Participatory Action Research for Adolescent Sexual and Reproductive Health: A Scoping Review
Abstract
1. Introduction
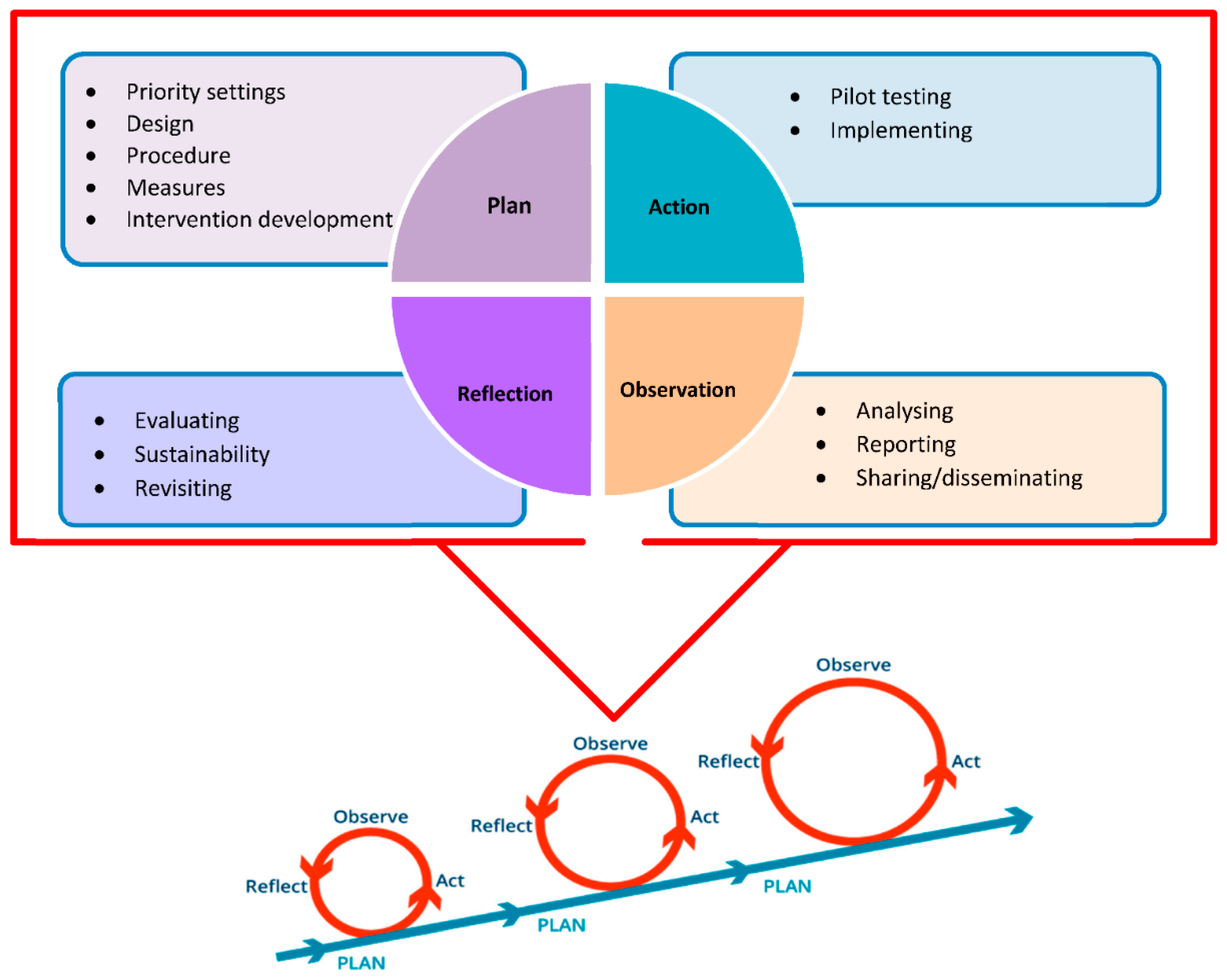
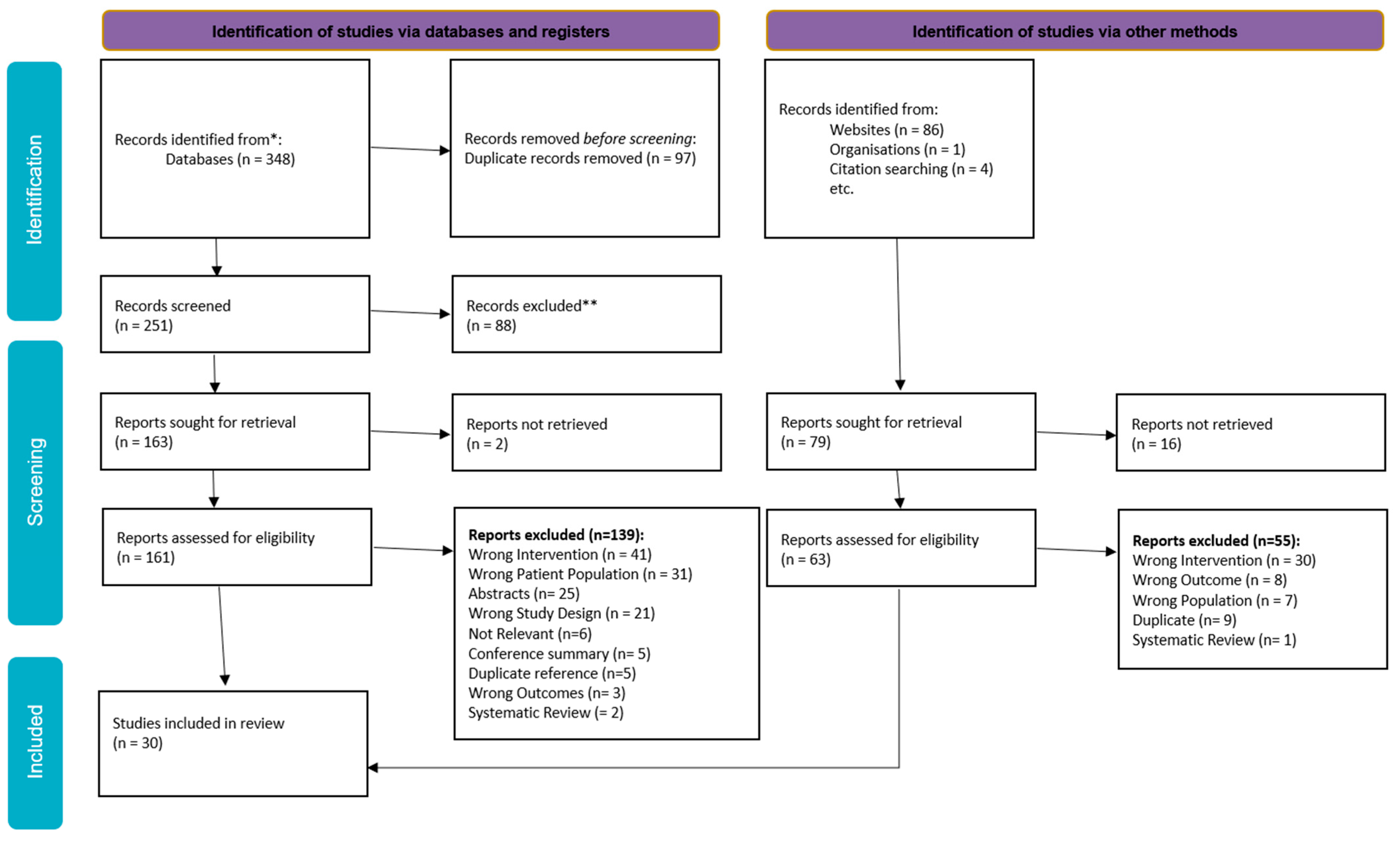
2. Methodology
3. Results
| Study Name | Country/Setting | Study Design | Participants and Sample Size | Other Stakeholders | Co-Designing Activities |
|---|---|---|---|---|---|
| Assifi 2020 [15] | Urban/community, NSW, Australia | Mixed-methods study | 16–19 years Females Stage 2-N = 384 Stage 3-N = 5–10 Stage 4-N = 6 | Research advisory group. Participants from diverse professional backgrounds n = 5–10. Service providers. Health professionals with abortion expertise. | Facilitated co-design workshop, create a framework and recommendations to inform adolescent friendly abortion service delivery in New South Wales. |
| Aventin 2021 [16] | Rural- Khayelitsha, South Africa, and Maseru, Lesetho. Community | Mixed methods | Advisory group: Lesotho: adolescents- 9 (5F/4M) Community 18+ 8 (4F/FM) Expert 18+ 13 (8F/5M) South Africa: Adolescents- 8 (5F/3M) Community 18+ 7 (5F/2M) Experts 18+ 8 (5F/3M) Focus group Lesotho: Adolescents- 28 (15F/13M) Adults- 12 (6F/6M) South Africa: Adolescents- 27 (14F/13M) Adults- 10 (8F/2M) | Advisory group: NGOs (8), health workers (2), teachers (3), principle (1), caregiver (2), community leader (2), ministry of education and training (6), ministry of health (2), UNICEF (1), social workers (2), department of health (1), western cape education department (5). Focus group: Caregivers (5), councillors (2), pastors (2), teachers (4), police officer (1), health worker (1), community leader (1), nurses (2), NGO (1), social worker (1). | Systematic and collaborative process ADVISORY GROUPS Collected primary data from 12 focus group discussions (6 in each country), eight with 55 adolescents and four with 22 adult participants.
|
| Cense 2020 [28] | Dutch high school The Netherlands | Mixed methods | Adolescents aged 12–18 N = 300 | 17 young peer researchers. | Short semi-structured interviews to explore the range of issues connected to how pupils experienced sexuality education at school. Focus group discussions to explore these issues. Photovoice sessions used to create a more open space for pupils to reflect on how sexuality education could be. |
| Cook 2021 [17] | Wollongong (NSW, Australia) School/rural | Mixed methods | 15–25 years n = not mentioned | Workshop leaders. | Condom-mapping workshops were held, and 11 ‘perfect’ condom maps were generated. Groups of young people ranged from two to five people per map. Participants sat around a large paper outline of a condom. Participants were asked to imagine their ‘perfect’ condom and to illustrate their ideas on the condom map, using both written and visual elements. |
| Cordova 2020 [29] | Michigan, USA | Mixed methods | 13 and 21 years N = 50 | Clinicians clinic director staff. | Youth leadership council involved in:
|
| Decker 2020 [13] | Community, rural, Fresno County, California, USA | cluster randomized controlled trial | 1260 youth ages 13–19 years | None stated. | October 2017 and ended in March 2020 Development:
|
| Fongkaew 2006 [41] | Public and Private schools Chaing Mai Province, Thailand | Mixed methods | 42 youth leader trainers or senior youth leaders (SYLs), 16 males and 26 females; 104 junior youth leaders (JYLs), including 38 males and 66 females, studying in Grade 7 at 12 schools; 2300 students in Grades 5–7 at 12 schools. 1159 males and 1141 females. | Youth leader trainers or senior youth leaders (n = 42), 16 males and 26 females; Junior youth leaders (n = 104), including 38 males and 66 females, studying in Grade 7 at 12 schools. Teacher (n = 46) from 12 schools, 11 males and 35 females; Parents. Other stakeholders including school administrators, school committee members, parent representatives and public health personnel. | Youth-adult partnership with schools. Youth leader trainers developed three curricula for SRH education and HIV/AIDS prevention on (1) leadership; (2) rights, duties, and responsibilities; and (3) HIV/SRH. YLTs attended skill training camps, rehearsed, and practiced being YLTs and served as trainers and mentors for YYLs. |
| Garwick 2008 [30] | Minneapolis and St. Paul, Minnesota, USA Urban/community | Mixed methods | 148 Native youth 13–15 and 16–18 years | Native community leaders and project consultants NTV research team included two faculty, a project coordinator from the University of Minnesota, and seven community consultants The project coordinator and community consultants (four adults; three youth, 18 –21 years). | Group discussion and questionnaires that took about 2 h. Focus group discussions co-led by an adult and youth native project consultant of the same gender as the participants in community-based organizations. The adult facilitator guided the focus group discussion using an interview guide containing core and probe questions. The youth facilitator captured participant ideas on a poster-sized flip chart and asked clarifying questions. |
| Gilbert 2021 [5] | Darwin, Australia | mixed methods | Youth working group (YWG): 4 Aboriginal and Torres Strait Islander and 3 non-Indigenous youth aged 18–25 years. | Clinicians Researchers Students working in the field of Aboriginal and Torres Strait Islander health and/ or sexual reproductive health. | Four 90 min consultations with YWG, 5 to 10 participants, with one researcher. YWG members shared their current understandings of preconception health, experiences of preconception care and how they currently obtain related health information. YWG members identified components of preconception health identified in q1 they would like to know more about and which components they felt were most important. YWG members asked what they believe are the strengths and weaknesses of current resources, what were the most useful sources of information and what resource features or functions would best suit their needs. Preferences for graphic design and illustrations were also discussed. |
| Gill 2016 [18] | Local youth outreach centre USA The Ottawa Hospital and St Mary’s Youville | Prospective qualitative community-based participatory research Nine-step validated qualitative participatory approach that combined documentary photography with focus groups | Ages 15–25 years | Key stakeholders at outreach centre. | Stage 1: Reviewing the objectives of the study and the photovoice method; brainstorming with the participants on the various structural and biological factors that affect reproductive and sexual health; training on the use of the disposable camera; and the ethics and safety of photography and the use of a third-party release form for individuals captured in photographs Stage 2: Occurred approximately 6–8 weeks later. This was to provide an opportunity for the participants to return their completed package, as well as for the researchers to print the photographs for the subsequent session. Participants had an opportunity to select approximately 10–15 pictures that they believed illustrated their perspective on reproductive and sexual health issues. The selected photographs were transferred to a laptop and each photograph was an interpretation by each participant, as it related to the key objectives of this study. Participants discussed each other’s photographs as a group and identified common key themes and how to best use their pictures to develop interventions to promote reproductive and sexual health among their peers. |
| Guerrero 2020 [31] | Peru (Lima, Ayacucho, and Loreto) rural community | Content development | STAGE 1: 68 13–24-year-old Aged 13–17 (22F/10M) Aged 13–24 (23F/13M) STAGE 2: No adolescents involved STAGE 3: 104 adolescents (52% F/48% M) | Adult advisers. | Six community consultations in the three study sites, with two meetings at each site with the following structure: one meeting with 13–17-year-old females and males and an adult adviser; and one meeting with 18–24-year-old females and males and an adult adviser. Development of short message services—no adolescent involvement. A total of 12 focus groups to validate SMS content each group of participants evaluated 36–37 SMS (146 SMS in total), each adolescent received a form to rate each SMS, ranging from very bad (1 point) to very good (4 points). |
| Haruna 2019 [32] | Three secondary schools from Dar es Salaam, Tanzania | Quasi-experimental andomized controlled trial research design | 348 secondary school participants (students) between 11 and 15 years of age There were 193 boys (55.5 per cent) and 155 girls (44.5 per cent) | Paediatricians, sexual and reproductive health specialists, sexual health teachers from participating schools, computer, information science specialists (including the game designer, who is a computer engineer), and the targeted end-users themselves (secondary school students in Dar es Salaam). | The evaluation of the effectiveness of iterations of the game was done using adolescent sexual health literacy tests and the validated Motivation, Attitude, Knowledge and Engagement framework. The whole process of game design, testing, evaluation, and refinement were underpinned by the activity theory and participatory design (PD) research. |
| Holiday 2020 [33] | Community, American southern states | Mixed methods | Research phase:
recruited 431 teens and enrolled 246 (57%) into the project. Among them, 178 (72%) completed all sessions. 14–18 years | Six adults in the focus groups Parents / guardians | Six focus groups were held with both teens and parents/guardians of teens. A total of 48 months (4 years).
|
| Hong 2010 [14] | China Public middle school/rural | Mixed methods | 10–14 years Males & females N = 102 | Teachers = 15 Parents = 12 | Program:
|
| Hubert 2021 [34] | Urban communities in the states of Mexico and Morelos, | Mixed methods | 45 participants (23 women and girls and 22 men and boys) aged 12 to 19 | E-learning: three exploratory workshops, no exact number of participants. Online chat: 21 including thematic and academic experts, public officials, members of civil society, and health personnel involved in SRH for adolescents. | Four focus groups (FGs) two FGs comprised adolescents aged 12 to 14 and two comprised adolescents 15- to 19-years old; each age group was divided by sex. |
| Ivanova 2016 [35] | Latin America (Bolivia, Ecuador, and Nicaragua) rural/community | Mixed methods | 9 adolescents 10–19 years | 10 parents 3 heath care providers 3 friends of youth/health promoters 6 community leaders 3 country implementers 3 project leaders 3 consortium management | 18 in-depth interviews and 21 focus group discussions with stakeholders and beneficiaries. Data were collected through key informant interviews (KIIs) and focus group discussions (FGDs) with the key stakeholders of CERCA–adolescents, parents, teachers, community leaders, peer educators, health care providers, project leaders at the country level, implementers at the country level and the international consortium management team |
| Jaworsky 2013 [19] | Ontario, Canada | Mixed methods | 18 youth (aged 16–28 years) sexual health peer educators | None stated |
|
| Jones 2012 [36] | School rural, Kabarole District, western Uganda | Mixed methods | 51 students (25F/26M) (age 13 to 18, average 15.6 years), 24 from School A and 27 from School B | School administrators and staff | Focus group discussions including students and teachers from two secondary schools in a rural district of western Uganda. Semi-structured focus groups and interviews and through meeting artefacts, including notes, flip charts, lesson plans and observations. A total of almost 25 h were recorded and transcribed. |
| Lofton 2020 [37] | Community, sub-Saharan Africa | Mixed methods | 24 youth, ages 13–17 (12 males and 12 females) | Two adult facilitators per photovoice session, 12 in total | Youth used a systematic action planning process to develop action plans.
Finally, the youth codified their ideas through the pile sorting activity, which allowed them to identify themes and rank these in terms of priorities. They then used a systematic action planning process, described in Results section, to develop an action plan for each prioritized theme. Youth also had to identify the target for their solution, specifically which stakeholders in the community will help them carry out the plan. |
| Marinkovich 2014 [38] | Kisumu, Kenya | Mixed methods | 40 adolescents (13–17 years) Living with HIV | Co-researchers/peer leaders | Participant-generated data was collected in the form of interviews and focus groups. Interviews and focus groups were voice-recorded, transcribed and when necessary, translated. The research team interviewed 40 participants through three individual interviews and seven focus groups. |
| Markus 2012 [20] | Wind River Wyoming, USA Wind River UNITY group | Mixed methods | 6 co-researchers 18- and 19-year-old AI/IN | Wyoming Health Council | Designing the content and activity of the program. In the photovoice project, the model provided a way for the participants to think about their project in terms of its potential to empower them, as individuals, to help them develop and sustain healthy relationships, and, in turn, to advocate for themselves in their communities, institutions, and even in society at large. Aided in analysis of each co-researchers photovoice stories. |
| Newby 2017 [21] | UK Urban/school | Mixed methods | 10 young people aged 11 to 16 years (making the YPPB) 13- to 19-year-old N = 24 | Two health psychologists: A public health consultant A project manager 12 professionals from a variety of services |
|
| Nolan 2020 [40] | Community, urban Kigali, peri-urban Ruhango, and peri-urban Butare Rwanda | Cluster randomized controlled trial | Design aspect N = 600 Control trial: 100 students per school, for a total of 6000 students in the study. | Parents Teachers Community leaders, including some religious leaders Health care providers Control trial: 60 schools in 8 districts in Rwanda | The first phase, conducted from 2016 to 2019. Design Research
Prototyping: Youth Having users (adolescents) react to a tangible idea in the form of a prototype, rather than abstract concept.
|
| Patchen 2020 [22] | District of Columbia (DC) and Birmingham, Alabama (AL) | Mixed methods | African American Males and females aged 15–21 N = 86 6 individuals, 3 males and 3 females 26 youths participated in usability testing, 54 individuals 23 from AL and 31 from DC participated in focus groups | Gaming experts with graduate and undergraduate degrees programmed the game with assistance from graphic artists, script writers, and audio/visual specialists. | Initial design and features of the game were driven by four meetings with the youth advisory board, where the initial game prototype—an initial version of the game—was developed and refined based on feedback obtained after each meeting. The advisory board then played the prototype for at least an hour and provided feedback on content, artwork, and design, minigames, dialogue, and entertainment value. All participants tested the game prototype and completed the system usability scale (SUS). Possible scores range from 0 (not usable) to 100 (perfectly usable). Focus groups with participants to guide additional development, to the game. |
| Pensak 2020 [23] | USA (Connecticut) urban/school | Mixed methods | Phase 1: 15 adolescents Phase 2: 24 participants of 15- to 17-year-old | Parents (of adolescents involved) | Phase 1: Focus group sessions to identify key themes and specific domains of impact Phase: 2
|
| Shahmanesh 2021 [24] | Community, rural south Africa uMkhanyakude district of KZN waZulu-Natal (KZN). | Mixed methods | 18–30 years | Two teams of four social science researchers | Between March 2018 and September 2019 Leadership training:
|
| Shegog 2017 [39] | USA (American Indian/Alaska Native (AI/AN)) rural/school | Mixed methods | Phase 1: AI/AN Youth (n = 80) ages 9–16 years Phase 3: AI/AN Youth (n = 45) ages 11–15 years | Parents Health educators Health care providers Community members adult stakeholders (n = 27) | Phase 1: Gain their perspectives on needed adaptations of of IYG-Tech. Phase 3: Usability testing of NATIVE-IYG tech. |
| Simuyaba 2021 [25] | Community rural, Zambia | Mixed methods | 230 adolescents and young people 15–24 years | 21 adults Adults (parents/guardians) community gate keepers and health committee members | Data were collected through focus group discussions, in-depth interviews, and observations. Between November 2018 and March 2019:
|
| Wood 2016 [26] | Schools, south Africa | Mixed methods | 24–11 graders (14F/10M) | Researcher from community | Data were generated through two purposive discussions with the participants. Discussions with the participants, led by a young researcher from their community rather than by (researchers), to encourage openness and honesty. The peer educator participants also decided to gather data from other youth in the school by means of short open-ended questionnaires. Individual interviews were taped and transcribed verbatim, and the peer educators synthesised the data they gathered by means of the questionnaires into narratives. |
| Zaleski 2015 [27] | USA (Illinois) Rural/community | Mixed-methods | Twenty youth leaders 84 interviewees, 16–22 years | not mentioned | Conducted four one-on-one interviews with their Chicago peers for a total of 80 individual interviews. Youth leaders created and disseminated surveys of their personal networks, including schools and colleges, and ICAH disseminated to national networks, including partnering organizations, movement building organizations, and school systems across the country that ICAH works with (convenience sample). Youth leaders participated in 1 in person focus group, facilitated by the youth education coordinator, which focused on connecting the online comfort-assessment survey to positive sexual decision-making among youths. |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Salam, R.A.; Faqqah, A.; Sajjad, N.; Lassi, Z.S.; Das, J.K.; Kaufman, M.; Bhutta, Z.A. Improving adolescent sexual and reproductive health: A systematic review of potential interventions. J. Adolesc. Health 2016, 59, S11–S28. [Google Scholar] [CrossRef] [PubMed]
- Chandra-Mouli, V.; Lane, C.; Wong, S. What does not woerk in adolescent sexual and reproductive health: A revew of evidence on interventions commonly accepted as best practices. Glob. Health Sci. Pract. 2015, 3, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Lassi, Z.S.; Salam, R.A.; Das, J.K.; Wazny, K.; Bhutta, Z.A. An unfinished agenda on adolescent health: Opportunities for interventions. Semin. Perinatol. 2015, 39, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Goodyear-Smith, F.; Jackson, C.; Greenhalgh, T. Co-design and implementation research: Challenges and solutions for ethics committees. BMC Med. Ethics 2015, 16, 78. [Google Scholar] [CrossRef]
- Gilbert, E.; Collins, R.; Webster, V.; Boyd, N.; Maple-Brown, L.; Boyle, J.; Smith-Vaughan, H. Using co-design to develop a culturally responsive reproductive health learning resource for Aboriginal and Torres Strait Islander youth. Health Promot. J. Aust. 2021, 32, 179–185. [Google Scholar] [CrossRef]
- Mbachu, C.O.; Clara Agu, I.; Onwujekwe, O. Collaborating to co-produce strategies for delivering adolescent sexual and reproductive health interventions: Processes and experiences from an implementation research project in Nigeria. Health Policy Plan. 2020, 35 (Suppl. 2), ii84–ii97. [Google Scholar] [CrossRef]
- Thabrew, H.; Fleming, T.; Hetrick, S.; Merry, S. Co-design of eHealth interventions with children and young people. Front. Psychiatry 2018, 9, 481. [Google Scholar] [CrossRef]
- Vindrola-Padros, C.; Barbosa, E.C.; Ramsay, A.I.; Turner, S.; Morris, S.; Agble, R.; Caldwell-Nichols, A.; Fulop, N.J. Mixed methods evaluation of a hospital group model using an embedded research approach: Study protocol. BMJ Open 2019, 9, e027086. [Google Scholar] [CrossRef]
- Denno, D.M.; Hoopes, A.J.; Chandra-Mouli, V. Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support. J. Adolesc. Health 2015, 56, S22–S41. [Google Scholar] [CrossRef]
- Mehta, S.D.; Seeley, J. Grand challenges in adolescent sexual and reproductive health. Front. Reprod. Health 2020, 2, 2. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Covidence Systematic Review Software. Veritas Health Innovation: Melbourne, Australia. Available online: www.covidence.org (accessed on 28 September 2021).
- Decker, M.J.; Gutmann-Gonzalez, A.; Price, M.; Romero, J.; Sheoran, B.; Yarger, J. Evaluating the effectiveness of an intervention integrating technology and in-person sexual health education for adolescents (in the know): Protocol for a cluster randomized controlled trial. JMIR Res. Protoc. 2020, 9, e18060. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Fongkaew, W.; Senaratana, W.; Tonmukayakul, O. Development of a theory-based sexual and reproductive health promotion and HIV prevention program for Chinese early adolescents. Nurs. Health Sci. 2010, 12, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Assifi, A.R.; Kang, M.; Sullivan, E.; Dawson, A.J. Assessing care trajectories of adolescent females seeking early induced abortion in New South Wales: Multistage, mixed-methods study protocol. BMJ Open 2020, 10, e039819. [Google Scholar] [CrossRef] [PubMed]
- Aventin, Á.; Rabie, S.; Skeen, S.; Tomlinson, M.; Makhetha, M.; Siqabatiso, Z.; Lohan, M.; Clarke, M.; Lohfeld, L.; Thurston, A.; et al. Adaptation of a gender-transformative sexual and reproductive health intervention for adolescent boys in South Africa and Lesotho using intervention mapping. Glob. Health Action 2021, 14, 1927329. [Google Scholar] [CrossRef]
- Cook, S.M.; Grozdanovski, L.; Renda, G.; Santoso, D.; Gorkin, R.; Senior, K. Can you design the perfect condom? Engaging young people to inform safe sexual health practice and innovation. Sex Educ. 2021, 22, 110–122. [Google Scholar] [CrossRef]
- Gill, R.; Black, A.; Dumont, T.; Fleming, N. Photovoice: A strategy to better understand the reproductive and sexual health needs of young mothers. J. Pediatr. Adolesc. Gynecol. 2016, 29, 467–475. [Google Scholar] [CrossRef]
- Jaworsky, D.; Larkin, J.; Sriranganathan, G.; Clout, J.; Janssen, J.; Campbell, L.; Flicker, S.; Stadnicki, D.; Erlich, L.; Flynn, S. Evaluating youth sexual health peer education programs: “Challenges and suggestions for effective evaluation practices”. J. Educ. Train. Stud. 2013, 1, 227–234. [Google Scholar] [CrossRef][Green Version]
- Markus, S.F. Photovoice for healthy relationships: Community-based participatory HIV prevention in a rural American Indian community. Am. Indian Alsk. Nativ. Ment. Health Res. 2012, 19, 102–123. [Google Scholar] [CrossRef]
- Newby, K.V.; Brown, K.E.; Bayley, J.; Kehal, I.; Caley, M.; Danahay, A.; Hunt, J.; Critchley, G. Development of an intervention to increase sexual health service uptake by young people. Health Promot. Pract. 2017, 18, 391–399. [Google Scholar] [CrossRef]
- Patchen, L.; Ellis, L.; Ma, T.X.; Ott, C.; Chang, K.H.K.; Araya, B.; Atreyapurapu, S.; Alyusuf, A.; Lanzi, R.G. Engaging african american youth in the development of a serious mobile game for sexual health education: Mixed methods study. JMIR Serious Games 2020, 8, e16254. [Google Scholar] [CrossRef] [PubMed]
- Pensak, M.J.; Lundsberg, L.S.; Stanwood, N.L.; Cutler, A.S.; Gariepy, A.M. Development and feasibility testing of a video game to reduce high-risk heterosexual behavior in spanish-speaking latinx adolescents: Mixed methods study. JMIR Serious Games 2020, 8, e17295. [Google Scholar] [CrossRef] [PubMed]
- Shahmanesh, M.; Okesola, N.; Chimbindi, N.; Zuma, T.; Mdluli, S.; Mthiyane, N.; Adeagbo, O.; Dreyer, J.; Herbst, C.; McGrath, N.; et al. Thetha Nami: Participatory development of a peer-navigator intervention to deliver biosocial HIV prevention for adolescents and youth in rural South Africa. BMC Public Health 2021, 21, 1393. [Google Scholar] [CrossRef]
- Simuyaba, M.; Hensen, B.; Phiri, M.; Mwansa, C.; Mwenge, L.; Kabumbu, M.; Belemu, S.; Shanaube, K.; Schaap, A.; Floyd, S.; et al. Engaging young people in the design of a sexual reproductive health intervention: Lessons learnt from the Yathu Yathu (“For us, by us”) formative study in Zambia. BMC Health Serv. Res. 2021, 21, 753. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.; Hendricks, F. A participatory action research approach to developing youth-friendly strategies for the prevention of teenage pregnancy. Educ. Action Res. 2017, 25, 103–118. [Google Scholar] [CrossRef]
- Zaleski, N.; Martin, P.; Messinger, J. Given and chosen: Youth-led research on family-supported conversations about sexuality. Fam. Community Health 2015, 38, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Cense, M.; Grauw, S.; Vermeulen, M. ‘Sex is not just about ovaries’. Youth participatory research on sexuality education in the netherlands. Int. J. Environ. Res. Public Health 2020, 17, 8587. [Google Scholar] [CrossRef] [PubMed]
- Cordova, D.; Munoz-Velazquez, J.; Mendoza Lua, F.; Fessler, K.; Warner, S.; Delva, J.; Adelman, N.; Counlic, Y.L.; Fernandez, A.; Bauermeister, J. Pilot study of a multilevel mobile health app for substance use, sexual risk behaviors, and testing for sexually transmitted infections and HIV among youth: Randomized controlled trial. JMIR Mhealth Uhealth 2020, 8, e16251. [Google Scholar] [CrossRef]
- Garwick, A.W.; Rhodes, K.L.; Peterson-Hickey, M.; Hellerstedt, W.L. Native teen voices: Adolescent pregnancy prevention recommendations. J. Adolesc. Health 2008, 42, 81–88. [Google Scholar] [CrossRef]
- Guerrero, F.; Lucar, N.; Garvich Claux, M.; Chiappe, M.; Perez-Lu, J.; Hindin, M.J.; Gonsalves, L.; Bayer, A.M. Developing an SMS text message intervention on sexual and reproductive health with adolescents and youth in Peru. Reprod Health 2020, 17, 116. [Google Scholar] [CrossRef]
- Haruna, H.; Zainuddin, Z.; Mellecker, R.R.; Chu, S.K.; Hu, X. An iterative process for developing digital gamified sexual health education for adolescent students in low-tech settings. Inf. Learn. Sci. 2019, 120, 723–742. [Google Scholar] [CrossRef]
- Holliday, R.C.; Phillips, R.; Akintobi, T.H. A community-based participatory approach to the development and implementation of an HIV health behavior intervention: Lessons learned in navigating research and practice systems from project Happy. Int. J. Environ. Res. Public Health 2020, 17, 399. [Google Scholar] [CrossRef] [PubMed]
- Hubert, C.; Estrada, F.; Campero, L.; Heredia-Pi, I.B.; Villalobos, A.; Suárez-López, L.; Ibáñez-Cuevas, M.; Barrientos, T. Designing digital tools capable of reaching disadvantaged adolescents and improving their sexual health: A mexican experience. J. Health Care Poor Underserved 2021, 32, 62–84. [Google Scholar] [CrossRef]
- Ivanova, O.; Cordova-Pozo, K.; Segura, Z.E.; Vega, B.; Chandra-Mouli, V.; Hindin, M.J.; Temmerman, M.; Decat, P.; De Meyer, S.; Michielsen, K. Lessons learnt from the CERCA Project, a multicomponent intervention to promote adolescent sexual and reproductive health in three Latin America countries: A qualitative post-hoc evaluation. Eval. Program Plan. 2016, 58, 98–105. [Google Scholar] [CrossRef]
- Jones, A.C. Exploring Ugandan Secondary School Students’ Sexual Health Education Needs and Developing School-Based Sexual Health Interventions through Participatory Action Research. Master’s Thesis, University of Alberta, Edmonton, AB, Canada, 2012. [Google Scholar]
- Lofton, S.; Norr, K.F.; Jere, D.; Patil, C.; Banda, C. Developing action plans in youth photovoice to address community-level HIV risk in rural Malawi. Int. J. Qual. Methods 2020, 19, 1609406920920139. [Google Scholar] [CrossRef]
- Marinkovich, Z.A.H. Growing up with HIV in Kisumu, Kenya: Participatory Action Research with Young People Living with HIV. Ph.D. Thesis, University of San Francisco, San Francisco, CA, USA, 2014. [Google Scholar]
- Shegog, R.; Craig Rushing, S.; Gorman, G.; Jessen, C.; Torres, J.; Lane, T.L.; Gaston, A.; Revels, T.K.; Williamson, J.; Peskin, M.F.; et al. NATIVE-it’s your game: Adapting a technology-based sexual health curriculum for american indian and alaska native youth. J. Prim. Prev. 2017, 38, 27–48. [Google Scholar] [CrossRef]
- Nolan, C.; Packel, L.; Hope, R.; Levine, J.; Baringer, L.; Gatare, E.; Umubyeyi, A.; Sayinzoga, F.; Mugisha, M.; Turatsinze, J.; et al. Design and impact evaluation of a digital reproductive health program in Rwanda using a cluster randomized design: Study protocol. BMC Public Health 2020, 20, 1701. [Google Scholar] [CrossRef]
- Fongkaew, W.; Fongkaew, K.; Muecke, M. HIV/sexual and reproductive health program for HIV prevention: The youth-adult partnership with schools approach. J. Med. Assoc. Thailand 2006, 89, 1721–1732. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lassi, Z.S.; Neideck, E.G.; Aylward, B.M.; Andraweera, P.H.; Meherali, S. Participatory Action Research for Adolescent Sexual and Reproductive Health: A Scoping Review. Sexes 2022, 3, 189-208. https://doi.org/10.3390/sexes3010015
Lassi ZS, Neideck EG, Aylward BM, Andraweera PH, Meherali S. Participatory Action Research for Adolescent Sexual and Reproductive Health: A Scoping Review. Sexes. 2022; 3(1):189-208. https://doi.org/10.3390/sexes3010015
Chicago/Turabian StyleLassi, Zohra S, Ebony Grace Neideck, Bridget Mary Aylward, Prabha H. Andraweera, and Salima Meherali. 2022. "Participatory Action Research for Adolescent Sexual and Reproductive Health: A Scoping Review" Sexes 3, no. 1: 189-208. https://doi.org/10.3390/sexes3010015
APA StyleLassi, Z. S., Neideck, E. G., Aylward, B. M., Andraweera, P. H., & Meherali, S. (2022). Participatory Action Research for Adolescent Sexual and Reproductive Health: A Scoping Review. Sexes, 3(1), 189-208. https://doi.org/10.3390/sexes3010015








