Functional Outcomes After Imaging- and Orthopedic Test-Guided Evaluation of Shoulder Disorders: Systematic Review and Meta-Analysis
Abstract
1. Introduction
1.1. Purpose
1.2. Hypothesis
2. Materials and Methods
2.1. Study Design
- Population: Adults with shoulder pain due to soft tissue injuries (e.g., rotator cuff tears and subacromial impingement).
- Intervention: Diagnostic approach using either orthopedic tests or imaging modalities.
- Comparison: Pre- vs. post-intervention measurements, or between different diagnostic strategies.
- Outcome: Functional clinical improvement, measured through validated quantitative scales.
2.2. Eligibility Criteria
- Population: Adults aged 18 or older with or without clinical diagnosis of soft tissue shoulder disorders (e.g., rotator cuff tears, subacromial impingement, and tendinopathy).
- Study design: Controlled clinical studies (randomized or non-randomized) including at least two comparison groups (e.g., symptomatic vs. asymptomatic, pre- vs. post-intervention).
- Interventions: Studies evaluating either (a) imaging-based assessment strategies (MSK ultrasound, MRI, or radiography) or (b) orthopedic physical examination tests (e.g., Neer, Hawkins, and Jobe).
- Outcomes: Studies must report at least one of the functional outcome scores (ASES, CMS, SST, VAS, and WOSI) or other quantitative measures suitable for standardized mean difference (SMD) calculation.
- Accessibility: Only full-text, peer-reviewed, open access articles published in English or Spanish were included.
- Exclusion criteria:
- Case reports, reviews, editorials, conference abstracts, or animal studies.
- Studies evaluating only surgical techniques or therapeutic interventions without a pre–post functional assessment component.
2.3. Information Sources and Search Strategy
- Anatomical regions (e.g., shoulder and glenohumeral joint);
- Target conditions (e.g., rotator cuff injuries and impingement syndromes);
- Diagnostic tools (e.g., orthopedic physical examination tests and imaging modalities);
- Functional outcome measures (e.g., validated clinical scores and quantitative scales).
- Anatomical region: “Shoulder” and “Glenohumeral joint”;
- Target conditions: “Rotator cuff tear”, “Rotator cuff tendinopathy”, “Shoulder impingement syndrome”, “Subacromial syndrome”, and “Biceps tendinitis”;
- Diagnostic tools: “Physical examination”, “Orthopedic test”, “Special test”, “Clinical assessment”, “Jobe”, “Hawkins”, “Neer”, and “Speed test”;
- Imaging modalities: “Musculoskeletal ultrasound”, “Ultrasonography”, “Magnetic resonance imaging”, “MRI”, and “Radiography”;
- Outcomes: Although the search strategy included terms such as “Sensitivity”, “Specificity”, “Accuracy”, and “Likelihood ratio” to ensure broad coverage of diagnostic literature, only studies reporting functional outcomes through validated clinical scales—such as “ASES”, “CMS”, “VAS”, “SST”, or “WOSI”—were ultimately included in the meta-analysis.
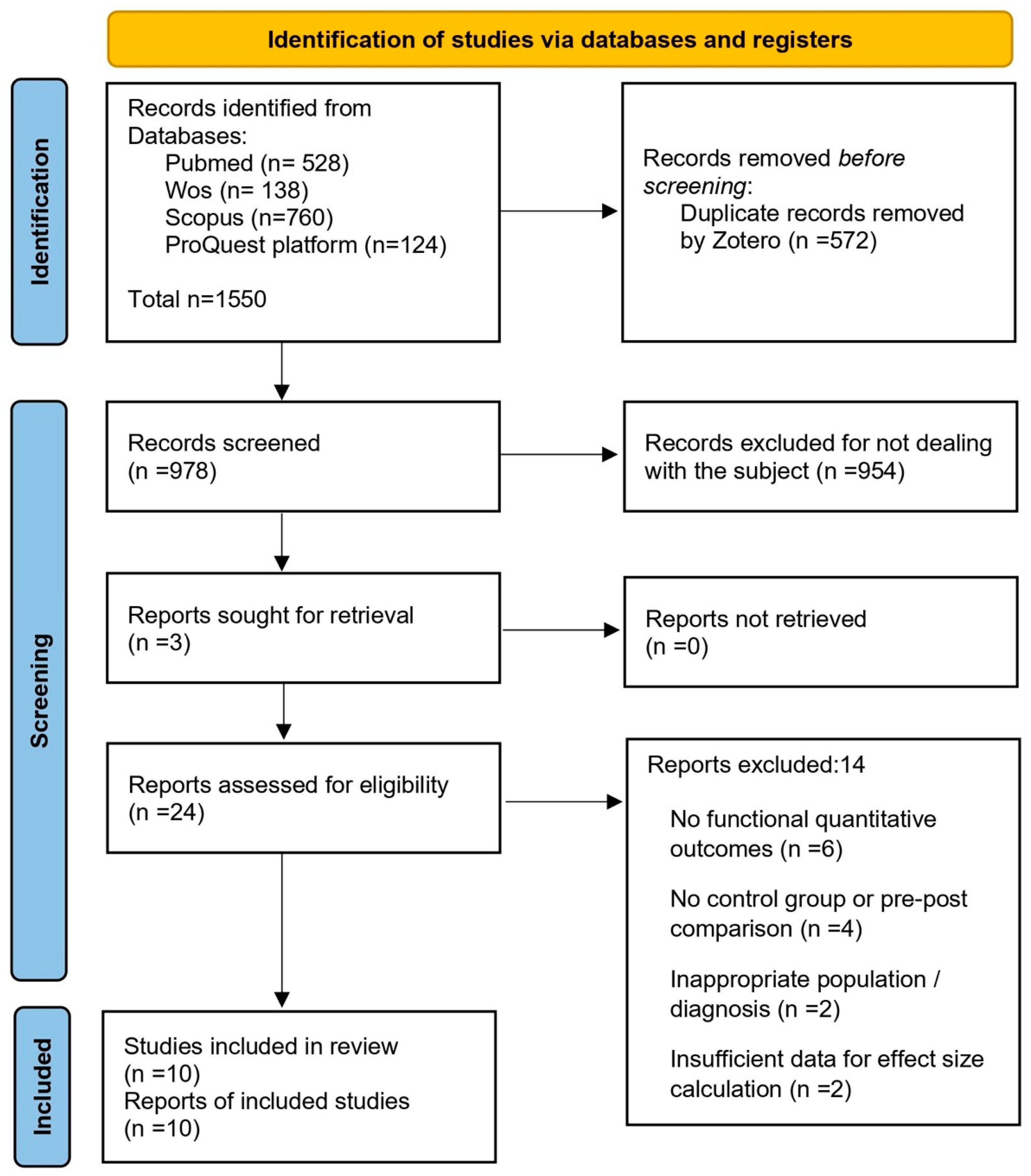
2.4. Study Selection
2.5. Data Extraction
- Study identifiers (authors, year, and country);
- Population characteristics (sample size, age, and sex);
- Assessment tool evaluated (imaging or orthopedic test);
- Target pathology;
- Outcome measures related to functional improvement (e.g., validated clinical scales or quantitative scores);
- Functional scores (ASES, CMS, SST, VAS, etc.);
- Pre- and post-intervention values, when applicable.
2.6. Data Synthesis and Statistical Analysis
3. Results
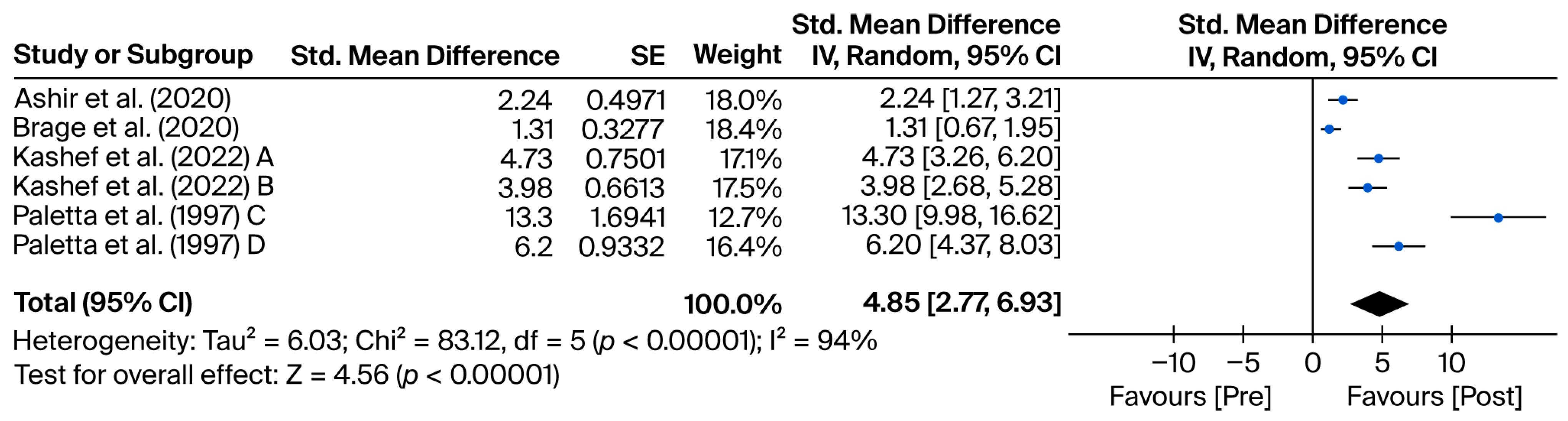
3.1. Diagnostic Tests
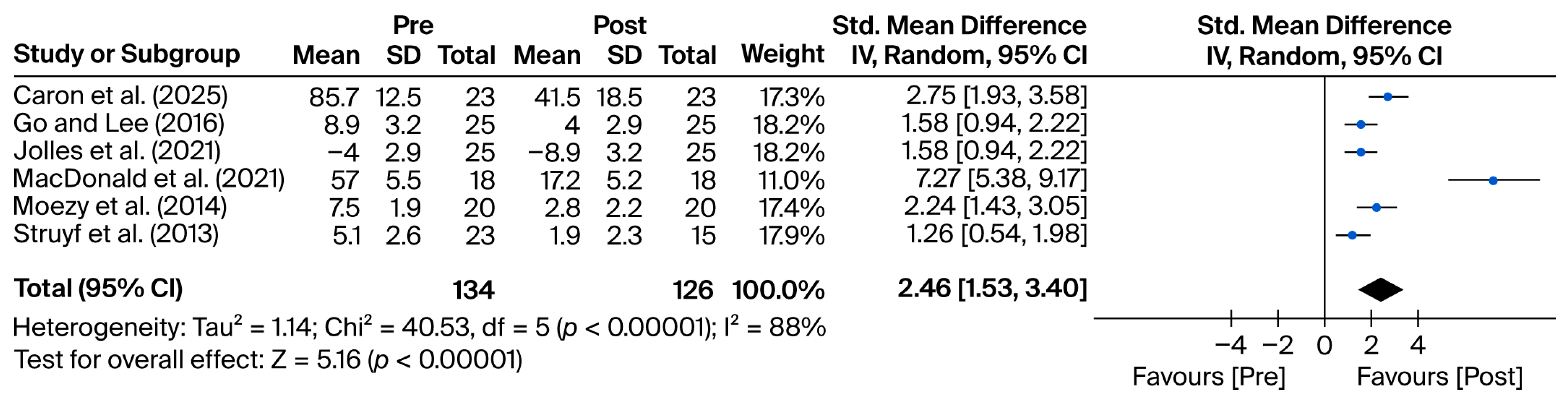
3.2. Orthopedic Tests
4. Discussion
4.1. Summary of Main Findings
4.2. Comparison with Previous Studies
4.2.1. Imaging Techniques
4.2.2. Discussion of Orthopedic Tests
4.3. Clinical Implications
4.4. Integration with Current Clinical Guidelines
4.5. Strengths and Limitations of the Study
4.6. Future Research and Clinical Conclusions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Requejo-Salinas, N.; Lewis, J.; Michener, L.A.; La Touche, R.; Fernández-Matías, R.; Tercero-Lucas, J.; Camargo, P.R.; Bateman, M.; Struyf, F.; Roy, J.-S.; et al. International physical therapists consensus on clinical descriptors for diagnosing rotator cuff related shoulder pain: A Delphi study. Braz. J. Phys. Ther. 2022, 26, 100395. [Google Scholar] [CrossRef]
- Hegedus, E.J.; Goode, A.; Campbell, S.; Morin, A.; Tamaddoni, M.; Moorman, C.T.; Cook, C. Physical examination tests of the shoulder: A systematic review with meta-analysis of individual tests. Br. J. Sports Med. 2008, 42, 80–92. [Google Scholar] [CrossRef]
- Gismervik, S.Ø.; Drogset, J.O.; Granviken, F.; Rø, M.; Leivseth, G. Physical examination tests of the shoulder: A systematic review and meta-analysis of diagnostic test performance. BMC Musculoskelet. Disord. 2017, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, P.M.; Deeks, J.J.; Leeflang, M.M.; Takwoingi, Y.; Flemyng, E. Evaluating medical tests: Introducing the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy. Cochrane Database Syst. Rev. 2023, 2023, ED000163. [Google Scholar] [CrossRef]
- Brage, K.; Juul-Kristensen, B.; Hjarbaek, J.; Boyle, E.; Kjaer, P.; Ingwersen, K.G. Strain elastography and tendon response to an exercise program in patients with supraspinatus tendinopathy: An exploratory study. Orthop. J. Sports Med. 2020, 8, 2325967120965185. [Google Scholar] [CrossRef]
- Paletta, G.A.; Warner, J.J.P.; Warren, R.F.; Deutsch, A.; Altchek, D.W. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J. Shoulder Elbow Surg. 1997, 6, 516–527. [Google Scholar] [CrossRef]
- Kashef, M.A.; El Sayyad, M.; Ahmed, H.H. Ultrasound versus kinesiotaping in relation to scapular stabilization exercises in shoulder impingement syndrome: A randomized controlled trial. Egypt. J. Phys. Ther. 2024, 19, 18–25. [Google Scholar] [CrossRef]
- Ashir, A.; Ma, Y.; Jerban, S.; Jang, H.; Wei, Z.; Le, N.; Du, J.; Chang, E.Y. Rotator Cuff Tendon Assessment in Symptomatic and Control Groups Using Quantitative MRI. J. Magn. Reson. Imaging 2020, 52, 864–872. [Google Scholar] [CrossRef]
- MacDonald, P.; McRae, S.; Old, J.; Marsh, J.; Dubberley, J.; Stranges, G.; Koenig, J.; Leiter, J.; Mascarenhas, R.; Prabhakar, S.; et al. Arthroscopic Bankart repair with and without arthroscopic infraspinatus remplissage in anterior shoulder instability with a Hill-Sachs defect: A randomized controlled trial. J. Shoulder Elbow Surg. 2021, 30, 1288–1298. [Google Scholar] [CrossRef]
- Caron, J.; Walsh, K.; Zhang, T.; AlAhmed, R.; MacDonald, P.B.; Bassi, C.; Pollock, J.W.; McIlquham, K.; Lapner, P. Approach to shoulder instability: A randomized, controlled trial. JSES Int. 2025, 9, 290–295. [Google Scholar] [CrossRef]
- Moezy, A.; Sepehrifar, S.; Dodaran, M.S. The effects of scapular stabilization based exercise therapy on pain, posture, flexibility and shoulder mobility in patients with shoulder impingement syndrome: A controlled randomized clinical trial. Med. J. Islam. Repub. Iran 2014, 28, 87. [Google Scholar]
- Jolles, B.M.; Duc, C.; Coley, B.; Aminian, K.; Pichonnaz, C.; Bassin, J.-P.; Farron, A. Objective evaluation of shoulder function using body-fixed sensors: A new way to detect early treatment failures? J. Shoulder Elbow Surg. 2011, 20, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Struyf, F.; Nijs, J.; Mollekens, S.; Jeurissen, I.; Truijen, S.; Mottram, S.; Meeusen, R. Scapular-focused treatment in patients with shoulder impingement syndrome: A randomized clinical trial. Clin. Rheumatol. 2013, 32, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Go, S.-U.; Lee, B.-H. Effects of scapular stability exercise on shoulder stability and rehabilitative ultrasound images in office workers. J. Phys. Ther. Sci. 2016, 28, 2999–3002. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.; Van Doorn, P.; Hegedus, E.; Lewis, J.; Van Der Windt, D. A systematic review of the global prevalence and incidence of shoulder pain. BMC Musculoskelet. Disord. 2022, 23, 1073. [Google Scholar] [CrossRef]
- Manoso-Hernando, D.; Bailón-Cerezo, J.; Angulo-Díaz-Parreño, S.; Reina-Varona, Á.; Elizagaray-García, I.; Gil-Martínez, A. Shoulder mobility and strength impairments in patients with rotator cuff related shoulder pain: A systematic review and meta analysis. PeerJ 2024, 12, e17604. [Google Scholar] [CrossRef]
- Zhao, Q.; Palani, P.; Kassab, N.S.; Terzic, M.; Olejnik, M.; Wang, S.; Tomassini-Lopez, Y.; Dean, C.; Shellenberger, R.A. Evidence-based approach to the shoulder examination for subacromial bursitis and rotator cuff tears: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2024, 25, 1028. [Google Scholar] [CrossRef]
- Ibounig, T.; Rämö, L.; Haas, R.; Jones, M.; Järvinen, T.L.N.; Taimela, S.; Docking, S.; Sanders, S.; Buchbinder, R. Imaging abnormalities of the acromioclavicular joint and subacromial space are common in asymptomatic shoulders: A systematic review. J. Orthop. Surg. 2025, 20, 7. [Google Scholar] [CrossRef]
- Roy, J.-S.; Braën, C.; Leblond, J.; Desmeules, F.; Dionne, C.E.; MacDermid, J.C.; Bureau, N.J.; Frémont, P. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1316–1328. [Google Scholar] [CrossRef]
- Kelley, M.J.; Shaffer, M.A.; Kuhn, J.E.; Michener, L.A.; Seitz, A.L.; Uhl, T.L.; Godges, J.J.; McClure, P. Shoulder Pain and Mobility Deficits: Adhesive Capsulitis: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health From the Orthopaedic Section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2013, 43, A1–A31. [Google Scholar] [CrossRef]
- Hurd, J.L.; Facile, T.R.; Weiss, J.; Hayes, M.; Hayes, M.; Furia, J.P.; Maffulli, N.; Winnier, G.E.; Alt, C.; Schmitz, C.; et al. Safety and efficacy of treating symptomatic, partial-thickness rotator cuff tears with fresh, uncultured, unmodified, autologous adipose-derived regenerative cells (UA-ADRCs) isolated at the point of care: A prospective, randomized, controlled first-in-human pilot study. J. Orthop. Surg. 2020, 15, 122. [Google Scholar] [CrossRef]
- López-Millán, J.M.; Ruiz Iban, M.Á.; Díaz Heredia, J.; Roca Ruiz, L.J. Preoperative management of patients with chronic moderate to severe shoulder pain to improve postoperative outcomes: A systematic review. Pain Med. 2025, 26, 299–320. [Google Scholar] [CrossRef] [PubMed]
- Van Doorn, P.F.; De Schepper, E.I.T.; Rozendaal, R.M.; Ottenheijm, R.P.G.; Van Der Lei, J.; Bindels, P.J.; Schiphof, D. The incidence and management of shoulder complaints in general practice: A retrospective cohort study. Fam. Pract. 2021, 38, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Sconfienza, L.M.; Albano, D.; Allen, G.; Bazzocchi, A.; Bignotti, B.; Chianca, V.; Facal De Castro, F.; Drakonaki, E.E.; Gallardo, E.; Gielen, J.; et al. Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur. Radiol. 2018, 28, 5338–5351. [Google Scholar] [CrossRef] [PubMed]
- On behalf of the Ultrasound and Interventional Subcommittees of the European Society of Musculoskeletal Radiology (ESSR); Sconfienza, L.M.; Adriaensen, M.; Albano, D.; Aparisi Gómez, M.P.; Bazzocchi, A.; Beggs, I.; Bignotti, B.; Chianca, V.; Corazza, A.; et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: A Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—Part II, elbow and wrist. Eur. Radiol. 2020, 30, 2220–2230. [Google Scholar] [CrossRef]
- Piitulainen, K.; Paloneva, J.; Ylinen, J.; Kautiainen, H.; Häkkinen, A. Reliability and validity of the Finnish version of the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section. BMC Musculoskelet. Disord. 2014, 15, 272. [Google Scholar] [CrossRef]
- Nasr, A.; Pierson, C.; Tzen, Y.-T.; Khazzam, M.; Jain, N.; Lin, Y.-S. Emerging Role of Quantitative Ultrasound-Based Imaging Techniques for Characterizing Rotator Cuff Tears: A Scoping Review. Diagnostics 2023, 13, 2011. [Google Scholar] [CrossRef]
- Aldon-Villegas, R.; Ridao-Fernández, C.; Torres-Enamorado, D.; Chamorro-Moriana, G. How to Assess Shoulder Functionality: A Systematic Review of Existing Validated Outcome Measures. Diagnostics 2021, 11, 845. [Google Scholar] [CrossRef]
- Harrisson, S.A.; Myers, H.; Wynne Jones, G.; Bajpai, R.; Bratt, C.; Burton, C.; Harrison, R.; Jowett, S.; Lawton, S.A.; Saunders, B.; et al. Clinical and Cost-Effectiveness of a Personalised Guided Consultation Versus Usual Physiotherapy Care in People Presenting with Shoulder Pain: A Protocol for the Panda-S Cluster Randomised Controlled Trial and Process Evaluation. BMJ Open 2025, 15, e100501. [Google Scholar] [CrossRef]
- Antonacci, C.; Longo, U.G.; Nazarian, A.; Schena, E.; Carnevale, A. Monitoring Scapular Kinematics through Wearable Magneto-Inertial Measurement Units: State of the Art and New Frontiers. Sensors 2023, 23, 6940. [Google Scholar] [CrossRef]
| Author (Year) | Country | Design | Sample (n) | Clinical Management Context | Duration | Outcomes | Key Findings (Conclusions) |
|---|---|---|---|---|---|---|---|
| Reference [9] | Egypt | Randomized Controlled Trial (RCT) | n = 45 (15 per group) | Scapular exercises + kinesiotaping or ultrasound vs. control | 4 weeks | VAS, QuickDASH, strength, ROM | Kinesiotaping showed greater improvements in pain and function compared to ultrasound and control. |
| Reference [8] | USA | Longitudinal observational study | n = 33 (18 instability, 15 RCT) | Radiographic evaluation before and after surgical repair (capsulolabral or rotator cuff) | 2 years | Glenohumeral and scapulothoracic kinematics | Most patients showed normalized glenohumeral kinematics after surgery; scapulothoracic kinematics normalized only in the rotator cuff group. |
| Reference [10] | Pakistan | Prospective quantitative imaging study | n = 48 shoulders (24 patients) | Quantitative MRI evaluation (UTE-Cones-MT and T2 mapping) | Single session | MMF, T2, WORC, VAS | Symptomatic tendons showed lower MMF and higher T2 values compared to controls. Alterations also present in asymptomatic contralateral shoulders. |
| Reference [7] | Spain | Prospective cohort study | n = 23 | 12-week exercise program for supraspinatus tendinopathy | 12 weeks | Strain elastography (RAW, DELT), DASH, VAS, tendon thickness, MRI | Improvements in pain and function (DASH, VAS); no structural changes observed on ultrasound or MRI. |
| Reference [15] | Belgium | Randomized Clinical Trial (RCT) | n = 46 (23 experimental, 23 control) | Scapula-focused treatment (education + scapular control exercises + manual therapy) vs. conventional treatment (mobility and strengthening exercises) | 6 weeks | SPADI, pain (VAS), rotator strength, functional tests | The scapular group showed significantly greater improvements in pain, function, and SPADI compared to the control group after 6 weeks of treatment. |
| Reference [13] | Iran | Randomized Clinical Trial (RCT) | n = 68 (34 experimental, 34 control) | Scapular stabilization exercises vs. conventional exercises for subacromial impingement | 12 weeks | VAS, abduction, external rotation, head posture, scapular symmetry | Significant improvements in VAS, joint mobility, and posture in the experimental group compared to the control. |
| Reference [16] | South Korea | Randomized Clinical Trial (RCT) | n = 30 (15 experimental, 15 control) | Scapular stability exercises vs. standard office routine | 6 weeks | Scapular stability, ultrasound imaging, posture | Significant reduction in forward head posture and greater scapular stability in the intervention group. |
| Reference [11] | Canada | Prospective longitudinal study | n = 40 (20 per group) | Specific conservative rehabilitation | 12 months | WOSI, ASES, SST | Progressive improvements in WOSI, ASES, and SST after 12 months of intervention. |
| Reference [14] | Switzerland | Observational study | n = 65 (34 experimental, 31 control) | No specific comparative intervention | 3–12 months | ASES, SST | Increase in SST; no significant changes in ASES. |
| Reference [12] | Canada | Controlled clinical trial | n = 60 (30 per group) | Conservative treatment in patients with shoulder instability vs. control | 24 months | WOSI, ASES | Both groups improved in WOSI and ASES, with no significant differences between groups. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-de-Pereda-Notario, C.M.; Palomeque-Del-Cerro, L.; García-Mata, R.; Arráez-Aybar, L.A. Functional Outcomes After Imaging- and Orthopedic Test-Guided Evaluation of Shoulder Disorders: Systematic Review and Meta-Analysis. Methods Protoc. 2025, 8, 133. https://doi.org/10.3390/mps8060133
García-de-Pereda-Notario CM, Palomeque-Del-Cerro L, García-Mata R, Arráez-Aybar LA. Functional Outcomes After Imaging- and Orthopedic Test-Guided Evaluation of Shoulder Disorders: Systematic Review and Meta-Analysis. Methods and Protocols. 2025; 8(6):133. https://doi.org/10.3390/mps8060133
Chicago/Turabian StyleGarcía-de-Pereda-Notario, Carlos Miquel, Luis Palomeque-Del-Cerro, Ricardo García-Mata, and Luis Alfonso Arráez-Aybar. 2025. "Functional Outcomes After Imaging- and Orthopedic Test-Guided Evaluation of Shoulder Disorders: Systematic Review and Meta-Analysis" Methods and Protocols 8, no. 6: 133. https://doi.org/10.3390/mps8060133
APA StyleGarcía-de-Pereda-Notario, C. M., Palomeque-Del-Cerro, L., García-Mata, R., & Arráez-Aybar, L. A. (2025). Functional Outcomes After Imaging- and Orthopedic Test-Guided Evaluation of Shoulder Disorders: Systematic Review and Meta-Analysis. Methods and Protocols, 8(6), 133. https://doi.org/10.3390/mps8060133









