef] [PubMed]
- Chan, Z.Y.; Zhang, J.H.; Au, I.P.; An, W.W.; Shum, G.L.; Ng, G.Y.; Cheung, R.T. Gait Retraining for the Reduction of Injury Occurrence in Novice Distance Runners: 1-Year Follow-up of a Randomized Controlled Trial. Am. J. Sports Med. 2018, 46, 388–395. [Google Scholar] [CrossRef]
- Napier, C.; Cochrane, C.K.; Taunton, J.E.; Hunt, M.A. Gait modifications to change lower extremity gait biomechanics in runners: A systematic review. Br. J. Sports Med. 2015, 49, 1382–1388. [Google Scholar] [CrossRef]
- Bredeweg, S.W.; Zijlstra, S.; Bessem, B.; Buist, I. The effectiveness of a preconditioning programme on preventing running-related injuries in novice runners: A randomised controlled trial. Br. J. Sports Med. 2012, 46, 865–870. [Google Scholar] [CrossRef] [PubMed]
- de Souza Júnior, J.R.; Rabelo, P.H.R.; Lemos, T.V.; Esculier, J.-F.; Barbosa, G.M.P.; Matheus, J.P.C. Effects of two gait retraining programs on pain, function, and lower limb kinematics in runners with patellofemoral pain: A randomized controlled trial. PLoS ONE 2024, 19, e0295645. [Google Scholar] [CrossRef] [PubMed]
- Kernozek, T.W.; Ricard, M.D. Foot placement angle and arch type: Effect on rearfoot motion. Arch. Phys. Med. Rehabil. 1990, 71, 988–991. [Google Scholar]
- Barton, C.J.; Lack, S.; Hemmings, S.; Tufail, S.; Morrissey, D. The ‘Best Practice Guide to Conservative Management of Patellofemoral Pain’: Incorporating level 1 evidence with expert clinical reasoning. Br. J. Sports Med. 2015, 49, 923–934. [Google Scholar] [CrossRef]
- Anderson, L.M.; Martin, J.F.; Barton, C.J.; Bonanno, D.R. What is the Effect of Changing Running Step Rate on Injury, Performance and Biomechanics? A Systematic Review and Meta-analysis. Sports Med. Open 2022, 8, 112. [Google Scholar] [CrossRef]
- dos Santos, A.F.; Nakagawa, T.H.; Lessi, G.C.; Luz, B.C.; Matsuo, H.T.; Nakashima, G.Y.; Maciel, C.D.; Serrão, F.V. Effects of three gait retraining techniques in runners with patellofemoral pain. Phys. Ther. Sport 2019, 36, 92–100. [Google Scholar] [CrossRef]
- Boldt, A.R.; Willson, J.D.; Barrios, J.A.; Kernozek, T.W. Effects of medially wedged foot orthoses on knee and hip joint running mechanics in females with and without patellofemoral pain syndrome. J. Appl. Biomech. 2013, 29, 68–77. [Google Scholar] [CrossRef]
- Esculier, J.-F.; Bouyer, L.J.; Dubois, B.; Fremont, P.; Moore, L.; McFadyen, B.; Roy, J.-S. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain?A randomised clinical trial. Br. J. Sports Med. 2018, 52, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Musgjerd, T.; Anason, J.; Rutherford, D.; Kernozek, T.W. Effect of Increasing Running Cadence on Peak Impact Force in an Outdoor Environment. Int. J. Sports Phys. Ther. 2021, 16, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Daoud, A.I.; Geissler, G.J.; Wang, F.; Saretsky, J.; Daoud, Y.A.; Lieberman, D.E. Foot strike and injury rates in endurance runners: A retrospective study. Med. Sci. Sports Exerc. 2012, 44, 1325–1334. [Google Scholar] [CrossRef]
- Bonacci, J.; Vicenzino, B.; Spratford, W.; Collins, P. Take your shoes off to reduce patellofemoral joint stress during running. Br. J. Sports Med. 2014, 48, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Eslami, M.; Begon, M.; Hinse, S.; Sadeghi, H.; Popov, P.; Allard, P. Effect of foot orthoses on magnitude and timing of rearfoot and tibial motions, ground reaction force and knee moment during running. J. Sci. Med. Sport 2009, 12, 679–684. [Google Scholar] [CrossRef]
- Jor, A.; Lau, N.W.; Daryabor, A.; Koh, M.W.; Lam, W.-K.; Hobara, H.; Kobayashi, T. Effects of foot orthoses on running kinetics and kinematics: A systematic review and meta-analysis. Gait Posture 2024, 109, 240–258. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- WMA—The World Medical Association-WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Participants. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki/ (accessed on 26 December 2024).
- Lavigne, A.; Lescure, Y.; Delacroix, S. La podologie orthopédique avancée. Rev. Du Podol. 2017, 13, 8–10. [Google Scholar] [CrossRef]
- Nigg, B.M.; Wakeling, J.M. Impact forces and muscle tuning: A new paradigm. Exerc. Sport Sci. Rev. 2001, 29, 37–41. [Google Scholar] [CrossRef]
- Guyot, M. Analyse Baropodométrique Embarquée Après un Programme de Rééducation sur Tapis de Marche dans la Maladie de Parkinson. Ph.D. Thesis, Université de Lorraine, Nancy, France, 2020. [Google Scholar]
- Bisiaux, M.; Moretto, P.; Lensel, G.; Thévenon, A. Détermination d’un seuil de pression plantaire attendu: Utilisation de l’approche adimensionnelle pour réduire la variabilité des pressions plantaires Determination of an expected plantar pressure threshold: Dimensionless approach use to reduce the variability of the plantar pressures. Ann. Readapt. Med. Phys. 2003, 46, 539–544. [Google Scholar] [CrossRef]
- Gouelle, A. Analyse des appuis plantaires sur tapis de marche: État actuel et perspectives. In Proceedings of the 35ème Journée Montpelliéraine de Podologie, Médecine et Chirurgie du Pied, Montpellier, France, 7 March 2014. [Google Scholar]
- Schubert, A.G.; Kempf, J.; Heiderscheit, B.C. Influence of stride frequency and length on running mechanics: A systematic review. Sports Health 2014, 6, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Ogasawara, I.; Shimokochi, Y.; Konda, S.; Mae, T.; Nakata, K. Effect of Rearfoot Strikes on the Hip and Knee Rotational Kinetic Chain During the Early Phase of Cutting in Female Athletes. Sports Med. Open 2021, 7, 75. [Google Scholar] [CrossRef] [PubMed]
- Lenhart, R.L.; Thelen, D.G.; Wille, C.M.; Chumanov, E.S.; Heiderscheit, B.C. Increasing Running Step Rate Reduces Patellofemoral Joint Forces. Med. Sci. Sports Exerc. 2014, 46, 557–564. [Google Scholar] [CrossRef]
- Nakhaee, M.; Mohseni-Bandpei, M.; Mousavi, M.E.; Shakourirad, A.; Safari, R.; Kashani, R.V.; Mimar, R.; Amiri, H.; Nakhaei, M. The effects of a custom foot orthosis on dynamic plantar pressure in patients with chronic plantar fasciitis: A randomized controlled trial. Prosthet. Orthot. Int. 2023, 47, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Farris, D.; Buckeridge, E.; Trewartha, G.; McGuigan, P. The Effects of Orthotic Heel Lifts on Achilles Tendon Force Strain During Running. Comp. Biochem. Physiol. Part A: Mol. Integr. Physiol. 2008, 150, S82. [Google Scholar] [CrossRef]
- Lieberman, D.E.; Venkadesan, M.; Werbel, W.A.; Daoud, A.I.; D’andrea, S.; Davis, I.S.; Mang’eni, R.O.; Pitsiladis, Y. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature 2010, 463, 531–535. [Google Scholar] [CrossRef]
- Bachand, R.; Bazett-Jones, D.M.; Esculier, J.-F.; Fox, C.; Norte, G.E.; Garcia, M.C. The Dogma of Running Injuries: Perceptions of Adolescent and Adult Runners. J. Athl. Train. 2024, 59, 955–961. [Google Scholar] [CrossRef]
- Heiderscheit, B.C.; Chumanov, E.S.; Michalski, M.P.; Wille, C.M.; Ryan, M.B. Effects of step rate manipulation on joint mechanics during running. Med. Sci. Sports Exerc. 2011, 43, 296–302. [Google Scholar] [CrossRef]
- Crago, D.; Bishop, C.; Arnold, J.B. The effect of foot orthoses and insoles on running economy and performance in distance runners: A systematic review and meta-analysis. J. Sports Sci. 2019, 37, 2613–2624. [Google Scholar] [CrossRef]
- Warne, J.P.; Gruber, A.H. Transitioning to Minimal Footwear: A Systematic Review of Methods and Future Clinical Recommendations. Sports Med. Open 2017, 3, 33. [Google Scholar] [CrossRef]
- Cheung, R.T.H.; Davis, I.S. Landing pattern modification to improve patellofemoral pain in runners: A case series. J. Orthop. Sports Phys. Ther. 2011, 41, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, D.R.; Murley, G.S.; Munteanu, S.E.; Landorf, K.B.; Menz, H.B. Effectiveness of foot orthoses for the prevention of lower limb overuse injuries in naval recruits: A randomised controlled trial. Br. J. Sports Med. 2018, 52, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Willy, R.W.; Davis, I.S. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J. Orthop. Sports Phys. Ther. 2011, 41, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Nigg, B.M.; Emery, C.; Hiemstra, L.A. Unstable shoe construction and reduction of pain in osteoarthritis patients. Med. Sci. Sports Exerc. 2006, 38, 1701–1708. [Google Scholar] [CrossRef][Green Version]
- Noehren, B.; Hamill, J.; Davis, I. Prospective evidence for a hip etiology in patellofemoral pain. Med. Sci. Sports Exerc. 2013, 45, 1120–1124. [Google Scholar] [CrossRef]

| Condition | Footwear | Drop | Cadence | Orthoses |
|---|---|---|---|---|
| C0 (Reference) | Control shoes | 10 mm | No adjustment (0%) | None |
| C1 (Cadence only) | Control shoes | 10 mm | +10% | None |
| C2 (Plantar orthoses) | Control shoes | 10 mm | No adjustment (0%) | ALIFOrthoses |
| C3 (Asics Noosa) | Asics NOOSA | 5 mm | No adjustment (0%) | None |
| C4 (Cross-interventions) | Asics NOOSA | 5 mm | +10% | ALIFOrthoses |
| Parameter | C0 (Mean ± SD) | C1 (Mean ± SD) | C2 (Mean ± SD) | C3 (Mean ± SD) | C4 (Mean ± SD) | Δ (vs. C0) | p-Value | Effect Size (Cohen’s d) |
|---|---|---|---|---|---|---|---|---|
| Rearfoot contact time (ms) | 42.22 ± 3.45 | 42.00 ± 5.34 | 41.00 ± 4.23 | 44.11 ± 2.87 | 41.83 ± 3.76 | −1.22 (C2), +1.89 (C3) | <0.001 * | 0.45 (C2), 0.61 (C3) |
| Midfoot contact time (ms) | 51.45 ± 2.3 | 53.28 ± 2.67 | 53.27 ± 4.22 | 53.43 ± 3.29 | 56.52 ± 3.98 | +1.83 (C1), +5.07 (C4) | <0.001 * | 0.48 (C1), 0.89 (C4) |
| Forefoot contact time (ms) | 79.4 ± 4.32 | 80.45 ± 3.4 | 80.09 ± 2.39 | 78.5 ± 4.2 | 79.02 ± 3.1 | +1.01 (C1), −0.94 (C3) | <0.001 * | 0.35 (C1), 0.38 (C3) |
| Rearfoot peak force (N) | 461.08 ± 76.5 | 379.72 ± 67.8 | 419.77 ± 38.8 | 388.95 ± 54.4 | 321.99 ± 59.2 | −81.36 (C1), −139.09 (C4) | <0.001 * | 0.55 (C1), 1.02 (C4) |
| Forefoot peak force (N) | 1041.7 ± 86.4 | 973.65 ± 79.2 | 1024.48 ± 89.3 | 976.63 ± 92.2 | 858.54 ± 85.2 | −68.07 (C1), −183.18 (C4) | <0.001 * | 0.47 (C1), 1.21 (C4) |
| Stride length (cm) | 240.17 ± 48.2 | 223.17 ± 37.3 | 240.12 ± 52.2 | 237.69 ± 39.1 | 223.57 ± 42.9 | −17.00 (C1), −16.60 (C4) | <0.001 * | 0.56 (C1), 0.54 (C4) |
| Step length (cm) | 119.75 ± 16.3 | 111.41 ± 21.7 | 119.99 ± 18.4 | 118.50 ± 19.3 | 111.67 ± 23.9 | −8.34 (C1), −8.08 (C4) | <0.001 * | 0.52 (C1), 0.50 (C4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicolas-Peyrot, M.A.; Lescure, Y.; Perrin, E.; Martinez-Rico, M.; Travouillon, C.; Gijon-Nogueron, G.; Lopezosa-Reca, E. Optimizing Running Mechanics, Effects of Cadence, Footwear, and Orthoses on Force Distribution: A Quasi-Experimental Study. J. Funct. Morphol. Kinesiol. 2025, 10, 89. https://doi.org/10.3390/jfmk10010089
Nicolas-Peyrot MA, Lescure Y, Perrin E, Martinez-Rico M, Travouillon C, Gijon-Nogueron G, Lopezosa-Reca E. Optimizing Running Mechanics, Effects of Cadence, Footwear, and Orthoses on Force Distribution: A Quasi-Experimental Study. Journal of Functional Morphology and Kinesiology. 2025; 10(1):89. https://doi.org/10.3390/jfmk10010089
Chicago/Turabian StyleNicolas-Peyrot, Marie Adelaide, Yves Lescure, Eleonore Perrin, Magdalena Martinez-Rico, Corentin Travouillon, Gabriel Gijon-Nogueron, and Eva Lopezosa-Reca. 2025. "Optimizing Running Mechanics, Effects of Cadence, Footwear, and Orthoses on Force Distribution: A Quasi-Experimental Study" Journal of Functional Morphology and Kinesiology 10, no. 1: 89. https://doi.org/10.3390/jfmk10010089
APA StyleNicolas-Peyrot, M. A., Lescure, Y., Perrin, E., Martinez-Rico, M., Travouillon, C., Gijon-Nogueron, G., & Lopezosa-Reca, E. (2025). Optimizing Running Mechanics, Effects of Cadence, Footwear, and Orthoses on Force Distribution: A Quasi-Experimental Study. Journal of Functional Morphology and Kinesiology, 10(1), 89. https://doi.org/10.3390/jfmk10010089








