Abstract
Introduction: Considering a growing number of female sex workers (FSWs) in Bangladesh, there remains a greater need to reduce sexually transmitted infection (STI) rates, as lower social and cultural status cause FSWs to have less access to education, employment opportunities, and health care, including opportunities for HIV tests, counseling, and medical care. Methods: A cross-sectional study was conducted among 546 street, hotel, and residence-based FSWs. This current study aimed to identify the prevalence and to ascertain the associated risk factors among the FSW populations in Dhaka. Results: We found a majority of the participants were in the working age of more than 26 years for the FSW profession, with a mean age of 28 years. While the majority were unemployed (42.5%), alcohol abuse (p = 0.01) and drug dependency (p = 0.01) had an association, and inconsistency of condom use had a higher risk factor (AOR = 3.54) for a new STI case. Conclusions: FSW-oriented service platform should be integrated with health literacy interventions in urban and rural locations in Bangladesh. Understanding the differences in risk patterns and tailoring intervention will increase contraception use and lower STI cases and improve overall FSW quality of life.
1. Introduction
Curable non-viral pathogens account for a significant burden of sexually transmitted infections (STIs), while evidence suggests that STIs increase both HIV infection and transmission [1]. Although there have been steady advances in diagnosis, treatment, and public health interventions, STIs continue to affect a large proportion of those living in resource-limited settings, particularly women of reproductive age [2]. In recent years, a synergistic relation of STI with HIV in global HIV/AIDS control programs have focused attention on STI prevention and control to combat an HIV epidemic [3]. Many countries around the world are experiencing an epidemic of sexually transmitted diseases [4]. While Bangladesh is still fortunate in avoiding an AIDS epidemic and prevalence for AIDS is low, the country is still highly vulnerable to HIV/AIDS because of high-risk behaviors and increased risk of contracting STIs [5]. Every day, there are more than 1 million new cases of curable STIs among people aged 15–49 years [6]. STIs have a profound impact on the health of adults and children worldwide. If untreated, they can lead to serious and chronic health effects that include neurological and cardiovascular disease, infertility, ectopic pregnancy, stillbirths, and increased risk of HIV [7]. Chronic pelvic pain from untreated bacterial STIs is an important reason for health care visits among females. In developing countries, sexually transmitted diseases are also among the leading causes of disability-adjusted life years lost for females of reproductive age [8].
According to the WHO Global Health Sector Strategy on Sexually Transmitted Infections 2016–2021, the first strategic direction is to collect information on STI prevalence and incidence among the key population [9]. However, unlike other developing countries, STIs and reproductive tract infections (RTIs) represent a major public health problem in Bangladesh [10]. In 1996, it was estimated that there were 2.3 million cases of STIs in Bangladesh, while 89% of women and 81% of men were identified as not knowing of any STIs other than acquired immune deficiency syndrome (AIDS) [11,12]. Additionally, STI cases are often underestimated among sexually active women, as many of the STI symptoms are not easily recognized and many STIs do not have visible symptoms [13]. Bangladesh, being a developing country, faces challenges in reporting STIs as elaborate laboratory methods are scarce [11]. Besides, Bangladeshi women have been documented to be vulnerable to STIs, including HIV/AIDS, and their knowledge about different diseases is reported to be poor [14]. Furthermore, lack of awareness and cultural taboos increase a woman’s risk of contracting STIs due to unsafe behavior stigmatization in the community and increasing non-disclosure. As a consequence, women may be less likely to discuss their sexual health and seek appropriate treatment [2,14].
There is a growing need to raise awareness about how to reduce rates and to manage STIs in Bangladesh as patients diagnosed with STIs receive very limited or no counseling services on safe sex, HIV transmission, and partner referral, largely because of time constraints of the service providers [14,15]. Considering a growing number of female sex workers (FSWs) in Bangladesh, their estimated population range from 50,000 to 100,000 [2,15]. However, there is limited information on how sexual health promotion and preventative measures against various STIs are effectively met by the government and non-government organizations for this key population [2,15]. In recent times, public health interventions (e.g., STI health promotion and preventative measures) have been categorized based on where FSWs solicit clients [16]. Women working in bars, hotels, and other recreational facilities have been documented to have a higher risk of STIs, including HIV, than the general population [17]. In addition, for FSWs working in brothels, streets, hotels, and residences in recent years, there has been a remarkable change in the nature of the sex industry, namely due to eviction of brothels from major cities; increased demand for sex workers in non-stigmatized locations; demand for flexible working times by FSWs; demands for more freedom and opportunity of income by FSWs [16,18]. Furthermore, hotel-based FSWs have a higher client turnover than their peers on the streets and in brothels, while the payment per client in a hotel remains considerably higher than that of the other two locations [8,15]. However, literature found that the rate of condom use among hotel-based FSWs remains low and the vulnerability of these populations to contract STIs and HIV remains very high [15].
FSWs are often responsible for the transmission of STIs and HIV to the general population who come in contact with this key population [19]. In addition, the majority of FSWs belong to lower social and cultural status, while having less access to education, employment opportunities, and health care, including opportunities for STI/HIV tests, counseling, and medical care [20]. Likewise, traditional gender roles result in women lagging behind men in the utilization of healthcare services in developing countries [21]. Prevailing norms of masculinity can encourage high-risk sexual behavior among men, making their partners more vulnerable to sexually transmitted diseases, and may prevent women from accessing proper information and services related to STIs [15]. As very limited research remains in determining the prevalence of new STI cases of FSWs from all three locations of the street, hotel, and residence-based sexual activity sites, this study aimed to identify the prevalence of STI cases from all three locations in Dhaka city of Bangladesh and the associated risk factors among the FSW populations.
2. Methods
A cross-sectional study was conducted through a nonrandom sampling procedure between October to December 2019 among street-based, hotel-based, and residence-based FSWs who were enlisted to receive services from three drop-in-centers (DICs) in Dhaka. The three DICs operate under a local non-government organization, Lighthouse Bangladesh. A total of 546 FSWs were calculated as the sample size by using a standard formula and considering a 95% confidence interval (CI) and extrapolated from the prevalence of earlier on FSW with STI cases in Bangladesh [2,22]. The identification of street-based, hotel-based, and residence-based FSWs followed the operational definition set during the serological surveillance in Bangladesh [5]. For our study, we operationalized the definition of a new STI case as ‘STI new syndrome or new case’ among FSWs as participants who previously were not diagnosed for an STI case at all and not the follow-up cases. Participants were enrolled in the study based on the following criteria: (a) enlisted to seek health counseling and STI/HIV prevention and treatment services from all three DICs; (b) FSWs who gave verbal or written consent voluntarily. While participants were not included in the study if: (a) they had a recent history of menstruation; (b) FSWs who were previously detected as HIV positive; (c) FSWs had a history of taking any antibiotic in the preceding two weeks before coming for health service in DIC; (d) FSWs did not give consent for performing gynecological examination (e.g., per vaginal examination). A formatted questionnaire was used as a data collection tool in the study. During the data collection process, the Lighthouse Bangladesh organization provided their administrative and technical support. Pre-testing of the checklist (e.g., past medical history, sexual history, obstetric and gynecological history, general examination) were performed by the relevant trained Lighthouse Bangladesh organization health personnel in coordination with the primary researchers to ensure its adequacy, appropriateness, and quality. Information was collected by the primary researchers who are registered medical practitioners and a registered assistant health care provider working at the DIC study location. Interviews were conducted on FSWs about symptoms suggestive of STI and the assistant health care provider performed a gynecological examination including an inspection and per vaginal examination (e.g., speculum examination). All data were kept confidential and the analysis was completed using IBM SPSS Statistics Version 27 (IBM, Armonk, NY, USA).
3. Results
In terms of sociodemographic profile, around 62.5% of the participants were in the working age of more than 26 years for the FSW profession, with a mean age of 28 years. The majority of FSWs were illiterate (52.7%) and 42.5% of FSWs were unemployed. More than half of the FSWs (56%) were married while only 12% were single and almost 23% lived as separated (Table 1). As for the prevalence from the study population of 546 FSW respondents, 313 patients (57.3%) had new sexually transmissible infection (STI) cases. In terms of STI symptoms for FSWs, the most common was vaginal discharge (56.8%), followed by vaginal itching (12.5%), and lower abdominal pain (10.8%) while dysuria was 3.3% and dyspareunia was 4.6% (Table 2). As FSW working professions are quite broad and varied, the working locations had certain variabilities as well. The majority of the FSWs worked from the street-based locations (46.7%) while some worked in residence (27.8%) and the remaining were mainly working at hotels (25.5%). Further, our data found that there were more new cases of STIs in hotels (62%) (Figure 1). We also found a significant association between the consistency of condom use and a new case of STI (p < 0.01). In addition, we found that more than half of the FSWs (54%) were engaged in frequent intercourse between 3-4 times, and contracting a new STI, but there was no significant association between the frequency of intercourse with that of a new STI case (Table 1).

Table 1.
Sociodemographic characteristics, sexual behavior, and associated risk of FSW with new STI cases.

Table 2.
Prevalence of STI among 546 FSWs from three DICs in Dhaka, Bangladesh.
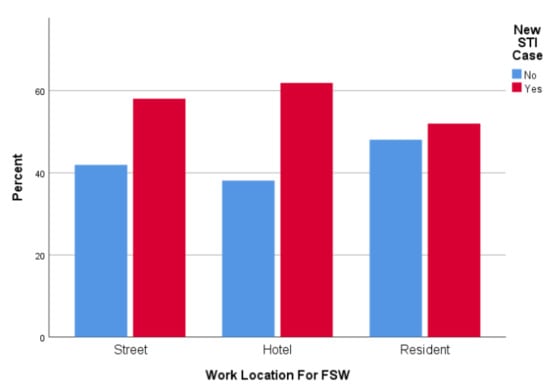
Figure 1.
Work Locations of FSW and new STI case.
We found that alcohol intake (p = 0.01) and drug dependency (p = 0.01) were significantly associated with contracting a new STI case. In multivariable analysis, we performed multiple logistic regression to identify the predictors associated with STI (Table 3). We considered the variables in our model which were found to be significant in our univariate analysis. We found that drug dependency was significantly associated with STI (adjusted OR = 0.51, 95% CI 0.31–0.86). Additionally, alcohol intake was more likely related to a new STI case (adjusted OR = 1.87, 95% CI 1.10–3.17). As for the consistency in condom use during intercourse, there was 3.5 times more probability for FSW to contract with a new case of STI (adjusted OR = 3.54, 95% CI 1.67–7.50) given when condoms were less frequently used.

Table 3.
Multiple logistic regression analysis of variables associated with new STI cases in FSWs.
4. Discussion
Data on the epidemiology of STIs among high-risk behavior groups, including FSWs, are limited in Bangladesh. In the majority of research on FSWs in Bangladesh, diagnostic facilities, limitation of resources, stigma, and discrimination associated with STIs, lack of coordination between service providers, and poor attendance of STI patients at public clinics are some of the main reasons for lack of STI data [23].
The sociodemographic profile of FSWs in the current study is similar to the previous report among brothel-based sex workers in Bangladesh [23]. Approximately one-third of the brothel-based sex workers surveyed were married, while few numbers of respondents were unmarried (meaning sex workers who were never married), while there was a high number of respondents who were living as separated (i.e., legally married but does not live together with their partner as a married couple). It is interesting to note that living separately was previously found to be a risk factor for STIs [15,24]. However, in our research, we found that the married FSWs were more sexually active and they had a greater number of new STI cases. The reason for this increase in STI cases may be due to a lack of health literacy and not taking necessary preventive measures during intercourse. Studies have found that Bangladeshi women have been documented to be vulnerable to STIs, including HIV/AIDS, and their knowledge about different diseases is reported to be poor [14]. Further, 40% of ever-married women had never heard of HIV/AIDS, 19% had heard but did not know how to prevent it, and only 41% knew how to prevent disease transmission [25]. In addition, findings have been consistent with previous studies [26] suggesting that the majority of women clients were illiterate, leading to challenges for the use of the information being disseminated through the DIC locations. Thus, the concept of health literacy is more evident from the fact that previous studies focused more on the provider’s point of view, which has shown there may remain differences from the way laypeople and health professionals understand and defined health [27]. Therefore, a set of stereotyped “do’s” and “don’ts” for health care delivery and health literacy (e.g., in terms of medication management, infection treatment, diagnostics, etc.) can often cause the consumers or patients to be defined by a fixed set of ethnic or cultural attributes [28]. For example, in certain situations, learning about a particular community can be helpful (such as ethnic background, social, professional, and religious beliefs), but when broadly applied, this approach can lead to stereotyping and oversimplification of culture [28]. As a consequence, it gets reflective of particular stigmatized and minority groups like FSWs as not being able to comprehend most of the health information which may cause them to engage in risky sexual practice behaviors. Therefore, more work can be done to include cultural competence into health service delivery policy as an important goal for the FSW minority group populations, funding regular staff training programs, offering patient navigators, expanding its relationships with community groups, and creating an environment that acknowledges diversity (e.g., language capacity, how to address sexual orientation, etc.) [29].
Studies have found that prevention and control of STIs can be important in reducing the incidence of HIV infection [15]. For example, the relative risk of genital ulcer disease (e.g., chancroid, herpes simplex, and syphilis) for the transmission of HIV is greater, while the population attributable risk of cervical infection is also a concern due to high prevalence, leading to an increased risk of HIV transmission [30]. We found that consistency in condom use during intercourse was low among FSWs and there was a significant association with new STI cases, which can be a concern for HIV infection as well. While the previous study mentioned that 19% and 18% of the FSWs in a brothel in central Bangladesh were positive for gonorrhea and chlamydia, respectively, but lower than the reported STIs among hotel-based FSWs in Dhaka, Bangladesh [2,15]. On a contrary, our study did not specifically identify the nature of the STI illness cases, but the STI symptoms for vaginal discharge were high and it was observed that hotel-based working locations had the highest number of new STI cases. While this could also be from the fact that clients who are in hotel-based locations may prefer to have unprotected sex and the FSWs who may not have a choice to refuse service, may have a risk of new STI cases [2,8,23]. Consequently, as a result of low condom use, poor negotiation skills for condom use with their clients, FSWs often get infected by clients and transmit the infection to new clients [15]. Although 80% of the sex workers in Bangladesh mentioned that condoms were used in their last sex [5], our study varies where only 13% of respondents reported that clients “always” used condoms during intercourse. This difference may be the result of self-reporting error or lack of exposure to a proper condom promotion intervention program (new STI and HIV intervention programs are being introduced in brothels after the behavioral surveillance survey in 2002) [5]. Further, there is now considerable evidence that the presence of bacterial vaginosis has a role in the acquisition of HIV [31]. Therefore, this study finding does warrant further exploratory studies to gain more comprehensive learning about social networks, social cohesion, and the risk-taking behaviors of FSW for their clients.
Besides, it was relevant to mention that alcohol intake and drug dependency were significantly associated with new STI illness cases. Studies have found that many women as sex workers recalled their initiation to alcohol use as ‘‘normal’’—using alcohol with friends, in response to peer pressure, or simply as part of maturing in the culture [32]. Further, the extant literature on sex workers globally has highlighted on FSW adverse social contexts that also includes alcohol use as one of the contributing factors towards STI and HIV risk [33,34]. Likewise, our study found that FSWs reported alcohol intake as a risky behavior towards new STI cases. Women often described using alcohol as a disinhibitory factor before their involvement in sexual risk behaviors [33]. Therefore, such behaviors of FSWs may explain the nature of why our study had an association with new STI cases, as oftentimes poverty, stigma, violence, sexual risk, and alcohol use shape their overall risky behaviors. These behaviors also further diminish women’s ability to put protective behaviors in place [33]. As a consequence, alcohol abuse becomes a strong predictor for the dependent variable of new STI cases. Further, recent studies in other settings have uncovered a high degree of overlap between sex work and drug use (e.g., injection drug use and having drug dependency) [35]. High HIV prevalence among FSWs who inject drugs or have unprotected sex with male injection drug users has also been associated with rapid HIV/sexually transmitted disease transmission [36]. Likewise, given the importance and strong future intervention prospects for health promotion and prevention of STI illness, our study found drug dependency to be strongly associated with new STI cases, which does indicate this variable to be a predictor for new STI cases as well. Understanding the sequence of drug use and sex work may suggest interventions to increase safer sex in this vulnerable population. For example, research has demonstrated that in the United States and Canada, FSWs often engaged in sex work to support their drug habits [37]. Therefore, it is important to initially consider the issues of drug dependency among FSWs in Bangladesh, which would allow STI service organizations to also focus on rehabilitation options for this target population. Therefore, we recommend that STI management services should strengthen behavior change communication (BCC) components or focus on information, education, and communication (IEC) resources to increase health literacy and STI awareness among FSWs. Additionally, as consistent condom use among FSWs remains low, counseling sessions should be an essential priority and focus on any harm reduction strategies. Hence, there is a need for adequate hiring and training facilities for human resources to ensure these services are effectively met.
In terms of limitations, our study was conducted among FSWs in Dhaka who are receiving services from DICs through a nonrandom sampling procedure for enrollment into the prevention and treatment program. Therefore, the data generated from this study may not be generalized to all FSWs but they provide an insight into the risk of STIs in FSWs who are receiving services. Furthermore, our study did not explore clients’ behaviors or structural factors that are known to enhance STI/HIV vulnerability. Notwithstanding the strengths of this study includes an understanding of the age-specific new case of STI, working locations for FSW and its relationship with an increased number of STI cases, while we also found that inconsistent condom use, alcohol intake, and drug dependency are all significantly related to a new STI case. This provides an important opportunity for realizing how to improve health promotion, health literacy, and STI prevention interventions in earnest for FSW communities in Bangladesh.
5. Conclusions
There remains an increasing demand for providing a more FSW-oriented service platform by integrating these aforementioned findings in urban and rural locations in Bangladesh. While there also remains a sense of vulnerability, lack of confidence in service providers, fear of disclosing health information, lack of awareness on the preventive measures and social norms, and traditional misconceptions on sexual health issues by these FSW populations. Hence, there should be a growing need to build community capacity and empower women in terms of improved sexual health promotion activities. In addition, research should address the current conceptions of illness stigma to develop interventions and policies that will address this formidable barrier to sexual care. Differences in risk patterns and tailoring intervention, that would allow improved health literacy, increased contraception use, and lower STI cases, should be a primary concern in FSW health intervention, and towards their quality of life.
Author Contributions
All authors made a substantive contribution to this study. Conceptualization, T.J.F.; methodology, T.J.F., M.D.H.H., Y.T.J., M.H.N., A.A.C.; software, T.J.F. and Y.T.J.; formal analysis, T.J.F., Y.T.J., M.H.N.; investigation, T.J.F.; data curation, T.J.F., and Y.T.J.; writing—original draft preparation, T.J.F., and Y.T.J.; writing—review and editing, T.J.F., Y.T.J., A.A.C., M.H.N., M.D.H.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study received ethics approval (2019/OR-NSU/IRB-No.0795) from the Institutional Review Board/Ethical Review Committee (IRB/ERC) of North South University, Bangladesh prior to any data collection.
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
Restrictions apply to the availability of these data. Data was obtained from Lighthouse Bangladesh and are available upon request to the authors and with the permission of Lighthouse Bangladesh.
Acknowledgments
We would like to acknowledge Lighthouse Bangladesh for their administrative and technical support in the data collection process.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kaida, A.; Dietrich, J.J.; Laher, F.; Beksinska, M.E.; Jaggernath, M.; Bardsley, M.; Smith, P.; Cotton, L.; Chitneni, P.; Closson, K.; et al. A high burden of asymptomatic genital tract infections undermines the syndromic management approach among adolescents and young adults in South Africa: Implications for HIV prevention efforts. BMC Infect. Dis. 2018, 18, 499. [Google Scholar] [CrossRef] [PubMed]
- Nessa, K.; Waris, S.-A.; Sultan, Z.; Monira, S.; Hossain, M.; Nahar, S.; Rahman, H.; Alam, M.; Baatsen, P.; Rahman, M. Epidemiology and Etiology of Sexually Transmitted Infection among Hotel-Based Sex Workers in Dhaka, Bangladesh. J. Clin. Microbiol. 2004, 42, 618–621. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Workowski, K.A.; Bolan, G.A. Sexually transmitted diseases treatment guidelines 2015. MMWR Recomm. Rep. 2015, 64, 1–37. [Google Scholar] [PubMed]
- Unemo, M.; Bradshaw, C.S.; Hocking, J.S.; De Vries, H.J.C.; Francis, S.C.; Mabey, D.; Marrazzo, J.M.; Sonder, G.J.B.; Schwebke, J.R.; Hoornenborg, E.; et al. Sexually transmitted infections: Challenges ahead. Lancet Infect. Dis. 2017, 17, e235–e279. [Google Scholar] [CrossRef]
- Bangladesh National AIDS/STD Programme (NASP). 4th National Strategic Plan for HIV and AIDS Response 2018–2022; Ministry of Health and Family Welfare Government of the People’s Republic of Bangladesh: Dhaka, Bangladesh, 2018; pp. 1–61. [Google Scholar]
- World Health Organisation (WHO). WHO Guidelines for the Treatment of Treponema pallidum (Syphilis); WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Newman, L.M.; Rowley, J.T.; Hoorn, S.V.; Wijesooriya, N.S.; Unemo, M.; Low, N.; Stevens, G.; Gottlieb, S.L.; Kiarie, J.; Temmerman, M. Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting. PLoS ONE 2015, 10, e0143304. [Google Scholar] [CrossRef]
- Azim, T.; Khan, S.I.; Haseen, F.; Huq, N.L.; Hening, L.; Pervez, M.; Chowdhury, M.E.; Sarafian, I. HIV and AIDS in Bangladesh. J. Health Popul. Nutr. 2008, 26, 311–324. [Google Scholar] [CrossRef]
- Francis, S.C.; Mthiyane, T.N.; Baisley, K.; Mchunu, S.L.; Ferguson, J.B.; Smit, T.; Crucitti, T.; Gareta, D.; Dlamini, S.; Mutevedzi, T.; et al. Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site. PLoS Med. 2018, 15, e1002512. [Google Scholar] [CrossRef]
- Adler, M.W. Sexually transmitted diseases control in developing countries. Sex. Transm. Infect. 1996, 72, 83–88. [Google Scholar] [CrossRef][Green Version]
- National Institute of Population Research and Training (NIPORT); Mitra and Associates; ICF International. Bangladesh Demografic and Health Survey 2014; NIPOT: Dhaka, Bangladesh; Mitra and Associates: Dhaka, Bangladesh; ICF International: Rockville, MD, USA, 2016. [Google Scholar]
- National Institute of Population Research and Training (NIPORT); Mitra and Associates; ICF International. Bangladesh Demographic and Health Survey 2011; NIPOT: Dhaka, Bangladesh; Mitra and Associates: Dhaka, Bangladesh; ICF International: Calverton, MD, USA, 2013. [Google Scholar]
- World Health Organisation (WHO). The Second Decade Improving Adolescent Health and Development; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Chowdhuri, S. Reproductive tract infections and sexually transmitted infections of women in Bangladesh. James P Grant Sch. Public Health BRAC Univ. 2007, 8, 1–6. [Google Scholar]
- Nessa, K.; Waris, S.A.; Alam, A.; Huq, M.; Nahar, S.; Chawdhury, F.A.H.; Monira, S.; Badal, M.U.; Sultana, J.; Mahmud, K.F.; et al. Sexually Transmitted Infections Among Brothel-Based Sex Workers in Bangladesh: High Prevalence of Asymptomatic Infection. Sex. Transm. Dis. 2005, 32, 13–19. [Google Scholar] [CrossRef]
- Katz, K.; McDowell, M.; Green, M.; Jahan, S.; Johnson, L.R.; Chen, M. Understanding the Broader Sexual and Reproductive Health Needs of Female Sex Workers in Dhaka, Bangladesh. Int. Perspect. Sex. Reprod. Health 2015, 41, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Manopaiboon, C.; Prybylski, D.; Subhachaturas, W.; Tanpradech, S.; Suksripanich, O.; Siangphoe, U.; Johnston, L.G.; Akarasewi, P.; Anand, A.; Fox, K.K.; et al. Unexpectedly high HIV prevalence among female sex workers in Bangkok, Thailand in a respondent-driven sampling survey. Int. J. STD AIDS 2013, 24, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Gibney, L.; Choudhury, P.; Khawaja, Z.; Sarker, M.; Vermund, S.H. Behavioural risk factors for HIV/AIDS in a low-HIV prevalence Muslim nation: Bangladesh. Int. J. STD AIDS 1999, 10, 184–194. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services; Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2017; Division of STD Prevention: Atlanta, GA, USA, 2018. [Google Scholar]
- Khanam, R.; Reza, M.; Ahmed, D.; Rahman, M.; Alam, M.S.; Sultana, S.; Alam, A.; Khan, S.I.; Mayer, K.H.; Azim, T. Sexually Transmitted Infections and Associated Risk Factors Among Street-Based and Residence-Based Female Sex Workers in Dhaka, Bangladesh. Sex. Transm. Dis. 2017, 44, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Khatun, F.; Heywood, A.E.; Hanifi, S.M.A.; Rahman, M.S.; Ray, P.K.; Liaw, S.T.; Bhuiya, A. Gender differentials in readiness and use of mHealth services in a rural area of Bangladesh. BMC Health Serv. Res. 2017, 17, 573. [Google Scholar] [CrossRef]
- Sullivan, K.M.; Soe, M.M. Documentation for Sample Size for a Cross-Sectional, Cohort, or Clinical Trial Studies. Available online: https://www.openepi.com/PDFDocs/SSCohortDoc.pdf (accessed on 5 October 2020).
- Jenkins, C.; Rahman, H. Rapidly changing conditions in the brothels of Bangladesh: Impact on HIV/STD. AIDS Educ. Prev. 2002, 14, 97–106. [Google Scholar] [CrossRef]
- Bogaerts, J.; Ahmed, J.; Akhter, N.; Begum, N.; Rahman, M.; Nahar, S.; Van Ranst, M.; Verhaegen, J. Sexually transmitted infections among married women in Dhaka, Bangladesh: Unexpected high prevalence of herpes simplex type 2 infection. Sex. Transm. Infect. 2001, 77, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Khanam, P.A.; e Khuda, B.; Khane, T.T.; Ashraf, A. Awareness of sexually transmitted disease among women and service providers in rural Bangladesh. Int. J. STD AIDS 1997, 8, 688–696. [Google Scholar] [CrossRef]
- Hoque, R.; Mazmum, F.A.; Bao, Y. e-Health in Bangladesh: Current Status, Challenges, and Future Direction. Int. Technol. Manag. Rev. 2014, 4, 87–96. [Google Scholar] [CrossRef]
- McClean, S.; Shaw, A. From Schism to Continuum? The Problematic Relationship Between Expert and Lay Knowledge—An Exploratory Conceptual Synthesis of Two Qualitative Studies. Qual. Health Res. 2005, 15, 729–749. [Google Scholar] [CrossRef]
- Betancourt, J.R. Cultural Competence—Marginal or Mainstream Movement? New Engl. J. Med. 2004, 351, 953–955. [Google Scholar] [CrossRef] [PubMed]
- Jahangir, Y.; Meyer, S.B. Understanding Access to and Utilisation of Sexual Health Services by South Asian Immigrant Men in Western Countries: A Scoping Review. J. Immigr. Minor. Heal. 2020, 22, 621–633. [Google Scholar] [CrossRef] [PubMed]
- Laga, M. STD control for HIV prevention—it works! Lancet 1995, 346, 518–519. [Google Scholar] [CrossRef]
- Schmid, G.; Markowitz, L.; Joesoef, R.; Koumans, E. Bacterial vaginosis and HIV infection. Sex. Transm. Infect. 2000, 76, 3–4. [Google Scholar] [CrossRef]
- Witte, S.S.; Batsukh, A.; Chang, M. Sexual Risk Behaviors, Alcohol Abuse, and Intimate Partner Violence Among Sex Workers in Mongolia: Implications for HIV Prevention Intervention Development. J. Prev. Interv. Community 2010, 38, 89–103. [Google Scholar] [CrossRef]
- Côté, A.-M.; Sobela, F.; Dzokoto, A.; Nzambi, K.; Asamoah-Adu, C.; Labbé, A.-C.; Mâsse, B.; Mensah, J.; Frost, E.; Pépin, J. Transactional sex is the driving force in the dynamics of HIV in Accra, Ghana. AIDS 2004, 18, 917–925. [Google Scholar] [CrossRef]
- Wechsberg, W.M.; Luseno, W.K.; Lam, W.K. Violence against substance-abusing South African sex workers: Intersection with culture and HIV risk. AIDS Care 2005, 17, 55–64. [Google Scholar] [CrossRef]
- Arora, P.; Cyriac, A.; Jha, P. India’s HIV-1 epidemic. CMAJ 2004, 171, 1337–1338. [Google Scholar] [CrossRef]
- Benotsch, E.G.; Somlai, A.M.; Pinkerton, S.D.; Kelly, J.A.; Ostrovski, D.; Gore-Felton, C.; Kozlov, A.P. Drug use and sexual risk behaviours among female Russian IDUs who exchange sex for money or drugs. Int. J. STD AIDS 2004, 15, 343–347. [Google Scholar] [CrossRef]
- Haley, N.; Roy, E.; Leclerc, P.; Boudreau, J.-F.; Boivin, J.-F. HIV risk profile of male street youth involved in survival sex. Sex. Transm. Infect. 2004, 80, 526–530. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).