Clinical Wound Healing After Lower Third Molar Surgery with Envelope and Bayonet Flaps: A Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Inclusion Criteria
2.3. Exclusion Criteria
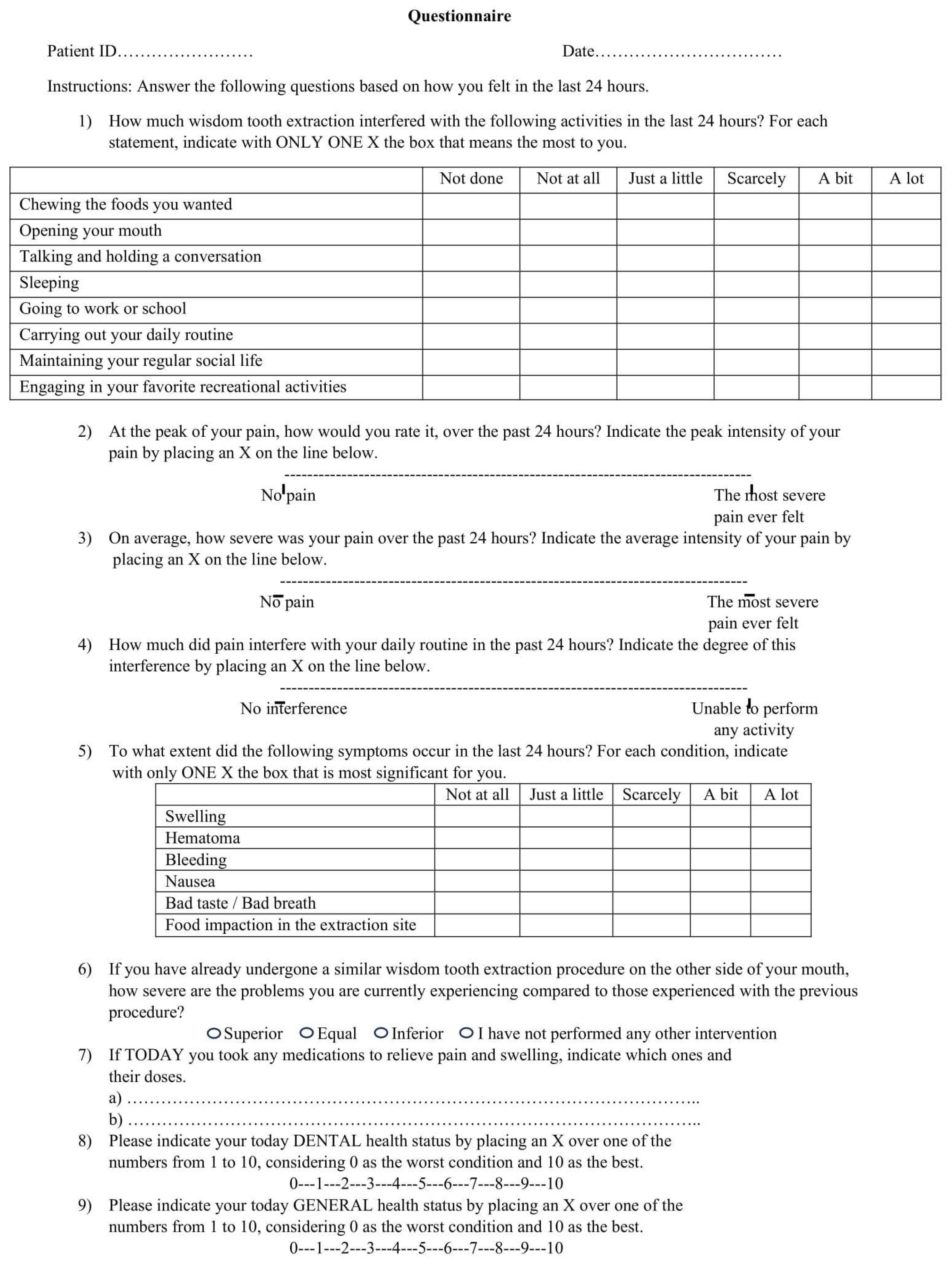
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. Descriptive Analysis
3.2. Inferential Analysis
- To assess differences in healing between the two types of flaps using the wound dehiscence as a principal parameter of healing. The null hypothesis was that the two groups could have the same proportion of post-surgical dehiscence.
- To evaluate whether the possible presence of dehiscence had any repercussions on wound healing. For each test, the null hypothesis was that there was no influence on healing.
- To investigate whether a correlation existed between clinical, anatomical and operational variables and surgical wound healing. For each test, the null hypothesis was that no influence on healing was associated with each variable.
- To find possible associations between the flap design and any changes in terms of post-surgical patient’s QOL. The null hypothesis was that there would be no differences in terms of QOL between one kind of flap and the other.
4. Discussion
4.1. Flap Design and Dehiscence
4.2. Effects of Dehiscence on Healing
4.3. Influence of Anatomical and Operative Variables on Healing
4.4. Influence of Flap Type on QOL
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blondeau, F.; Daniel, N.G. Extraction of impacted mandibular third molars: Postoperative complications and their risk factors. J. Can. Dent. Assoc. 2007, 73, 325. [Google Scholar] [PubMed]
- Colorado-Bonnin, M.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Quality of life following lower third molar removal. Int. J. Oral Maxillofac. Surg. 2006, 35, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Shugars, D.A.; Gentile, M.A.; Ahmad, N.; Stavropoulos, M.F.; Slade, G.D.; Phillips, C.; Conrad, S.M.; Fleuchaus, P.T.; White, R.P., Jr. Assessment of oral health-related quality of life before and after third molar surgery. J. Oral Maxillofac. Surg. 2006, 64, 1721–1730. [Google Scholar] [CrossRef] [PubMed]
- Şimşek Kaya, G.; Yapıcı Yavuz, G.; Saruhan, N. The influence of flap design on sequelae and quality of life following surgical removal of impacted mandibular third molars: A split-mouth randomised clinical trial. J. Oral Rehabil. 2019, 46, 828–835. [Google Scholar] [CrossRef]
- Glera-Suárez, P.; Soto-Peñaloza, D.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Patient morbidity after impacted third molar extraction with different flap designs. A systematic review and meta-analysis. Med. Oral Patol. Oral Cir. Bucal 2020, 25, e233–e239. [Google Scholar] [CrossRef]
- Pippi, R. Post-surgical clinical monitoring of soft tissue wound healing in periodontal and implant surgery. Int. J. Med. Sci. 2017, 14, 721–728. [Google Scholar] [CrossRef]
- Jakse, N.; Bankaoglu, V.; Wimmer, G.; Eskici, A.; Pertl, C. Primary wound healing after lower third molar surgery: Evaluation of 2 different flap designs. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 93, 7–12. [Google Scholar] [CrossRef]
- Burkhardt, R.; Lang, N.P. Influence of suturing on wound healing. Periodontol. 2000 2015, 68, 270–281. [Google Scholar] [CrossRef]
- Burkhardt, R.; Lang, N.P. Role of flap tension in primary wound closure of mucoperiosteal flaps: A prospective cohort study. Clin. Oral Implant. Res. 2010, 21, 10–14. [Google Scholar] [CrossRef]
- Yamano, S.; Kuo, W.P.; Sukotjo, C. Downregulated gene expression of TGF-βs in diabetic oral wound healing. J. Cranio-Maxillofac. Surg. 2013, 41, e42–e48. [Google Scholar] [CrossRef]
- Moores, J. Vitamin C: A wound healing perspective. Br. J. Community Nurs. 2013, 18 (Suppl. S6), S8–S11. [Google Scholar] [CrossRef]
- Anstead, G.M. Steroids, retinoids, and wound healing. Adv. Wound Care J. Prev. Heal 1998, 11, 277–285. [Google Scholar]
- Balaji, S.M. Tobacco smoking and surgical healing of oral tissues: A review. Indian J. Dent. Res. 2008, 19, 344–348. [Google Scholar] [CrossRef]
- Sandhu, A.; Sandhu, S.; Kaur, T. Comparison of two different flap designs in the surgical removal of bilateral impacted mandibular third molars. Int. J. Oral Maxillofac. Surg. 2010, 39, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Lodi, G.; Figini, L.; Sardella, A.; Carrassi, A.; Del Fabbro, M.; Furness, S. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst. Rev. 2012, 11, CD003811. [Google Scholar] [CrossRef] [PubMed]
- Pippi, R. Evaluation capability of surgical difficulty in the extraction of impacted mandibular third molars: A retrospective study from a post-graduate institution. Ann. Stomatol. 2014, 5, 7–14. [Google Scholar] [CrossRef]
- Quinn, J.V.; Wells, G.A. An assessment of clinical wound evaluation scales. Acad. Emerg. Med. 1998, 5, 583–586. [Google Scholar] [CrossRef]
- Pippi, R.; Santoro, M.; Cafolla, A. The use of a Chitosan-derived hemostatic agent for post-extraction bleeding control in patients on antiplatelet treatment. J. Oral Maxillofac. Surg. 2017, 75, 1118–1123. [Google Scholar] [CrossRef]
- Shugars, D.A.; Benson, K.; White, R.P., Jr.; Simpson, K.N.; Bader, J.D. Developing a measure of patient perceptions of short-term outcomes of third molar surgery. J. Oral Maxillofac. Surg. 1996, 54, 1402–1408. [Google Scholar] [CrossRef]
- Rahpeyma, A.; Khajehahmadi, S.; Ilkhani, S. Wound dehiscence after wisdom tooth removal in mandibular mesioangular class IB impactions: Triangular transposition flap versus envelope flap. J. Dent. Res. Dent. Clin. Dent. Prospect. 2015, 9, 175–180. [Google Scholar] [CrossRef]
- Zhu, J.; Yuan, X.; Yan, L.; Li, T.; Guang, M.; Zhang, Y. Comparison of postoperative outcomes between envelope and triangular flaps after mandibular third molar surgery: A systematic review and meta-analysis. J. Oral Maxillofac. Surg. 2020, 78, 515–527. [Google Scholar] [CrossRef]
- Azenha, M.R.; Kato, R.B.; Bueno, R.B.L.; Neto, P.J.O.; Ribeiro, M.C. Accidents and complications associated to third molar surgeries performed by dentistry students. Oral Maxillofac. Surg. 2014, 18, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Bailey, E.; Kashbour, W.; Shah, N.; Worthington, H.V.; Renton, T.F.; Coulthard, P. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst. Rev. 2020, 7, CD004345. [Google Scholar] [CrossRef] [PubMed]
- Baqain, Z.H.; Al-Shafii, A.; Hamdan, A.A.; Sawair, F.A. Flap design and mandibular third molar surgery: A split mouth randomized clinical study. Int. J. Oral Maxillofac. Surg. 2012, 41, 1020–1024. [Google Scholar] [CrossRef]
- Albanese, M.; Zangani, A.; Manfrin, F.; Bertossi, D.; De Manzoni, R.; Tomizioli, N.; Faccioni, P.; Pardo, A. Influence of surgical technique on post-operative complications in the extraction of the lower third molar: A retrospective study. Dent. J. 2023, 11, 238. [Google Scholar] [CrossRef]
- Azab, M.; Ibrahim, S.; Li, A.; Khosravirad, A.; Carrasco-Labra, A.; Zeng, L.; Brignardello-Petersen, R. Efficacy of secondary vs primary closure techniques for the prevention of postoperative complications after impacted mandibular third molar extractions: A systematic review update and meta-analysis. J. Am. Dent. Assoc. 2022, 153, 943–956.e48. [Google Scholar] [CrossRef]
- Mazzotti, C.; Mounssif, I.; Rendón, A.; Mele, M.; Sangiorgi, M.; Stefanini, M.; Zucchelli, G. Complications and treatment errors in root coverage procedures. Periodontol. 2000 2023, 92, 62–89. [Google Scholar] [CrossRef]
- Drumond, A.N.G.; Terra, G.R.; Rodrigues, L.C.; Glória, J.C.R.; Gonçalves, P.F.; Flecha, O.D.; Douglas-de-Oliveira, D.W. Effect of periodontal dressing on the wound healing after gingivectomy. Swiss Dent. J. 2025, 135, 201–217. [Google Scholar] [CrossRef] [PubMed]
- Engeland, C.G.; Bosch, J.A.; Cacioppo, J.T.; Marucha, P.T. Mucosal wound healing: The roles of age and sex. Arch. Surg. 2006, 141, 1193–1197; discussion 1198. [Google Scholar] [CrossRef] [PubMed]
- Renton, T.; Smeeton, N.; Mcgurk, M. Oral surgery: Factors predictive of difficulty of mandibular third molar surgery. Br. Dent. J. 2001, 190, 607–610. [Google Scholar] [CrossRef]
- Alqahtani, N.A.; Khaleelahmed, S.; Desai, F. Evaluation of two flap designs on the mandibular second molar after third molar extractions. J. Oral Maxillofac. Pathol. 2017, 21, 317–318. [Google Scholar] [CrossRef]
- Pham, T.A.V.; Nguyen, N.H. Periodontal status of the adjacent second molar after impacted mandibular third molar surgical extraction. Contemp. Clin. Dent. 2019, 10, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Cardaropoli, G.; Araújo, M.; Lindhe, J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J. Clin. Periodontol. 2003, 30, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.S. A clinical study of “dry socket”. Int. J. Oral Surg. 1982, 11, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Sharif, M.O.; Dawoud, B.E.S.; Tsichlaki, A.; Yates, J.M. Interventions for the prevention of dry socket: An evidence-based update. Br. Dent. J. 2014, 217, 27–30. [Google Scholar] [CrossRef][Green Version]
- Phillips, C.; White, R.P., Jr.; Shugars, D.A.; Zhou, X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J. Oral Maxillofac. Surg. 2003, 61, 1436–1448. [Google Scholar] [CrossRef] [PubMed]
- Kugelberg, C.F. Periodontal healing two and four years after impacted lower third molar surgery. A comparative retrospective study. Int. J. Oral Maxillofac. Surg. 1990, 19, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Pippi, R. Effectiveness of a personalized device in the evaluation of mandibular second molar periodontal healing after surgical extraction of adjacent third molar. Ann. Stomatol. 2014, 4, 218–229. [Google Scholar] [PubMed] [PubMed Central]
- Erdogan, O.; Tatlı, U.; Ustün, Y.; Damlar, I. Influence of two different flap designs on the sequelae of mandibular third molar surgery. Oral Maxillofac. Surg. 2011, 15, 147–152. [Google Scholar] [CrossRef]
- Kirk, D.G.; Liston, P.N.; Tong, D.C.; Love, R.M. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, e1–e6. [Google Scholar] [CrossRef]
- Koyuncu, B.Ö.; Cetingül, E. Short-term clinical outcomes of two different flap techniques in impacted mandibular third molar surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, e179–e184. [Google Scholar] [CrossRef]
- Ruvo, A.T.; Shugars, D.A.; White, R.P., Jr.; Phillips, C. The impact of delayed clinical healing after third molar surgery on health-related quality-of-life outcomes. J. Oral Maxillofac. Surg. 2005, 63, 929–935. [Google Scholar] [CrossRef] [PubMed]


| Variable | N (%) | ± sd | |
|---|---|---|---|
| Total patient sample | 56 (100) | ||
| Mean patient age (years) | 23.7 | 4.48 | |
| Race | Caucasian | 55 (98.21) | |
| Asian | 1 (1.79) | ||
| Gender | Females | 38 (67.86) | |
| Males | 18 (32.14) | ||
| Mean pre-operative inter-incisal high (cm) | 4.02 | ||
| Mean FMPS (%) | 29.70 | ||
| Mean local plaque index score (%) | 31 | ||
| Pre-operative symtoms | Present | 9 (16.07) | |
| Absent | 47 (83.93) | ||
| Third molar site | Left | 29 (51.79) | |
| Right | 27 (48.21) | ||
| Radiographic third molar impaction type | Osteo-mucosal | 48 (85.71) | |
| Completely osseous | 8 (14.29) | ||
| Pell&Gregory Class | I | 5 (8.93) | |
| II | 44 (78.57) | ||
| III | 7 (12.50) | ||
| Class of depth impaction | A | 7 (12.50) | |
| B | 32 (57.14) | ||
| C1 | 15 (26.79) | ||
| C2 | 2 (3.57) | ||
| Relationship with the second molar | Contiguity | 44 (78.57) | |
| Overlapping | 8 (14.29) | ||
| None | 4 (7.14) | ||
| Third molar position | Mesio-angular | 29 (51.79) | |
| Horizontal | 16 (28.57) | ||
| Disto-angular | 2 (3.57) | ||
| Vertical | 9 (16.07) | ||
| Root number for each third molar | 1 | 5 (8.93) | |
| 2 | 50 (89.29) | ||
| More than 2 | 1 (1.79) | ||
| Root morphology | Separated, slightly divergent | 38 (67.86) | |
| Separated, highly divergent | 2 (3.57) | ||
| Fused | 15 (26.79) | ||
| With apical anomalies | 1 (1.79) | ||
| Mean pre-operative probing depth at the second molar distal surface (mm) | 5 | ||
| Mean amount of adherent gingiva, buccally to the second molar (mm) | 2.5 | ||
| Pre-operative soft tissue level in relation to the CEJ | Coronal | 43 (76.79) | |
| Apical | 1 (1.79) | ||
| Normal | 12 (21.43) | ||
| Post-operative soft tissue level in relation to the CEJ | Coronal | 43 (76.79) | |
| Apical | 1 (1.79) | ||
| Normal | 12 (21.43) | ||
| Mean maximum diameter of the final bone cavity (mm) | 12 ± 2.61 | ||
| Average maximum depth of the residual bone cavity in relation to the CEJ (mm) | 9.72 | ||
| Mean surgery duration without suturing time (seconds) | 1520 | ||
| Mean suturing duration (seconds) | 481 | ||
| Dehiscence at 2 days | Present | 3 (5.36) | |
| Absent | 53 (94.64) | ||
| Dehiscence at 7 days | Present | 14 (25.00) | |
| Absent | 42 (75.00) | ||
| Dehiscence at 14 days | Present | 23 (41.07) | |
| Absent | 33 (58.93) | ||
| Facial edema at 2 days | Mild | 13 (23.21) | |
| Moderate | 31 (55.36) | ||
| Severe | 12 (21.43) | ||
| Facial edema at 7 days | Mild | 42 (75.00) | |
| Moderate | 13 (23.21) | ||
| Severe | 1 (1.79) | ||
| Facial edema at 14 days | Absent | 16 (28.57) | |
| Mild | 37 (66.07) | ||
| Moderate | 3 (5.36) | ||
| Severe | 0 (0.00) | ||
| Mean dehiscence at 2 days (mm) | 5 | 3.55 | |
| Mean dehiscence at 7 days (mm) | 3.04 | 2.33 | |
| Mean dehiscence at 14 days (mm) | 2.56 | 1.29 | |
| Mean healing index at 2 days | 6 | 1.49 | |
| Mean healing index at 7 days | 6.25 | 1.67 | |
| Mean healing index at 14 days | 7.41 | 1.47 |
| Envelope M (ds) | Bayonet M (ds) | t | p | |
|---|---|---|---|---|
| 14 days diameter | 1.26 (1.80) | 0.84 (1.18) | 1.045 | 0.300 |
| 7 days diameter | 1.00 (2.16) | 0.54 (1.29) | 0.976 | 0.333 |
| General Healing Index § | |||
|---|---|---|---|
| Flap | Dehiscence | Average | Standard deviation |
| Envelope | Absent | 1.7500 | 2.23607 |
| Present | 0.1667 | 1.80067 | |
| Total | 1.0714 | 2.17611 | |
| Bayonet | Absent | 1.9412 | 1.59963 |
| Present | 1.1818 | 1.83402 | |
| Total | 1.6429 | 1.70434 | |
| Total | Absent | 1.8485 | 1.90593 |
| Present | 0.6522 | 1.84905 | |
| Total | 1.3571 | 1.95800 | |
| F | p | |
|---|---|---|
| Flap | 1.382 | 0.245 |
| Dehiscence | 5.212 | 0.027 |
| Flap*Dehiscence | 0.645 | 0.426 |
| Maximum Diameter of Dehiscence at 7 Days | Maximum Diameter of Dehiscence at 14 Days | |||
|---|---|---|---|---|
| Healing | R | p | r | p |
| 2 days | −0.131 | 0.336 | −0.065 | 0.635 |
| 7 days | −0.259 | 0.054 | −0.218 | 0.106 |
| 14 days | −0.211 | 0.119 | −0.493 | <0.001 |
| GHI | −0.059 | 0.664 | −0.325 | 0.015 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pippi, R.; Mazzei, C.; Pietrantoni, A. Clinical Wound Healing After Lower Third Molar Surgery with Envelope and Bayonet Flaps: A Randomized Clinical Trial. Methods Protoc. 2025, 8, 101. https://doi.org/10.3390/mps8050101
Pippi R, Mazzei C, Pietrantoni A. Clinical Wound Healing After Lower Third Molar Surgery with Envelope and Bayonet Flaps: A Randomized Clinical Trial. Methods and Protocols. 2025; 8(5):101. https://doi.org/10.3390/mps8050101
Chicago/Turabian StylePippi, Roberto, Chiara Mazzei, and Alessandra Pietrantoni. 2025. "Clinical Wound Healing After Lower Third Molar Surgery with Envelope and Bayonet Flaps: A Randomized Clinical Trial" Methods and Protocols 8, no. 5: 101. https://doi.org/10.3390/mps8050101
APA StylePippi, R., Mazzei, C., & Pietrantoni, A. (2025). Clinical Wound Healing After Lower Third Molar Surgery with Envelope and Bayonet Flaps: A Randomized Clinical Trial. Methods and Protocols, 8(5), 101. https://doi.org/10.3390/mps8050101






