Factors Influencing Sexual Health Service Use by South Asian Immigrant Men Living in Ontario, Canada: A Qualitative Study
Abstract
1. Introduction
2. Methods
2.1. Study Context and Participant Selection
2.2. Data Collection and Analysis
3. Results
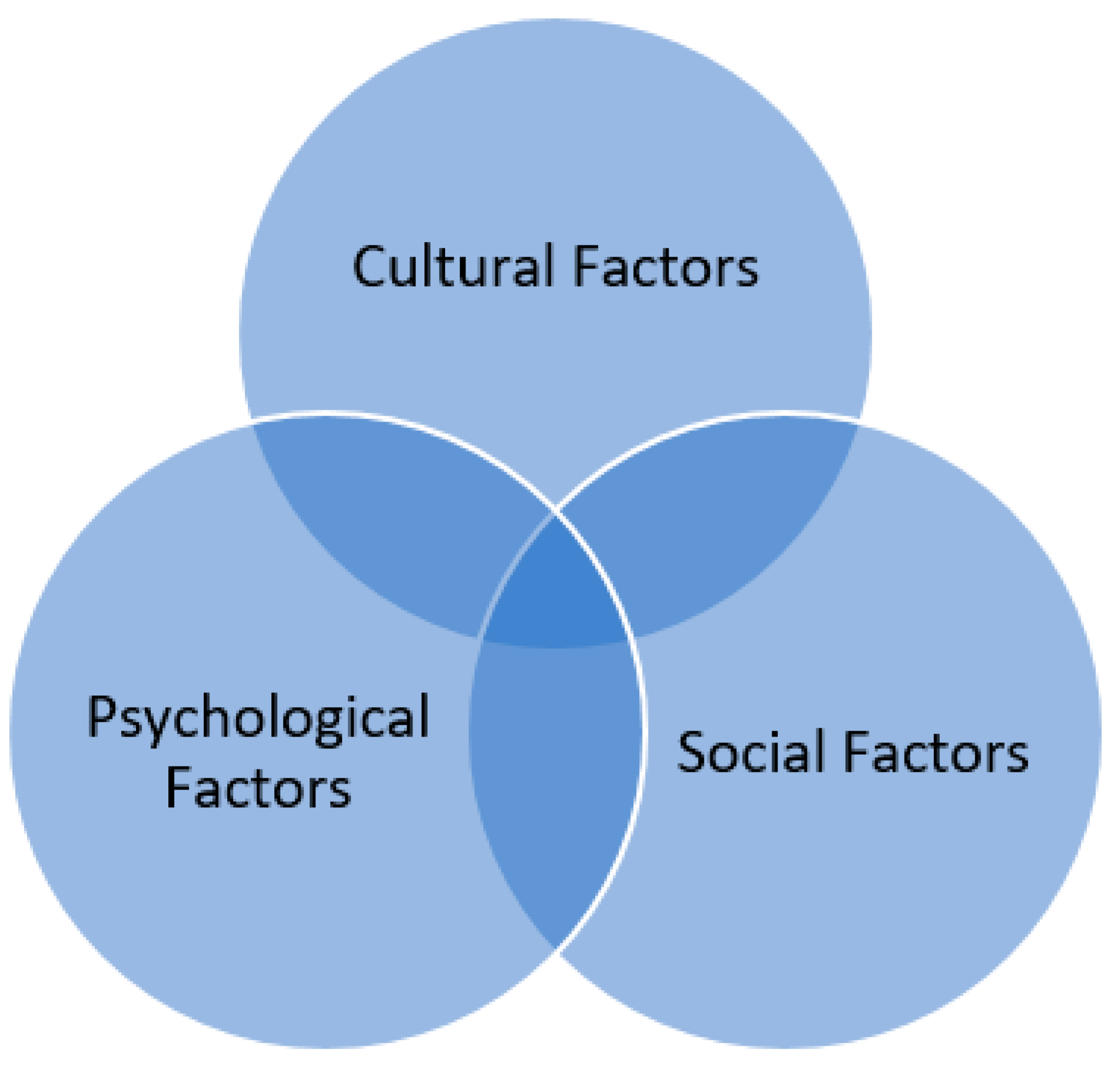
3.1. Cultural Factors
3.1.1. Culture Influences Perceptions about Sexual Health
“Yes! I would say so [culture does influence sexual health use], because the culture like within different states or a different part of the country, I could experience that, some people follow their culture strictly, because of the way they were brought up, so your culture has a particular influence on you, and also it shapes your overall understanding about health in general and also about using sexual health information and using these services.”—(Anand, an immigrant from India)
3.1.2. Prescriptive Gender Stereotypes about South Asian Men
“I think men and women from South Asian origin would be reluctant to use [sexual] health clinics or feel uncomfortable or insecure [in using services]. [The reason being] the set cultural views and opinions you may have. Like, you may go to a clinic, and you might see somebody or, you know, the clinic is located [nearby], and you feel uncomfortable going there because somebody from your community might also see you there. So, you know, it’s quite common that people talk about people, and, if someone sees you, then they can tell your family or others about your visit [to the sexual health clinic]. There are some prescriptive gender stereotypes about sexual health in our society. People [men] will be stereotyped as not worthy [as a man in the society]. Yeah, culture can play a big part in not letting people use these [sexual health] services.”—(Sriram, an immigrant from India)
3.2. Psychological Factors
3.2.1. Perceived Severity of Illness
“Yes, [the choice of using sexual health services] depends on the severity of the [sexual] illness as well and the level of my tolerance. If this [the sexual complication/illness] is something that gets cured easily like with medication and stuff, then I think I wouldn’t bother to use services […].”—(Zaiyan, an immigrant from Bangladesh)
“I mean, if you ask me, ‘oh, do you know, this [sexual health services] does exist? I would say probably, but I wouldn’t tell you […] I don’t think…I would probably not inquire. I probably not go for it [sexual health service]. I see it [sexual health check-ups] not to be so important, and just go for it when I need to, yeah. But, yeah, so, I guess I would probably seek help if something [sexual health complications/illness] happened.”—(Hossain, an immigrant from Pakistan)
3.2.2. Attitude towards Sexual Health
“Generally, you don’t need them [sexual health services]. So it can be important. But it’s largely a personal thing where you choose to go, and it [availing services] can be considered as an optional choice for a check-up. And I guess going to the doctor for the right reasons it’s more of a tool, I would say. And they can be used, or you don’t need it all the time.”—(Ikram, an immigrant from Bangladesh)
3.2.3. Sexual Health Considered Negatively by Some South Asian Men
“Oh, boy, I mean, my family, my parents, they never taught me anything [about sexual health]. You know, my dad was a strong, silent type. But I have found on many occasions that some of the [sexual health] things you know what it is [meaning sexual illness/complications], to discuss about them is kind of prohibited as some see these things negatively, you know, people look at it as something that’s kind of a bad thing. Or even learning about it is seen as a bad thing to do.”—(Hossain, an immigrant from Pakistan)
“But I think society takes the wrong ideas and like makes these implications [about sexual health] and there remains limited access to information in South Asian communities, like from childhood or school days. And it’s been a tradition, and it has been passed down from like generations. And I think part of it is cultural and the other part could be how people take sexual health negatively [the mentality].”—(Ezaan, an immigrant from Bangladesh)
3.3. Social Factors
3.3.1. Sexual Health as Taboo
“Well, really, in my house, usually this [sexual health] was a really taboo subject, so no one really spoke about it [sexual health], and we didn’t have any sort of like sexual health or sex ed at school. But so, when I was coming of age, like during puberty, my dad kind of told me how to, like, get through that stage. But I wouldn’t really call it like, being made aware of sexual health. It was more of being made aware of what I might be going through [as a teenager] like during that time. Yeah, I definitely think there’s this sort of stigma or taboo associated with it [sexual health], or there is the religion that is tied to it [in not discussing sexual health] as well in the South Asian communities, like, oh, it’s something you shouldn’t talk about within the family and it is prohibited.”—(Mizaan, an immigrant from Bangladesh)
3.3.2. Issues Related to Sex Positivity and Sex Negativity
“I think being sex positive is really important, as it helps you to be educated and become proactive to get like sexual health check-ups regularly because like, you never know when you might be infected with some type of disease or even if it’s not a disease, it’s some…like some sort of like dysfunction. Like because if you do not have proper [sex] education, you don’t have the mindset and maybe never went for a check-up, so you wouldn’t know what’s wrong with you unless, like, sometimes it [illness] might even be hidden and you wouldn’t know until you’re like in a situation where you find it out, and it’s like, it’s affecting you.”—(Ezaan, an immigrant from Bangladesh)
“The culture we grew up in is more directed towards academics, so, for some South Asian men, they would be very sex negative and would be like, ‘hey, you should be focused more on studies. This [sexual health education] is stuff you should not be getting into because we know what the…what this stuff can get you to end’, that you’ll be stuck there [thinking about sexual health] because that’s a lot of people who grew up, they, when they’re exposed to these things [sexual health education] and when they get a lot of knowledge about it, they get stuck there. And like that’s the belief that we had. Like, ‘hey, they got stuck there.’ But these South Asian men think people should focus more on other stuff, like improving life skills, etc., and not on sexual health.”—(Rohan, an immigrant from India)
3.3.3. Sexual Health Discussion with Trusted Sources and Following the Western Lifestyle Approach
“It [sexual health discussion] went relatively well, especially like it depends also on the type of friendship that we have and also if I can confide in a particular family member to talk to. And so, I think based on the type of friendship that I had with my friends, or family bonding like that was the main factor that led to a very open conversation [about sexual health]. But like, if I were to discuss this just about like someone who I just met or like who I’ve been talking to for a few days, and it wouldn’t go so well. So that’s kind of the environment that you were in. Also, similar age range matters in an open discussion.”—(Rashed, an immigrant from Bangladesh)
“Like for someone who is purely Canadian or Canadianized [following a lifestyle that participants understand as relate to being open-minded in Canada], they’re going to think in the Western-lifestyle way, and they’re gonna assume that everyone or they would want their significant other to have that mindset and discuss sexual health more openly.”—(Ahmed, an immigrant from Pakistan)
“In my family, we are quite ‘Canadianized’ [following a lifestyle that participants understand as related to being open-minded in Canada] and can talk about it [sexual health]. We do not have any issues within our family as we can share openly. You know we are more Canadian than South Asian in our culture, and we are less conservative.”—(Zaiyan, an immigrant from Bangladesh)
4. Discussion
5. Implications
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hamadeh, N.; Van Rompaey, C.; Metreau, E. New World Bank Country Classifications by Income Level: 2021–2022. Available online: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2021-2022 (accessed on 26 December 2021).
- United Nations Population Fund. Migration. United Nations Popul Fund 2015. Available online: http://www.unfpa.org/migration (accessed on 14 December 2021).
- Statistics Canada. Immigration and Ethnocultural Diversity Statistics. Available online: https://www.statcan.gc.ca/en/subjects-start/immigration_and_ethnocultural_diversity (accessed on 22 December 2021).
- Islam, F.; Khanlou, N.; Tamim, H. South Asian populations in Canada: Migration and mental health. BMC Psychiatry 2014, 14, 154. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Canada Year Book 2011; Statistics Canada: Ottawa, ON, Canada, 2011.
- Degni, F.; Suominen, S.; Essén, B.; El Ansari, W.; Vehviläinen-Julkunen, K. Communication and cultural issues in providing reproductive health care to immigrant women: Health care providers’ experiences in meeting Somali women living in Finland. J. Immigr. Minor. Health 2012, 14, 330–343. [Google Scholar] [CrossRef] [PubMed]
- Doll, L.S.; Beeker, C. Male bisexual behavior and HIV risk in the United States: Synthesis of research with implications for behavioral interventions. AIDS Educ. Prev. 1996, 8, 205–225. [Google Scholar] [PubMed]
- Hahm, H.C.; Song, I.H.; Ozonoff, A.; Sassani, J.C. HIV Testing Among Sexually Experienced Asian and Pacific Islander Young Women: Association With Routine Gynecologic Care. Women’s Health Issues 2009, 19, 279–288. [Google Scholar] [CrossRef][Green Version]
- Salehi, R.; Hynie, M.; Flicker, S. Factors associated with access to sexual health services among teens in Toronto: Does immigration matter? J. Immigr. Minor. Health 2014, 16, 638–645. [Google Scholar] [CrossRef]
- Ottawa Public Health. Sexually Transmitted Infections and Sexual Health in Ottawa 2011. Ott. Public Health 2011, 1–48. Available online: https://www.ottawapublichealth.ca/en/reports-research-and-statistics/resources/Documents/sexually_transmitted_infections_2011_en.pdf (accessed on 28 December 2021).
- Smith, A.L. Health Policy and the Coloring of an American Male Crisis: A Perspective on Community-Based Health Services. Am. J. Public Health 2003, 93, 749–752. [Google Scholar] [CrossRef]
- Jayaraman, G.; Totten, S.; Perrin, M.; Fang, L.; Remes, O. Report on Sexually Transmitted Infections in Canada: 2008. 2008. Available online: https://www.phac-aspc.gc.ca/std-mts/report/sti-its2008/PDF/10-047-STI_report_eng-r1.pdf (accessed on 26 December 2021).
- Manderson, L.; Allotey, P. Storytelling, Marginality, and Community in Australia: How Immigrants Position Their Difference in Health Care Settings. Med. Anthropol. Cross Cult. Stud. Health Illn. 2003, 22, 1–21. [Google Scholar] [CrossRef]
- Hancock, J. Can mainstream services learn from male only sexual health pilot projects? Sex Transm. Infect. 2004, 80, 484–487. [Google Scholar] [CrossRef][Green Version]
- Government of Ontario: Sexual Health Clinics-How to Get Free Sexual Health Testing, Counselling and Treatment Services. Available online: https://www.ontario.ca/page/sexual-health-clinics#section-0 (accessed on 16 December 2021).
- Government of Canada. Sexual Health and Promotion. Available online: https://www.canada.ca/en/health-canada/services/healthy-living/sexual-health-promotion.html (accessed on 15 January 2022).
- Government of Canada. STBBI Prevention Guide. Available online: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/stbbi-prevention-guide.html (accessed on 15 January 2022).
- The Public Health Agency of Canada. A Pan-Canadian Framework for Action: Reducing the Health Impact of Sexually Transmitted and Blood-Borne Infections in Canada by 2030. 2018; 25p, ISBN 978-0-660-26528-5. Available online: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/reports-publications/sexually-transmitted-blood-borne-infections-action-framework.html (accessed on 18 January 2022).
- Public Health Agency of Canada. Canadian Guidelines for Sexual Health Education (Archived); Public Health Agency of Canada: Ottawa, ON, Canada, 2009. Available online: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/cgshe-ldnemss/pdf/guidelines-eng.pdf (accessed on 28 November 2021).
- Kennell, S. Action Canada for Sexual Health & Rights 2018, 18. Available online: https://www.actioncanadashr.org/sites/default/files/2019-03/Ontario-CSE-submission-FINAL.pdf (accessed on 29 December 2021).
- Public Health Agency of Canada. Report on Hepatitis B and C Surveillance in Canada: 2019. ISBN 2369-3843. Available online: https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/diseases-conditions/report-hepatitis-b-c-canada-2019/report-hepatitis-b-c-canada-2019.pdf (accessed on 3 February 2022).
- Boyce, W.; Doherty, M.; Fortin, C.; MacKinnon, D. Canadian Youth, Sexual Health and HIV/AIDS Study. 2003. Available online: http://www.cmec.ca/Publications/Lists/Publications/Attachments/180/CYSHHAS_2002_EN.pdf (accessed on 23 December 2021).
- Ramanathan, V.; Sitharthan, G.; Pepper, K.; Wylie, K. Sexual health of Indian immigrant men in Australia: An exploratory research on help-seeking attitudes. Sex. Health 2013, 10, 380–381. [Google Scholar] [CrossRef]
- Sawleshwarkar, S.; Kakar, S.R.; Jones, R.; Lagios, K.; Mindel, A.; Hillman, R.J. Indian-born patients attending a sexual health clinic in Australia have differing characteristics to their Australian-born counterparts. Intern. Med. J. 2013, 43, 1327–1330. [Google Scholar] [CrossRef]
- Maticka-Tyndale, E.; Shirpak, K.R.; Chinichian, M. Providing for the sexual health needs of Canadian immigrants: The experience of immigrants from Iran. Can. J. Public Health 2007, 98, 183–186. [Google Scholar] [CrossRef]
- Neville, S.; Adams, J.; Researcher, S. Views about HIV/STI and health promotion among gay and bisexual Chinese and South Asian men living in Auckland, New Zealand. Int. J. Qual. Stud. Health Well-Being 2016, 1, 30764. [Google Scholar] [CrossRef]
- Kang, E.; Rapkin, B.D.; Springer, C.; Kim, J.H. The “Demon Plague” and Access to Care among Asian Undocumented Immigrants Living with HIV Disease in New York City. J. Immigr. Health 2003, 5, 49–58. [Google Scholar] [CrossRef]
- Zhou, Y.R.; Majumdar, B.; Vattikonda, N. Culture, but more than culture: An exploratory study of the HIV vulnerability of Indian immigrants in Canada. Cult. Health Sex 2016, 18, 1067–1080. [Google Scholar] [CrossRef]
- Donnelly, L.R.; Bailey, L.; Jessani, A.; Postnikoff, J.; Kerston, P.; Brondani, M. Stigma Experiences in Marginalized People Living With HIV Seeking Health Services and Resources in Canada. J. Assoc. Nurses AIDS Care 2016, 27, 768–783. [Google Scholar] [CrossRef]
- Sudhinaraset, M.; Ling, I.; To, T.M.; Melo, J.; Quach, T. Dreams deferred: Contextualizing the health and psychosocial needs of undocumented Asian and Pacific Islander young adults in Northern California. Soc. Sci. Med. 2017, 184, 144–152. [Google Scholar] [CrossRef]
- Vlassoff, C.; Ali, F. HIV-related stigma among South Asians in Toronto. Ethn. Health 2011, 16, 25–42. [Google Scholar] [CrossRef]
- Jahangir, Y.T.; Meyer, S.B. Understanding Access to and Utilisation of Sexual Health Services by South Asian Immigrant Men in Western Countries: A Scoping Review. J. Immigr. Minor. Health 2020, 22, 621–633. [Google Scholar] [CrossRef]
- Flicker, S.; Flynn, S.; Larkin, J.; Travers, R.; Guta, A.; Pole, J.; Layne, C. Sexpress: The Toronto Teen Survey Report; Planned Parenthood Toronto: Toronto, ON, Canada, 2009. [Google Scholar]
- Shoveller, J.; Johnson, J.; Rosenberg, M.; Greaves, L.; Patrick, D.M.; Oliffe, J.L.; Knight, R. Youth’s experiences with STI testing in four communities in British Columbia, Canada. Sex. Transm. Infect. 2009, 85, 397–401. [Google Scholar] [CrossRef]
- Public Health Agency of Canada. At a Glance: Prevention of Sexually Transmitted and Blood Borne Infections among Ethnocultural Communities 2015. pp. 1–27. Available online: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/std-mts/assets/pdf/blood_ethno_commun-sang_commun_ethno-eng.pdf (accessed on 30 December 2021).
- Weston, H.J. Public honour, private shame and HIV: Issues affecting sexual health service delivery in London’s South Asian communities. Health Place 2003, 9, 109–117. [Google Scholar] [CrossRef]
- Gender and Health: World Health Organziation. Available online: https://www.who.int/health-topics/gender#tab=tab_1 (accessed on 16 December 2021).
- Johnson, J.L.; Greaves, L.; Repta, R. Better science with sex and gender: Facilitating the use of a sex and gender-based analysis in health research. Int. J. Equity Health 2009, 8, 14. [Google Scholar] [CrossRef]
- Clow, B.; Pederson, A.; Haworth-Broackman, M.; Bernier, J. Rising to the Challenge: Sex- and gender-based analysis for health planning, policy and research in Canada 2009. Available online: http://pwhce.ca/pdf/RisingToTheChallenge.pdf (accessed on 12 February 2022).
- Ross, S. Gender mainstreaming in health. Gend. Med. 2006, 3, S22. [Google Scholar] [CrossRef]
- Barker, G.; Ricardo, C.; Nascimento, M. Engaging Men and Boys in Changing Gender-Based Inequity in Health: Evidence from Programme Interventions. World Health Organziation 2007. Available online: https://www.who.int/gender/documents/Engaging_men_boys.pdf (accessed on 26 December 2021).
- Wood, W.; Eagly, A.H. A cross-cultural analysis of the behavior of women and men: Implications for the origins of sex differences. Psychol. Bull. 2002, 128, 699. [Google Scholar] [CrossRef]
- Baldwin, J.D.; Baldwin, J.I. Gender differences in sexual interest. Arch. Sex. Behav. 1997, 26, 181–210. [Google Scholar] [CrossRef]
- Heinemann, J.; Atallah, S.; Rosenbaum, T. The Impact of Culture and Ethnicity on Sexuality and Sexual Function. Curr. Sex. Health Rep. 2016, 8, 144–150. [Google Scholar] [CrossRef]
- Khan, S.I.; Hudson-Rodd, N.; Saggers, S.; Bhuiyan, M.I.; Bhuiya, A.; Karim, S.A.; Rauyajin, O. Phallus, performance and power: Crisis of masculinity. Sex. Relatsh. Ther. 2008, 23, 37–49. [Google Scholar] [CrossRef]
- Lo, S.S.T.; Kok, W.M. Sexual behavior and symptoms among reproductive age chinese women in Hong Kong. J. Sex. Med. 2014, 11, 1749–1756. [Google Scholar] [CrossRef] [PubMed]
- Walton-roberts, M. South Asian Diasporas in Canada. South Asian Diaspora 2013, 5, 1–5. [Google Scholar] [CrossRef]
- Dahal, G.P.; Hennink, M.; Hinde, A. Risky Sexual Behaviour among Young Men in Nepal. 2005. Available online: http://eprints.soton.ac.uk/id/eprint/14213 (accessed on 11 November 2021).
- Nag, M. Sexual behaviour in India with risk of HIV/AIDS transmission. Health Transit. Rev. 1995, 5, 293–305. [Google Scholar]
- Statistics Canada. Immigration and Ethnocultural Diversity: Key Results from the 2016 Census. Dly 2017. Available online: https://www150.statcan.gc.ca/n1/en/daily-quotidien/171025/dq171025b-eng.pdf?st=xGmu0I8E (accessed on 27 December 2021).
- The Regional Municipality of Durham Information Report: Commissioner of Planning and Economic Development. 2018. Available online: https://www.durham.ca/en/resources/2018-Durham-Regional-Annual-Report.pdf (accessed on 22 December 2021).
- BC Centre for Disease Control and Prevention. STI in British Columbia: Annual Surveillance Report 2016; BC Centre for Disease Control: Vancouver, BC, Canada, 2016; pp. 24–37. Available online: http://www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/STI/STI_Annual_Report_2016.pdf (accessed on 5 December 2021).
- Women in Canada: A Gender-Based Statistical Report, 5th ed.; Catalogue No. 89-503-XIE; Statistics Canada: Ottawa, ON, Canada, 2005; Available online: https://www150.statcan.gc.ca/n1/en/pub/89-503-x/89-503-x2005001-eng.pdf?st=ZwvOgDeZ (accessed on 30 December 2021).
- Thorne, S.; Kirkham, S.R.; MacDonald-Emes, J. Interpretive Description: A Noncategorical Qualitative Alternative for Developing Nursing Knowledge. Res. Nurs. Health 1997, 20, 169–177. [Google Scholar] [CrossRef]
- Thorne, S. Interpretive Description: Qualitative Research for Applied Practice; Routledge Publisher: New York, NY, USA, 2016; ISBN 9781629582986. [Google Scholar]
- Hunt, M.R. Strengths and challenges in the use of interpretive description: Reflections arising from a study of the moral experience of health professionals in humanitarian work. Qual. Health Res. 2009, 19, 1284–1292. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Qualitative Research in Psychology Using thematic analysis in psychology Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Carnevale, F.A. Authentic qualitative research and the quest for methodological rigour. Can. J. Nurs. Res. 2002, 34, 121–128. [Google Scholar]
- Sandelowski, M.; Barroso, J. Finding the findings in qualitative studies. J. Nurs. Sch. 2002, 34, 213–219. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Golden, S.D.; Earp, J.A.L. Social Ecological Approaches to Individuals and Their Contexts: Twenty Years of Health Education & Behavior Health Promotion Interventions. Health Educ. Behav. 2012, 39, 364–372. [Google Scholar] [CrossRef]
- Tamang, L.; Raynes-Greenow, C.; McGeechan, K.; Black, K.I. Knowledge, experience, and utilisation of sexual and reproductive health services amongst Nepalese youth living in the Kathmandu Valley. Sex. Reprod. Healthc. 2017, 11, 25–30. [Google Scholar] [CrossRef]
- Health Canada. “Certain Circumstances”: Issues in Equity in and Responsiveness of the Health Care in Canada [A Collection of Papers and Reports Prepared for Health Canada.]. 2001. Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/hcs-sss/alt_formats/hpb-dgps/pdf/pubs/2001-certain-equit-acces/2001-certain-equit-acces-eng.pdf (accessed on 22 February 2022).
- Gill, J.M.; Mainous, A.G., 3rd. The role of provider continuity in preventing hospitalizations. Arch. Fam. Med. 1998, 7, 352–357. [Google Scholar] [CrossRef]
- Furber, A.S.; Newell, J.N.; Lubben, M.M. A systematic review of current knowledge of HIV epidemiology and of sexual behaviour in Nepal. Trop. Med. Int. Health 2002, 7, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Jahangir, Y.T.; Shrestha, A.; Alhaan, F.; Meyer, S.B. Service user and healthcare provider perspectives on barriers for men using sexually transmitted infection services in public hospital of Nepal: A qualitative study. J. Commun. Healthc. 2020, 13, 314–324. [Google Scholar] [CrossRef]
- Smith, J.A.; Braunack-Mayer, A.; Wittert, G. What do we know about men’s help-seeking and health service use? Med. J. Aust. 2006, 184, 81–83. [Google Scholar] [CrossRef]
- Addis, M.E.; Mahalik, J.R. Men, Masculinity, and the Contexts of Help Seeking. Am. Psychol. 2003, 58, 5. [Google Scholar] [CrossRef]
- Majumdar, B. Stigma as a Barrier to HIV Prevention among an Indian-Immigrant Population in Canada: A Qualitative Study. Primary Health Care 2013, 3, 137. [Google Scholar] [CrossRef]
- Islam, T.; Selvaratnam, I.; Shan, N. Building an Effective South Asian Health Strategy in Ontario. 2013. Available online: https://pchs4u.com/documents/research-reports-and-resources/CASSAs-South-Asian-Strategy-Report.pdf (accessed on 27 December 2021).
- Williams, D.J.; Prior, E.; Wegner, J. Resolving social problems associated with sexuality: Can a “sex-positive” approach help? Soc. Work 2013, 58, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Ivanski, C.; Kohut, T. Exploring definitions of sex positivity through thematic analysis. Can. J. Hum. Sex. 2017, 26, 216–225. [Google Scholar] [CrossRef]
- Dang, S.S.; Gorzalka, B.B.; Brotto, L.A. Dual Control Model in a Cross-Cultural Context: Role of Sexual Excitation in Sexual Response and Behavior Differences Between Chinese and Euro-Caucasian Women in Canada. Arch. Sex. Behav. 2019, 48, 2519–2535. [Google Scholar] [CrossRef] [PubMed]
- Cuddy, A.J.C.; Wolf, E.B.; Glick, P.; Crotty, S.; Chong, J.; Norton, M.I. Men as cultural ideals: Cultural values moderate gender stereotype content. J. Personal. Soc. Psychol. 2015, 109, 622–635. [Google Scholar] [CrossRef]
- Buzi, R.S.; Smith, P.B. Access to Sexual and Reproductive Health Care Services: Young Men’s Perspectives. J. Sex. Marital. Ther. 2014, 40, 149–157. [Google Scholar] [CrossRef]
| Characteristics | Participants (n) |
|---|---|
| Age (years) 20–22 23–25 >25 | 2 2 14 |
| Length of time in Ontario (years) 1–2 3–4 | 13 5 |
| Education Level Master’s Degree Undergraduate Degree | 6 12 |
| Country of Origin Bangladesh India Pakistan Nepal | 5 9 2 2 |
| Occupation Full-time employment Part-time employment Self-employment | 8 7 3 |
| Religion Islam Hindu | 7 11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jahangir, Y.T.; Neiterman, E.; Janes, C.R.; Meyer, S.B. Factors Influencing Sexual Health Service Use by South Asian Immigrant Men Living in Ontario, Canada: A Qualitative Study. Sexes 2022, 3, 267-281. https://doi.org/10.3390/sexes3020021
Jahangir YT, Neiterman E, Janes CR, Meyer SB. Factors Influencing Sexual Health Service Use by South Asian Immigrant Men Living in Ontario, Canada: A Qualitative Study. Sexes. 2022; 3(2):267-281. https://doi.org/10.3390/sexes3020021
Chicago/Turabian StyleJahangir, Yamin Tauseef, Elena Neiterman, Craig R. Janes, and Samantha B. Meyer. 2022. "Factors Influencing Sexual Health Service Use by South Asian Immigrant Men Living in Ontario, Canada: A Qualitative Study" Sexes 3, no. 2: 267-281. https://doi.org/10.3390/sexes3020021
APA StyleJahangir, Y. T., Neiterman, E., Janes, C. R., & Meyer, S. B. (2022). Factors Influencing Sexual Health Service Use by South Asian Immigrant Men Living in Ontario, Canada: A Qualitative Study. Sexes, 3(2), 267-281. https://doi.org/10.3390/sexes3020021






