Arthrodesis and Hemiarthroplasty: Different Techniques in the Treatment of Hallux Rigidus—Surgery and Postoperative Rehabilitation
Abstract
:1. Introduction
2. Materials and Methods
Postoperative Rehabilitation [10]
3. Results
4. Discussion
Author Contributions
Conflicts of Interest
Financial Disclosure
References
- Davies-Colley, N. Contraction of the metatarsophalangeal joint of the great toe (hallux flexus). Br. Med. J. 1887, 1, 728. [Google Scholar]
- Rubio-Lorenzo, M.; Prieto-Montaña, J.R. Epidemiological factors of hallux rigidus. J. Bone Jt. Surg. 2009, 91B, 324. [Google Scholar]
- Scarfì, G; Veneziani, C. Alluce rigido: semeiotica clinica e strumentale. In L’alluce Rigido, monografia della Società Italiana di Medicina e Chirurgia del piede; De Palma, L., Giannini, S., Eds.; Bologna: Rome, Italy, 2001; Volume 1, pp. 21–26. [Google Scholar]
- Shereff, M.J.; Baumhauer, J.F. Hallux rigidus and osteoarthrosis of the first metatarsophalangeal joint. J. Bone Jt. Surg. 1998, 80, 898–909. [Google Scholar]
- Regnauld, B. Disorders of the great toe. In The Foot: Pathology, Aetiology, Seminology, Clinical Investigation and Treatment; Springer–Verlag: Berlin, Germany, 1986; pp. 345–359. [Google Scholar]
- Collins, M.J.; Shurnas, P.S. Hallux rigidus: Grading and long term results of operative treatment. J. Bone Jt. Surg. 2003, 85A, 2072–2088. [Google Scholar]
- Olms, K.; Dietze, A. Replacement arthroplasty for hallux rigidus. Int. Orthop. 1999, 23, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Beeson, P. The surgical treatment of hallux limitus/rigidus: A critical review of the literature. Foot. 2004, 14, 6–22. [Google Scholar] [CrossRef]
- Hasselman, C.T.; Shields, N. Resurfacing of the first metatarsal head in the treatment of hallux rigidus. Tech. Foot Ankle Surg. 2008, 7, 31–40. [Google Scholar] [CrossRef]
- Martinelli, N.; Denaro, V.; Gosheger, G.; Pejman, Z.; Buchhorn, T. Recreational sport activity after total replacement of the first metatarsophalangeal joint: a prospective study. Int. Orthop. 2010, 34, 973–979. [Google Scholar]
- Andreasi, A.; Ceschi, M. L’artrodesi della I metatarsofalangea nell’alluce rigido. In L’alluce Rigido, monografia della Società Italiana di Medicina e Chirurgia del piede; De Palma, L., Giannini, S., Eds.; Bologna: Rome, Italy, 2001; pp. 139–152. [Google Scholar]
- Wassink, S.; van den Oeven, M. Arthrodesis of the first metatarsophalangeal joint using a single screw: Retrospective analysis of 109 feet. J. Foot Ankle Surg. 2009, 48, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Mann, R.A.; Clanton, T.O. Hallux rigidus: treatment by cheilectomy. J. Bone Jt. Surg. 1988, 70A, 400–406. [Google Scholar] [CrossRef]
- Verrina, F. La cheilectomia nel trattamento chirurgico dell’alluce rigido. In L’alluce Rigido, monografia della Società Italiana di Medicina e Chirurgia del piede; De Palma, L., Giannini, S., Eds.; Bologna: Rome, Italy, 2001; Volume 1, pp. 59–64. [Google Scholar]
- Brosky, T.A.; Menke, C.R.; Xenos, D. Reconstruction of the first metatarsophalangeal joint following post-cheilectomy avascular necrosis of the first metatarsal head: A case report. J. Foot Ankle Surg. 2009, 48, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Erdil, M.; Bilsel, K.; Imren, Y.; Mutlu, S.; Güler, O.; Gürkan, V.; Elmadağ, N.M.; Tuncay, I. Metatarsal head resurfacing hemiarthroplasty in the treatment of advanced stage hallux rigidus: Outcomes in the short-term. Acta Orthop. Traumatol. Turc. 2012, 46, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Giza, E.; Sullivan, M.; Ocel, D.; Lundeen, G.; Mitchell, M.; Frizzell, L. First metatarsophalangeal hemiarthroplasy for hallux rigidus. Int. Orthop. 2010, 34, 1193–1198. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization: International Classification of Diseases (ICD). Available online: http://www.who.int/classifications/icd/en/ (accessed on 2 February 2014).
- Ibrahim, T.; Beiri, A.; Azzabi, M.; Best, A.J.; Taylor, G.J.; Menon, D.K. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J. Foot Ankle Surg. 2007, 46, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Hopson, M.; Stone, P.; Paden, M. First metatarsal head osteoarticular transfer system for salvage of a failedhemicap-implant: A case report. J. Foot Ankle Surg. 2009, 48, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Sorbie, C.; Saunders, G.A. Hemiarthroplasty in the treatment of hallux rigidus. Foot Ankle Int. 2008, 29, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Mah, C.D.; Banks, A.S. Immediate weight bearing following first metatarsophalangeal joint fusion with Kirschner wire fixation. J. Foot Ankle Surg. 2009, 48, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Raikin, S.M.; Ahmad, J.; Pour, A.E.; Abidi, N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J. Bone Jt. Surg. 2007, 89A, 1979–1985. [Google Scholar] [CrossRef] [PubMed]
- Casillas, M.M.; Jacobs, M. “Alluce Rigido”. Sta in: La riabilitazione in ortopedia –II edizione. Brotzman, S.B., Wilk, K.E., Boccardi, S., Eds.; Excerpta Medica: Milano, Italy, 2004; pp. 422–429. [Google Scholar]
| Parameters | Value |
|---|---|
| Patients | 12 |
| Feet | 14 |
| Mean age (months) | 57.7 |
| Males | 2 |
| Females | 10 |
| Arthrodesis (feet) | 6 |
| Arthroplasty (feet) | 8 |
| Grade II (feet) | 3 |
| Grade III (feet) | 11 |
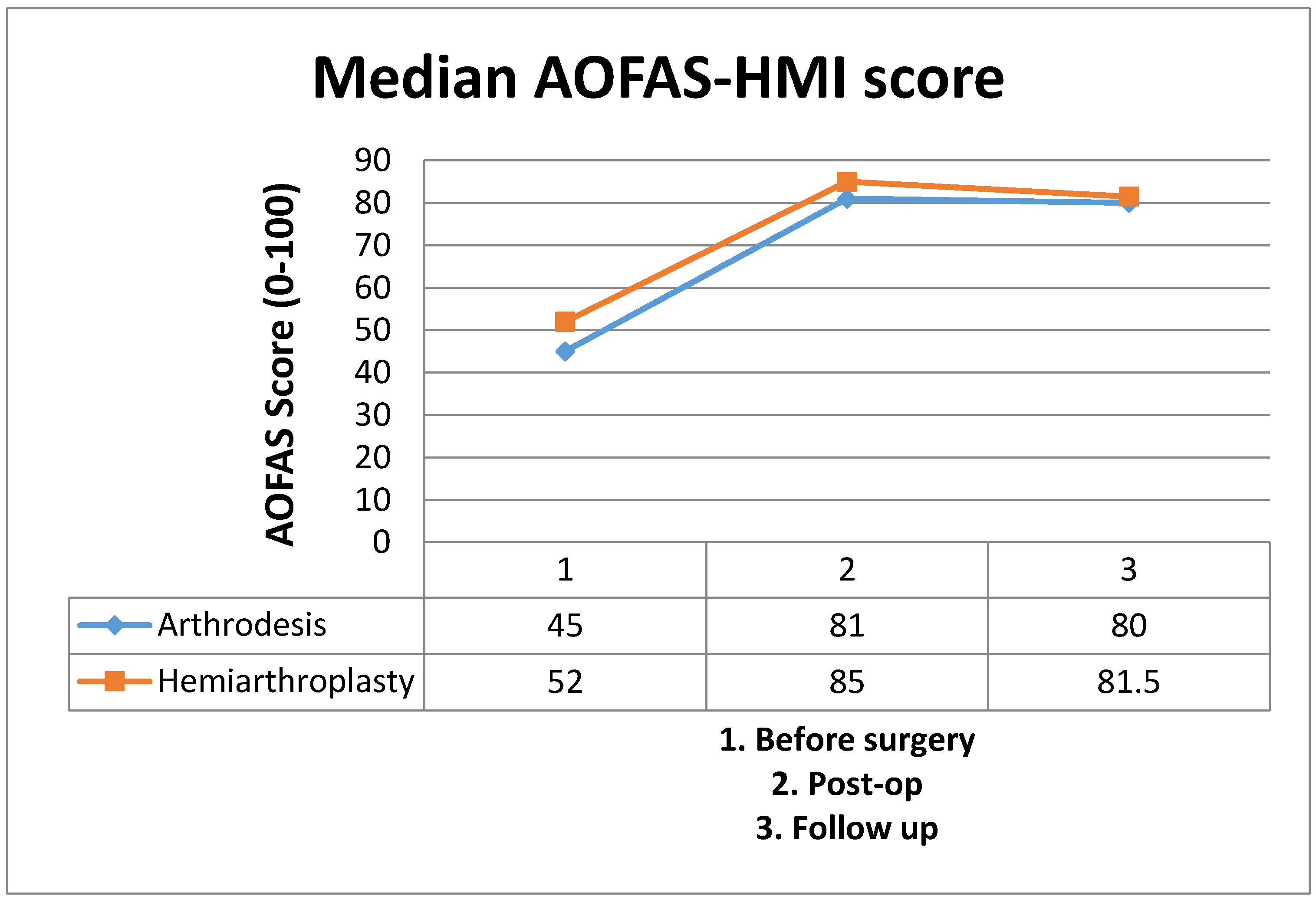
| Procedure | N. of Feet | Grade II | Grade III | AOFAS Preoperative (Median) | AOFAS Postoperative (Median) | AOFAS Control (Median) | Pre-Postoperative Difference (Median of Differences) | p Value | |
|---|---|---|---|---|---|---|---|---|---|
| Hemiarthroplasty | 8 | 3 | 5 | 52 | 85 | 81.5 | 33.0 | 0.022 | |
| Arthrodesis | 6 | 0 | 6 | 45 | 81 | 80 | 35.5 | 0.036 | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannavò, L.; Costarella, L.; Pavone, V.; Testa, G.; De Gori, M.; Sessa, G. Arthrodesis and Hemiarthroplasty: Different Techniques in the Treatment of Hallux Rigidus—Surgery and Postoperative Rehabilitation. J. Funct. Morphol. Kinesiol. 2016, 1, 102-108. https://doi.org/10.3390/jfmk1010102
Cannavò L, Costarella L, Pavone V, Testa G, De Gori M, Sessa G. Arthrodesis and Hemiarthroplasty: Different Techniques in the Treatment of Hallux Rigidus—Surgery and Postoperative Rehabilitation. Journal of Functional Morphology and Kinesiology. 2016; 1(1):102-108. https://doi.org/10.3390/jfmk1010102
Chicago/Turabian StyleCannavò, Luca, Luciano Costarella, Vito Pavone, Gianluca Testa, Marco De Gori, and Giuseppe Sessa. 2016. "Arthrodesis and Hemiarthroplasty: Different Techniques in the Treatment of Hallux Rigidus—Surgery and Postoperative Rehabilitation" Journal of Functional Morphology and Kinesiology 1, no. 1: 102-108. https://doi.org/10.3390/jfmk1010102






