Tracking HIV Outcomes Among Key Populations in the Routine Health Information Management System: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Systematic Review Registration and Methodological Approach
2.2. Inclusion and Exclusion Criteria of the Studies
2.3. Data Sources and Search Strategies
2.4. Study Selection and Data Extraction
2.5. Quality Appraisal
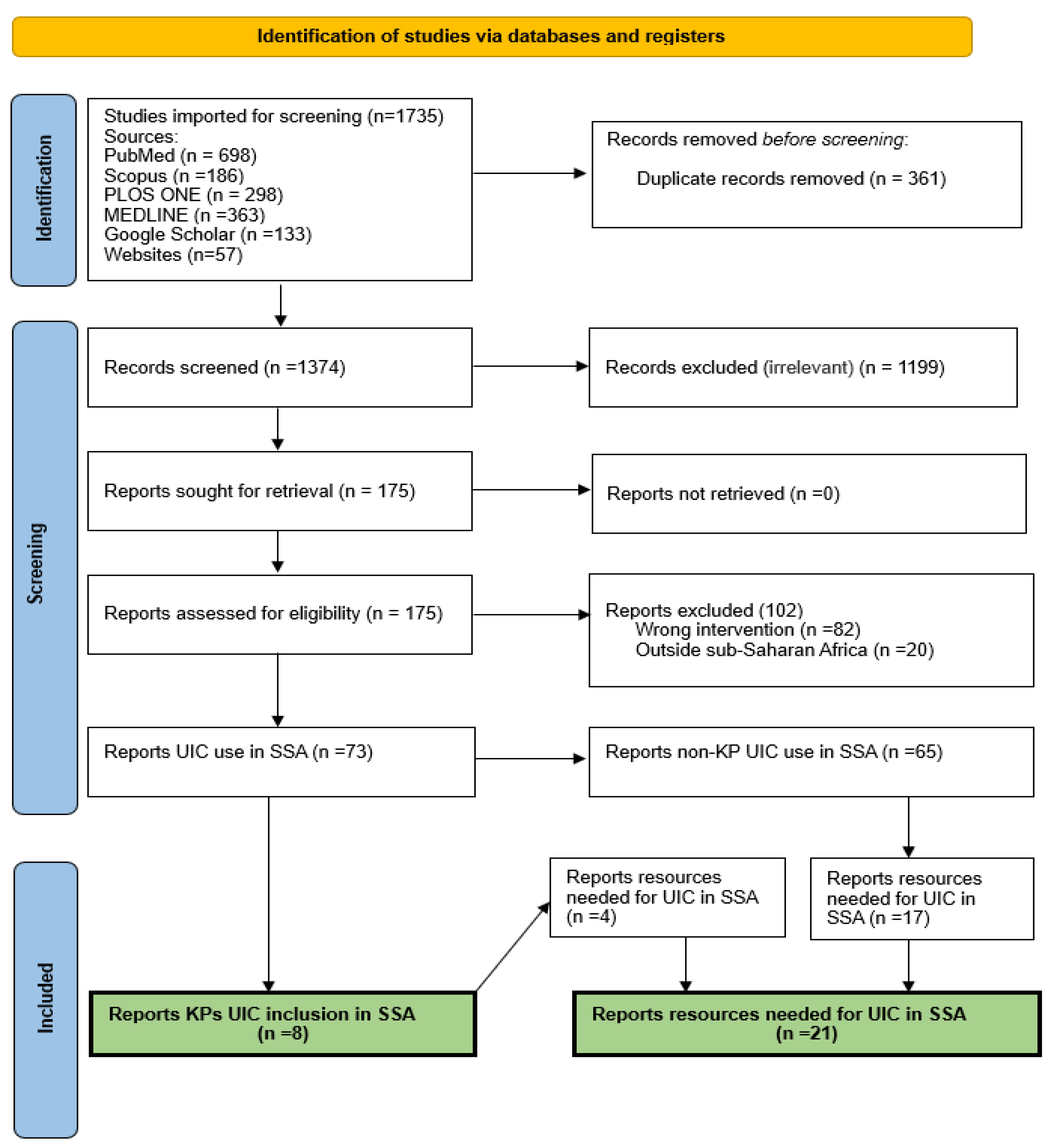
2.6. Summary of the Systematic Review Selection Process
3. Results
3.1. Studies That Included KPs’ UIC on the Government RHIMS
3.2. Methods Used to Create KPs’ UIC by Country
3.3. Resources Required for the Implementation of KPs’ UICs
| Author and Year | Country | UIC Type | Target Population | Title | Resources Mentioned | |
|---|---|---|---|---|---|---|
| 1. | National AIDS and STIs Control Programme (NASCOP), 2015 [17] | Kenya | Alphanumeric code | FSW/MSM/TG/PWUD/PWID | “Unique Identifier Code for Key Population Programmes in Kenya” | Technical support |
| 2. | Family Health International (FHI) 360, 2019 [21] | Liberia | Alphanumeric code | MSM, FSW and TG | “Linkages across the Continuum of HIV Services for Key Populations Affected by HIV (LINKAGES) Project” | SOP for UIC creation |
| Technical support | ||||||
| Human resources | ||||||
| Capacity building | ||||||
| Finance | ||||||
| 3. | Chapman et al., 2020 [22] | Uganda and Burundi | Alphanumeric code and Biometric fingerprint | FSW, TG, PWID, MSM, and people in prisons and closed settings | “Changing the landscape of data and digital health solutions” | Mobile and web based UIC App |
| Human resources | ||||||
| Finance | ||||||
| Capacity building | ||||||
| 4. | Bore et al., 2017 [23] | Mali | Alphanumeric code | FWS, partners of FSW and MSM | “Improving Key Population Tracking and Links to HIV Services Using Unique Identifier Codes in Mali” | Cellular reception |
| Electricity | ||||||
| 5. | Zan et al., 2016 [24] | Burkina Faso and Togo | Alphanumeric code | FSW and MSM | “Strategies and Resources for Implementing HIV Prevention, Care, and Treatment Programming with Key Populations in West Africa” | UIC system |
| Technical support | ||||||
| 6. | Odei-Lartey et al., 2016 [25] | Ghana | Biometric fingerprint | General population | “The application of a biometric identification technique for linking community and hospital data in rural Ghana” | UIC system |
| UIC card | ||||||
| Field notebooks | ||||||
| Desktop computers | ||||||
| Laptops | ||||||
| Laptop spare batteries | ||||||
| Fingerprint scanning device | ||||||
| License key for fingerprint scanning devices | ||||||
| Server space to store backups | ||||||
| 7. | Wall et al., 2015 [27] | Zambia | Biometric fingerprint | FSW | “Implementation of an electronic fingerprint-linked data collection system: a feasibility and acceptability study among Zambian female sex workers” | Fingerprint scanners |
| Tablets | ||||||
| Portable single-finger multi-spectral imaging sensor | ||||||
| Technical support | ||||||
| Finance | ||||||
| Capacity building | ||||||
| Central server | ||||||
| 8. | You et al., 2020 [28] | South Africa | Biometric fingerprint | FSW | “Facilitators and barriers to incorporating digital technologies into HIV care among cisgender female sex workers living with HIV in South Africa” | Biometric devices |
| 9. | Harichund et al., 2013 [29] | South Africa | Biometric fingerprint | HIV negative adult Females | “Participant verification: Prevention of co-enrolment in clinical trials in South Africa” | Computers |
| Laptops | ||||||
| Biometric software | ||||||
| Internet connection fees | ||||||
| IT technicians to install Biometric software. | ||||||
| 3G card for back-up | ||||||
| 10. | Snidal et al., 2015 [30] | Uganda | Biometric fingerprint | TB patients | “Use of eCompliance, an Innovative Biometric System for Monitoring of Tuberculosis Treatment in Rural Uganda” | Notebook computer |
| Biometric software | ||||||
| Fingerprint scanner | ||||||
| Training | ||||||
| Implementation cost | ||||||
| Hardware maintenance | ||||||
| Software support | ||||||
| 11. | Jaafa et al., 2021 [31] | Kenya | Biometric fingerprint | Clients on HIV care and treatment | “Implementation of Fingerprint Technology for Unique Patient Matching and Identification at an HIV Care and Treatment Facility, in Western Kenya: Cross-sectional Study” | Capacity building |
| Java Web Start (Oracle Corporation) | ||||||
| 12. | Sharkey et al., 2021 [32] | Zambia | Biometric fingerprint and manual fingerprint | HIV-Negative couples | “A cluster randomized trial to reduce HIV risk from outside partnerships in Zambian HIV-Negative couples using a novel behavioural intervention, “Strengthening Our Vows”: Study protocol and baseline data” | Tablet-based biometric software |
| Fingerprint ink | ||||||
| Papers | ||||||
| Wi-Fi router | ||||||
| 13. | Dalhatu et al., 2023 [34] | Nigeria | Biometric fingerprint | General ART patients | “From Paper Files to Web-Based Application for Data-Driven Monitoring of HIV Programs: Nigeria’s Journey to a National Data Repository for Decision-Making and Patient Care” | Internet services |
| Computer hardware | ||||||
| Human capacity | ||||||
| Skillsets | ||||||
| Personnel | ||||||
| 14. | Radmanovic, 2021 [36] | Uganda | Biometric fingerprint | Fisherfolks | “Biometric fingerprint technology for estimating frequent HIV testing and HIV incidence among mobile men women in fishing communities along Lake Victoria, Uganda” | Biometric identification system |
| 15. | Family Health International (FHI) 360, 2019 [40] | Mali | Alphanumeric code | FSW and MSM | “Unique identifier code create continuity and improve client tracking. A success story” | Capacity building |
| UIC system | ||||||
| Finance | ||||||
| Human resources | ||||||
| 16. | Harkaway N. 2019 [41] | Burkina Faso and Togo | Alphanumeric code | FSW and MSM | “The Unique Identifier Code (UIC) as a System to track Key Populations—The Experience of PACTE-VIH Project in Burkina Faso and Togo” | Capacity building |
| User manuals | ||||||
| Technical support | ||||||
| 17. | Bengtson et al., 2021 [42] | Malawi | Biometric fingerprint | Pregnant women with HIV and HCWs | “Improving monitoring of engagement in HIV care for women in Option B+: a pilot test of biometric fingerprint scanning in Lilongwe, Malawi” | Wireless internet |
| Battery-powered, handheld biometric fingerprint scanner | ||||||
| Web-based application to register fingerprints. | ||||||
| Bluetooth technology | ||||||
| Tablets | ||||||
| Fingerprint scanners | ||||||
| Centralized cloud-based location | ||||||
| 18. | Mazanderani et al., 2018 [43] | South Africa | Alphanumeric code | Babies done PCR testing after birth | “Leveraging the road to health booklet as a unique patient identifier to monitor the prevention of mother-to-child transmission programme” | Barcoded stickers |
| Barcoded sticker printer | ||||||
| Laminated barcoded peal-out card | ||||||
| Adhesive strips | ||||||
| 19. | Nyamhuno, 2019 [44] | South Africa | Biometric fingerprint | FSW | “Assessing the acceptability of biometrics in HIV prevention programme by Hillbrow sex workers” | Biometric devices |
| Computers | ||||||
| 20. | Global Fund, 2022 [45] | South Africa | Biometric fingerprint | AGYW | “Global Fund Grants in South Africa: Audit report” | Finance |
| Biometric devices | ||||||
| Capacity building | ||||||
| Human resources | ||||||
| 21. | White et al., 2018 [46] | Uganda | Biometric fingerprint | TB patient contacts | “Feasibility, acceptability, and adoption of fingerprint scanning during contact investigation for tuberculosis in Kampala, Uganda: A parallel-convergent, mixed-methods analysis” | Digital scanner |
| Training on fingerprints and biometric scanners |
3.4. Facilitators and Barriers for the Implementation of KPs’ UIC
3.4.1. Facilitators
3.4.2. Barriers
| Authors (Year) | Country Name | Study Title | KP | UIC Type | Facilitators | Barriers | |
|---|---|---|---|---|---|---|---|
| 1. | Wall et al., 2015 [27] | Zambia | “Implementation of an electronic fingerprint-linked data collection system: a feasibility and acceptability study among Zambian female sex workers” | FSW | Biometric fingerprint | Knowledge about technology | Misconception about technology |
| Location | Fear of the unknown | ||||||
| Time | Absence of peers | ||||||
| Confidentiality | Identity of officials taking fingerprints | ||||||
| Presence of peers | |||||||
| Trust | |||||||
| Identity of officials taking fingerprints | |||||||
| Incentives | |||||||
| 2. | You et al., 2020 [28] | South Africa | “Facilitators and barriers to incorporating digital technologies into HIV care among cisgender female sex workers living with HIV in South Africa” | FSW | Biometric fingerprint | Convenience | Long nails |
| Iris scan | Security | Fear of police | |||||
| Voice recognition | Reliability | Fear that the scanner may cause damage to the eyes | |||||
| Anonymity | System failure | ||||||
| Confidentiality | |||||||
| Precision | |||||||
| Accuracy | |||||||
| 3. | Family Health International (FHI) 360, 2019 [40] | Mali | “Unique identifier code creates continuity and improves client tracking | FSW and MSM | Alphanumeric code | Precision | |
| Accuracy | |||||||
| Trust | |||||||
| Confidentiality | |||||||
| 4. | Harkaway, 2019 [41] | Burkina Faso and Togo | “The Unique Identifier Code (UIC) as a System to track Key Populations The Experience of PACTE-VIH Project in Burkina Faso and Togo” | FSW and MSM | Alphanumeric code | Anonymity | Low literacy |
| Confidentiality | System maintenance | ||||||
| Security and protection | Turnover of healthcare providers | ||||||
| Precision | |||||||
| Allows movement between services | |||||||
| Accuracy | |||||||
| Easy to generate | |||||||
| 5. | Nyamhuno, 2019 [44] | South Africa | “Assessing the acceptability of biometrics in HIV prevention programme by Hillbrow sex workers” | FSW | Biometric fingerprint | Knowledge | Fear of the unknown |
| Faith or trust | Poor relationship with officials collecting fingerprints | ||||||
| Presence of peers | Privacy concerns | ||||||
| Fear of deportation (foreigners) | |||||||
| Fear that biometrics may inhibit them from getting new jobs | |||||||
| Connection between clinic and police | |||||||
| Criminals accessing fingerprints | |||||||
| 6. | Prata et al., 2021 [47] | Togo | “A mixed-methods study to explore opportunities and challenges with using a mHealth approach to engage men who have sex with men in HIV prevention, treatment and care in Lomé, Togo” | MSM | Biometric fingerprint | Confidentiality | |
| 7. | Njoroge, 2019 [49] | Kenya | “The Last Mile: Use of Innovative Technologies to Attain the UNAIDS 90-90-90 Target” | Biometric iris scan | Not used in any government identification processes, thus eliminating the fear of being arrested | Data leakage | |
| Time | |||||||
| Religious/cultural concerns | |||||||
| Lack of understanding | |||||||
| Fear that biometric cameras will exacerbate eye problems. | |||||||
| Poor internet connection | |||||||
| System failure | |||||||
| Computer/software error | |||||||
| ID Number generation failure | |||||||
| Poor image quality | |||||||
| Eye deformity |
3.5. Feasibility and Acceptability of Implementing KPs’ UIC
3.5.1. Feasibility
3.5.2. Acceptability
| Author and Year | Country | Study Objective | Target Population | UIC Type | |
|---|---|---|---|---|---|
| 1 | Odei-Lartey et al., 2016 [25] | Ghana | “To assess the feasibility of using fingerprint identification to link community data and hospital data in a rural African setting” | General population | Biometric fingerprint |
| 2 | Wall et al., 2015 [27] | Zambia | “To detail the feasibility, including technical challenges, of implementing an electronic fingerprint linked data capture system in clinics in Zambia, and the acceptability and barriers to uptake of this system among FSWs” | FSW | Biometric fingerprint |
| 3. | Harichund et al., 2013 [29] | South Africa | “To report the development and feasibility of a digital fingerprint-based participant identification method to prevent co-enrolment at multiple clinical trial sites” | HIV-negative adult females | Biometric fingerprint |
| 4. | Jaafa et al., 2021 [31] | Kenya | “To evaluate the performance and acceptability of fingerprint technology for unique patient matching and identification in the LMIC setting of Kenya” | Clients on HIV care and treatment | Biometric fingerprint |
| 5. | Sharkey et al., 2021 [32] | Zambia | “Assess the ability of an e-fingerprinting system to enhance follow-up and detection of study outcomes, multiple enrolments, and potential spillover effect” | HIV-negative couples | Biometric fingerprint and manual fingerprint |
| 6. | Radmanovic, 2021 [36] | Uganda | “To assess the plausibility of applying novel technologies (i.e., fingerprint technology) to assess HIV healthcare (i.e., HIV testing) services among mobile fisherfolks in Uganda” | Fisherfolks | Biometric fingerprint |
| 7. | Nyamhuno, 2019 [44] | South Africa | “To investigate the acceptability of biometrics by sex workers in the Hillbrow Health Precinct programme” | FSW | Biometric fingerprint |
| 8. | White et al., 2018 [46] | Uganda | “To understand the feasibility, acceptability, and adoption of digital fingerprinting for patient identification in a household tuberculosis contact investigation study in Kampala, Uganda” | TB patient contacts | Biometric fingerprint |
| 9. | Bengtson et al., 2021 [42] | Malawi | “To evaluate the feasibility and acceptability of using biometric fingerprint scanning to accurately identify women and register HIV visits at two large urban antenatal clinics in Lilongwe, Malawi” | Pregnant women with HIV and HCWs | Biometric fingerprint |
4. Discussion
4.1. Main Findings
4.2. Required Resources for Implementing KPs’ UIC
4.3. Facilitators and Barriers for Implementing KPs’ UIC
4.4. Factors Influencing the Feasibility and Acceptability of Implementing KPs’ UIC
4.5. Strengths and Limitations of the Study
5. Conclusions
Recommendations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Joint United Nations Programme on HIV/AIDS (UNAIDS). The Path That Ends AIDS: UNAIDS Global AIDS Update 2023. 2023. Available online: https://thepath.unaids.org/wp-content/themes/unaids2023/assets/files/2023_report.pdf (accessed on 17 July 2024).
- Human Sciences Research Council (HSRC). New HIV Survey Highlights Progress and Ongoing Disparities in South Africa’s HIV Epidemic. 2023. Available online: https://hsrc.ac.za/press-releases/hsc/new-hiv-survey-highlights-progress-and-ongoing-disparities-in-south-africas-hiv-epidemic/#:~:text=SABSSM%20VI%20found%20that%20the,to%207.9%20million%20in%202017 (accessed on 9 August 2024).
- Pan American Health Organization (PAHO). Framework for Monitoring HIV/STI Services for Key Populations in Latin America and the Caribbean; PAHO: Washington, DC, USA, 2019; p. 10. [Google Scholar] [CrossRef]
- Phaswana-Mafuya, R.N.; Phalane, E.; Sisel, H.; Motsieloa, L.; Journeay, K.; Dubula, V.; Sibeko, J.; Ramothwala, P. Country ownership and sustainable programming of the HIV response in South Africa: A scoping review. S. Afr. J. HIV Med. 2023, 24, 1511. [Google Scholar] [CrossRef]
- Sandset, T. ‘Ending AIDS’ between comparison and commensuration and the role of global health indicators. Glob. Public Health 2024, 19. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Focus on Key Populations in National HIV Strategic Plans in the WHO African Region. 2018, pp. 13–30. Available online: https://www.who.int/publications/i/item/WHO-AF-CDS-HIV-02-2018 (accessed on 1 September 2024).
- Moyo, E.; Moyo, P.; Murewanhema, G.; Mhango, M.; Chitungo, I.; Dzinamarira, T. Key populations and Sub-Saharan Africa’s HIV response. Front. Public Health 2023, 11, 1079990. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.; Dorrington, R. Thembisa Version 4.7: A Model for Evaluating the Impact of HIV/AIDS in South Africa; Centre for Infectious Disease Epidemiology and Research, University of Cape Town: Cape Town, South Africa, 2024; pp. 94–96. Available online: https://www.thembisa.org/content/downloadPage/Thembisa4_7report (accessed on 17 July 2024).
- Cloete, A.; Mabaso, M.; Savva, H.; van der Merwe, L.L.; Naidoo, D.; Petersen, Z.; Kose, Z.; Mthembu, J.; Moyo, S.; Skinner, D.; et al. The HIV care continuum for sexually active transgender women in three metropolitan municipalities in South Africa: Findings from a biobehavioural survey 2018-19. Lancet HIV 2023, 10, e375–e384. [Google Scholar] [CrossRef] [PubMed]
- Scheibe, A.; Makapela, D.; Brown, B.; dos Santos, M.; Hariga, F.; Virk, H.; Bekker, L.-G.; Lyan, O.; Fee, N.; Molnar, M.; et al. HIV prevalence and risk among people who inject drugs in five South African cities. Int. J. Drug Policy 2016, 30, 107–115. [Google Scholar] [CrossRef]
- Kavanagh, M.M.; Agbla, S.C.; Joy, M.; Aneja, K.; Pillinger, M.; Case, A.; Erondu, N.A.; Erkkola, T.; Graeden, E. Law, criminalisation and HIV in the world: Have countries that criminalise achieved more or less successful pandemic response? BMJ Glob. Health 2021, 6, e006315. [Google Scholar] [CrossRef]
- Semá Baltazar, C.; Boothe, M.; Chitsondzo Langa, D.; Sathane, I.; Horth, R.; Young, P.; Schaad, N.; Raymond, H.F. Recognizing the hidden: Strengthening the HIV surveillance system among key and priority populations in Mozambique. BMC Public Health 2021, 21, 91. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Consolidated Guidelines on Person-Centred HIV Patient Monitoring and Case Surveillance; World Health Organization (WHO): Geneva, Switzerland, 2017.
- Zhao, J.; Garcia, S.A.; Ngoksin, E.; Calleja, J.M.G.; Ogbuanu, C.; Kuzmanovska, S.; Oliphant, N.; Lowrance, D.; Zorzi, N.; Hansen, P.M.; et al. Are monitoring and evaluation systems adequate to report the programmatic coverage of HIV services among key populations in countries? Infect. Dis. Poverty 2019, 8, 58. [Google Scholar] [CrossRef] [PubMed]
- Zharima, C.; Griffiths, F.; Goudge, J. Exploring the barriers and facilitators to implementing electronic health records in a middle-income country: A qualitative study from South Africa. Front. Digit. Health 2023, 5, 1207602. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- National AIDS and STIs Control Program (NASCOP). Unique Identifier Code for Key Population Programmes in Kenya; NASCOP: Nairobi, Kenya, 2015; pp. 4–5. Available online: https://policycommons.net/artifacts/1608583/unique-identifier-code-for-key-population-programmes-in-kenya/2298352/ (accessed on 17 July 2024).
- Ghana Aids Commission (GAC). National HIV & AIDS Strategic Plan 2021–2025. 2020; p. 26. Available online: https://books.google.com.au/books/about/National_HIV_AIDS_Strategic_Plan.html?id=qoPJzwEACAAJ&redir_esc=y (accessed on 15 November 2024).
- Rucinski, K.; Banda, L.M.; Olawore, O.; Akolo, C.; Zakaliya, A.; Chilongozi, D.; Schwartz, S.; Wilcher, R.; Persaud, N.; Ruberintwari, M.; et al. HIV testing approaches to optimize prevention and treatment for key and priority populations in Malawi. Open Forum Infect. Dis. 2022, 9, ofac038. [Google Scholar] [CrossRef] [PubMed]
- West African Health Organization (WAHO). ECOWAS Regional Strategy for HIV, Tuberculosis, Hepatitis B&C and Sexual and Reproductive Health and Rights among Key Populations. 2020, p. 25. Available online: https://www.undp.org/sites/g/files/zskgke326/files/migration/africa/ECOWAS-HIV-TB-Hep-SRH-strategy-23072020_EN.pdf (accessed on 20 August 2024).
- Family Health International (FHI) 360 LINKAGES. LINKAGES Liberia Quarterly Progress Report. FHI 360. 2019; p. 11. Available online: https://pdf.usaid.gov/pdf_docs/PA00X6QN.pdf (accessed on 18 July 2023).
- Jenifer, C.; Emily, H. Changing the Landscape of Data and Digital Health Solutions. 2020. Available online: https://datafi.thepalladiumgroup.com/wp-content/uploads/2020/12/Data.FI-Overview-and-COP21-Solutions-for-website-Dec-2020.pdf (accessed on 17 July 2024).
- Bore, D.; Soumaila, D.; Hamdallah, M.; Sidibe, F.M. Improving Key Population Tracking and Links to HIV Services Using Unique Identifier Codes in Mali PEPFAR. FHI 360, 2019. author profiles f. Available online: https://www.researchgate.net/publication/331233712 (accessed on 17 July 2024).
- Zan, T.; Miller, T.; Tchupo, J.P.; Ettiegne-Traore, V. Strategies and Resources for Implementing HIV Prevention, Care, and Treatment Programming with Key Populations in West Africa. Available online: https://www.fhi360.org/wp-content/uploads/drupal/documents/resource-pacte-vih-toolkit.PDF (accessed on 12 November 2024).
- Odei-Lartey, E.O.; Boateng, D.; Danso, S.; Kwarteng, A.; Abokyi, L.; Amenga-Etego, S.; Gyaase, S.; Asante, K.P.; Owusu-Agyei, S. The application of a biometric identification technique for linking community and hospital data in rural Ghana. Glob. Health Action 2016, 9, 29854. [Google Scholar] [CrossRef]
- Anne, N.; Dunbar, M.D.; Abuna, F.; Simpson, P.; Macharia, P.; Betz, B.; Cherutich, P.; Bukusi, D.; Carey, F. Feasibility and acceptability of an iris biometric system for unique patient identification in routine HIV services in Kenya. Int. J. Med. Inform. 2020, 133, 104006. [Google Scholar] [CrossRef] [PubMed]
- Wall, K.M.; Kilembe, W.; Inambao, M.; Chen, Y.N.; Mchoongo, M.; Kimaru, L.; Hammond, Y.T.; Sharkey, T.; Malama, K.; Fulton, T.R.; et al. Implementation of an electronic fingerprint-linked data collection system: A feasibility and acceptability study among Zambian female sex workers. Glob. Health 2015, 11, 27. [Google Scholar] [CrossRef]
- You, W.X.; Comins, C.A.; Jarrett, B.A.; Young, K.; Guddera, V.; Phetlhu, D.R.; Mulumba, N.; Mcingana, M.; Hausler, H.; Baral, S.; et al. Facilitators and barriers to incorporating digital technologies into HIV care among cisgender female sex workers living with HIV in South Africa. MHealth 2020, 6, 15. [Google Scholar] [CrossRef]
- Harichund, C.; Haripersad, K.; Ramjee, G. Participant verification: Prevention of co-enrolment in clinical trials in South Africa. S. Afr. Med. J. 2013, 103, 491–493. [Google Scholar] [CrossRef]
- Snidal, S.J.; Barnard, G.; Atuhairwe, E.; Ben Amor, Y. Use of eCompliance, an innovative biometric system for monitoring of tuberculosis treatment in rural Uganda. Am. J. Trop. Med. Hygiene 2015, 92, 1271. [Google Scholar] [CrossRef]
- Jaafa, N.K.; Mokaya, B.; Savai, S.M.; Yeung, A.; Siika, A.M.; Were, M. Implementation of fingerprint technology for unique patient matching and identification at an HIV care and treatment facility in western Kenya: Cross-sectional study. J. Med. Internet Research 2021, 23, e28958. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, T.; Wall, K.M.; Parker, R.; Tichacek, A.; Pappas-DeLuca, K.A.; Kilembe, W.; Inambao, M.; Malama, K.; Hoagland, A.; Peeling, R.; et al. A cluster randomized trial to reduce HIV risk from outside partnerships in Zambian HIV-Negative couples using a novel behavioral intervention, “strengthening our zows”: Study protocol and baseline data. Contemp. Clin. Trials Commun. 2021, 24, 100850. [Google Scholar] [CrossRef]
- Hortense, M.; Jean-Paul, T.; Fatoumata, T.T.; Marian, H.; Gwatiena, Y.; Clotilde, T. The Unique Identifier Code (UIC) as a System to Track Key POPULATIONS—The Experience of PACTE-VIH Project in Burkina Faso and Togo. Available online: https://pdf.usaid.gov/pdf_docs/PA00MRQX.pdf (accessed on 17 July 2024).
- Dalhatu, I.; Aniekwe, C.; Bashorun, A.; Abdulkadir, A.; Dirlikov, E.; Ohakanu, S.; Adedokun, O.; Oladipo, A.; Jahun, I.; Murie, L.; et al. From paper files to web-based application for data-driven monitoring of HIV programs: Nigeria’s journey to a national data repository for decision-making and patient care. Methods Inf. Med. 2022, 62, 130–139. [Google Scholar] [CrossRef]
- Family Health International (FHI) 360 LINKAGES. LINKAGES Malawi Quarterly Progress Report. FHI 360. 2016; pp. 1–3. Available online: https://pdf.usaid.gov/pdf_docs/PA00MMF9.pdf (accessed on 18 July 2023).
- Radmanovic, J. Biometric Fingerprint Technology for Estimating Frequent HIV Testing and HIV Incidence among Mobile Men and Women in Fishing Communities along Lake Victoria Uganda. Master’s Thesis, University of Gothenburg, Göteborg, Sweden, 2022. Available online: https://gupea.ub.gu.se/handle/2077/72716 (accessed on 29 September 2024).
- Assefa, Y.; Gilks, C.F. Ending the epidemic of HIV/AIDS by 2030: Will there be an endgame to HIV, or an endemic HIV requiring an integrated health systems response in many countries? Int. J. Infect. Dis. 2020, 100, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Annang, D.; Ayamah, P.; Amoako, A.S.A. Counting That Counts: The Success Story of the Ghana Key Population Unique Identification System (GKPUIS). 2022, p. 1. Available online: https://programme.aids2022.org/Abstract/Abstract/?abstractid=6695 (accessed on 5 June 2024).
- Kamanga, J.; Stankevitz, K.; Martinez, A.; Chiegil, R.; Nyirenda, L.; Mulenga, F.; Chen, M.; Mpofu, M.; Lubasi, S.; Bateganya, M. Improved HIV case finding among key populations after differentiated data driven community testing approaches in Zambia. PLoS ONE 2021, 16, e0258573. [Google Scholar] [CrossRef]
- Family Health International (FHI) 360. Unique Identifier Codes Create Continuity and Improve Client Tracking for LINKAGES Mali: Success Story. 2019, pp. 1–3. Available online: https://www.fhi360.org/wp-content/uploads/drupal/documents/linkages-success-story-mali-september-19.pdf (accessed on 5 May 2024).
- Harkaway, N. Unique Identifier Code for KP: Anonimity, Precicion and Mobility. FHI 360. 2017, pp. 1–11. Available online: https://www.fhi360.org/wp-content/uploads/drupal/documents/resource-pacte-vih-identifier-code.pdf (accessed on 17 July 2024).
- Bengtson, A.M.; Kumwenda, W.; Lurie, M.; Klyn, B.; Owino, M.; Miller, W.C.; Go, V.; Hosseinipour, M.C. Improving monitoring of engagement in HIV care for women in option B+: A pilot test of biometric fingerprint scanning in Lilongwe, Malawi. AIDS Behav. 2020, 24, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Haeri Mazanderani, A.; Sherman, G.G.; Moyo, F.; Goga, A.E.; Feucht, U. Leveraging the road to health booklet as a unique patient identifier to monitor the prevention of mother-to-child transmission programme. South Afr. Med. J. 2018, 108, 729–733. [Google Scholar] [CrossRef] [PubMed]
- Nyamhuno, S. Assessing the Acceptability of Biometrics in HIV Prevention Program by Hillbrow Sex Workers. Master’s Thesis, University of the Witwatersrand, Johannesburg, South Africa, 2019. Available online: https://wiredspace.wits.ac.za/server/api/core/bitstreams/a29f08ee-cf7a-4874-9fc3-3a8e2e7d6023/content (accessed on 11 April 2024).
- The Global Fund. Global Fund Grants in South Africa: Audit Report. 2022, pp. 1–9. Available online: https://www.theglobalfund.org/media/11824/oig_gf-oig-22-004_report_en.pdf (accessed on 17 July 2024).
- White, E.B.; Meyer, A.J.; Ggita, J.M.; Babirye, D.; Mark, D.; Ayakaka, I.; Haberer, J.E.; Katamba, A.; Armstrong-Hough, M.; Davis, J.L. Feasibility, acceptability, and adoption of digital fingerprinting during contact investigation for tuberculosis in Kampala, Uganda: A parallel-convergent mixed-methods analysis. J. Med. Internet Res. 2018, 20, e11541. [Google Scholar] [CrossRef]
- Prata, N.; Weidert, K.; Soro, D.R. A mixed-methods study to explore opportunities and challenges with using a mHealth approach to engage men who have sex with men in HIV prevention, treatment and care in Lomé, Togo. MHealth 2021, 7, 47. [Google Scholar] [CrossRef]
- Zan, T.; Miller, M.; Tchupo, J.P.; Virginie, E.T. PACTE-VIH Replication Toolkit: Strategies and Resources for Implementing HIV Prevention, Care, and Treatment Programming with Key Populations in West Africa. 2016, pp. 12–23. Available online: https://www.fhi360.org/sites/default/files/media/documents/resource-pacte-vih-toolkit.PDF (accessed on 16 December 2024).
- Njoroge Anne, W. The Last Mile: Use of Innovative Technologies to Attain the UNAIDS 90-90-90 Target. Washington. 2019. Available online: https://digital.lib.washington.edu/researchworks/handle/1773/45071 (accessed on 17 July 2024).
- Park, S.Y.; Nicksic Sigmon, C.; Boeldt, D. A Framework for the implementation of digital mental health interventions: The importance of feasibility and acceptability research. Cureus 2022, 14, e29329. [Google Scholar] [CrossRef]
- Hugo, T.; Van Ewijk, S. Acceptability and Feasibility of Biometric Identification Systems in the Delivery of Health Services to Key Populations: A Narrative Review. Available online: https://www.semanticscholar.org/paper/Acceptability-and-Feasibility-of-Biometric-Systems-Ewijk/b27e159f94de88b89af1cee5f7ce86d721f8a30a (accessed on 1 February 2024).
- PAHO. Why Data Disaggregation Is Key during a Pandemic: Digital Transformation Toolkit. OECD. 2020. Available online: https://iris.paho.org/bitstream/handle/10665.2/52002/Data-Disaggregation-Factsheet-eng.pdf?sequence=19&isAllowed=y (accessed on 1 February 2024).
- Global Summary of Findings of an Assessment of HIV Services Packages for Key Populations in Six Regions. Available online: https://www.aidsdatahub.org/resource/global-summary-findings-assessment-hiv-services-packages-key-populations-six-regions (accessed on 12 April 2024).
- Lyons, C.E.; Rwema, J.O.T.; Makofane, K.; Diouf, D.; Njindam, I.M.; Ba, I.; Kouame, A.; Tamoufe, U.; Cham, B.; Djaló, M.A.; et al. Associations between punitive policies and legal barriers to consensual same-sex sexual acts and HIV among gay men and other men who have sex with men in sub-Saharan Africa: A multicountry, respondent-driven sampling survey. Lancet HIV 2023, 10, e186–e194. [Google Scholar] [CrossRef]
- Harm Reduction International. The Global STATE of harm Reduction, 7th Edition. 2022. Available online: https://idpc.net/publications/2020/10/the-global-state-of-harm-reduction-2020 (accessed on 25 April 2025).
- Platt, L.; Grenfell, P.; Meiksin, R.; Elmes, J.; Sherman, S.G.; Sanders, T.; Mwangi, P.; Crago, A.L. Associations between sex work laws and sex workers’ health: A systematic review and meta-analysis of quantitative and qualitative studies. PLoS Med. 2018, 15, e1002680. [Google Scholar] [CrossRef]
- Govender, K.; Long, L.; Miot, J. Progress towards Unique Patient Identification and Case-Based Surveillance within the Southern African Development Community (SADC). Health Inform. J. 2020, 29, 14604582221139058. [Google Scholar] [CrossRef]
- Mills, S.; Lee, J.K.; Rassekh, B.M.; Zorko Kodelja, M.; Bae, G.; Kang, M.; Pannarunothai, S.; Kijsanayotin, B. Unique health identifiers for universal health coverage. J Health Popul. Nutr. 2019, 38 (Suppl. S1), 22. [Google Scholar] [CrossRef] [PubMed]
- Katurura, M.C.; Cilliers, L. Electronic health record system in the public health care sector of South Africa: A systematic literature review. Afr. J. Prim. Health Care Fam Med. 2018, 10, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Abrams, M.P.; Torres, F.E.; Little, S.J. Biometric registration to an HIV research study may deter participation. AIDS Behav. 2021, 25, 1552–1559. [Google Scholar] [CrossRef] [PubMed]
- Identity Theft Center (ITRC). The 2021 Data Breach Annual Report. 2022, p. 3. Available online: https://www.idtheftcenter.org/post/identity-theft-resource-center-2021-annual-data-breach-report-sets-new-record-for-number-of-compromises/ (accessed on 12 February 2024).
- Burgess, M. London HIV Clinic Fined £180,000 for “Serious” Data Breach. Available online: https://www.theguardian.com/technology/2016/may/09/london-hiv-clinic-fined-180000-for-revealing-service-users-names (accessed on 1 February 2024).
- Yong, G.K. Statement by Minister (Health) Mr. Gan Kim Yong on the Unauthorized Possession and Disclosure of from HIV registry. 2019. Available online: https://www.moh.gov.sg/news-highlights/details/statement-by-minister-(health)-mr-gan-kim-yong-on-the-unauthorised-possession-and-disclosure-of-information-from-hiv-registry (accessed on 1 February 2024).
- Hudson, A. HIV Scotland Fined £10,000 for Email Data Breach. Available online: https://www.bbc.com/news/uk-scotland-59008366 (accessed on 1 February 2024).
- Davis, S.; Maleche, A. “Everyone Said No” Biometrics, HIV and Human Rights, Kenya Case Study. 2018. Available online: https://www.hhrjournal.org/2018/07/everyone-said-no-key-populations-and-biometrics-in-kenya/ (accessed on 5 February 2024).
- SANAC. National Strategic Plan for HIV, TB and STI 2023-2028. Available online: https://sanac.org.za/national-strategic-plan-2023-2028/ (accessed on 17 July 2024).
- Health Communication Capacity Collaborative (HCCC). Integrated Social and Behavior Communication Programs Kit. 2014. Available online: https://sbccimplementationkits.org/integrated-sbcc-programs/wp-content/uploads/sites/11/2017/06/Integrated-SBCC-Programs-I-Kit_Online-Print-080917-FINAL.pdf (accessed on 18 July 2024).
- AFAO. Mongolia SKPA-2 Baseline Assessment Report. 2023. Available online: https://assets.healthequitymatters.org.au/wp-content/uploads/2023/06/16053225/SKPA-2-Baseline-Report_Overarching_FINALv2.pdf (accessed on 17 July 2024).
- WHO. Burundi Adopts Community-Based Approach to Prevent Mother-to-Child Transmission of HIV. 2024. Available online: https://www.afro.who.int/countries/burundi/news/burundi-adopts-community-based-approach-prevent-mother-child-transmission-hiv (accessed on 5 May 2025).
- Malawi COP. Malawi Country Operational Plan COP 2023 Strategic Direction Summary. 2024. Available online: https://www.prepwatch.org/wp-content/uploads/2024/06/Malawi-Strategic-Direction-Summary-2023.pdf (accessed on 17 July 2024).
- UNAIDS. The Urgency of Now: AIDS at a Crossroads. Geneva: Geneva: Joint United Nations Programme on HI. 2024, p. 50. Available online: https://crossroads.unaids.org/wp-content/uploads/2024/09/GAU-2024-Full-report_En.pdf (accessed on 17 July 2024).
- United Nations. UN Liberia Annual Results Report. 2024, p. 27. Available online: https://www.who.int/about/accountability/results/who-results-report-2024-2025/country-profile/2024/liberia (accessed on 19 July 2024).
| Authors, Year | Country | Title | Key Populations | UIC Type | Level Where UIC Was Incorporated on RHIMS | |
|---|---|---|---|---|---|---|
| 1. | National AIDS and STI Commission Programme (NASCOP), 2015 [17] | Kenya | “Unique identifier code for Key population programmes in Kenya” | FSW/MSM/TG/PWUD/PWID | Alphanumeric code | National |
| 2. | Ghana Aids Commission (GAC), 2020 [18] | Ghana | “National HIV & AIDS strategic plan 2021–2025” | FSW and MSM | Alphanumeric code | National |
| 3. | Rucinski et al., 2022 [19] | Malawi | “HIV testing approaches to optimize prevention and treatment for Key and priority populations in Malawi” | FSW, MSM, TGW, and MSW | Alphanumeric code | Sub-national |
| 4. | West African Health Organization (WAHO), 2020 [20] | Togo | “ECOWAS regional strategy for HIV, tuberculosis, hepatitis B & C and sexual and reproductive health and rights among key populations”. | FSW, MSM, TGW, and MSW | Alphanumeric code | National |
| 5. | Family Health International (FHI) 360, 2019 [21] | Liberia | “LINKAGES Liberia quarterly progress report 1 July–30 September 2019” | MSM, FSW and TG | Alphanumeric code | National |
| 6. | Chapman et al., 2020 [22] | Uganda and Burundi | “Changing the landscape of data and digital health solutions” | FSW, TG, PWID, MSM, and people in prisons and closed settings | Alphanumeric code and Biometric fingerprint | Sub-national |
| 7. | Bore et al., 2017 [23] | Mali | “Improving key population tracking and links to HIV Services using unique identifier codes in Mali” | FWS, partners of FSW, and MSM | Alphanumeric code | Sub-national |
| 8. | Zan et al., 2016 [24] | Burkina Faso and Togo | “Strategies and resources for implementing HIV prevention, care, and treatment programming with key populations in West Africa” | FSW and MSM | Alphanumeric code | Sub-national |
| Country Name | UIC Creation Method |
|---|---|
| Kenya | County code (2-digit) + Sub-County code (3-digit) + Ward code (3-digit) + Implementing partner code (3-digit) + Hotspot code (3-digit) + KP type (e.g., 01) + first 2 letters of first name + first 2 letters of middle name + first 2 letters of last name + month of birth (2-digit) + 4-digit serial number |
| Ghana | KP type + first 2 letters of first name + first 2 letters of middle name + first 2 letters of surname + month of birth (2-digit) |
| Malawi | Country code + Initials of health facility name + last 2 digits of year of enrolment + population type code (e.g., 00, 01, 02, 03) |
| Liberia | County code (2-digit) + Health facility name initials + last 2 digits of year of enrolment + 4-digit serial number + population type code (e.g., 00, 01, 02, 03) |
| Mali | First letter of KP type + last 2 digits of birth year + first 2 letters of client’s last name + first 2 letters of mother’s last name + first 3 letters of country of origin + first 2 letters of birth town |
| Burkina Faso | Gender + last 2 digits of birth year + first letter of last name + first letter of first name + first 2 letters of mother’s first name |
| Togo | Not fully specified; national alphanumeric UIC used across stakeholders at national level |
| Uganda | Not fully specified; alphanumeric code + biometric fingerprint |
| Burundi | Not fully specified; alphanumeric code + biometric fingerprint |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rampilo, M.; Phalane, E.; Phaswana-Mafuya, R.N. Tracking HIV Outcomes Among Key Populations in the Routine Health Information Management System: A Systematic Review. Sexes 2025, 6, 32. https://doi.org/10.3390/sexes6030032
Rampilo M, Phalane E, Phaswana-Mafuya RN. Tracking HIV Outcomes Among Key Populations in the Routine Health Information Management System: A Systematic Review. Sexes. 2025; 6(3):32. https://doi.org/10.3390/sexes6030032
Chicago/Turabian StyleRampilo, Mashudu, Edith Phalane, and Refilwe Nancy Phaswana-Mafuya. 2025. "Tracking HIV Outcomes Among Key Populations in the Routine Health Information Management System: A Systematic Review" Sexes 6, no. 3: 32. https://doi.org/10.3390/sexes6030032
APA StyleRampilo, M., Phalane, E., & Phaswana-Mafuya, R. N. (2025). Tracking HIV Outcomes Among Key Populations in the Routine Health Information Management System: A Systematic Review. Sexes, 6(3), 32. https://doi.org/10.3390/sexes6030032







