De La Chapelle Syndrome: Clinical and Physical Performance Implications
Abstract
1. Introduction
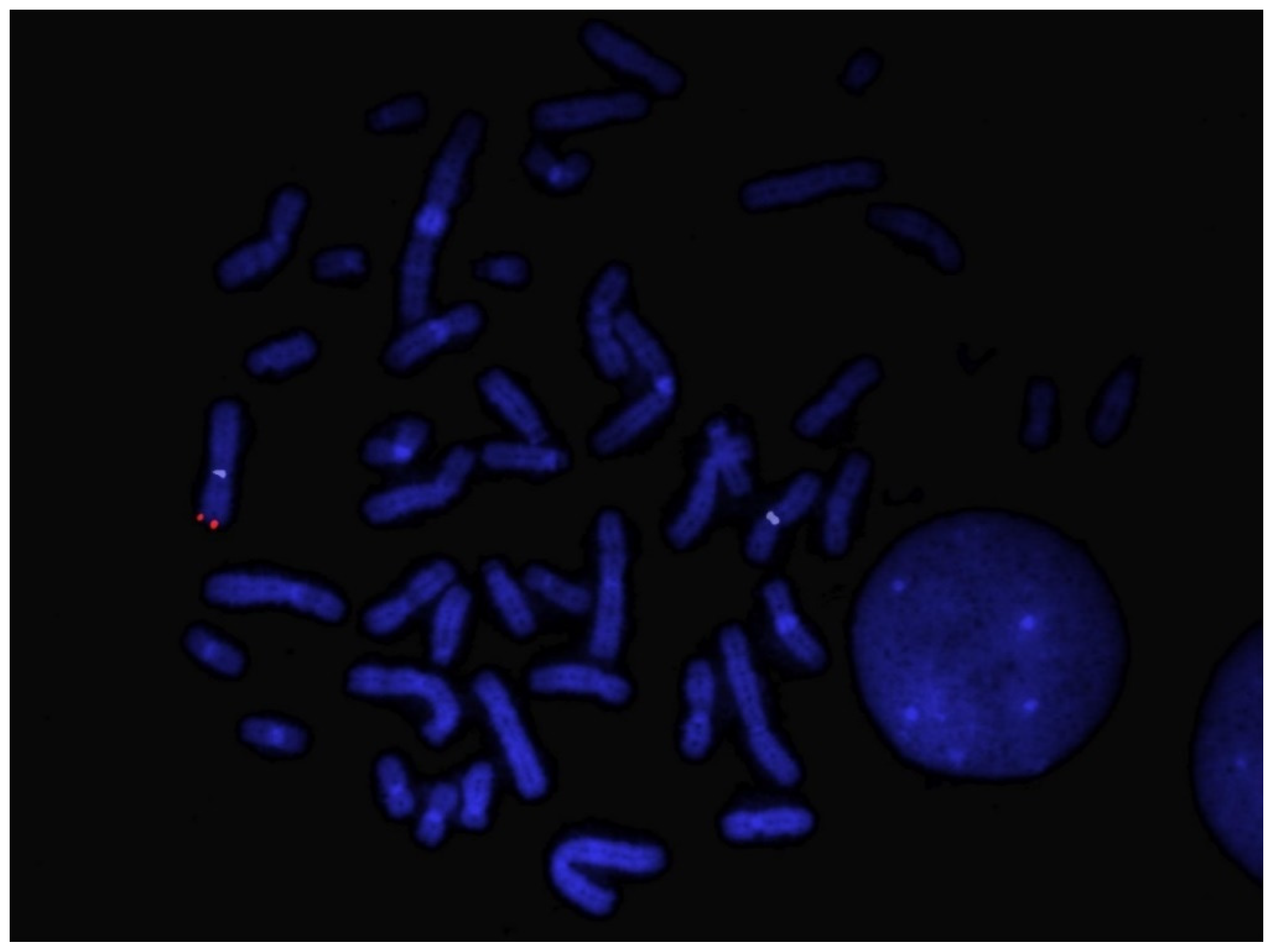
2. Patient and Methods
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cemaine, V.; Cayci, C.; Simmons, P.S.; Petty, P. Gynecomastia in Adolescent Males. Semin. Plast. Surg. 2013, 27, 56–61. [Google Scholar]
- Limony, Y.; Friger, M.; Hochberg, Z. Pubertal gynecomastia coincides with peak height velocity. J. Clin. Res. Pediatr. Endocrinol. 2013, 5, 142–144. [Google Scholar] [PubMed]
- Kanakis, G.A.; Nordkap, L.; Bang, A.K.; Calogero, A.E.; Bártfai, G.; Corona, G.; Forti, G.; Toppari, J.; Goulis, D.G.; Jørgensen, N. EAA clinical practice guidelines-gynecomastia evaluation and management. Andrology 2019, 7, 778–793. [Google Scholar] [CrossRef] [PubMed]
- Sansone, A.; Romanelli, F.; Sansone, M.; Lenzi, A.; Di Luigi, L. Gynecomastia and hormones. Endocrine 2017, 55, 37–44. [Google Scholar] [CrossRef]
- Sobel, V.; Imperato-McGinley, J. Hypergonadotropic Hypergonadism. Encyclopedia of Endocrine Diseases; Elsevier: Amsterdam, The Netherlands, 2004; Volume 2. [Google Scholar]
- De la Chapelle, A. The etiology of maleness in XX men. Hum. Genet. 1981, 58, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Massy-Westropp, N.M.; Gill, T.K.; Taylor, A.W.; Bohannon, R.W.; Hill, C.L. Hand Grip Strength: Age and gender stratified normative data in a population-based study. BMC Res. Notes. 2011, 4, 127. [Google Scholar] [CrossRef] [PubMed]
- McKay, M.J.; Baldwin, J.N.; Ferreira, P.; Simic, M.; Vanicek, N.; Burns, J. 1000 Norms Project Consortium. Reference values for developing responsive functional outcome measures across the lifespan. Neurology 2017, 88, 1512–1519. [Google Scholar] [CrossRef]
- Grinspon, R.P.; Rey, R.A. Molecular Characterization of XX Maleness. Int. J. Mol. Sci. 2019, 20, 6089. [Google Scholar] [CrossRef]
- Cools, M.; Nordenström, A.; Robeva, R.; Hall, J.; Westerveld, P.; Flück, C.; Köhler, B.; Berra, M.; Springer, A.; Schweizer, K.; et al. COST Action BM1303 working group 1. Caring for individuals with a difference of sex development (DSD): A Consensus Statement. Nat. Rev. Endocrinol. 2018, 14, 415–429. [Google Scholar] [CrossRef]
- Vorona, E.; Zitzmann, M.; Gromoll, J.; Schüring, A.N.; Nieschlag, E. Clinical, endocrinological, and epigenetic features of the 46,XX male syndrome, compared with 47,XXY Klinefelter patients. J. Clin. Endocrinol. Metab. 2007, 92, 3458–3465. [Google Scholar] [CrossRef]
- Huang, W.J.; Yen, P.H. Genetics of spermatogenic failure. Sex. Dev. 2008, 2, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Bouayed Abdelmoula, N.; Portnoi, M.F.; Keskes, L.; Recan, D.; Bahloul, A.; Boudawara, T.; Saad, A.; Rebai, T. Skewed X-chromosome inactivation pattern in SRY positive XX maleness: A case report and review of literature. Ann. Genet. 2003, 46, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Lindhardt Johansen, M.; Hagen, C.P.; Johannsen, T.H.; Main, K.M.; Picard, J.Y.; Jørgensen, A.; Rajpert-De Meyts, E.; Juul, A. Anti-müllerian hormone and its clinical use in pediatrics with special emphasis on disorders of sex development. Int. J. Endocrinol. 2013, 2013, 198698. [Google Scholar] [CrossRef] [PubMed]
- Josso, N.; Rey, R.A. What Does AMH Tell Us In Pediatric Disorders of Sex Development? Front. Endocrinol. 2020, 11, 619. [Google Scholar] [CrossRef] [PubMed]
- Narula, H.S.; Carlson, H.E. Gynaecomastia--pathophysiology, diagnosis and treatment. Nat. Rev. Endocrinol. 2014, 10, 684–698. [Google Scholar] [CrossRef] [PubMed]
- Di Luigi, L.; Greco, E.A.; Fossati, C.; Aversa, A.; Sgrò, P.; Antinozzi, C. Clinical Concerns on Sex Steroids Variability in Cisgender and Transgender Women Athletes. Int. J. Sports Med. 2023, 44, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Osaka, A.; Ide, H.; Matsuoka, K.; Iwahata, T.; Kobori, Y.; Ban, S.; Okada, H.; Saito, K. SRY-Positive 46, XX Testicular Disorder of Sexual Development with Leydig Cell Tumor. Am. J. Mens. Health 2020, 14, 1557988320970071. [Google Scholar] [CrossRef]
- Pleskacova, J.; Hersmus, R.; Oosterhuis, J.W.; Setyawati, B.A.; Faradz, S.M.; Cools, M.; Wolffenbuttel, K.P.; Lebl, J.; Drop, S.L.; Looijenga, L.H. Tumor risk in disorders of sex development. Sex. Dev. 2010, 4, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Kathrins, M.; Kolon, T.F. Malignancy in disorders of sex development. Transl. Androl. Urol. 2016, 5, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Mameli, C.; Selvaggio, G.; Cerini, C.; Bulfamante, G.; Madia, C.; Riccipetitoni, G.; Zuccotti, G.V. Atypical Leydig Cell Tumor in Children: Report of 2 Cases. Pediatrics 2016, 138, e20160151. [Google Scholar] [CrossRef]
- Slowikowska-Hilczer, J.; Szarras-Czapnik, M.; Duranteau, L.; Rapp, M.; Walczak-Jedrzejowska, R.; Marchlewska, K.; Oszukowska, E.; Nordenstrom, A.; dsd-LIFE group. Risk of gonadal neoplasia in patients with disorders/differences of sex development. Cancer Epidemiol. 2020, 69, 101800. [Google Scholar] [CrossRef] [PubMed]
- Rapp, M.; Mueller-Godeffroy, E.; Lee, P.; Roehle, R.; Kreukels, B.P.C.; Köhler, B.; Nordenström, A.; Bouvattier, C.; Thyen, U.; dsd-LIFE group. Multicentre cross-sectional clinical evaluation study about quality of life in adults with disorders/differences of sex development (DSD) compared to country specific reference populations (dsd-LIFE). Health Qual. Life Outcomes 2018, 16, 54. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, M.; Nieschlag, E. Effects of androgen replacement on metabolism and physical performances in male hypogonadism. J. Endocrinol. Investig. 2003, 26, 886–892. [Google Scholar] [CrossRef] [PubMed]
- La Vignera, S.; Izzo, G.; Emerenziani, G.P.; Cannarella, R.; Condorelli, R.A.; Calogero, A.E.; Aversa, A. Male hypogonadism: Therapeutic choices and pharmacological management. Minerva Endocrinol. 2020, 45, 189–203. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiarello, P.; Seminara, G.; Bossio, S.; Sicilia, L.; Greco, F.; Malatesta, P.; Greco, E.A.; Aversa, A. De La Chapelle Syndrome: Clinical and Physical Performance Implications. Sexes 2024, 5, 198-203. https://doi.org/10.3390/sexes5030015
Chiarello P, Seminara G, Bossio S, Sicilia L, Greco F, Malatesta P, Greco EA, Aversa A. De La Chapelle Syndrome: Clinical and Physical Performance Implications. Sexes. 2024; 5(3):198-203. https://doi.org/10.3390/sexes5030015
Chicago/Turabian StyleChiarello, Paola, Giuseppe Seminara, Sabrina Bossio, Luciana Sicilia, Francesca Greco, Paola Malatesta, Emanuela Alessandra Greco, and Antonio Aversa. 2024. "De La Chapelle Syndrome: Clinical and Physical Performance Implications" Sexes 5, no. 3: 198-203. https://doi.org/10.3390/sexes5030015
APA StyleChiarello, P., Seminara, G., Bossio, S., Sicilia, L., Greco, F., Malatesta, P., Greco, E. A., & Aversa, A. (2024). De La Chapelle Syndrome: Clinical and Physical Performance Implications. Sexes, 5(3), 198-203. https://doi.org/10.3390/sexes5030015







