Abstract
This study examines the trends, impacts, and challenges of HIV in Bangladesh from 2000 to 2024, with a focus on its epidemiology, demographic distribution, and socioeconomic determinants. Despite maintaining one of the lowest HIV prevalence rates globally (<0.1%), Bangladesh faces a concentrated epidemic among high-risk populations, including people who inject drugs (PWID), men who have sex with men (MSM), sex workers, transgender individuals, and migrant workers. Analysis reveals a steady increase in reported infections, attributed to enhanced diagnostic capacities and public awareness. The 25–49 year age group remains the most affected, accounting for over 65% of cases, underscoring the vulnerability of the economically active population. Gender disparities persist, with males representing the majority of infections but lower ART coverage among females and transgender individuals. While interventions such as PMTCT programs, ART expansion, and targeted awareness campaigns have contributed to improved outcomes, barriers such as stigma, healthcare inequities, and limited rural access hinder progress. The study also evaluates Bangladesh’s progress toward the 95-95-95 targets, highlighting significant strides in treatment and viral suppression but gaps in diagnosis. Future research must address behavioral trends, stigma reduction, and integration of HIV services for marginalized populations. This paper emphasizes the need for evidence-based strategies to ensure equitable healthcare delivery and sustainable progress in combating HIV.
1. Introduction
Acquired Immunodeficiency Syndrome (AIDS), caused by the Human Immunodeficiency Virus (HIV), has evolved from a mysterious illness first identified in the early 1980s into a global epidemic that reshaped public health policies, highlighting humanity’s ongoing battle against one of the most profound medical and social challenges of modern times [1]. However, the origins of HIV date back much earlier, with the earliest known case identified in 1959 from a blood sample of a man in Kinshasa, Democratic Republic of Congo [2]. Phylogenetic studies suggest that HIV likely crossed into humans from non-human primates in the early 20th century, with the virus circulating undetected for decades before doctors began to understand its devastating impact [3,4]. Despite advances in tracing its origins, pinpointing ‘patient zero’ remains elusive, highlighting the complexity of this global health crisis.
HIV, the causative agent of AIDS, is primarily transmitted through specific pathways involving the exchange of bodily fluids, making it a highly preventable but persistently challenging public health issue. The most common mode of transmission is unprotected sexual contact, accounting for the majority of cases globally. During sexual intercourse, the virus is transmitted via semen, vaginal fluids, or rectal fluids, particularly when mucosal surfaces are compromised. Another significant route is the sharing of contaminated needles and syringes, particularly among individuals who inject drugs, which facilitates direct entry of the virus into the bloodstream [5]. HIV can also spread through transfusion of infected blood products, although this has been largely mitigated in many countries through rigorous blood screening protocols [1]. Vertical transmission from mother to child during pregnancy, childbirth, or breastfeeding represents another critical pathway. Without medical intervention, the risk of transmission in such cases ranges from 15% to 45%, but ART significantly reduces this risk to below 5% [6]. Other, less common modes include occupational exposure among healthcare workers through needle-stick injuries and, rarely, through deep kissing if both parties have open sores or bleeding gums [7,8]. HIV is not transmitted through casual contact, air, water, or by sharing food or utensils, reflecting the specificity of its transmission routes. These mechanisms underscore the importance of targeted prevention strategies such as promoting condom use, harm reduction programs, safe blood transfusion practices, and ensuring access to ART for pregnant women to curb the spread of HIV.
The first documented cases of HIV in Bangladesh emerged in the mid-1980s, marking the country’s initial encounter with the global epidemic. The first officially reported case was in 1989, involving a Bangladeshi migrant worker who had returned from a Middle Eastern country [9]. This case underscored the role of international migration in the early spread of the disease within Bangladesh, particularly among returning expatriates. By the early 1990s, the number of reported cases remained relatively low, largely due to limited diagnostic capacity and the low prevalence within the general population. However, stigma, a lack of awareness, and an insufficient healthcare infrastructure posed significant barriers to early containment efforts [10]. Early government responses, supported by international organizations such as UNAIDS and WHO, focused on surveillance, raising awareness, and targeting high-risk groups, including migrant workers, sex workers, and intravenous drug users [11]. These initial interventions laid the foundation for subsequent strategies aimed at managing the epidemic in Bangladesh.
From 2000 to 2023, Bangladesh made significant progress in combating the HIV epidemic, characterized by one of the lowest HIV prevalence rates globally, remaining consistently below 0.1% [1]. Vulnerable populations, including sex workers, men who have sex with men (MSM), transgender individuals, and intravenous drug users (IDUs), have shown higher infection rates, reflecting disparities in risk and healthcare access [12]. Additionally, the influx of Rohingya refugees since 2017 has posed new challenges to the national response, as inadequate healthcare provisions and high-risk behaviors among displaced populations have increased the risk of localized outbreaks [9]. In 2024, Bangladesh reported a cumulative 1438 confirmed HIV cases and approximately 200 HIV-related deaths, with concentrated outbreaks among high-risk groups [13].
HIV remains a significant public health concern in Bangladesh, particularly among vulnerable and marginalized populations. Despite numerous awareness campaigns, the level of knowledge about HIV remains low, with married women often holding misconceptions about its transmission [14,15]. Furthermore, internal stigma significantly affects people living with HIV, reducing their likelihood of accessing timely care and support [16]. High-risk populations, such as injecting drug users and commercial sex workers, contribute disproportionately to the spread of the epidemic, necessitating targeted interventions [17,18]. The dual burden of tuberculosis and HIV further complicates prevention and treatment efforts, highlighting the need for integrated health strategies [19].
Despite significant progress, challenges persist in Bangladesh’s efforts to control the HIV epidemic. Urbanization, international migration, and limited healthcare coverage for rural populations continue to complicate prevention and treatment efforts. Social stigma and discrimination remain significant barriers, deterring individuals from seeking timely diagnosis and care. Furthermore, gaps in healthcare infrastructure and funding hinder the sustainability of comprehensive responses [1].
This study presents a unique perspective by providing a comprehensive analysis of HIV outbreak trends in Bangladesh over a 24-year period, making it one of the most detailed examinations of the epidemic in the country to date. While previous studies have explored individual aspects such as prevalence among high-risk populations or the effectiveness of specific interventions, this research synthesizes infection, death, and demographic data to reveal broader trends and insights. By integrating socioeconomic indicators such as Gross Domestic Product (GDP), Gross National Income (GNI), Human Development Index (HDI), and urbanization, the study also examines how macro-level factors influence the epidemic’s progression, offering a novel intersectional approach to understanding HIV in Bangladesh. A significant research gap exists in the longitudinal analysis of HIV in Bangladesh. While much attention has been paid to high-prevalence regions globally, studies focusing on low-prevalence countries like Bangladesh remain sparse. This gap is further accentuated by limited data on the relationship between socioeconomic shifts, demographic transitions, and HIV trends in the Bangladeshi context. Addressing this gap is crucial for tailoring interventions to the unique epidemiological profile of the country and ensuring that prevention strategies are data-driven and locally relevant.
The aim of this research is to study the outbreak trends of HIV in Bangladesh from 2000 to 2024 by analyzing infection and death data, with the ultimate objective of understanding how the virus’s impact on the population has evolved over time. The two main outcomes examined in this study are the number of individuals infected with HIV and the number of HIV-related deaths, aggregated by year and division. Since the first documentation of HIV in Bangladesh back in 1989, the country has experienced annual outbreaks, with steady infection and death rates, case fatality ratios, and regional spread. This study seeks to uncover the key factors that have influenced the transmission dynamics and severity of HIV outbreaks, as well as the effectiveness of public health interventions. This study is of critical importance as it addresses the dual challenges of underreporting and underdiagnosis, which have historically skewed perceptions of the epidemic in Bangladesh. By leveraging improved diagnostic capabilities and enhanced datasets, it provides a clearer picture of the epidemic’s trajectory. Furthermore, the study’s findings can guide policymakers in designing targeted interventions to achieve the 95-95-95 goals, ensuring that resources are efficiently allocated to high-risk groups and underserved regions. In doing so, this research not only contributes to the academic understanding of HIV in Bangladesh but also serves as a practical tool for public health planning and intervention design.
2. Methods
2.1. Data Description
The data for this study was gathered from various publicly available sources, including the National AIDS/STD Control (https://asp.portal.gov.bd/, accessed on 12 December 2024), which falls under the Institute of Epidemiology, Disease Control, and Research (IEDCR, https://www.iedcr.org/, accessed on 12 December 2024); the World Health Organization (WHO) (https://www.who.int/, accessed on 12 December 2024); and others. The dataset covers the period from 2000 to 2024 and includes key variables such as the number of infected cases, deaths, and social factors like GDP/GNI (https://www.worldbank.org/en/country/bangladesh, https://www.imf.org/external/datamapper/profile/BGD, accessed on 12 December 2024), HDI (https://data.undp.org/countries-and-territories/BGD, accessed on 12 December 2024), and poverty rate (https://www.adb.org/where-we-work/bangladesh/poverty, accessed on 12 December 2024). The dataset also includes population dynamics such as urbanization and population density, sourced from the Bangladesh Bureau of Statistics (https://bbs.gov.bd/, accessed on 12 December 2024) and Worldometer, Bangladesh (https://www.worldometers.info/world-population/bangladesh-population/, accessed on 12 December 2024).
2.2. Limitations of the Data
HIV-related data in Bangladesh faces significant limitations, which affect the accuracy and comprehensiveness of epidemiological assessments and public health interventions. One major issue is underreporting and limited surveillance. Many HIV cases remain undiagnosed or unreported due to the lack of robust surveillance systems, particularly in rural and hard-to-reach areas [20]. Another significant challenge is the inadequate availability of testing and diagnostic facilities. Many rural areas in Bangladesh lack access to affordable and reliable testing centers, leaving numerous cases undiagnosed [11]. The social stigma surrounding HIV further exacerbates this problem, discouraging individuals from seeking testing or treatment, which creates gaps in data collection and reporting [21]. These issues hinder the ability to accurately estimate the true prevalence of the epidemic and plan targeted interventions.
Furthermore, data on high-risk populations such as sex workers, men who have sex with men (MSM), and people who inject drugs (PWID) are often incomplete or missing. This gap stems from the legal and social barriers that impede outreach and data collection efforts within these marginalized groups [21]. These groups are critical to understanding the dynamics of HIV transmission and require focused attention to improve data quality.
Resource constraints further contribute to the limitations of HIV-related data. Insufficient funding and human resources dedicated to HIV research and data collection hamper efforts to maintain accurate and up-to-date records. This lack of resources often leads to incomplete datasets and reduced capacity for advanced statistical analyses, such as those incorporating regional and socio-environmental factors [20]. Addressing these limitations will require strengthening the surveillance infrastructure, increasing testing accessibility, and allocating sufficient financial and human resources to HIV programs in Bangladesh. Such measures will improve data accuracy and support evidence-based policymaking to combat the epidemic effectively.
2.3. Data Analysis
Our study’s response variables are the discrete count variables of HIV infection and mortality cases. We aim to explore the role of environmental and demographic factors in these responses. To analyze these relationships, we employed statistical methods such as correlation analysis and seasonal decomposition and explored key metrics like the CFR and mortality rate. This paper primarily focuses on the statistical analysis of the available data, with descriptive statistics used to provide insights into the overall structure of the dataset. The limited availability of HIV-related data in Bangladesh restricted our ability to perform more advanced analyses incorporating socioeconomic factors. For our study, we utilized Python v3.13 for data preprocessing, matplotlib and seaborn for visualizations, geopandas for mapping, and the StatsModels library for conducting seasonal decomposition.
3. Socioeconomic and Health Trends in Bangladesh (2000–2024)
Over the years, Bangladesh’s socioeconomic and health trends have highlighted the nation’s progress and ongoing challenges. These trends reflect the impact of economic growth, urbanization, healthcare improvements, and targeted policy interventions [22,23,24,25,26,27].
3.1. HIV Infections and Deaths
The prevalence of HIV in Bangladesh has shown significant variability over the years, with infection rates peaking sporadically. Despite a relatively low prevalence rate among the population, the number of HIV cases has increased in specific periods, reflecting gaps in prevention efforts. However, deaths from HIV have remained comparatively low, indicating progress in medical interventions and awareness campaigns. Programs focusing on early detection, treatment availability, and public health awareness may have contributed to this outcome. Nevertheless, periodic infection surges suggest challenges in outreach and maintaining consistent preventive measures [28].
3.2. Population Trends
Bangladesh’s population has grown steadily, with urbanization accelerating rapidly. The urban population has expanded faster than the rural population, driven by migration to cities for industrial jobs, better infrastructure, and improved living standards. However, this rapid urbanization has created challenges, such as increased urban poverty and inequality. By 2030, it is projected that the majority of poor households will reside in urban areas, emphasizing the need for targeted urban poverty alleviation programs [29]. Moreover, Rahman [30] highlighted significant spatial inequalities within Bangladesh, indicating the need for development strategies that address these imbalances.
3.3. Economic Trends
Bangladesh has experienced robust GDP growth, reflecting its economic transformation and industrialization. GDP per capita has consistently increased, showcasing improvements in national productivity and living standards. However, economic growth has not fully translated into proportional reductions in poverty. Urban areas, particularly, have witnessed slower progress in poverty reduction, with growing income disparities [31]. The economic divide within the country remains a critical issue, as highlighted by the World Bank’s [32] analysis of the East–West development disparity. Addressing these gaps requires inclusive policies to ensure equitable economic benefits across regions and socioeconomic groups.
3.4. Human Development Index (HDI)
The steady improvement in Bangladesh’s HDI reflects advancements in healthcare, education, and living standards. Initiatives to improve access to education, reduce maternal and child mortality, and increase life expectancy have significantly contributed to this upward trend. However, rural areas often lag behind urban centers regarding healthcare access, infrastructure, and educational opportunities [31]. Rahman [30] also noted that regional disparities in human development persist, underscoring the importance of equitable policy interventions. Sustained improvements will require reducing these inequalities and ensuring long-term regional growth.
Bangladesh’s health, population, and economic development trends reflect a dynamic interplay between progress and challenges. While significant strides have been made in combating HIV, urbanization, and economic growth, the country faces persistent gaps in equitable resource distribution, urban poverty alleviation, and public health outreach. A holistic approach—integrating health, urban planning, and inclusive economic policies—is essential for sustaining Bangladesh’s developmental momentum and addressing its social challenges effectively.
4. Findings and Discussion
The geographic distribution of HIV in Bangladesh from 1989 to 2023, as depicted in the map in Figure 1, highlights significant regional disparities. The axes in Figure 1 represent geographic coordinates (longitude and latitude) of Bangladesh. The map is a geospatial visualization based on administrative boundaries (ADM1 level) of the eight divisions. It represents the spatial placement of regions on a map of Bangladesh. Dhaka Division accounts for the highest proportion of cases, with 35.44% of the total infections. This is likely due to Dhaka’s position as the nation’s capital and economic hub, characterized by high population density, urbanization, and the presence of migrant workers. The concentration of healthcare facilities and advanced diagnostic capabilities in Dhaka also contributes to higher reporting rates compared to other regions. The Chittagong Division follows with 27.51% of cases, driven by its role as a major port city and economic zone, which attracts high-risk populations, including migrant laborers and urban settlers. Sylhet Division, with 14.20% of reported cases, has a disproportionately high share relative to its population size. This can largely be attributed to the significant number of migrant workers originating from Sylhet, many of whom work in high-risk environments abroad and may transmit the virus upon returning. Khulna (10.70%) and Barisal (3.65%) contribute smaller shares to the national total, with Khulna reflecting the effects of urbanization, while Barisal’s relatively low figures may indicate underreporting due to limited healthcare infrastructure and connectivity. The northern divisions, Rajshahi, Rangpur, and Mymensingh, report lower cumulative proportions of cases at 5.12%, 1.51%, and 1.85%, respectively. These predominantly rural regions are characterized by less mobility and weaker healthcare access. However, the low numbers might also reflect underdiagnosis due to stigma and limited HIV testing services.
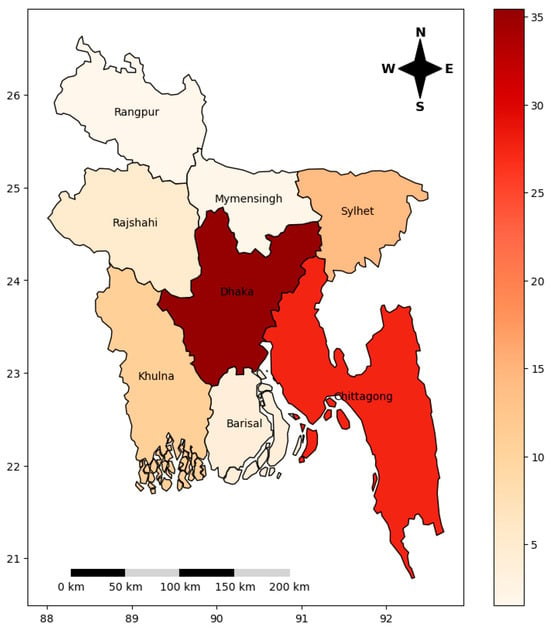
Figure 1.
Division-wise cumulative HIV infection rates in Bangladesh (1989–2023) [33].
Table 1 below summarizes the current state of HIV infection in Bangladesh, providing key indicators that highlight both progress and ongoing challenges in managing the epidemic. As of 2024, an estimated 16,069 people are living with HIV (PLHIV), with 1438 new cases reported and 195 HIV-related deaths recorded in the same year. Despite these challenges, significant strides have been made in raising awareness and providing treatment. Approximately 77% of PLHIV are aware of their HIV status, 78% of diagnosed individuals are on antiretroviral therapy (ART), and 91% of those on treatment have achieved viral suppression.

Table 1.
Current state of HIV in Bangladesh [13].
The dataset used in this study is shown in Table 2. It contains yearly records of HIV infection and death counts, which serve as two key response variables for this analysis. These variables provide insights into the trends and severity of the epidemic over time. Additionally, the dataset includes population dynamics to evaluate whether densely populated areas are more susceptible to infection, potentially uncovering regional disparities in HIV spread and management.

Table 2.
Dataset used for the study [32,33,34].
Socioeconomic indicator variables such as Gross Domestic Product (GDP) per capita, Gross National Income (GNI) per capita, Human Development Index (HDI), and poverty rate (PR) are also included. These variables allow for the exploration of the relationship between economic development, living standards, and HIV outcomes. For instance, GDP and GNI serve as proxies for economic prosperity, while HDI captures broader aspects of development, including education and health. The poverty rate highlights disparities in resource access that may exacerbate vulnerabilities to HIV infection. Together, these indicators provide a comprehensive view of the demographic, economic, and social factors influencing the HIV epidemic in Bangladesh.
4.1. Descriptive Statistics
The descriptive statistics presented in Table 3 provide a detailed summary of key variables related to HIV infection and associated socioeconomic indicators in Bangladesh from 2000 to 2024. The average yearly number of HIV-infected individuals (mean) was 492, with a standard deviation of 383.80, reflecting notable variability in infection counts across the years. HIV-related deaths averaged 91 annually, with a standard deviation of 77.88, indicating a similarly wide range of death counts. The highest recorded infections and deaths in a single year were 1438 and 266, respectively, while the minimum recorded counts were 31 and 1.

Table 3.
Descriptive statistics of HIV-related variables and socioeconomic indicators in Bangladesh (2000–2024).
Population dynamics are also captured in the dataset, with an average total population (PoP) of 154.48 million, comprising an urban population (Upop) mean of 50.38 million and a rural population (Rpop) mean of 104.11 million. The standard deviations for Upop and Rpop, 12.99 million and 1.83 million, respectively, highlight the steady growth in urbanization over the study period. The largest Upop recorded was 70.82 million, reflecting the increasing urbanization trend in Bangladesh.
Economic indicators such as GDP per capita and GNI per capita averaged USD 1193.56 and USD 1278.56, respectively, with significant variability as indicated by their standard deviations. The minimum GDP per capita was USD 620, while the maximum reached USD 2624. The HDI averaged 0.58, with the highest value of 0.67, showcasing progress in development metrics over the years. Poverty rate averaged 27.19%, with a minimum of 6.10% and a maximum of 49.80%, underscoring the socioeconomic disparities prevalent during this period.
4.2. Trends and Severity of HIV Outbreaks
Figure 2 consists of two panels illustrating trends in HIV infections, deaths, and the case fatality rate (CFR) in Bangladesh from 2000 to 2024. The left panel shows the annual counts of HIV-infected individuals and HIV-related deaths. The number of infections demonstrates a consistent upward trend, with a significant surge in recent years, reaching its peak in 2024. In contrast, deaths remained relatively stable over time, showing only moderate fluctuations. This supports the fact that people can survive for a longer period of time, even being HIV-positive, provided they have a strong immune system and/or are under prescribed medications.
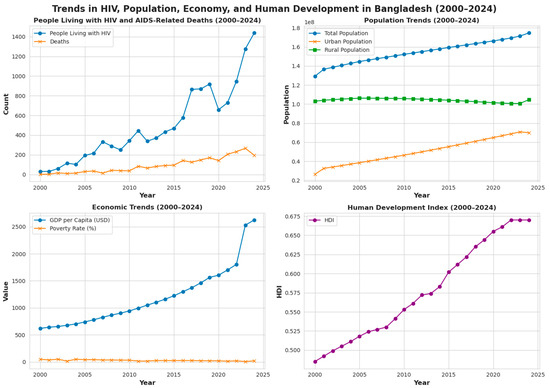
Figure 2.
Trends in infections, deaths, and CFR of HIV in Bangladesh (2000–2024).
The right panel highlights CFR, calculated as the ratio of HIV-related deaths to new infections annually. The CFR demonstrates considerable variability over the years, with noticeable spikes and declines. While the CFR shows a general decline in recent years, reflecting improvements in treatment accessibility and survival rates, the earlier variability points to challenges in managing the epidemic during its initial phases. The CFR for HIV is distinct from mortality rates, as it does not account for the time period between disease onset and death. The CFR, calculated based on the available data, reveals that HIV deaths constituted 0.08% of total deaths in Bangladesh. Additionally, the age-adjusted death rate is 0.36 per 100,000 people, placing Bangladesh 130th globally in HIV-related mortality [35]. Globally, the CFR for HIV was reported to be approximately 90% in 2008, though more recent estimates around the year 2021 suggest it may be as high as 80% [36], highlighting the persistent severity of the epidemic.
Figure 3 illustrates four key socioeconomic indicators of Bangladesh from 2000 to 2024: GDP per capita, GNI per capita, poverty rate, and HDI. These metrics highlight the country’s economic progress, developmental achievements, and ongoing challenges during this period. The top-left and top-right panels show the trends in GDP and GNI per capita. Over the 24-year period, both metrics exhibit consistent growth, reflecting substantial economic progress. GDP per capita starts at approximately USD 620 in 2000 and rises to over USD 2500 by 2024, showing a more than fourfold increase. Similarly, GNI per capita follows a similar trajectory, starting below USD 500 in 2000 and peaking at nearly USD 2860 around 2021 before slightly stabilizing in subsequent years. This rapid economic growth underscores Bangladesh’s transition from a low-income to a middle-income country, driven by export-oriented industries, remittances, and improved macroeconomic management.
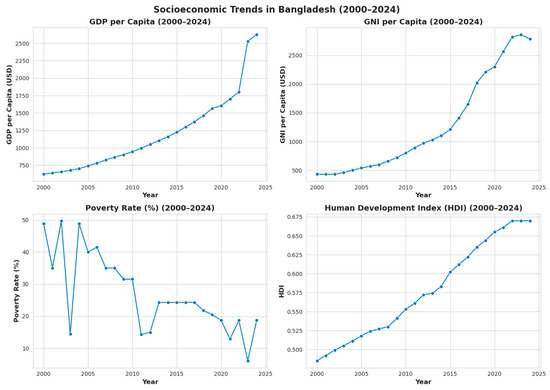
Figure 3.
Key socioeconomic indicators of Bangladesh (2000–2024).
The bottom-left panel depicts the poverty rate, which demonstrates a significant decline over the study period. The poverty rate was around 50% in 2000, reflecting widespread economic challenges, but it has steadily decreased, dropping below 10% in recent years. This remarkable reduction in poverty aligns with the improvements in GDP and GNI per capita, suggesting that economic growth has translated into better living conditions for a significant portion of the population. However, the graph also reveals intermittent fluctuations, indicating that certain socioeconomic vulnerabilities persist, particularly during global economic downturns or natural disasters. The bottom-right panel illustrates the trend in HDI, which measures overall development through education, health, and income dimensions. The HDI shows a steady upward trend, increasing from approximately 0.48 in 2000 to 0.67 in 2024. However, the HDI value remains below the global average (0.727 approx.), indicating that there is still room for improvement in achieving higher levels of human development.
The decline in poverty rates, as shown in the bottom-left panel, directly impacts the dynamics of HIV. Poverty is often associated with limited access to healthcare, education, and resources, which increases vulnerability to HIV infection. The reduction in poverty suggests that more individuals may now have better access to healthcare services, including HIV testing and ART. However, marginalized groups, such as female sex workers, men who have sex with men (MSM), and intravenous drug users (IDUs), may still face socioeconomic barriers despite the overall progress.
The upward trend in HDI signifies improvements in education and healthcare, which are critical for HIV awareness and prevention. Higher literacy rates and better health outcomes empower individuals to make informed decisions about HIV prevention and treatment. However, regional and urban–rural disparities in HDI remain a concern, as rural areas often lack the healthcare infrastructure and awareness programs necessary to address HIV effectively.
While the socioeconomic progress is promising, the persistent challenges of stigma, gender inequality, and the concentration of HIV infections in high-risk groups must be addressed to translate these gains into meaningful reductions in HIV prevalence. Policies should leverage economic growth and poverty reduction to expand HIV services, improve ART coverage, and increase public awareness campaigns. These efforts, combined with targeted investments in healthcare and education, can further reduce the burden of HIV in Bangladesh and ensure sustainable progress.
4.3. Correlation Analysis
The correlation heatmap provides valuable insights into the relationships between HIV-related variables and socioeconomic indicators in Bangladesh from 2000 to 2024 (Figure 4). While socioeconomic improvements, such as increased GDP/capita, GNI/capita, and HDI, are generally expected to reduce the overall burden of HIV, the data indicate a steadily increasing trend in reported infections. This rise in infection cases may be attributed more to enhanced diagnostic capabilities and increased social awareness than to an actual increase in HIV prevalence [10]. Improved identification and reporting of HIV cases, combined with reduced stigma and expanded access to testing facilities, likely contribute to this upward trend in diagnoses [19].
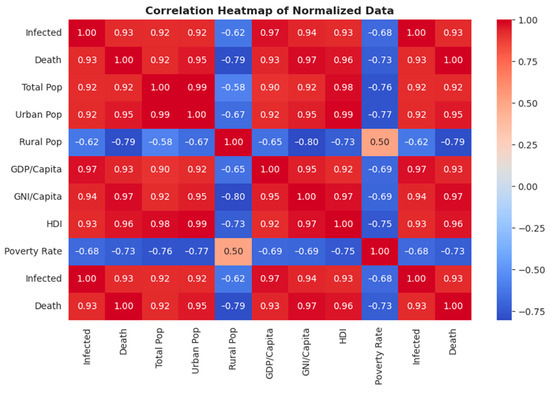
Figure 4.
Correlation heat map of the different variables and indicators.
The correlation heatmap highlights several strong positive correlations. For instance, infection rates are highly correlated with GDP/capita (0.97), GNI/capita (0.94), and HDI (0.93), suggesting that economically advanced regions and individuals with better access to healthcare are more likely to be diagnosed, reflecting improved healthcare infrastructure and diagnostic capabilities in wealthier areas [11]. Similarly, the urban population shows a strong positive correlation with infection rates (0.92), underlining the concentration of diagnoses in urban areas where healthcare facilities are better developed.
In contrast, the rural population exhibits moderate to strong negative correlations with infection rates (−0.62), GDP per capita (−0.65), and HDI (−0.73). These findings highlight disparities in healthcare access and awareness between urban and rural areas, suggesting that HIV cases in rural populations might be underreported or undiagnosed [17]. Additionally, the poverty rate shows negative correlations with infection rates (−0.68) and HDI (−0.75), indicating that poverty alleviation is generally associated with improved health outcomes. However, this may also reflect limited diagnostic capacity and healthcare access in impoverished regions, potentially masking the true prevalence of HIV in these areas.
The steady increase in reported HIV cases, despite socioeconomic improvements, underscores the role of underreporting and underdiagnosis in earlier years. With enhanced diagnostic capacities and awareness, more cases are being identified, contributing to the upward trend in infection numbers [10]. This trend is supported by the increasing urban population and decreasing rural population, as urbanization provides better healthcare access and infrastructure for diagnosis. Cultural factors may also play a role, as observed in marital status trends, where HIV infections are steadily increasing among single individuals, potentially due to changing social norms and behaviors [16].
4.4. Pair Plot
The pair plot in Figure 5 provides a detailed visualization of the relationships between HIV prevalence and various socioeconomic indicators in Bangladesh. Each subplot illustrates either a scatterplot, showing pairwise relationships between variables, or a univariate distribution, highlighting the individual distribution of each variable. These visualizations reveal significant insights into how HIV-related outcomes interact with broader social and economic factors.
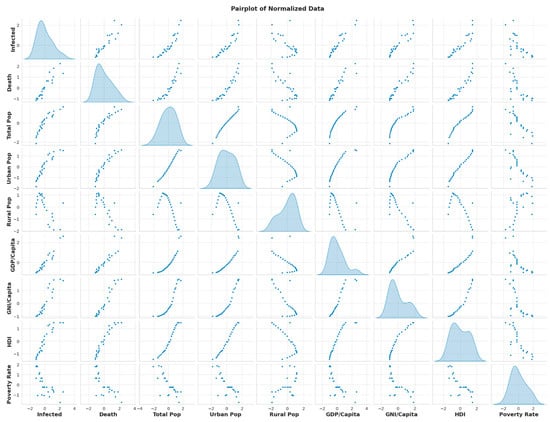
Figure 5.
Pair plot of normalized data.
The scatterplots demonstrate positive correlations between HIV infections and indicators such as GDP per capita and HDI. This pattern suggests that economically advanced regions or periods with higher development indices report more cases of HIV. However, this relationship likely reflects improved diagnostic capabilities and reporting mechanisms in these areas rather than a direct causation. Similar observations have been made globally, where urbanized and developed regions often exhibit higher reported HIV cases due to better access to healthcare and awareness campaigns [37]. Urbanization, another variable depicted in the pair plot, shows a strong correlation with HIV prevalence. Urban areas, characterized by dense populations and increased risky behaviors, often have better access to healthcare services, leading to higher testing rates and improved reporting accuracy [17].
The univariate distributions along the diagonal provide additional context. The distributions for HIV infections and deaths are right-skewed, indicating that while most regions or time periods report relatively low numbers, a few instances exhibit disproportionately high counts. This pattern aligns with localized outbreaks or the introduction of enhanced diagnostic techniques during specific years. Conversely, the more normally distributed variables, such as GDP per capita and HDI, reflect Bangladesh’s diverse economic landscape and its varying influence on health outcomes [10].
These relationships have significant implications for public health. The data underscores the need for equitable resource allocation, as economically disadvantaged and rural areas with limited diagnostic capabilities may have underreported cases of HIV. Strategies to address urban–rural disparities, such as mobile health clinics and targeted awareness programs, are crucial for an inclusive healthcare approach [38]. Additionally, understanding the socioeconomic factors influencing HIV prevalence can aid in designing tailored interventions. For instance, regions with lower HDI may benefit from programs that integrate economic development with health education, tackling the root causes of vulnerability to HIV [39].
From a theoretical standpoint, the socioeconomic determinants included in our analysis—such as GDP per capita, HDI, urban population ratio, and poverty rate—are known to influence health outcomes through several mechanisms, as outlined by the WHO Social Determinants of Health framework. Improved GDP and HDI generally reflect increased access to healthcare services, better education, and awareness, all of which are critical for early HIV diagnosis. Therefore, the observed strong positive correlations between HIV case reporting and variables like GDP per capita and urbanization do not necessarily indicate a higher disease burden, but rather an enhanced diagnostic capability in more developed and urbanized regions. Conversely, the negative correlation with poverty and rural population may reflect healthcare access limitations and underreporting in these areas.
We acknowledge that correlation-based analyses, such as those presented in the heatmap and pair plots, do not establish causality. These results are interpreted as associations that highlight important patterns but do not imply direct cause-and-effect relationships. Importantly, the associations revealed through the correlation and scatter plots can serve as the basis for a conceptual model linking socioeconomic progress to HIV-related health outcomes. We now suggest that future studies could build on our findings by developing and testing such theoretical models using more advanced statistical tools suited for causal analysis. This may include integrating time-lag effects, mediating variables (e.g., stigma reduction, testing coverage), and spatial–temporal variations.
4.5. HIV Indicators for Testing
The data in Table 4 provides critical insights into HIV testing trends in Bangladesh from 2018 to 2023, reflecting progress in targeted interventions and persistent gaps that require attention. Testing among key populations (KPs), which include groups at high risk such as sex workers, injecting drug users, and men who have sex with men, increased significantly over the years, from 33,883 in 2018 to 82,825 in 2023. This upward trend underscores the impact of enhanced outreach efforts and awareness campaigns targeting vulnerable populations. These interventions align with global best practices for addressing HIV epidemics in concentrated populations, where early detection and treatment linkage are vital to controlling transmission [17].

Table 4.
HIV indicators for testing [33].
Testing for TB-HIV comorbidities showed a dramatic increase from 16,087 in 2020 to 77,897 in 2023. This rise reflects improved integration of HIV screening into tuberculosis programs, an essential strategy in high-burden settings where co-infections are common. The surge aligns with recommendations from global health organizations advocating for the simultaneous management of TB and HIV to optimize early detection and patient outcomes. The integration of services not only improves diagnostic capabilities but also reduces barriers to accessing care for individuals who may otherwise go undiagnosed.
Efforts in the Prevention of Mother-To-Child Transmission (PMTCT) of HIV have also been critical, with the number of tests peaking at 113,219 in 2021. This peak likely corresponds to heightened global initiatives emphasizing the elimination of vertical transmission. However, the decrease to 81,615 in 2023 indicates potential challenges in maintaining consistent programmatic reach. These fluctuations emphasize the importance of sustained investment in antenatal HIV screening and ensuring the availability of antiretroviral therapy for pregnant women, as these are key components of successful PMTCT interventions [39].
Interestingly, there are no recorded figures for safe blood transfusion practices (SBTP) across the years. While this might indicate a strong pre-screening mechanism that minimizes the need for separate reporting, it raises questions about the completeness of data collection in this area. Blood transfusion safety remains a cornerstone of HIV prevention, and further investigation into the status of these practices in Bangladesh could provide valuable insights.
The data highlights significant achievements, particularly in scaling up testing among high-risk populations and integrating HIV-TB care. However, the observed variations in PMTCT testing and the absence of SBTP data suggest areas where improvements are needed. Strengthening program integration, ensuring sustained resources, and expanding access to underserved populations will be crucial in addressing these gaps and maintaining progress in HIV prevention and care.
4.6. HIV Impact and Gender
The data in Table 5 illustrates the gendered impact of HIV in Bangladesh from 2016 to 2023, revealing disparities that underscore the need for targeted interventions tailored to different demographic groups. Across the years, males consistently account for the majority of HIV cases, with proportions ranging from 65% in 2016 to 76% in 2021 and 2020. This trend highlights the ongoing vulnerabilities among men, particularly those in high-risk groups such as injecting drug users, migrant workers, and men who have sex with men [40]. The high proportion of male cases may reflect both behavioral risk factors and greater access to testing services in comparison to other genders.

Table 5.
HIV impact on gender [33].
The percentage of females affected by HIV has fluctuated, peaking at 33% in 2016 before declining to 24% in 2023. While this decrease could indicate progress in addressing some of the factors contributing to HIV risk among women, such as mother-to-child transmission and sexual violence, it also raises questions about potential underdiagnosis or barriers to accessing healthcare services for women. Gender norms and stigma may further deter women from seeking HIV testing or treatment, necessitating more inclusive and empowering healthcare strategies to ensure equitable access [39].
Transgender individuals, while consistently representing a small proportion of cases, face unique vulnerabilities and systemic barriers that exacerbate their risk of HIV. The proportion of transgender individuals among HIV cases fluctuates slightly, with a peak of 3% in 2020 before declining to 1% in 2023. These figures likely underrepresent the true burden of HIV in transgender populations due to stigma, discrimination, and underreporting. Targeted interventions, including community-based outreach programs, inclusive healthcare services, and anti-discrimination policies, are essential to address the unique challenges faced by this group [38].
4.7. Trend in Marital Status and HIV Susceptibility in Bangladesh
Table 6 highlights the trends in marital status among individuals living with HIV in Bangladesh from 2016 to 2023, showing a notable increase in the proportion of infections among single individuals. In 2016, single individuals accounted for only 17.99% of reported HIV cases, but by 2023, this percentage had risen to 31.50%, reflecting a steady upward trend. On the other hand, the proportion of married individuals diagnosed with HIV has relatively decreased in the years 2021 to 2023 compared to 2020 and before. Divorced and widowed individuals have consistently accounted for smaller shares of HIV cases, though their percentages have fluctuated slightly over the years.

Table 6.
HIV susceptibility based on marital status [33].
The steady increase in HIV cases among single individuals can be attributed to multiple factors. First, changing societal norms and attitudes toward sexual activity may play a significant role. With urbanization and globalization, younger populations, particularly those who are single, may be engaging in higher-risk behaviors, such as unprotected sex or multiple sexual partnerships, which increases their susceptibility to HIV infection [17]. These behavioral changes may stem from evolving social dynamics where premarital sexual activity is becoming more common, albeit often in a context lacking adequate sexual education or access to preventive measures.
The growing vulnerability of single individuals to HIV has critical implications for public health policy in Bangladesh. This demographic may not perceive themselves to be at high risk of infection, leading to lower engagement with prevention programs. Awareness campaigns should, therefore, target single populations with messaging tailored to their specific vulnerabilities and behaviors. Comprehensive sexual education programs, particularly for youth and unmarried individuals, are essential to reducing risky behaviors and encouraging safe practices such as condom use [38,40,41,42].
Additionally, the decreasing proportion of HIV cases among married individuals suggests that prevention strategies targeting this group, such as programs promoting antenatal HIV screening and PMTCT, have been relatively effective. However, divorced and widowed individuals remain underrepresented in current data and prevention efforts. These groups may also face significant stigma and barriers to accessing healthcare, requiring targeted interventions to address their unique vulnerabilities [16].
4.8. Age Distribution Trends of HIV in Bangladesh (2016–2023)
Table 7 illustrates the age distribution of individuals living with HIV in Bangladesh from 2016 to 2023, revealing critical patterns across different age groups. The youngest age groups, particularly children aged 0–5 years, exhibit a relatively small percentage of total cases, ranging from 1.00% to 3.20% over the years. These cases are most likely a result of vertical transmission (mother-to-child), indicating gaps in PMTCT programs despite some progress in antenatal HIV screening and interventions [43]. Irregular fluctuations in diagnosis among children could reflect underreporting, limited testing, or varying effectiveness of targeted interventions.

Table 7.
Age distribution trends of HIV in Bangladesh (2016–2023) [33].
A concerning trend is observed in the 19–24 year age group, which shows a steady increase in the proportion of HIV cases, rising from 6.75% in 2016 to 16.54% in 2023. This age group is typically the target of social awareness programs and education campaigns aimed at promoting safe sexual practices and reducing risky behaviors. The consistent rise in infections within this demographic suggests that these programs may not be achieving their intended impact, particularly in effectively reaching young adults. Factors such as inconsistent messaging, stigma, and lack of access to preventive resources may hinder their effectiveness [17].
The majority of HIV cases are concentrated in the 25–49 year age group, which consistently accounts for the highest proportion of infections, ranging from 65.05% to 77.39% over the years. This age group represents the economically active population, many of whom are migrant workers, sex workers, or individuals engaging in high-risk behaviors. The prevalence in this group underscores the need for sustained interventions, including targeted testing, access to ART, and community-based education programs to reduce transmission [40].
The 50+ year age group has shown a slight but steady increase in cases, rising from 9.84% in 2018 to 13.00% in 2021, before stabilizing around 11% in 2023. This trend highlights the necessity of addressing misconceptions that HIV predominantly affects younger populations. Older adults may face unique barriers to diagnosis and treatment, such as stigma and lack of targeted healthcare services, requiring tailored interventions to ensure comprehensive HIV care for all age groups [16].
The data indicates that while PMTCT programs are helping reduce vertical transmission among younger children, further efforts are needed to ensure complete elimination of this preventable mode of HIV transmission. Expanding access to antenatal HIV screening and ART for pregnant women can significantly mitigate infections in the 0–5 year age group [44,45].
For the 19–24 year age group, the steady increase in HIV cases highlights the need to strengthen social awareness campaigns and education initiatives. Campaigns should be modernized and tailored to effectively reach younger populations through platforms they engage with, such as social media. Additionally, comprehensive sexual education in schools and universities should be prioritized to address misconceptions about HIV and promote safe practices [41].
The high prevalence in the 25–49 year age group necessitates targeted interventions for high-risk populations, particularly migrant workers and individuals engaging in unprotected sex. Mobile clinics, workplace awareness programs, and expanded access to HIV testing in urban and peri-urban areas could help reduce the burden in this demographic [46,47].
For the 50+ year age group, greater emphasis should be placed on reducing stigma and ensuring access to diagnosis and treatment. Awareness campaigns should also address misconceptions that older adults are not at risk for HIV, fostering a culture of inclusivity in prevention and care [48,49,50].
The age distribution trends of HIV in Bangladesh reveal both successes and challenges in addressing the epidemic across different demographics. While progress is evident in reducing mother-to-child transmission, the increasing susceptibility of younger adults to HIV and the consistent prevalence in the 25–49 year age group demand renewed focus on targeted interventions. A multi-pronged approach that includes strengthened prevention programs, expanded testing facilities, and tailored community outreach efforts is critical to reducing the burden of HIV across all age groups [10,38,51].
4.9. Gender Based ART Coverage (Antiretroviral Therapy)
The data in Table 8 highlights the gender-based antiretroviral therapy (ART) coverage trends in Bangladesh from 2018 to 2023, reflecting both progress and persistent gaps in addressing the HIV epidemic across different gender groups. ART coverage among males has shown a steady increase, rising from 47.99% in 2018 to 66.61% in 2023. This trend suggests improvements in the availability and accessibility of treatment services for men, who constitute the majority of reported HIV cases in Bangladesh [40]. However, the consistent disparity between male and female coverage raises concerns about gender equity in HIV treatment access.

Table 8.
Gender-based ART coverage [33].
Females, accounting for a smaller proportion of HIV cases, exhibit fluctuating ART coverage, with a peak of 28.81% in 2021, followed by a decline to 21.79% in 2023. The observed variations may reflect systemic barriers, including stigma, limited healthcare access, and gender norms that deter women from seeking treatment [39]. The data for transgender individuals, while consistently low, shows some improvement, increasing from 0.58% in 2018 to 1.98% in 2020 before declining to 0.71% in 2023. The low ART coverage among transgender individuals highlights their unique vulnerabilities, often exacerbated by social exclusion, discrimination, and inadequate representation in healthcare programs [38].
4.10. Prevention of Mother-to-Child Transmission (PMTCT) Performance
The data in Table 9 provides an overview of the performance of Prevention of Mother-to-Child Transmission (PMTCT) programs in Bangladesh from 2018 to 2023. These programs aim to eliminate vertical transmission of HIV by ensuring early detection and treatment for HIV-positive pregnant women and monitoring the health outcomes of their newborns.

Table 9.
PMTCT performance [33].
The total number of pregnant women tested for HIV has shown fluctuations over the years, with the highest number of tests conducted in 2021 (109,087) and lower figures in 2019 (69,941) and 2018 (66,701). This variability may reflect shifts in resource allocation, outreach efforts, and healthcare system priorities. However, the consistent inclusion of HIV testing in antenatal care underscores progress in integrating PMTCT strategies into routine maternal health services [39]. The number of new HIV-positive pregnant women identified annually has decreased significantly, from 147 in 2018 to 21 in 2023. This decline could be attributed to targeted interventions, such as enhanced antenatal screening and public health campaigns, aimed at high-risk groups. The data also reveals that the proportion of HIV-positive pregnant women receiving ART has improved over time. For instance, in 2023, 35 out of 21 newly identified HIV-positive pregnant women were on ART. This coverage rate suggests strengthened efforts to ensure timely treatment, which is critical to reducing the risk of mother-to-child transmission. The health outcomes for live births among HIV-positive mothers indicate promising progress. Most newborns tested were HIV-negative, with no reported positive cases in 2020 and 2021. These results demonstrate the effectiveness of ART in preventing vertical transmission. However, the occasional HIV-positive cases, such as in 2019 (two cases) and 2018 (two cases), highlight the need for sustained vigilance and continuous improvement in PMTCT program coverage and quality [40]. The trends in PMTCT performance suggest that while significant progress has been made, consistent testing, treatment coverage, and resource allocation remain critical to achieving the goal of zero mother-to-child transmission of HIV. Addressing gaps in rural and underserved regions, where healthcare access may be limited, will further strengthen the national PMTCT strategy.
4.11. Population Category Among Newly Diagnosis People Living with HIV (PLHIV)
The data in Table 10 highlights the distribution of newly diagnosed people living with HIV (PLHIV) across various population categories in Bangladesh from 2019 to 2023. This breakdown reveals important trends in how the epidemic is concentrated among high-risk and general populations, shedding light on the effectiveness of targeted interventions and the shifting dynamics of the HIV burden.

Table 10.
Population category among newly diagnosed people living with HIV (PLHIV) [33].
The proportion of newly diagnosed cases among people who inject drugs (PWID) fluctuates significantly, peaking at 24% in 2019 before declining to 13.1% in 2023. This decline suggests some success in harm reduction initiatives, such as needle exchange programs and education campaigns, aimed at reducing transmission within this high-risk group [37]. However, the persistently high proportions indicate that more efforts are needed to sustain progress, particularly in providing access to HIV testing and ART for PWID.
Men who have sex with men (MSM) consistently account for a significant proportion of newly diagnosed cases, rising from 5% in 2020 to 18.2% in 2023. This upward trend underscores the need for targeted outreach programs and de-stigmatized healthcare access for MSM, as stigma and discrimination often prevent individuals in this group from seeking timely diagnosis and treatment [40]. Similarly, the proportion of male sex workers (MSW) has increased slightly, highlighting the ongoing vulnerability of this subgroup, which may face compounded risks due to social and economic barriers.
The proportion of transgender (TG) individuals diagnosed with HIV remains low but relatively stable, ranging between 1% and 2% over the years. Despite their smaller representation, TG individuals often face systemic barriers to healthcare access and social support, making targeted and inclusive interventions essential to reducing their vulnerability [39].
Migrant workers consistently represent a significant portion of new diagnoses, with their share ranging from 15% in 2020 to 17.6% in 2023. Migration-related vulnerabilities, such as lack of access to healthcare, social disconnection, and exploitation, contribute to this high representation. This underscores the need for pre-departure and post-arrival HIV prevention and testing programs tailored to this population [10].
The general population (GPoP) accounts for the largest proportion of new diagnoses, peaking at 37% in 2019 before decreasing to 27.7% in 2023. While this indicates a broader spread of HIV outside traditionally high-risk groups, it also emphasizes the importance of continued public awareness campaigns and expanded access to testing and treatment services for the general population.
The data also captures the significant representation of Forcibly Displaced Myanmar Nationals (FDMN), or Rohingya refugees, who account for 12.4% of new diagnoses in 2023, down from a peak of 26% in 2021. The high initial burden among FDMN likely reflects vulnerabilities related to displacement, lack of healthcare access, and poor living conditions in refugee camps. Targeted humanitarian responses and the integration of HIV services into refugee healthcare systems remain critical for managing this group’s vulnerabilities [52].
4.12. Bangladesh and the 95-95-95 HIV Targets
The 90-90-90 targets, set by UNAIDS in 2014, aimed to ensure that by 2020, 90% of all people living with HIV (PLHIV) would know their status, 90% of those diagnosed would receive antiretroviral therapy (ART), and 90% of those on treatment would achieve viral suppression. While globally these targets have accelerated the response to HIV, Bangladesh has faced unique challenges in meeting them due to its low prevalence of HIV and the disproportionate impact on high-risk groups such as injecting drug users, sex workers, and migrant workers [53,54,55].
In recent years, Bangladesh has transitioned to adopting the 95-95-95 targets for 2030, which aim to further enhance progress by increasing each threshold to 95% [56]. According to the National AIDS/STD Program [11], significant strides have been made, particularly in diagnosing PLHIV and expanding ART coverage. By 2024, Bangladesh reported that approximately 77% of PLHIV were aware of their status, 78% of those diagnosed were receiving ART, and 91% of individuals on treatment had achieved viral suppression [13]. These figures indicate notable progress but also highlight gaps in early diagnosis and linkage to care. Factors such as stigma, limited healthcare infrastructure, and underreporting in rural areas remain barriers to achieving the targets fully. The following table shows the stats regarding 95-95-95 HIV targets.
The proportion of PLHIV aware of their status has increased steadily from 50% in 2018 to 73% in 2023, as presented in Table 11. This improvement reflects enhanced public awareness campaigns, expanded access to HIV testing, and reductions in stigma associated with diagnosis. However, the figure remains far below the 95% target, indicating that many individuals, particularly in marginalized or hard-to-reach populations, are still unaware of their status. To address this gap, targeted outreach and community-based interventions are crucial. Similarly, the percentage of diagnosed individuals receiving ART improved from 60% in 2018 to 75% in 2023, as presented in Table 11. Despite this progress, the rate of improvement has slowed in recent years, with only marginal increases since 2020. Structural barriers such as limited healthcare access, stigma, and logistical challenges in ensuring consistent ART availability contribute to this plateau. Addressing these barriers is critical to scaling up ART coverage and ensuring uninterrupted treatment for those diagnosed. The most consistent success has been observed in the proportion of individuals achieving viral suppression once on ART. This metric increased from 85% in 2019 to 93% in 2021, stabilizing at 90% in subsequent years.

Table 11.
95-95-95 HIV targets [33].
To achieve the ambitious 95-95-95 targets, Bangladesh must focus on expanding HIV testing, improving ART coverage, and strengthening targeted outreach to marginalized populations while reducing stigma. Sustained investments in public awareness campaigns and healthcare infrastructure, particularly in rural and underserved areas, are essential. Community-driven programs, stronger healthcare systems, and adequate funding will be critical to addressing structural barriers and ensuring equitable access to HIV prevention and treatment services. By enhancing efforts to reach high-risk populations and ensuring consistent support for those in care, Bangladesh can make significant progress toward ending the HIV epidemic and achieving the 95-95-95 targets by 2030.
5. Awareness and Mitigation Strategy
HIV prevention and mitigation efforts in Bangladesh have evolved significantly over the past two decades. While the country has maintained one of the lowest HIV prevalence rates globally, the epidemic remains concentrated among high-risk and marginalized populations. Taking on these challenges head-on requires a multifaceted approach that combines public awareness, targeted interventions, and strengthened healthcare systems [56]. The success of any strategy hinges on its ability to address both the structural and individual barriers that perpetuate vulnerabilities.
Throughout this period, targeted interventions played a critical role in containing the epidemic. These included needle exchange programs for IDUs, condom promotion campaigns for sex workers, and ART to prevent mother-to-child transmission [57,58]. Efforts to raise awareness among marginalized populations have also improved, particularly following studies emphasizing the importance of education and positive attitudes toward HIV prevention among women [12]. Despite these successes, ongoing vulnerabilities remain, particularly for underserved groups like female street child laborers who face compounded socioeconomic and healthcare barriers, making them more susceptible to risks such as HIV infection [59].
Moreover, gender disparities in knowledge and empowerment underscore the importance of enhancing women’s agency in combating HIV [60]. Dealing with these challenges requires a comprehensive, evidence-based approach to strengthen public health responses and reduce the burden of HIV in Bangladesh [10].
Research highlights significant gaps in HIV knowledge across different population groups. For instance, a study among primary school teachers in Bangladesh revealed that while awareness about HIV was relatively high, misconceptions about transmission persisted, demonstrating the need for comprehensive training programs to address these gaps [61]. Similarly, adolescents represent a critical demographic for awareness campaigns, as they often have incomplete or incorrect knowledge about HIV. A cross-sectional study found that while many adolescents had heard of HIV, their understanding of transmission and prevention was limited, underscoring the need for age-appropriate education programs [62].
Secondary school students are another key target group for educational interventions. Training teachers to deliver HIV education has proven effective in improving knowledge among students. Sarma et al. [63] demonstrated that teacher training programs significantly enhanced students’ understanding of HIV, suggesting that well-trained educators can act as catalysts for spreading accurate information. Similarly, a study by Sarma and Oliveras [64] emphasized that integrating HIV education into school curricula not only increases awareness but also reduces stigma and misconceptions among students.
The role of higher education institutions in promoting awareness is also crucial. A study among tertiary students found that while many had a basic understanding of HIV, deeper knowledge about preventive practices and the social implications of HIV was lacking [65]. Incorporating comprehensive HIV modules into university curricula can help bridge this gap and prepare young adults to make informed decisions.
Community-based interventions and gender-sensitive programs are vital for addressing disparities in knowledge. Women, particularly those in rural areas, often face restricted access to health information due to cultural norms and limited autonomy. Programs designed to empower women through education and community engagement can significantly improve their awareness and reduce vulnerability [66]. Furthermore, a study by Hosain and Islam [67] highlighted the importance of targeting marginalized populations, such as sex workers and transgender individuals, with tailored educational initiatives to ensure equitable access to information.
Educational awareness initiatives in Bangladesh must address the unique cultural, social, and economic contexts of its population. By leveraging trained educators, community engagement, and digital tools, such programs can empower individuals with the knowledge and resources necessary to prevent HIV transmission and promote health-seeking behaviors [68].
Gender disparities in knowledge about HIV also highlight the importance of targeted interventions for women. Female populations in Bangladesh often face restricted access to health information due to cultural norms and limited autonomy, leading to higher vulnerabilities [51]. Campaigns designed specifically for women, emphasizing empowerment and access to healthcare services, can address these disparities. For instance, programs encouraging dialogue about HIV prevention within families and communities have proven effective in enhancing awareness and reducing stigma for women and their families [69].
Digital media and technology also offer new opportunities to expand awareness. Social media platforms and mobile health applications can deliver tailored messaging to younger audiences, addressing misconceptions and promoting preventive behaviors [70]. These tools can complement traditional methods by reaching broader audiences and engaging individuals in more interactive and accessible ways.
Moving forward, Bangladesh must address these key challenges by strengthening healthcare delivery systems, enhancing public awareness, and tackling urban–rural inequities [71]. Furthermore, tackling the underlying social determinants of health and enhancing the resilience of marginalized and high-risk populations are critical for achieving sustained progress in managing and reducing the impact of the HIV epidemic [72].
6. Future Research Directions
Based on the review of current literature and data, we have been able to single out several areas of interest for future research:
- It was seen that the dynamics of HIV infection have changed in several ways in recent years. The relationship between cultural changes and the steady increase in HIV in youth and single populations warrants further investigation.
- Based on our review of the current state of HIV and the study data, we found that the number of infected among the age group of 19 to 24 years has steadily increased from 2016 to 2023. Further research is required to pinpoint the social, economic, and other viable reasons behind this steady increase, as this group is generally the most targeted group for social awareness and education campaigns.
- Single people showed a steady increase in HIV-positive counts. Further focused research is required to explore the reasons behind this increase and whether this increase is due to underreporting or if this group poses a high risk for HIV infection.
- Not enough research or data were found that studied the difference in urban and rural disparities in the transmission of HIV.
- Bangladesh is a very socially conservative country. Future studies can be carried out to assess the impact of social stigma on healthcare-seeking behavior and develop interventions to reduce discrimination against people living with HIV.
- The effectiveness of digital health tools in increasing awareness, testing, and treatment adherence requires further evaluation, particularly in underserved regions.
- The influence of socioeconomic factors, including poverty, gender inequality, and education levels, on HIV transmission and prevention should be examined further for trends and patterns.
- Sustained monitoring and research on the long-term effectiveness of antiretroviral therapy (ART) in improving quality of life and reducing transmission rates among different demographic groups are required.
- More extensive research on PMTCT programs is required, focusing on factors contributing to incomplete ART coverage for pregnant women in rural areas and risk populations.
- We must analyze gaps in the existing healthcare system to propose scalable models for HIV care and prevention. This is particularly relevant in terms of the differences between healthcare infrastructure in rural and urban regions and how healthcare facilities and policies can be improved to address high-risk populations.
- Investigating the role of cross-border migration in HIV transmission dynamics and developing strategies to address regional challenges.
These points provide a framework for advancing research to address gaps and improve HIV prevention and care in Bangladesh.
7. Conclusions
The HIV epidemic in Bangladesh remains low in prevalence but presents significant challenges. Between 2000 and 2024, testing, treatment access, and awareness have improved, especially among high-risk populations. Furthermore, certain groups, such as individuals aged 19 to 24 and those who are single, show a steady increase in HIV-positive cases, warranting further investigation. However, disparities in healthcare access, stigma, and underdiagnosis persist, particularly in rural and marginalized groups. Key populations, including people who inject drugs, men who have sex with men, sex workers, transgender individuals, and migrant workers, are the most affected. Tailored interventions are necessary to address their needs. While socioeconomic improvements have strengthened healthcare infrastructure and diagnostic capacity, they have not been evenly distributed, leaving rural and underserved populations vulnerable. Programs like PMTCT and ART show promise in reducing transmission and improving survival, but gaps in implementation require urgent attention. To meet the 95-95-95 targets by 2030, investments in public health, education, and healthcare accessibility, alongside efforts to reduce stigma and address social determinants of health, are essential. A collaborative, inclusive approach will be vital to sustaining progress and addressing emerging challenges.
Author Contributions
A.B.: methodology, software, data curation, writing—original draft preparation, visualization, investigation. M.H.: methodology, software, data curation, writing—original draft preparation, visualization, investigation. M.S.: writing—reviewing and editing. G.S.: conceptualization, data curation, supervision, writing—reviewing and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable, as no human participants were involved.
Data Availability Statement
All data are available in the manuscript.
Acknowledgments
The authors used AI-assisted technology (ChatGPT-3.5) for language editing and grammar checking.
Conflicts of Interest
All authors declared that there are no conflicts of interest to disclose.
References
- UNAIDS. Global HIV/AIDS Statistics, 2023. Available online: https://www.unaids.org/en/resources/documents/2023/2023_unaids_data (accessed on 26 December 2024).
- Sharp, P.M.; Hahn, B.H. Origins of HIV and the AIDS pandemic. Cold Spring Harb. Perspect. Med. 2011, 1, a006841. [Google Scholar] [CrossRef] [PubMed]
- Faria, N.R.; Rambaut, A.; Suchard, M.A.; Baele, G.; Bedford, T.; Ward, M.J.; Tatem, A.J.; Sousa, J.D.; Arinaminpathy, N.; Pépin, J.; et al. HIV epidemiology. Science 2014, 346, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Keele, B.F.; Van Heuverswyn, F.; Li, Y.; Bailes, E.; Takehisa, J.; Santiago, M.L.; Bibollet-Ruche, F.; Chen, Y.; Wain, L.V.; Liegeois, F.; et al. Chimpanzee reservoirs of pandemic and nonpandemic HIV-1. Eur. J. Immunol. 2006, 37, 673–679. [Google Scholar] [CrossRef]
- Des Jarlais, D.C.; Perlis, T.; Arasteh, K. HIV incidence among injecting drug users in New York City, 1990 to 2001: Declining and widening racial/ethnic disparities. Am. J. Public Health 2001, 95, 1439–1445. [Google Scholar] [CrossRef]
- De Cock, K.M.; Fowler, M.G.; Mercier, E.; de Vincenzi, I.; Saba, J.; Hoff, E.; Alnwick, D.J.; Rogers, M.; Shaffer, N. Prevention of mother-to-child HIV transmission in resource-poor countries: Translating research into policy and practice. JAMA 2000, 283, 1175–1182. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). How HIV Spreads, 2022. Available online: https://www.cdc.gov/hiv/causes/index.html (accessed on 26 December 2024).
- Centers for Disease Control and Prevention (CDC). HIV Occupational Transmission, 2022. Available online: https://www.cdc.gov/hiv/causes/occupational-transmission.html (accessed on 26 December 2024).
- Wahab, M.; Mollah, A.H.; Bardhan, J. Bangladesh is threatened by the HIV epidemic during the Rohingya refugee crisis. Infect. Dis. 2024, 56, 78–80. [Google Scholar] [CrossRef]
- Rahman, M.; Islam, F.; Rahaman, S.; Sultana, N.A.; Fahim, N.F.; Ahmed, M. Studies on the prevalence of HIV/AIDS in Bangladesh including other developing countries. Adv. Tradit. Med. 2021, 23, 647–658. [Google Scholar] [CrossRef]
- National AIDS/STD Program (NASP.) Annual Report of the National AIDS/STD Program (Bangladesh), 2020. Ministry of Health and Family Welfare, Government of Bangladesh. Available online: https://asp.portal.gov.bd/sites/default/files/files/asp.portal.gov.bd/publications/1033aeb6_8ac6_43a1_9126_04de2b8bfaf9/2021-02-24-14-12-c87fc40d8bfd0d2fca748e57fb5b257c.pdf (accessed on 26 December 2024).
- Billah, M.A.; Mohd Yusof, R.A.A.; Khan, M.N.; Mat Min, R. Comprehensive knowledge and positive attitudes regarding HIV/AIDS among reproductive-aged women in Bangladesh and their associated factors: A cross-sectional study using the Multiple Indicator Cluster Survey 2019. medRxiv 2024, 1–33. [Google Scholar] [CrossRef]
- National AIDS/STD Program (NASP). HIV/AIDS Situation in Bangladesh: Annual Report 2024. Ministry of Health and Family Welfare, Government of Bangladesh. Available online: https://asp.portal.gov.bd/sites/default/files/files/asp.portal.gov.bd/page/febb60ca_6e01_40df_89d7_e4b23954e191/2024-12-01-08-48-353bfca697dde75ef03c2be2c971f6fd.pdf (accessed on 26 December 2024).
- Haque, M.A.; Hossain, M.S.N.; Chowdhury, M.A.B.; Uddin, M.J. Factors associated with knowledge and awareness of HIV/AIDS among married women in Bangladesh: Evidence from a nationally representative survey. SAHARA-J. J. Soc. Asp. HIV/AIDS 2018, 15, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Bhowmik, J.; Biswas, R.K. Knowledge about HIV/AIDS and its transmission and misconception among women in Bangladesh. Int. J. Health Policy Manag. 2022, 11, 2542–2551. [Google Scholar] [CrossRef]
- Sultana, S. Impacts of internal stigma among the people living with HIV/AIDS in Bangladesh: An empirical account. Asian Soc. Sci. 2014, 10, 180–187. [Google Scholar] [CrossRef]
- Azim, T.; Chowdhury, E.I.; Reza, M.; Faruque, M.O.; Ahmed, G.; Khan, R.; Rahman, M.; Pervez, M.M.; Jana, S.; Strathdee, S.A. Prevalence of infections, HIV risk behaviors and factors associated with HIV infection among male injecting drug users attending a needle/syringe exchange program in Dhaka, Bangladesh. Subst. Use Misuse 2008, 43, 2124–2144. [Google Scholar] [CrossRef] [PubMed]
- Hosain, G.M.M.; Chatterjee, N. Beliefs, sexual behaviours and preventive practices with respect to HIV/AIDS among commercial sex workers in Daulatdia, Bangladesh. Public Health 2005, 119, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, S.A.I. TB and HIV/AIDS in Bangladesh. J. AIDS HIV Res. 2010, 2, 63–72. [Google Scholar]
- UNAIDS. Country Report: Bangladesh, 2018. Available online: https://www.unaids.org/sites/default/files/country/documents/BGD_2018_countryreport.pdf (accessed on 26 December 2024).
- AIDS Data Hub. Bangladesh Country Data 2022. Available online: https://www.aidsdatahub.org/resource/bangladesh-country-data-2022 (accessed on 26 December 2024).
- Mahmud, W.; Asadullah, M.N.; Savoia, A. Bangladesh’s achievements in social development indicators: Explaining the puzzle. Econ. Political Wkly. 2013, 48, 26–28. [Google Scholar]
- Khandker, S.R.; Mahmud, W. Seasonal Hunger and Public Policies: Evidence from Northwest Bangladesh; World Bank Publications: Washington, DC, USA, 2012. [Google Scholar]
- Mottaleb, K.A.; Sonobe, T. An Inquiry into the Rapid Growth of the Garment Industry in Bangladesh. Econ. Dev. Cult. Chang. 2011, 60, 67–89. [Google Scholar] [CrossRef]
- Rahman, M.M.; Alam, K. Clean energy, population density, urbanization and environmental pollution nexus: Evidence from Bangladesh. Renew. Energy 2021, 172, 1063–1072. [Google Scholar] [CrossRef]
- Ahmed, S.M.; Islam, Q.S. Availability and rational use of drugs in primary healthcare facilities following the national drug policy of 1982: Is Bangladesh on right track? J. Health Popul. Nutr. 2012, 30, 99–108. [Google Scholar] [CrossRef]
- Riaz, B.K.; Islam, Z.; Islam, A.N.M.S.; Zaman, M.M.; Hossain, A.; Rahman, M.; Khanam, F.; Amin, K.M.B.; Noor, I.N. Risk factors for non-communicable diseases in Bangladesh: Findings of the population-based cross-sectional national survey 2018. BMJ Open 2020, 10, e041334. [Google Scholar] [CrossRef]
- Faruk, O.; Begum, N.; Rana, S. Trends of HIV/AIDS Epidemic and Awareness Levels in Bangladesh. Int. J. Data Sci. Technol. 2017, 3, 56–65. [Google Scholar] [CrossRef]
- World Bank. The Urbanization of Global Poverty; World Bank: Washington, DC, USA, 2007; Available online: https://documents.worldbank.org/en/publication/documents-reports/documentdetail/289981468314073224/the-urbanization-of-global-poverty (accessed on 30 December 2024).
- Rahman, M. Spatial Inequality in Socio-economic Development in Bangladesh: An Analysis. Soc. Indic. Res. 2023, 171, 1087–1109. [Google Scholar] [CrossRef]
- World Bank. Bangladesh Poverty Assessment: Facing Old and New Frontiers in Poverty Reduction; World Bank: Washington, DC, USA, 2019; Available online: https://documents1.worldbank.org/curated/en/793121572582830383/pdf/Bangladesh-Poverty-Assessment-Facing-Old-and-New-Frontiers-in-Poverty-Reduction.pdf (accessed on 26 December 2024).
- World Bank. Poverty Assessment for Bangladesh: Creating Opportunities and Bridging the East-West Divide (Bangladesh Development Series, Paper No. 26); World Bank: Dhaka, Bangladesh, 2008; Available online: https://hdl.handle.net/10986/28239 (accessed on 26 December 2024).
- National AIDS/STD Control (NASC). Directorate General of Health Services, Ministry of Health and Family Welfare. Available online: https://dghs.mohfw.gov.in/ (accessed on 26 December 2024).
- Bhowmik, A.; Hasan, M.; Redoy, M.M.H.; Saha, G. Nipah Virus Outbreak Trends in Bangladesh during the Period 2001 to 2024: A Brief Review. Sci. One Health 2024, 4, 100103. [Google Scholar] [CrossRef]
- World Life Expectancy. Bangladesh HIV/AIDS Statistics. Data Source: World Health Organization, 2020. Available online: https://www.worldlifeexpectancy.com/bangladesh-hiv-aids (accessed on 26 December 2024).
- Shabir, O. What is Case Fatality Rate (CFR)? News-Medical. Available online: https://www.news-medical.net/health/What-is-Case-Fatality-Rate-(CFR).aspx (accessed on 26 December 2024).
- Islam, S.M.S.; Conigrave, K.M. HIV and AIDS in Bangladesh: A review. Int. J. STD AIDS 2007, 18, 438–445. [Google Scholar]
- Haque, A.; Chowdhury, M.A.B.; Uddin, M.J. Knowledge of HIV/AIDS among married women in Bangladesh: Analysis of the 2019 Multiple Indicator Cluster Survey. AIDS Res. Ther. 2022, 19, 68. [Google Scholar] [CrossRef]
- UNAIDS. Global AIDS Monitoring 2021: Indicators for Monitoring the 2016 United Nations Political Declaration on Ending AIDS, 2020. Available online: https://www.aidsdatahub.org/sites/default/files/resource/unaids-global-aids-monitoring-2021.pdf (accessed on 29 December 2024).
- Azim, T.; Khan, S.I.; Haseen, F.; Huq, N.L.; Henning, L.; Pervez, M.; Chowdhury, M.E.; Sarafian, I. HIV and AIDS in Bangladesh. J. Health Popul. Nutr. 2008, 26, 311–324. [Google Scholar] [CrossRef]
- Fonner, V.A.; Armstrong, K.S.; Kennedy, C.E.; O’Reilly, K.R.; Sweat, M.D. School-based sex education and HIV prevention in low- and middle-income countries: A systematic review and meta-analysis. PLoS ONE 2014, 9, e89692. [Google Scholar] [CrossRef]
- Paul, A. HIV/AIDS in Bangladesh: Stigmatized People, Policy and Place; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar] [CrossRef]
- Rahman, M.A.; Kalam, A.; Al-Mamun, M. Unplanned urbanization and health risks of Dhaka City in Bangladesh: Uncovering the associations between urban environment and public health. Front. Public Health 2023, 11, 1269362. [Google Scholar] [CrossRef]
- Selph, S.S.; Bougatsos, C.; Dana, T.; Grusing, S.; Chou, R. Screening for HIV Infection in Pregnant Women: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2019, 321, 2349–2360. [Google Scholar] [CrossRef]
- Mugwaneza, P.; Lyambabaje, A.; Umubyeyi, A.; Humuza, J.; Tsague, L.; Mwanyumba, F.; Mutabazi, V.; Nsanzimana, S.; Ribakare, M.; Irakoze, A.; et al. Impact of maternal ART on mother-to-child transmission (MTCT) of HIV at six weeks postpartum in Rwanda. BMC Public Health 2018, 18, 1248. [Google Scholar] [CrossRef]
- Weine, S.M.; Kashuba, A.B. Labor Migration and HIV Risk: A Systematic Review of the Literature. AIDS Behav. 2012, 16, 1605–1621. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Migrant Health: Access to HIV Prevention, Treatment and Care for Migrant Populations in the EU/EEA, 2009. ECDC. Available online: https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/0907_TER_Migrant_health_HIV_Access_to_treatment.pdf (accessed on 26 December 2024).
- Emlet, C.A. A comparison of HIV stigma and disclosure patterns between older and younger adults living with HIV/AIDS. AIDS Patient Care STDs 2006, 20, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). HIV and Older Americans, 2020. Available online: https://hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-and-older-people (accessed on 26 December 2024).
- National Institute on Aging (NIA). HIV, AIDS, and Older Adults, 2021. Available online: https://www.nia.nih.gov/health/hiv-aids-and-older-adults (accessed on 26 December 2024).
- Tariqujjaman, M.; Hasan, M.; Kafi, M.A.H.; Hossain, A.; Khan, S.A.; Sultana, N.; Azad, R.; Hossain, A.; Rahman, M.; Hossain, M.B.; et al. Trends and correlates of low HIV knowledge among ever-married women of reproductive age: Evidence from cross-sectional Bangladesh Demographic and Health Survey 1996–2014. PLoS ONE 2023, 18, e0286184. [Google Scholar] [CrossRef] [PubMed]
- Bulstra, C.A.; Hontelez, J.A.C.; Otto, M.; Stepanova, A.; Lamontagne, E.; Yakusik, A.; El-Sadr, W.M.; Apollo, T.; Rabkin, M.; UNAIDS Expert Group on Integration; et al. Integrating HIV services and other health services: A systematic review and meta-analysis. PLoS Med. 2021, 18, e1003836. [Google Scholar] [CrossRef]
- Islam, M.M.; Conigrave, K.M.; Miah, S.; Kalam, K.A. HIV Awareness of Outgoing Female Migrant Workers of Bangladesh: A Pilot Study. J. Immigr. Minor. Health 2010, 12, 940–946. [Google Scholar] [CrossRef]
- Urmi, A.Z.; Leung, D.T.; Wilkinson, V.; Miah, M.A.A.; Rahman, M.; Azim, T. Profile of an HIV Testing and Counseling Unit in Bangladesh: Majority of New Diagnoses among Returning Migrant Workers and Spouses. PLoS ONE 2015, 10, e0141483. [Google Scholar] [CrossRef]
- Kabir, H.; Fatema, S.R.; Hoque, S.; Ara, J.; Maple, M. Risks of HIV/AIDS Transmission: A Study on the Perceptions of the Wives of Migrant Workers of Bangladesh. J. Int. Women’s Stud. 2020, 21, 379–394. [Google Scholar]
- Huq, M.N.; Khan, S.; Yasmin, S.; Hossain, M.M. Strategic investment and program effectiveness: A roadmap to ending AIDS in Bangladesh by 2030. AIDS Care 2024, 36, 1690–1703. [Google Scholar] [CrossRef] [PubMed]
- Khosla, N. HIV/AIDS interventions in Bangladesh: What can application of a social exclusion framework tell us? J. Health Popul. Nutr. 2009, 27, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.M.; Conigrave, K.M. HIV and sexual risk behaviors among recognized high-risk groups in Bangladesh: Need for a comprehensive prevention program. Int. J. Infect. Dis. 2008, 12, 363–370. [Google Scholar] [CrossRef]
- Sohel, M.S.; Alam, S.; Rahman, M.M.; Obaidullah, M.; Anam, A.S.M.T.; Hossain, B.; Hossain, M.A. Exploring the multifaceted vulnerabilities of female street child labor in the capital city of Bangladesh. Heliyon 2024, 10, e37302. [Google Scholar] [CrossRef]
- Magnani, E.; Piu, Z.A.; Sinha, K. Women’s agency and HIV/AIDS knowledge deprivation: An analysis of married women in Bangladesh. Fem. Econ. 2024, 30, 157–184. [Google Scholar] [CrossRef]
- Choudhary, M.S.R.; Rahman, M.M. Knowledge, awareness and perception about HIV/AIDS among primary school teachers in Bangladesh. Bangladesh J. Med. Sci. 2014, 13, 192–198. [Google Scholar] [CrossRef]
- Rahman, M.M.; Kabir, M.; Shahidullah, M. Adolescent knowledge and awareness about AIDS/HIV and factors affecting them in Bangladesh. J. Ayub Med. Coll. Abbottabad 2009, 21, 3–7. [Google Scholar] [PubMed]
- Sarma, H.; Islam, M.A.; Khan, J.R.; Chowdhury, K.I.A.; Gazi, R. Impact of teachers training on HIV/AIDS education program among secondary school students in Bangladesh: A cross-sectional survey. PLoS ONE 2017, 12, e0181627. [Google Scholar] [CrossRef]
- Sarma, H.; Oliveras, E. Implementing HIV/AIDS education: Impact of teachers’ training on HIV/AIDS education in Bangladesh. J. Health Popul. Nutr. 2013, 31, 20–27. [Google Scholar] [CrossRef]
- Hossain, M.B.; Kabir, M.A.; Ferdous, H. Knowledge of HIV and AIDS among Tertiary Students in Bangladesh. Int. Q. Community Health Educ. 2006, 26, 271–285. [Google Scholar] [CrossRef]
- Huda, M.N.; Amanullah, A. HIV/AIDS-related knowledge among secondary school students in Bangladesh: A cross-sectional study. Adv. Infect. Dis. 2013, 3, 274–280. [Google Scholar] [CrossRef]
- Hosain, M.T.; Islam, M.Z. Factors affecting knowledge, attitudes, and behavior of HIV/AIDS: A study on Bangladesh. Aust. J. Bus. Sci. Des. Lit. 2016, 9, 1–12. [Google Scholar]
- Pathfinder International. Advancing Digital Health to Improve the Sexual and Reproductive Health of Adolescents and Youth. Available online: https://www.pathfinder.org/publications/advancing-digital-health-to-improve-aysrhr-in-bangladesh/ (accessed on 26 December 2024).
- Mahmood, S. Female garment workers’ understandings of HIV in Bangladesh. Am. J. Public Health Res. 2021, 9, 81–89. [Google Scholar]
- Goodyear, V.A.; Armour, K.M. Young People’s Perspectives on and Experiences of Health-Related Social Media, Apps, and Wearable Health Devices. Soc. Sci. 2018, 7, 137. [Google Scholar] [CrossRef]
- Rahman, T.; Gasbarro, D.; Alam, K.; Alam, K. Rural–urban disparities in household catastrophic health expenditure in Bangladesh: A multivariate decomposition analysis. Int. J. Equity Health 2024, 23, 43. [Google Scholar] [CrossRef] [PubMed]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2010; Available online: https://apps.who.int/iris/handle/10665/44489 (accessed on 26 December 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).