Protocol Study: Resistance Training Program, Nutritional, Sleep, and Screen Use Recommendations in Schoolchildren from Educational Centers in the Extreme South of Chile
Abstract
1. Introduction
- General objective
- Specific objectives (SO)
2. Materials and Methods
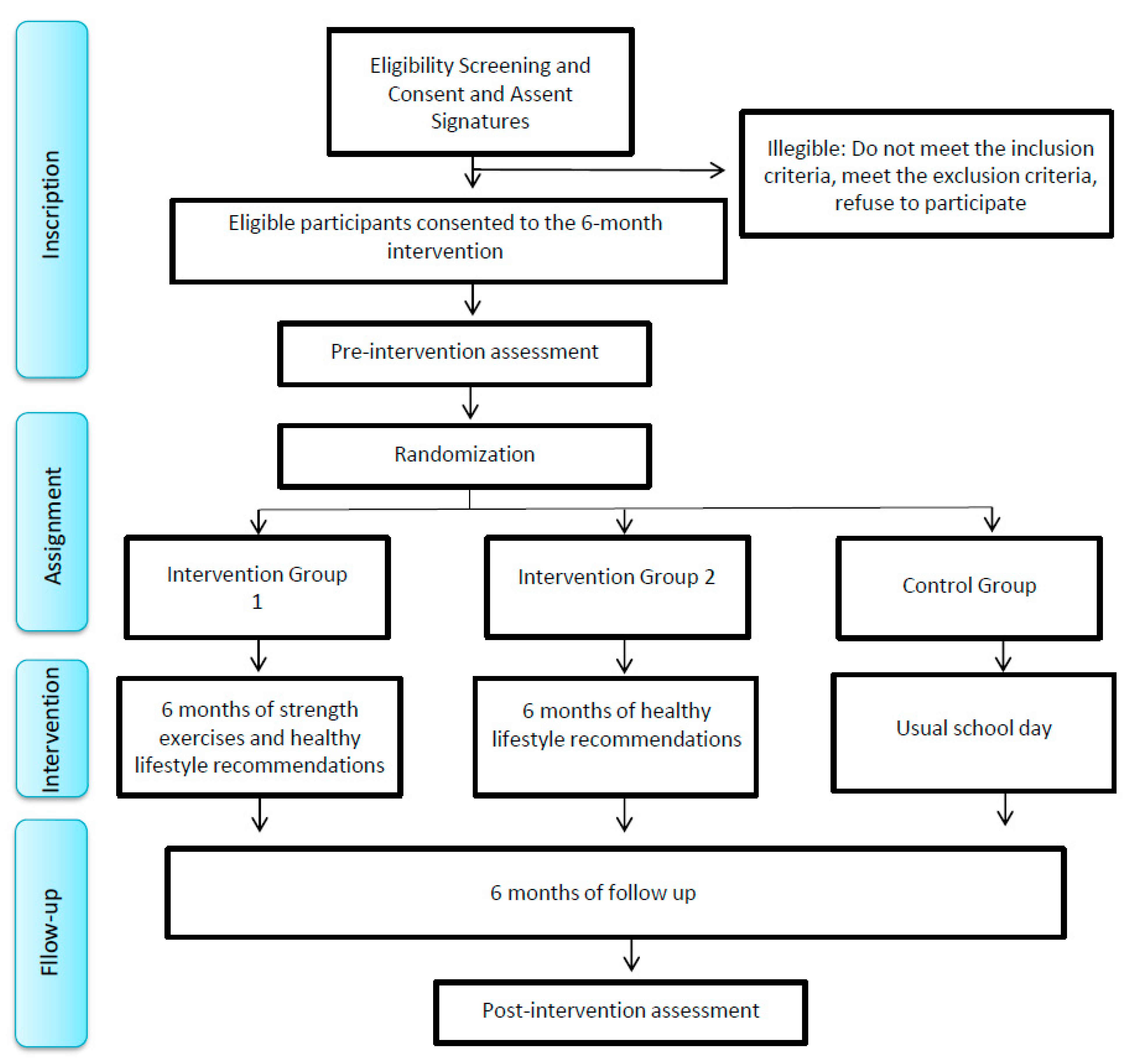
2.1. Experimental Design
2.2. Participants
2.3. Inclusion and Exclusion Criteria
3. Procedure
3.1. Training for Project Collaborators
3.2. Training for Teachers of the Educational Center
3.3. Information Collection
3.4. Randomization
3.5. Program: “Strong Schoolchildren with Healthy Lifestyle” (EF-Salud)
3.5.1. Intervention Groups
Group 1: Strength Training + Nutritional, Sleep, and Screen Use Recommendations (ST + NSSR)
- Strength exercise program
- Warm-up
- Main exercises
- −
- Elbow flexion. Main active muscle: biceps. The participants will perform 2 series of 10 repetitions with each arm.
- −
- Elbow extension. Main active muscle: triceps. The participants will perform 2 series of 10 repetitions with each arm.
- Exercise description:
- −
- Each child will perform the elbow flexion exercise in a sitting position. The elastic band (circular) will be located at one end on one foot which will hold it, while the other end of the band will be taken by hand. The exercise consists of flexing the elbow (which will be resting on the thigh) 10 times. Once the ten repetitions are finished, they will perform the same exercise with the other arm and repeat it in two series.
- −
- The elbow extension exercise will be performed with the same elastic band that was used in the previous exercise. This will be held at one end by the back of the chair and the other end of the band will be held by both hands. The exercise will be performed with the hands behind the head, extending the elbow above it and pointing toward the ceiling of the room. Two series of ten repetitions will be performed.
- −
- Flexion–extension of hip and knee (squat). Main active muscles: quadriceps and gluteus magnus. The participants will perform 2 series of 10 repetitions of sitting down and getting up from a chair.
- −
- Knee flexion. Main active muscle: biceps femoris. The participants will perform 2 series of 10 repetitions of performing a knee flexion, standing up.
- Exercise description:
- −
- The children will perform squats sitting on a chair with their feet separated between 10 and 20 cm from each other. They will stand up without help to reach the bipedal position, completing 2 series of 10 repetitions, with a 30 s break between series.
- −
- The knee flexion will be performed with a circular elastic band, standing up on the side of a chair. The children will join their extremities, aligning the knees, one against the other, and proceed to flex the knee, bringing the leg back until a 90-degree angle is achieved. This exercise will be repeated 10 times with each leg, for two series.
- Stretching
- Nutritional recommendations
- Recommendations for sleeping habits and screen use:
Group 2: Nutritional, Sleep, and Use of Screens Recommendations (NSSR)
Group 3: Control Group (CG)
3.6. Variables
3.6.1. Cardiovascular Risk
3.6.2. Physical Fitness
3.6.3. Lifestyle
3.7. Statistical Analysis
4. Expected Results
5. Discussion
- Intervention characteristics:
- Limitations and strengths:
- Impact of the intervention:
- Practical applications:
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesidad y Sobrepeso 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 20 March 2023).
- Independent Expert Group of Global Nutrition Report. Informe de la Nutrición Mundial 2021. Asociacion Civil de Centros de Estudios Sobre Nutrición Infantil. 2021. Available online: http://cesni-biblioteca.org/fuente/global-nutrition-Report/ (accessed on 20 March 2023).
- Nemet, D.; Ben-Haim, I.; Pantanowits, M.; Eliakim, A. Effects of a combined intervention for treating severely obese prepubertal children. J. Pediatr. Endocrinol. Metab. 2012, 26, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.R.; Pratt, C.A.; Hayman, L.L. Reduction of risk for cardiovascular disease in children and adolescents. Circulation 2011, 124, 1673–1686. [Google Scholar] [CrossRef] [PubMed]
- Renehan, A.G.; Tyson, M.; Egger, M.; Heller, R.F.; Zwahlen, M. Body-mass index and incidence of cancer: A systematic review and meta-analysis of prospective observational studies. Lancet 2008, 371, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Lira, M. Informe Mapa Nutricional 2021. Junta Nacional de Auxilio Escolar y Becas (JUNAEB) [Internet]. 2021. Available online: www.juaneb.cl (accessed on 20 March 2023).
- Kesztyüs, D.; Wirt, T.; Kobel, S.; Schreiber, A.; Kettner, S.; Dreyhaupt, J.; Kilian, R.; Steinacker, J.M.; The “Komm mit in das gesunde Boot-Grundschule”-Research Group. Is central obesity associated with poorer health and health-related quality of life in primary school children? Cross-sectional results from the Baden-Württemberg Study. BMC Public Health 2013, 13, 260. [Google Scholar] [CrossRef]
- Verrotti, A.; Penta, L.; Zenzeri, L.; Agostinelli, S.; De Feo, P. Childhood obesity: Prevention and strategies of intervention. A systematic review of school-based interventions in primary schools. J. Endocrinol. Investig. 2014, 37, 1155–1164. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T. Lifestyle intervention in childhood obesity: Changes and challenges. Nat. Rev. Endocrinol. 2013, 9, 607–614. [Google Scholar] [CrossRef]
- Seidell, J.C.; Halberstadt, J. The global burden of obesity and the challenges of prevention. Ann. Nutr. Metab. 2015, 66 (Suppl. 2), 7–12. [Google Scholar] [CrossRef]
- Adab, P.; Pallan, M.J.; Lancashire, E.R.; Hemming, K.; Frew, E.; Barrett, T.; Bhopal, R.; Cade, J.E.; Canaway, A.; Clarke, J.L.; et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6 and 7 year olds: Cluster randomised controlled trial (WAVES study). BMJ 2018, 360, k211. [Google Scholar] [CrossRef]
- Wabitsch, M.; Moss, A.; Kromeyer-Hauschild, K. Unexpected plateauing of childhood obesity rates in developed countries. BMC Med. 2014, 12, 17. [Google Scholar] [CrossRef]
- Albornoz-Guerrero, J.; García, S.; de Sevilla, G.G.P.; Cigarroa, I.; Zapata-Lamana, R. Characteristics of Multicomponent Interventions to Treat Childhood Overweight and Obesity in Extremely Cold Climates: A Systematic Review of a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 3098. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.A. Physical Inactivity in Childhood from Preschool to Adolescence. ACSM’S Health Fit. J. 2019, 23, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Solomonova, E.; Picard-Deland, C.; Rapoport, I.L.; Pennestri, M.-H.; Saad, M.; Kendzerska, T.; Veissiere, S.P.L.; Godbout, R.; Edwards, J.D.; Quilty, L.; et al. Stuck in a lockdown: Dreams, bad dreams, nightmares, and their relationship to stress, depression and anxiety during the COVID-19 pandemic. PLoS ONE 2021, 16, e0259040. [Google Scholar] [CrossRef]
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental health impacts of the COVID-19 pandemic on children and youth—A systematic review. Child Adolesc. Ment. Health 2022, 27, 173–189. [Google Scholar] [CrossRef]
- Madigan, S.; Eirich, R.; Pador, P.; McArthur, B.A.; Neville, R.D. Assessment of Changes in Child and Adolescent Screen Time During the COVID-19 Pandemic: A Systematic Review and Meta-analysis. JAMA Pediatr. 2022, 176, 1188–1198. [Google Scholar] [CrossRef] [PubMed]
- Burkart, S.; Parker, H.; Weaver, R.G.; Beets, M.W.; Jones, A.; Adams, E.L.; Chaput, J.; Armstrong, B. Impact of the COVID-19 pandemic on elementary schoolers’ physical activity, sleep, screen time and diet: A quasi-experimental interrupted time series study. Pediatr. Obes. 2022, 17, e12846. [Google Scholar] [CrossRef] [PubMed]
- Sturm, D.J.; Kelso, A.; Kobel, S.; Demetriou, Y. Physical activity levels and sedentary time during school hours of 6th-grade girls in Germany. J. Public Health 2021, 29, 847–855. [Google Scholar] [CrossRef]
- Colella, D.; Monacis, D.; Limone, P. Active Breaks and Motor Competencies Development in Primary School: A Systematic Review. Adv. Phys. Educ. 2020, 10, 233–250. [Google Scholar] [CrossRef]
- Moscatelli, F.; De Maria, A.; Marinaccio, L.A.; Monda, V.; Messina, A.; Monacis, D.; Toto, G.; Limone, P.; Monda, M.; Messina, G.; et al. Assessment of Lifestyle, Eating Habits and the Effect of Nutritional Education among Undergraduate Students in Southern Italy. Nutrients 2023, 15, 2894. [Google Scholar] [CrossRef]
- Alonso-Martínez, A.M.; Ramírez-Vélez, R.; García-Alonso, Y.; Izquierdo, M.; García-Hermoso, A. Physical Activity, Sedentary Behavior, Sleep and Self-Regulation in Spanish Preschoolers during the COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2021, 18, 693. [Google Scholar] [CrossRef]
- Mahar, M.T.; Kenny, R.K.; Shields, A.T.; Scales, D.P.; Collins, G. Energizers Classroom-Based Physical Activities 3–5: The Way Teachers Integrate Physical Activity with Academic Concepts. 2006. Available online: https://thescholarship.ecu.edu/handle/10342/5945 (accessed on 8 November 2022).
- Neil-Sztramko, S.E.; Caldwell, H.; Dobbins, M. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2021, 2021, CD007651. [Google Scholar] [CrossRef]
- Watson, A.; Timperio, A.; Brown, H.; Best, K.; Hesketh, K.D. Effect of classroom-based physical activity interventions on academic and physical activity outcomes: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 114. [Google Scholar] [CrossRef]
- Peláez-Flor, V.; Prieto-Ayuso, A. “Aprendo Moviéndome”: Active breaks program for primary education. Sport TK 2021, 10, 107–135. [Google Scholar] [CrossRef]
- Masini, A.; Marini, S.; Leoni, E.; Lorusso, G.; Toselli, S.; Tessari, A.; Ceciliani, A.; Dallolio, L. Active Breaks: A Pilot and Feasibility Study to Evaluate the Effectiveness of Physical Activity Levels in a School Based Intervention in an Italian Primary School. Int. J. Environ. Res. Public Health 2020, 17, 4351. [Google Scholar] [CrossRef] [PubMed]
- Sánchez López, M.; García López, L.M.; Ruiz Hermosa, A. Fichas de Descansos Activos para Educación Infantil y Primaria. Guía para el Profesorado; Repositorio RUIdeRA; Ediciones de la Universidad de Castilla La Mancha: Cuenca, Spain, 2020. [Google Scholar] [CrossRef]
- Ortega, F.B.; Lavie, C.J.; Blair, S.N. Obesity and cardiovascular disease. Circ. Res. 2016, 118, 1752–1770. [Google Scholar] [CrossRef] [PubMed]
- Peña, G.; Heredia, J.R.; Lloret, C.; Martín, M.; Da Silva-Grigoletto, M.E. Iniciación al entrenamiento de fuerza en edades tempranas: Revisión. Rev. Andal. Med. Deporte 2016, 9, 41–49. [Google Scholar] [CrossRef][Green Version]
- Smith, J.J.; Eather, N.; Morgan, P.J.; Plotnikoff, R.C.; Faigenbaum, A.D.; Lubans, D.R. The health benefits of muscular fitness for children and adolescents: A systematic review and meta-analysis. Sports Med. 2014, 44, 1209–1223. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martínez-Vizcaino, V.; Redondo-Tébar, A.; Pozuelo-Carrascosa, D.P.; Sánchez-López, M. Relationship between both cardiorespiratory and muscular fitness and health-related quality of life in children and adolescents: A systematic review and meta-analysis of observational studies. Health Qual. Life Outcomes 2021, 19, 127. [Google Scholar] [CrossRef]
- Lavie, C.J.; Kachur, S.; Sui, X. Impact of fitness and changes in fitness on lipids and survival. Prog. Cardiovasc. Dis. 2019, 62, 431–435. [Google Scholar] [CrossRef]
- Yu, C.C.W.; Sung, R.Y.T.; Hau, K.-T. The effect of diet and strength training on obese children’s physical self-concept. J. Sports Med. Phys. Fit. 2008, 48, 76. [Google Scholar]
- Carbone, S.; Kirkman, D.L.; Garten, R.S.; Rodriguez-Miguelez, P.; Artero, E.G.; Lee, D.-C.; Lavie, C.J. Muscular Strength and Cardiovascular Disease: An updated state-of-the-art narrative review. J. Cardiopulm. Rehabil. Prev. 2020, 40, 302–309. [Google Scholar] [CrossRef]
- Artero, E.G.; Lee, D.-C.; Lavie, C.J.; España-Romero, V.; Sui, X.; Church, T.S.; Blair, S.N.P. Effects of muscular strength on cardiovascular risk factors and prognosis. J. Cardiopulm. Rehabil. Prev. 2012, 32, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Cai, L.; Wu, Y.; Wilson, R.F.; Weston, C.; Fawole, O.; Bleich, S.N.; Cheskin, L.J.; Showell, N.N.; Lau, B.D.; et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes. Rev. 2015, 16, 547–565. [Google Scholar] [CrossRef] [PubMed]
- Marker, A.M.; Steele, R.G.; Noser, A.E. Physical activity and health-related quality of life in children and adolescents: A systematic review and meta-analysis. Health Psychol. 2018, 37, 893–903. [Google Scholar] [CrossRef]
- Bacopoulou, F.; Landis, G.; Rentoumis, A.; Tsitsika, A.; Efthymiou, V. Mediterranean diet decreases adolescent waist circumference. Eur. J. Clin. Investig. 2017, 47, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Sadeghirad, B.; Duhaney, T.; Motaghipisheh, S.; Campbell, N.R.C.; Johnston, B.C. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: A systematic review and meta-analysis of randomized trials. Obes. Rev. 2016, 17, 945–959. [Google Scholar] [CrossRef]
- Boyland, E.J.; Nolan, S.; Kelly, B.; Tudur-Smith, C.; Jones, A.; Halford, J.C.; Robinson, E. Advertising as a cue to consume: A systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am. J. Clin. Nutr. 2016, 103, 519–533. [Google Scholar] [CrossRef]
- Wu, C.; Xu, Y.; Chen, Z.; Cao, Y.; Yu, K.; Huang, C. The effect of intensity, frequency, duration and volume of physical activity in children and adolescents on skeletal muscle fitness: A systematic review and meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2021, 18, 9640. [Google Scholar] [CrossRef]
- Mead, E.; Brown, T.; Rees, K.; Azevedo, L.B.; Whittaker, V.; Jones, D.; Olajide, J.; Mainardi, G.M.; Corpeleijn, E.; O’Malley, C.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017, 6, CD012651. [Google Scholar] [CrossRef]
- Luttikhuis, H.O.; Baur, L.; Jansen, H.; A Shrewsbury, V.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane Database Syst. Rev. 2009, CD001872. [Google Scholar] [CrossRef]
- Li, D.; Chen, P. The Effects of Different Exercise Modalities in the Treatment of Cardiometabolic Risk Factors in Obese Adolescents with Sedentary Behavior—A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Children 2021, 8, 1062. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Lin, J.; Lin, Y.; Xu, L.; Lu, D.; Li, F.; Hou, L.; Yu, C.C.W. Effects of aerobic exercise and resistance exercise on physical indexes and cardiovascular risk factors in obese and overweight school-age children: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0257150. [Google Scholar] [CrossRef]
- Diao, H.; Wang, H.; Yang, L.; Li, T. The impacts of multiple obesity-related interventions on quality of life in children and adolescents: A randomized controlled trial. Health Qual. Life Outcomes 2020, 18, 213. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trials. Ann. Intern. Med. 2010, 152, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Suchomel, T.J.; Nimphius, S.; Bellon, C.R.; Stone, M.H. The Importance of Muscular Strength: Training Considerations. Sports Med. 2018, 48, 765–785. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Vinstrup, J.; Jakobsen, M.D.; Sundstrup, E. Validity and reliability of elastic resistance bands for measuring shoulder muscle strength. Scand. J. Med. Sci. Sports 2017, 27, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Pochetti, J.; Ponczosznik, D.; Rojas, P.; Testa, N. Strength training in children and adolescents: Benefits, risks and recommendations. Arch. Argent. Pediatr. 2018, 116, S82–S91. [Google Scholar] [CrossRef]
- González-Rosalén, J.; Medina-Mirapeix, F.; Cuerda-Del Pino, A.; Moreno-Segura, N.; Gacto-Sánchez, M.; Martín-San Agustín, R. Analysis of Compliance with Time under Tension and Force during Strengthening Exercises with Elastic Bands. Diagnostics 2021, 11, 2016. [Google Scholar] [CrossRef]
- Folkins, E.; Sahni, S.; Ryan, J.; Wooden, S.; Bushby, G.; Radzinski, C. Concentric and Eccentric Force Changes with Elastic Band and Isotonic Heavy Resistance Training: A Randomized Controlled Trial. Int. J. Sports Phys. Ther. 2021, 16, 756–765. [Google Scholar] [CrossRef]
- Ocampo, N.V.; Fredy Ramírez-Villada, J.; De Revisión, A. El efecto de los programas de fuerza muscular sobre la capacidad funcional. Revisión sistemática Effects of muscular strength training programs on functional performance: Systematic review. Rev. Fac. Med. 2018, 66, 399–410. [Google Scholar] [CrossRef]
- Wick, K.; Kriemler, S.; Granacher, U. Effects of a Strength-Dominated Exercise Program on Physical Fitness and Cognitive Performance in Preschool Children. J. Strength Cond. Res. 2021, 35, 983–990. [Google Scholar] [CrossRef] [PubMed]
- Sciences du Sport|Évaluation de la Résistance des Bandes Élastiques Sci-Sport Lors d’essais de Traction en Laboratoire. Available online: https://www.sci-sport.com/articles/evaluation-de-la-resistance-des-bandes-elastiques-sci-sport-lors-d-essais-de-tractions-en-laboratoire-060.php (accessed on 24 July 2023).
- División de Nutrición AF y O. Medición de la Intensidad de la Actividad Física. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/physicalactivity/basics/measuring/index.html (accessed on 23 March 2023).
- Williams, N. The Borg Rating of Perceived Exertion (RPE) scale. Occup. Med. 2017, 67, 404–405. [Google Scholar] [CrossRef]
- Ramírez-Vélez, R.; Peña-Ibagon, J.C.; Martínez-Torres, J.; Tordecilla-Sanders, A.; Correa-Bautista, J.E.; Lobelo, F.; García-Hermoso, A. Handgrip strength cutoff for cardiometabolic risk index among Colombian children and adolescents: The FUPRECOL Study. Sci. Rep. 2017, 7, 42622. [Google Scholar] [CrossRef]
- Albornoz-Guerrero, J.; Zapata-Lamana, R.; Reyes-Molina, D.; Cigarroa, I.; García Pérez de Sevilla, G.; García-Merino, S. Overweight/Obese Schoolchildren with Low Muscle Strength Have a Lower Cardiorespiratory Capacity and Greater Cardiovascular Risk: Results of the School Health Survey of the Extreme South of Chile 2019. Children 2021, 8, 734. [Google Scholar] [CrossRef]
- Lo, K.; Wong, M.; Khalechelvam, P.; Tam, W. Waist-to-height ratio, body mass index and waist circumference for screening paediatric cardio-metabolic risk factors: A meta-analysis. Obes. Rev. 2016, 17, 1258–1275. [Google Scholar] [CrossRef] [PubMed]
- García, J.; Cárdenas, A.; Burgos, S.; Santiago, C.; Hernández, F.; Sanz, V.; Fernandez-Del-Valle, M.; Rubio, M.; Pérez, M. Estilo de vida y distribución de grasa en adolescentes asmáticos y sanos. Rev. Int. Med. Cienc. Act. Física Deporte 2019, 19, 107–118. [Google Scholar] [CrossRef]
- Habicht, J.-P. Estandarización de metodos epidemiológicos cuantitativos sobre el terreno. Boletín Oficina Sanit. Panam. (OSP) 1974, 76, 375–384. [Google Scholar]
- Aber, L.; Brown, J.L.; Jones, S.M.; Berg, J.; Torrente, C. School-based strategies to prevent violence, trauma, and psychopathology: The challenges of going to scale. Dev. Psychopathol. 2011, 23, 411–421. [Google Scholar] [CrossRef]
- Batería ALPHA-Fitness: Test de Campo para la Evaluación de la Condición Física Relacionada con la Salud en Niños y Adolescentes. Available online: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0212-16112011000600003 (accessed on 30 November 2021).
- Aguilar, M.M.; Vergara, F.A.; Velásquez, E.J.A.; García-Hermoso, A. Physical activity, screen time and sleep patterns in Chilean girls. An. Pediatría (Engl. Ed.) 2015, 83, 304–310. [Google Scholar] [CrossRef]
- Orgilés, M.; Owens, J.; Espada, J.P.; Piqueras, J.A.; Carballo, J.L. Spanish version of the Sleep Self-Report (SSR): Factorial structure and psychometric properties. Child Care Health Dev. 2013, 39, 288–295. [Google Scholar] [CrossRef]
- Artero, E.G.; Ruiz, J.R.; Ortega, F.B.; España-Romero, V.; Vicente-Rodríguez, G.; Molnar, D.; Gottrand, F.; González-Gross, M.; Breidenassel, C.; Moreno, L.A.; et al. Muscular and cardiorespiratory fitness are independently associated with metabolic risk in adolescents: The HELENA study. Pediatr. Diabetes 2011, 12, 704–712. [Google Scholar] [CrossRef]
- Steene-Johannessen, J.; Anderssen, S.A.; Kolle, E.; Andersen, L.B. Low muscle fitness is associated with metabolic risk in youth. Med. Sci. Sports Exerc. 2009, 41, 1361–1367. [Google Scholar] [CrossRef] [PubMed]
- Grøntved, A.; Ried-Larsen, M.; Møller, N.C.; Kristensen, P.L.; Froberg, K.; Brage, S.; Andersen, L.B. Muscle strength in youth and cardiovascular risk in young adulthood (the European Youth Heart Study). Br. J. Sports Med. 2015, 49, 90–94. [Google Scholar] [CrossRef] [PubMed]
- de Quadros, T.M.B.; Gordia, A.P.; Silva, L.R. Anthropometry and clustered cardiometabolic risk factors in young people: A systematic review. Rev. Paul. Pediatr. 2017, 35, 340–350. [Google Scholar]
- de Quadros, T.M.B.; Gordia, A.P.; Andaki, A.C.R.; Mendes, E.L.; Mota, J.; Silva, L.R. Utility of anthropometric indicators to screen for clustered cardiometabolic risk factors in children and adolescents. J. Pediatr. Endocrinol. Metab. 2019, 32, 49–55. [Google Scholar] [CrossRef]
- Smith, J.J.; Eather, N.; Weaver, R.G.; Riley, N.; Beets, M.W.; Lubans, D.R. Behavioral Correlates of Muscular Fitness in Children and Adolescents: A Systematic Review. Sports Med. 2019, 49, 887–904. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Correa-Bautista, J.E.; Olloquequi, J.; Ramírez-Vélez, R. Health-related physical fitness and weight status in 13- to 15-year-old Latino adolescents. A pooled analysis. J. Pediatr. 2019, 95, 435–442. [Google Scholar] [CrossRef]
- Ryan, R.M.; Williams, G.C.; Patrick, H.; Deci, E.L. Self-Determination Theory and Physical Activity: The Dynamics of Motivation in Development and Wellness. Hell. J. Psychol. 2009, 6, 107–124. [Google Scholar]
- Fox, K.R.; Corbin, C.B. The Physical Self-Perception Profile: Devlopment and Preliminary Validation. J. Sport Exerc. Psychol. 2016, 11, 408–430. [Google Scholar] [CrossRef]
- Lubans, D.R.; Plotnikoff, R.C.; Lubans, N.J. Review: A systematic review of the impact of physical activity programmes on social and emotional well-being in at-risk youth. Child Adolesc. Ment. Health 2012, 17, 2–13. [Google Scholar] [CrossRef]
- Moliner-Urdiales, D.; Ruiz, J.R.; Vicente-Rodriguez, G.; Ortega, F.B.; Rey-Lopez, J.P.; España-Romero, V.; Casajús, J.A.; Molnar, D.; Widhalm, K.; Dallongeville, J.; et al. Associations of muscular and cardiorespiratory fitness with total and central body fat in adolescents: The HELENA study. Br. J. Sports Med. 2011, 45, 101–108. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Ramírez-Campillo, R.; Izquierdo, M. Is Muscular Fitness Associated with Future Health Benefits in Children and Adolescents? A Systematic Review and Meta-Analysis of Longitudinal Studies. Sports Med. 2019, 49, 1079–1094. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Cavero-Redondo, I.; Ramírez-Vélez, R.; Ruiz, J.R.; Ortega, F.B.; Lee, D.-C.; Martínez-Vizcaíno, V. Muscular Strength as a Predictor of All-Cause Mortality in an Apparently Healthy Population: A Systematic Review and Meta-Analysis of Data From Approximately 2 Million Men and Women. Arch. Phys. Med. Rehabil. 2018, 99, 2100–2113.e5. [Google Scholar] [CrossRef]
- Fraser, B.J.; Blizzard, L.; Cleland, V.; Schmidt, M.D.; Smith, K.J.; Gall, S.L.; Dwyer, T.; Venn, A.J.; Magnussen, C.G. Factors associated with persistently high muscular power from childhood to adulthood. Med. Sci. Sports Exerc. 2020, 52, 49–55. [Google Scholar] [CrossRef]
- Zeller, M.; Kirk, S.; Claytor, R.; Khoury, P.; Grieme, J.; Santangelo, M.; Daniels, S. Predictors of attrition from a pediatric weight management program. J. Pediatr. 2004, 144, 466–470. [Google Scholar] [CrossRef] [PubMed]
- Braet, C.; Van Winckel, M.; Van Leeuwen, K. Follow-up results of different treatment programs for obese children. Acta Paediatr. 1997, 86, 397–402. [Google Scholar] [CrossRef]
- Nemet, D.; Barkan, S.; Epstein, Y.; Friedland, O.; Kowen, G.; Eliakim, A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics 2005, 115, e443–e449. [Google Scholar] [CrossRef]
- Epstein, L.H.; Roemmich, J.N.; Raynor, H.A. Behavioral therapy in the treatment of pediatric obesity. Pediatr. Clin. N. Am. 2001, 48, 981–993. [Google Scholar] [CrossRef]
- Juliana Kain, B.; Fernando Vio, D.; Barbara Leyton, D.; Ricardo Cerda, R.; Sonia Olivares, C.; Ricardo Uauy, D.; Cecilia Albala, B. School-based health promotion intervention for primary schoolchildren from casablanca, chile. Rev. Chil. Nutr. 2005, 32, 126–132. [Google Scholar] [CrossRef]
- Waters, E.; De Silva-Sanigorski, A.; Burford, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011, 2011, CD001871. [Google Scholar] [CrossRef]
- Yoong, S.L.; Lum, M.; Wolfenden, L.; Jackson, J.; Barnes, C.; Hall, A.E.; McCrabb, S.; Pearson, N.; Lane, C.; Jones, J.Z.; et al. Healthy eating interventions delivered in early childhood education and care settings for improving the diet of children aged six months to six years. Cochrane Database Syst. Rev. 2023, 2023, CD013862. [Google Scholar] [CrossRef]
- Martin, A.; Booth, J.N.; Laird, Y.; Sproule, J.; Reilly, J.J.; Saunders, D.H. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Syst. Rev. 2018, 1, CD009728. [Google Scholar] [CrossRef]
- Wright, C.M.; Duquesnay, P.J.; Anzman-Frasca, S.; Chomitz, V.R.; Chui, K.; Economos, C.D.; Langevin, E.G.; Nelson, M.E.; Sacheck, J.M. Study protocol: The Fueling Learning through Exercise (FLEX) study—A randomized controlled trial of the impact of school-based physical activity programs on children’s physical activity, cognitive function, and academic achievement. BMC Public Health 2016, 16, 1078. [Google Scholar] [CrossRef]
- Storz, M.A. The COVID-19 pandemic: An unprecedented tragedy in the battle against childhood obesity. Clin. Exp. Pediatr. 2020, 63, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Steenblock, C.; Hassanein, M.; Khan, E.G.; Yaman, M.; Kamel, M.; Barbir, M.; Lorke, D.E.; Everett, D.; Bejtullah, S.; Lohmann, T.; et al. Obesity and COVID-19: What are the Consequences? Horm. Metab. Res. 2022, 54, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Mavilidi, M.F.; Lubans, D.R.; Morgan, P.J.; Miller, A.; Eather, N.; Karayanidis, F.; Lonsdale, C.; Noetel, M.; Shaw, K.; Riley, N. Integrating physical activity into the primary school curriculum: Rationale and study protocol for the “Thinking while Moving in English” cluster randomized controlled trial. BMC Public Health 2019, 19, 379. [Google Scholar] [CrossRef] [PubMed]
- Watson, A.; Timperio, A.; Brown, H.; Hesketh, K.D. A primary school active break programme (ACTI-BREAK): Study protocol for a pilot cluster randomised controlled trial. Trials 2017, 18, 433. [Google Scholar] [CrossRef]
- Wright, R.R.; Nelson, R.; Garcia, S.; Butler, A. Health Behavior Change in the Classroom: A Means to a Healthy End? J. Prim. Prev. 2020, 41, 445–472. [Google Scholar] [CrossRef]
- Lee, M.; Lee, H.; Kim, Y.; Kim, J.; Cho, M.; Jang, J.; Jang, H. Mobile App-Based Health Promotion Programs: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2018, 15, 2838. [Google Scholar] [CrossRef]
- Milne-Ives, M.; LamMEng, C.; de Cock, C.; van Velthoven, M.H.; Ma, E.M. Mobile Apps for Health Behavior Change in Physical Activity, Diet, Drug and Alcohol Use, and Mental Health: Systematic Review. JMIR mHealth uHealth 2020, 8, e17046. [Google Scholar] [CrossRef]
- Congdon, P. Obesity and Urban Environments. Int. J. Environ. Res. Public Health 2019, 16, 464. [Google Scholar] [CrossRef] [PubMed]
- Pouliou, T.; Elliott, S.J. Individual and socio-environmental determinants of overweight and obesity in Urban Canada. Health Place 2010, 16, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Verger, P.; Saliba, B.; Guagliardo, V.; Bouhnik, A.D.; Eichenbaum-Voline, S. [Individual social characteristics, municipal environment and the prevalence of weight problems in early childhood: A multilevel analysis]. Rev. D’épidémiologie Santé Publique 2007, 55, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Ley Chile-Decreto 290 17-SEP-1984 Ministerio de Educación Pública-Biblioteca del Congreso Nacional [Internet]. Available online: https://www.bcn.cl/leychile/navegar?idNorma=11989 (accessed on 26 July 2023).
| Inclusion Criteria | Exclusion Criteria | ||
|---|---|---|---|
| - Current registration at the time of the study. | - Physical, mental, or cognitive health conditions that prevent the proper completion of a program of exercise. | ||
| - Both sexes, fifth grade (10–12 years old). | |||
| - Residence in Punta Arenas. | - Acute or chronic decompensated pathology. | ||
| - Parents’ or tutors’ legal consent. - Assent of schoolchildren. | - Severe vision or hearing loss. | ||
| - Presence of vertigo or epilepsy. | |||
| - Be participating in a physical exercise program regularly outside the educational center. | |||
| March | April | May | June | July | Aug. | Sept. | Oct./Nov. | |
|---|---|---|---|---|---|---|---|---|
| Recruitment of support researchers | x | |||||||
| Training of support professionals | x | |||||||
| Coordination meeting with the director of the educational center | x | |||||||
| Coordination meetings with teachers from the educational center | x | |||||||
| Training for teachers of educational centers | x | |||||||
| Delivery and collection of consents to parents and/or legal guardians | x | x | ||||||
| Delivery and collection of informed consents of schoolchildren | x | x | ||||||
| Preintervention measurements | x | |||||||
| Group randomization | x | |||||||
| Intervention within the educational centers | x | x | x | x | x | x | ||
| Post intervention measurements | x | |||||||
| Data analysis | x | |||||||
| Delivery of reports to educational centers | x |
| Intervention Group 1 | Intervention Group 2 | Control Group 3 |
|---|---|---|
| Strength exercises * | Usual routine habits | Usual routine habits |
| 1 Warm-up | ||
| 2 Elbow flexion | ||
| 3 Elbow extension | ||
| 4 Hip and knee flexo-extension | ||
| 5 Knee flexion | ||
| 6 Stretching | ||
| Nutritional recommendations ** | Nutritional recommendations ** | Usual routine habits |
| 1 Water | 1 Water | |
| 2 Carbohydrates | 2 Carbohydrates | |
| 3 Proteins | 3 Proteins | |
| 4 Sugars | 4 Sugars | |
| 5 Lipids | 5 Lipids | |
| Sleep and screen use recommendations *** | Sleep and screen use recommendations *** | Usual routine habits |
| 1 Sleep habits | 1 Sleep habits | |
| 2 Screen time | 2 Screen time |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albornoz-Guerrero, J.; Barceló, O.; García-Merino, S.; García-Pérez-de-Sevilla, G.; Cigarroa, I.; Zapata-Lamana, R. Protocol Study: Resistance Training Program, Nutritional, Sleep, and Screen Use Recommendations in Schoolchildren from Educational Centers in the Extreme South of Chile. Methods Protoc. 2023, 6, 74. https://doi.org/10.3390/mps6050074
Albornoz-Guerrero J, Barceló O, García-Merino S, García-Pérez-de-Sevilla G, Cigarroa I, Zapata-Lamana R. Protocol Study: Resistance Training Program, Nutritional, Sleep, and Screen Use Recommendations in Schoolchildren from Educational Centers in the Extreme South of Chile. Methods and Protocols. 2023; 6(5):74. https://doi.org/10.3390/mps6050074
Chicago/Turabian StyleAlbornoz-Guerrero, Javier, Olga Barceló, Sonia García-Merino, Guillermo García-Pérez-de-Sevilla, Igor Cigarroa, and Rafael Zapata-Lamana. 2023. "Protocol Study: Resistance Training Program, Nutritional, Sleep, and Screen Use Recommendations in Schoolchildren from Educational Centers in the Extreme South of Chile" Methods and Protocols 6, no. 5: 74. https://doi.org/10.3390/mps6050074
APA StyleAlbornoz-Guerrero, J., Barceló, O., García-Merino, S., García-Pérez-de-Sevilla, G., Cigarroa, I., & Zapata-Lamana, R. (2023). Protocol Study: Resistance Training Program, Nutritional, Sleep, and Screen Use Recommendations in Schoolchildren from Educational Centers in the Extreme South of Chile. Methods and Protocols, 6(5), 74. https://doi.org/10.3390/mps6050074









