The VISTA Approach in Canine Disimpaction
Abstract
:1. Introduction
2. Experimental Design
2.1. Patient Selection
- Anamnesis;
- Inspection;
- Palpation of the vestibular fornix overlying the lateral incisor to eventually highlight the presence of the bulge of the impacted canine;
- Intra- and extra-oral photos;
- Plaster models;
- X-ray prescription:
- ○
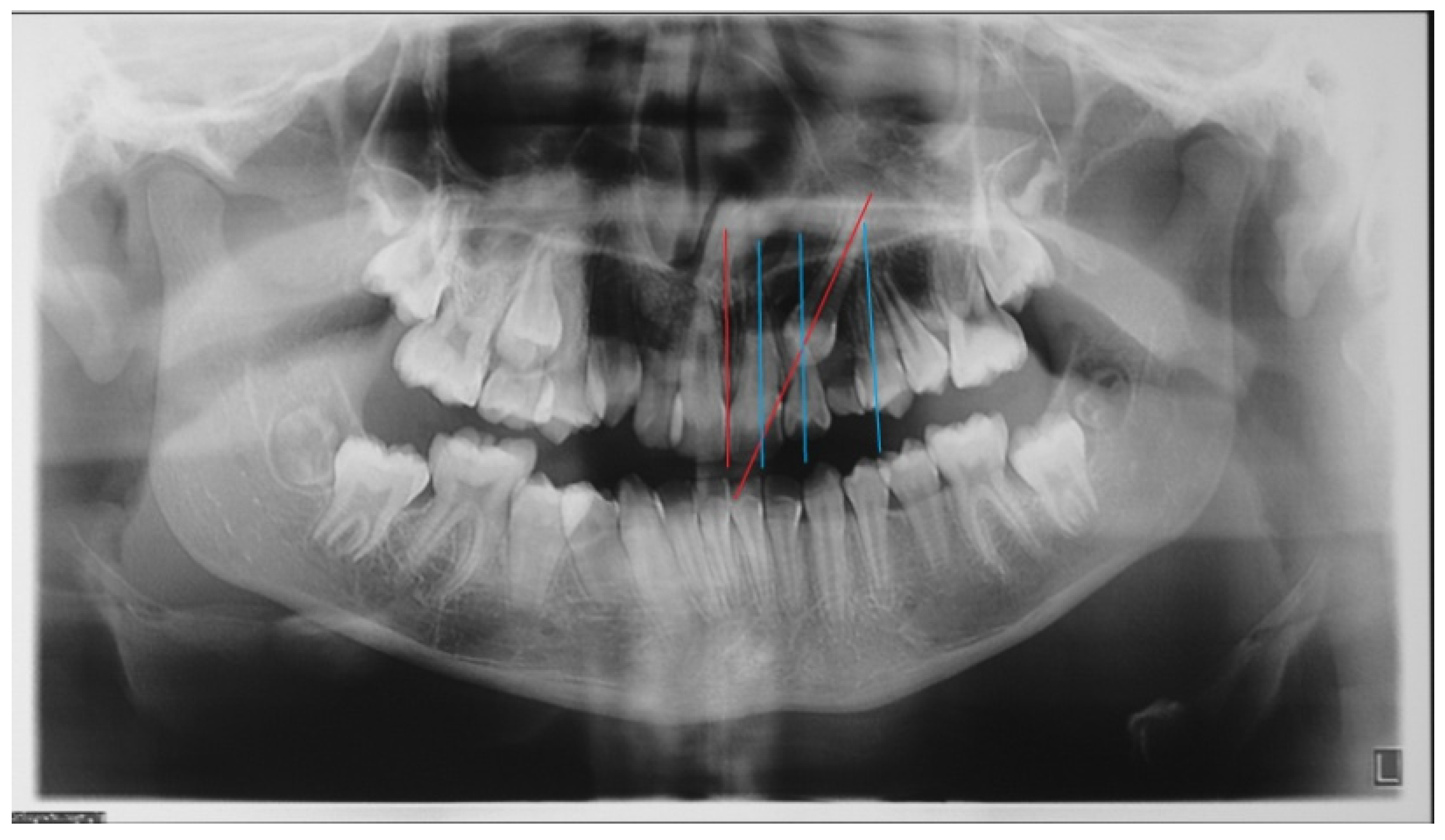
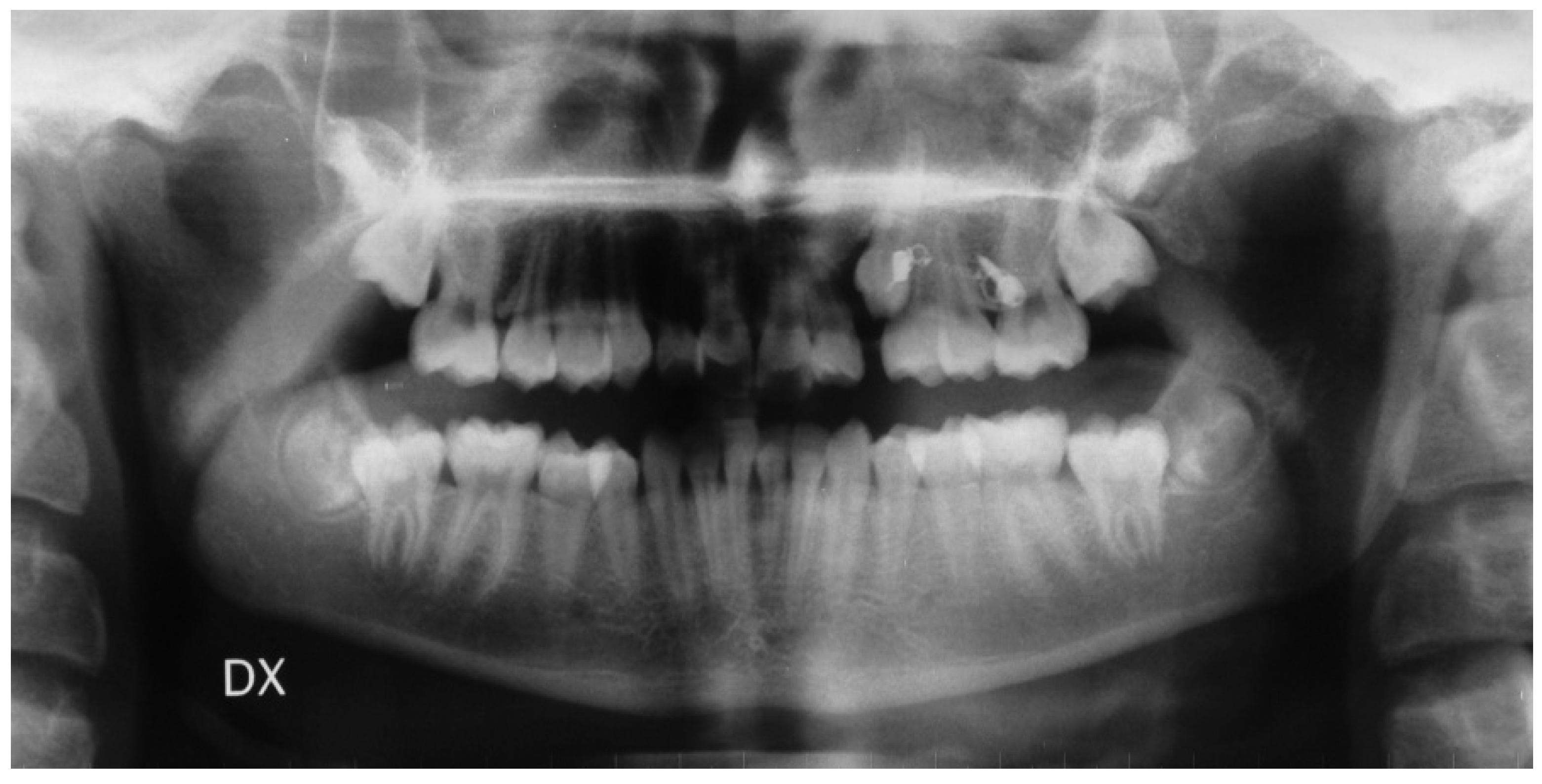
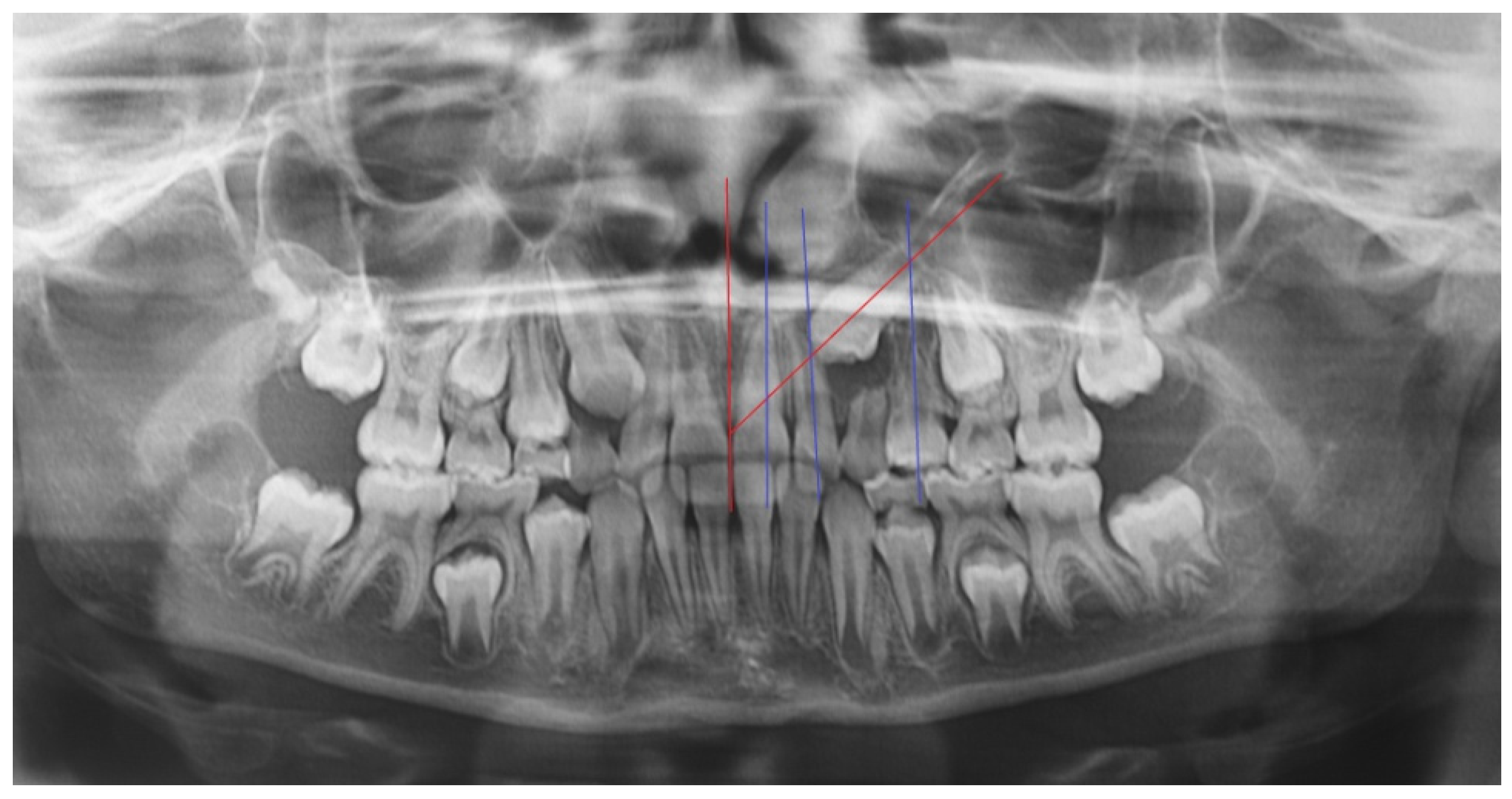
- In the first step, a panoramic radiograph and a teleradiography of the skull in latero-lateral projection is required. The observation of the panoramic radiography should show the position of the impacted canine, evaluating the relationships of the canine crown with the roots of the adjacent teeth, the alpha angle, and the distance of the impacted tooth from the occlusal plane. The cephalometric study of the teleradiography should provide information about the eventually present malocclusion and treatment needed;
- ○
- A cone beam CT, eventually limited to the sector of the impacted tooth, is mandatory to evaluate the three-dimensional relationships of the teeth with the adjacent structures and all of the conditions eventually limiting the correct insertion of temporary anchoring devices (TADs) such as anatomical variation of the lateral extension of the maxillary sinus, the availability of correct inter-root space, or the presence of the premolars buds in mixed dentition. The use of a tridimensional imaging is justified from the need of an accurate assessment of the position of the impacted canine and of its relation with the adjacent structures, due to the higher spatial resolution obtained with lower radiation dose [15].
2.2. Needed Equipment
2.3. Needed Equipment 2
2.4. Needed Equipment 3
Surgical Kit
3. Procedure
3.1. Orthodontic Surgical Protocol
- Local infiltrative anesthesia with vasoconstrictor is performed both in the miniscrew insertion site and at the level of the impacted canine crown;
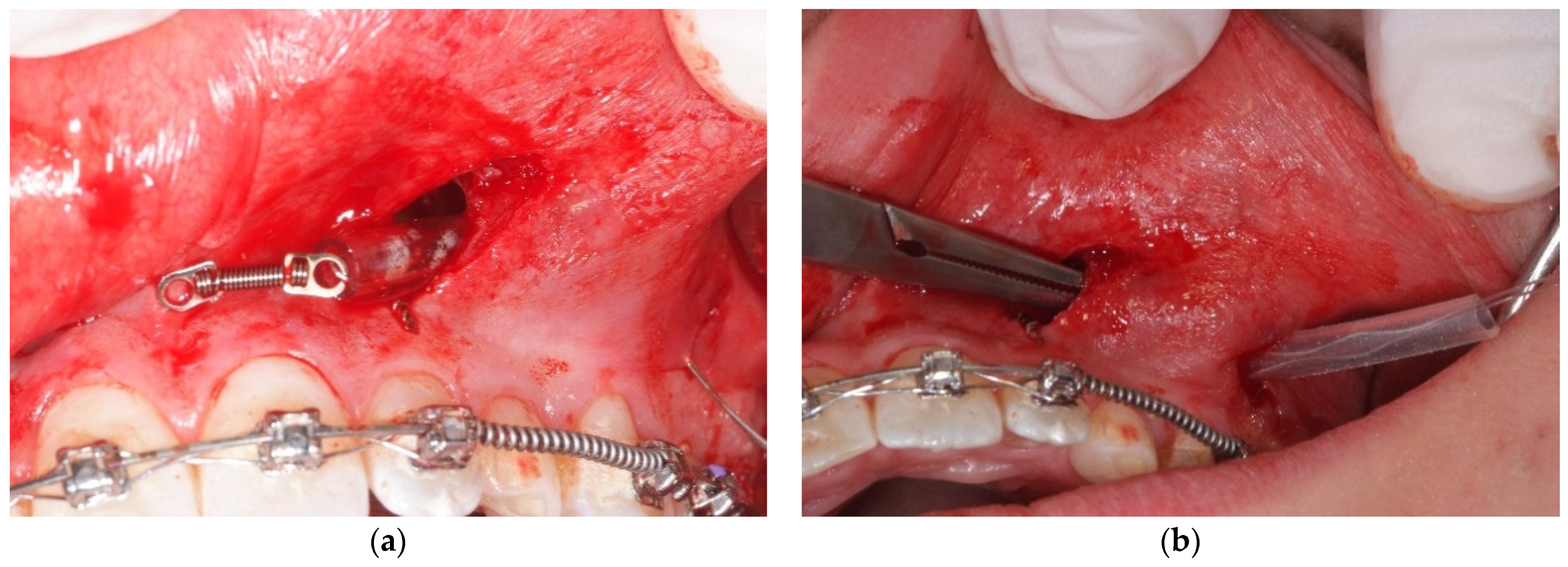
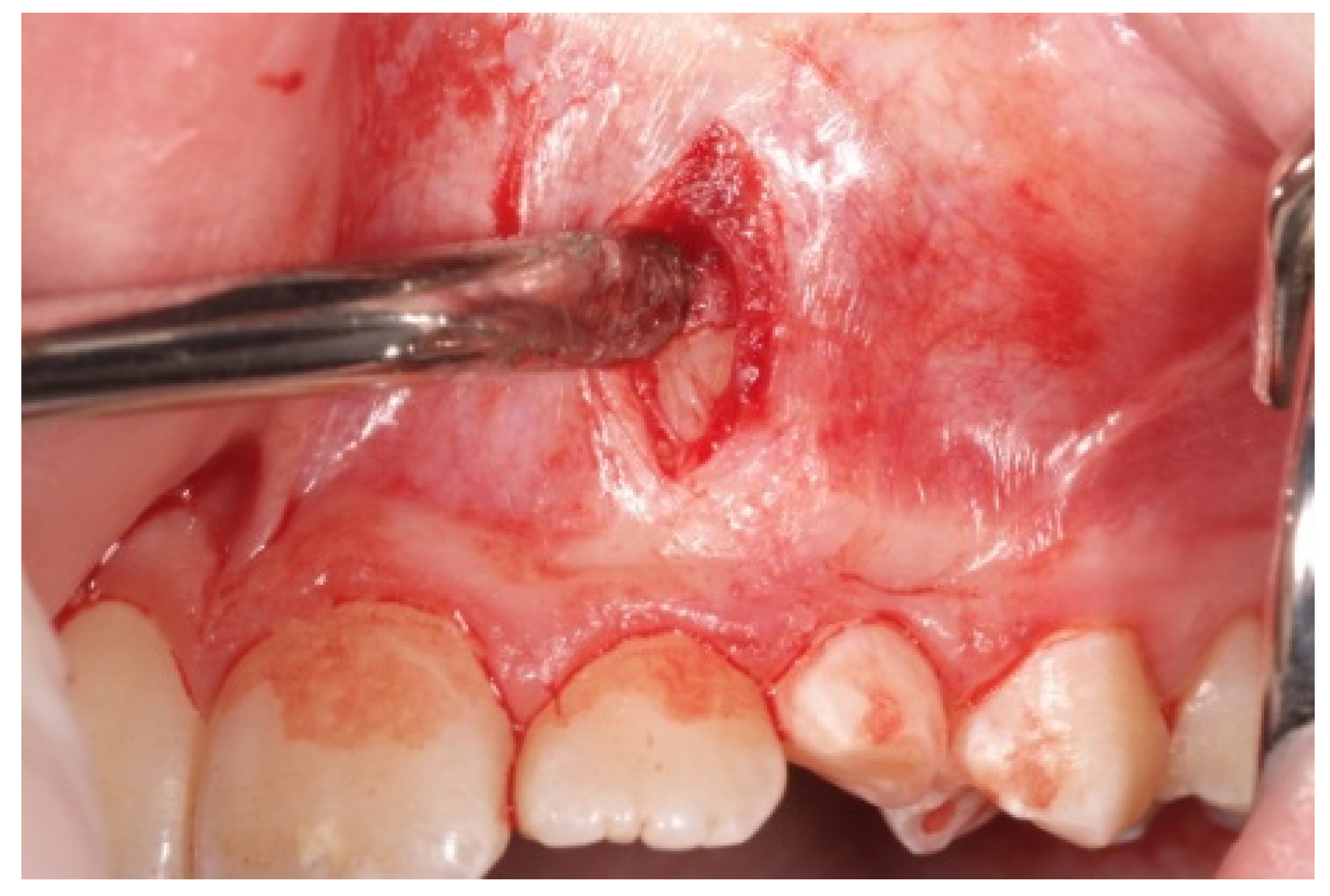
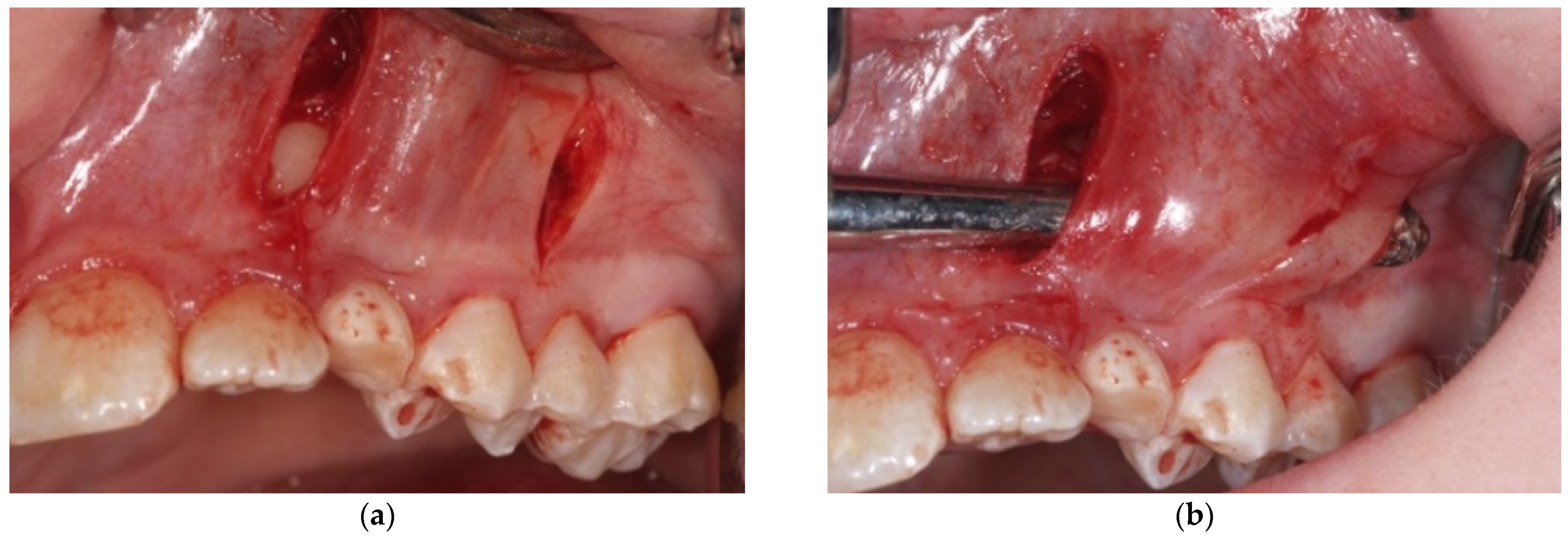
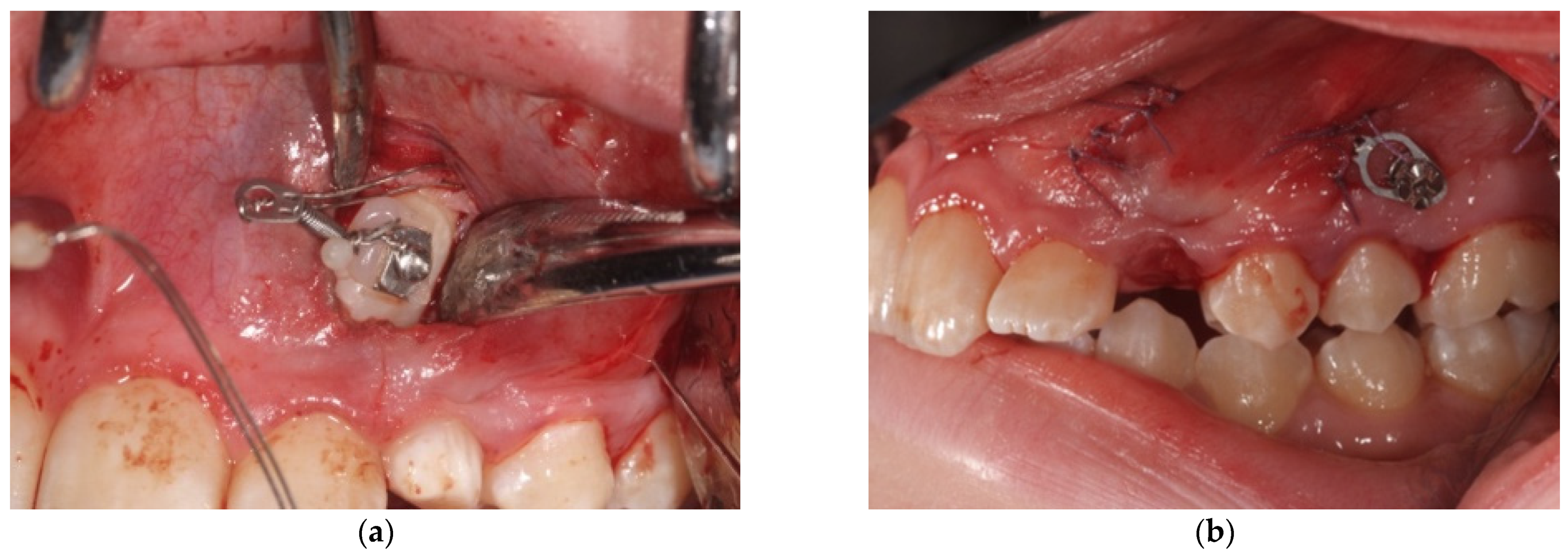
- A first vertical incision, at the level of the impacted tooth crown, and its exposure, with a periosteal elevator, are then performed. If a bony cortex is present overlying the crown, a small bony cavity is made using the multi-blade conical burr with a low-speed right-angle handpiece to expose all of the canine’s crown surface (Figure 3). In any case, a thin groove must be present peripherally to the canine’s crown to guarantee a good isolation from bleeding. Moreover, a further ostectomy is performed on the tooth side toward which the orthodontic traction will be performed (traction route);
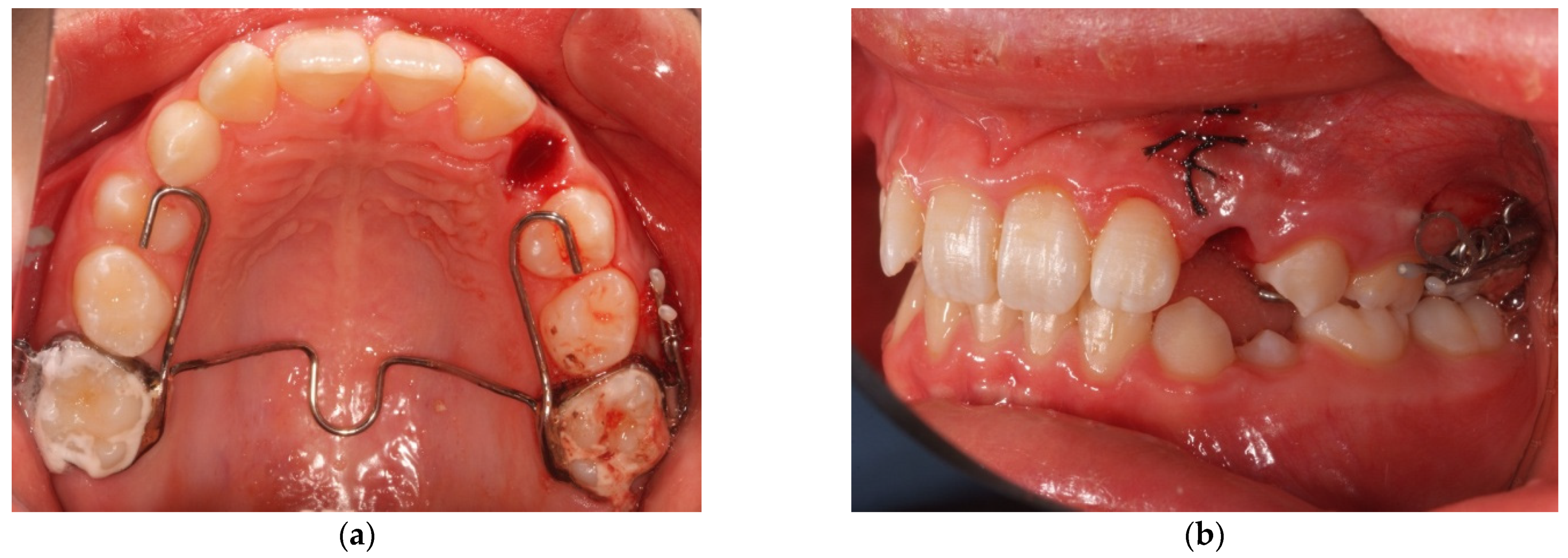
- A second vertical incision is made between the first and second premolar, and the sub-periosteal tunnel is created with a periosteal elevator to connect the two incisions from front to back (Figure 4);
- After a good hemostasis is reached, the button is attached to the buccal canine crown’s surface, following all necessary steps including enamel etching with 37% orthophosphoric acid for 30 s and applying adhesive. Therefore, the button is connected by means of a metal ligature to a 150 gr closed coil spring (NiTi). At the distal end of the NiTi coil, another metal ligature is inserted to facilitate the passage of the traction system under the subperiosteal tunnel (Figure 5);
- Then, the second metallic ligature is inserted in the subperiosteal tunnel to leak out from the posterior vertical incision. Alternatively, the Klemmer forceps can be inserted through the posterior vertical incision and pushed forward inside the tunnel until its end is visible from the anterior incision, to take the spring end and train it posteriorly until it exits from the rear end of the tunnel;
- The correct site of miniscrew insertion is previously established by means of cone beam CT images, and it is usually planned in the inter-radicular area between the second premolar and the first molar;
- The miniscrew chosen for the present protocol (Firma, Sweden & Martina, Padua, Italy) is 1.8 mm in diameter, 8 mm in length, and it is characterized by a standard head and of a double cross-slot, dimensions 0.022 × 0.022 (Figure A1). It is placed on the impacted canine’s side, at approximately 5 mm from the alveolar ridge, according to the indications of Kocsis [15];
- The miniscrew is inserted, using a special screwer, with a direction forming an angle between 30° and 45° with respect to the occlusal plane;
- After checking the primary stability, the miniscrew is connected to the NiTi spring.
- 6.
- Then, the suture of the surgical wounds is performed with an absorbable Vicryl 4-0 thread;
- 7.
- The at-home use of 2% chlorhexidine spray is prescribed.
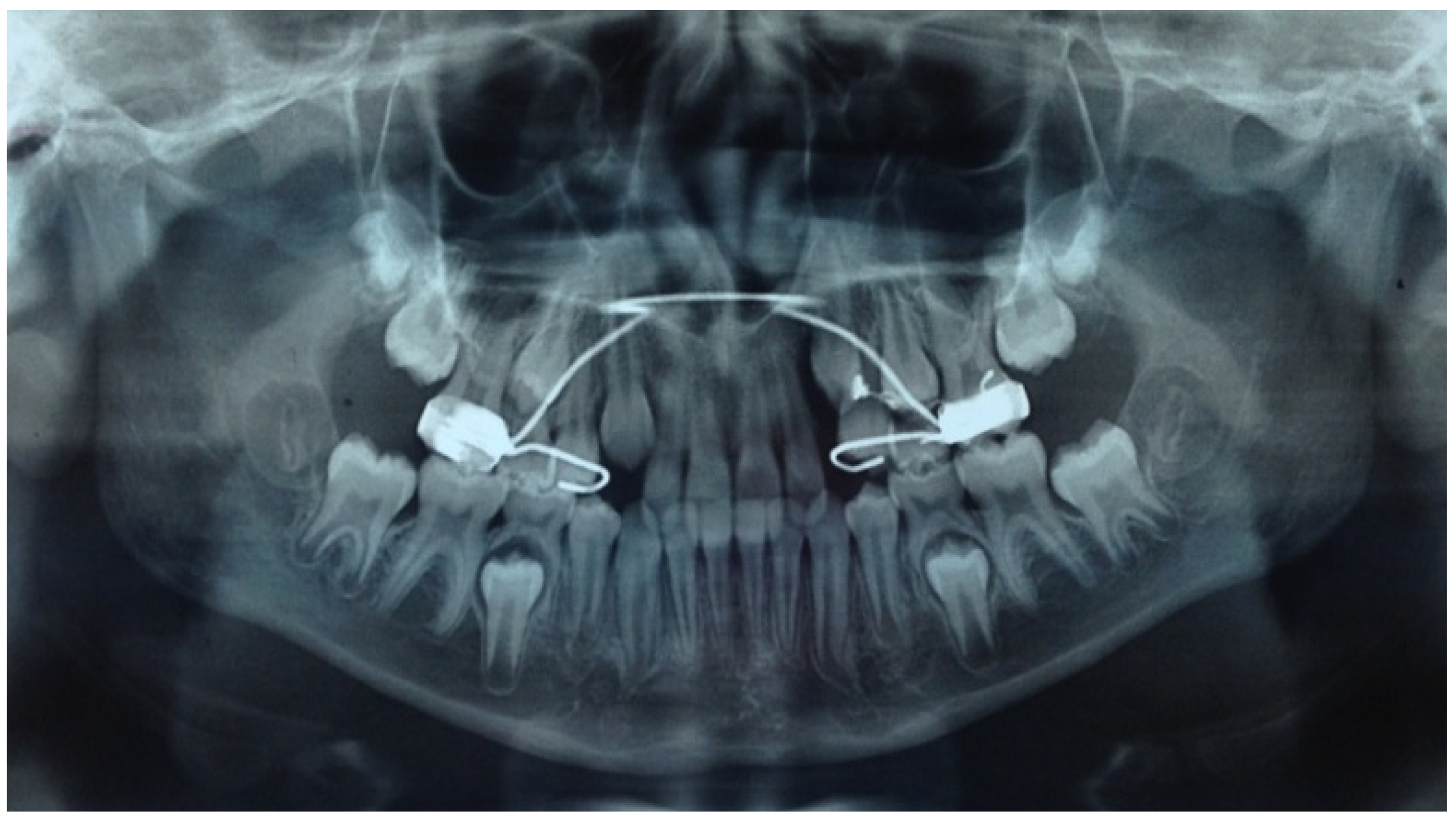
- After steps 1–5 for canine preparation, the previously prepared intraoral anchorage devices are banded to the first molars with glass–ionomeric cement
3.2. Time for Completion
Checklist for the Periodical Control
- ■
- Check the gingival condition around the miniscrew and at the emergence point of the traction metallic ligature. In case of necessity, antiseptic rinses or gel applications are sufficient for inflammation control;
- ■
- Check the miniscrew stability using a tweezer. If necessary, it is possible to screw it again, but a shorter time interval for the next control is appropriate to promptly intercept the possible miniscrew loss;
- ■
- Check the crown position of the contiguous lateral incisor. The displacement of this tooth is related to the pressure exerted on its root by the canine crown during its distal movement. If necessary, a further radiographic control can be performed.
4. Expected Results
- -
- Vestibular Canine in High Position: Patients with a canine impacted in the high position—intended as severely distant from the occlusal plane—have an indication to use the modified VISTA technique as the use of other orthodontic traction techniques, such as cantilever or disinclusion arms welded to orthodontic appliances, can often determine the onset of decubitus and periodontal problems, especially in the lower arch. The canines in high inclusion are not covered by adherent gingiva but by alveolar mucosa and can be approached with the excision of a fibro-mucous operculum, with possible removal of a thin layer of bone or with a closed eruption technique with a full-thickness trapezoidal flap [19,20]. Both of these techniques could have periodontal disadvantages of no adherent gingiva on the damage to the marginal periodontium of the adjacent teeth and also related to the initial canine position [20,21,22,23]. In the VISTA protocol technique, no horizontal cuts are provided, avoiding the use of full-thickness flaps that could affect the marginal periodontium of adjacent teeth, since experimental studies on animal models and humans also suggested that the exposure of the alveolar bone that occurs following the execution of a full-thickness flap stimulates the activity of the osteoclasts with a risk of bone resorption [21].
- -
- Mesioinclinated Canine in Close Relation to The Root of The Lateral Incisor: In cases of vestibular canine impaction, a tight relation between the canine crown and the lateral incisor root is often visible. Every so often, moreover, the lateral incisor presents with a horizontal displacement due to the pressure of the erupting mispositioned canine. This condition frequently correlates with an increased risk of root resorption for the lateral and sometimes also for the central incisor. An orthodontic force applied on the canine crown and directed with a distal and occlusal vector could increase the probability of pressure, due to the fact of this latter component, and could therefore increase the risk of root resorption. Conventional treatment should provide a traction arm in a high position and with a horizontal force direction, thus increasing the patient’s discomfort and the likelihood of eruption in free mucosa. Complex and multidisciplinary cases are particularly prone to this difficult operating condition with wide areas of contact between roots and crowns of impacted teeth [24,25]. In any case, a previous evaluation of the disimpaction prognosis is mandatory (angulation, better if the impacted tooth is mesio-angled, α angle, and sector S of localization of the crown according to the classification of Ericson and Kuroll modified by Baccetti [22]).
- -
- Adequate/Inadequate Interadicular Space for The Insertion of The Miniscrew: The positioning of TADs requires a careful choice of the insertion site to select a position useful for the traction of the impacted teeth but respectful of the teeth and of other anatomical structures. The right selection of the patient performed through an accurate study of the radiographic images is essential, preferably on a 3D imaging of the interested arch. A correct inter-radicular space between the first molar and the second premolar is necessary and should be selected adding 1 mm of bone width and 0.5 mm of periodontium width on both sides to the screw diameter measurement. If any adequate inter-radicular space is available, as often occurs in the patient with a mixed dentition, the variant of the technique provides an anchorage to the distalizing force by an intraoral device, usually consisting of a palatal bar with rests on the premolars and a vertical vestibular arm to which the closed coil-spring should be fixed by a metal chain. A similar vestibular arm can in the same way be soldered also on palatal expanders devices eventually needed for the orthodontic therapy.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A


References
- Manne, R.; Gandikota, C.; Juvvadi, S.R.; Rama, H.R.; Anche, S. Impacted canines: Etiology, diagnosis, and orthodontic management. J. Pharm. Bioallied Sci. 2012, 4, S234–S238. [Google Scholar]
- Becker, A.; Brin, I.; Ben-Bassat, Y.; Zilberman, Y.; Chaushu, S. Closed-eruption surgical technique for impacted maxillary incisors: A postorthodontic periodontal evaluation. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Yan, B.; Sun, Z.; Fields, H.; Wang, L.; Luo, L. Etiologic factors for buccal and palatal maxillary canine impaction: A perspective based on cone-beam computed tomography analyses. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 527–534. [Google Scholar] [CrossRef]
- Becker, A.; Chaushu, S. Etiology of maxillary canine impaction: A review. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 557–567. [Google Scholar] [CrossRef]
- Galluccio, G.; Impellizzeri, A.; De Stefano, A.A.; Serritella, E.; Guercio Monaco, E. Multiple Dental Inclusion in Monozygotic Twins with Congenital Visual Impairment. Case Rep. Dent. 2020, 2020, 8856206. [Google Scholar] [CrossRef]
- Baricevic, M.; Mravak-Stipetic, M.; Majstorovic, M.; Baranovic, M.; Baricevic, D.; Loncar, B. Oral mucosal lesions during orthodontic treatment. Int. J. Paediatr.Dent. 2011, 21, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Zadeh, H.H. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int. J. Period. Rest. Dent. 2011, 31, 653–660. [Google Scholar]
- Chen, C.K.; Chang, C.H.; Roberts, W.E. Class III multiple gingival recession: Vestibular incision subperiosteal tunnel access (VISTA) and platelet-derived growth factor BB. Int. J. Orthod. Implantol. 2014, 35, 22–36. [Google Scholar]
- Bariani, R.C.; Milani, R.; Guimaraes Junior, C.H.; Moura, W.S.; Ortolani, C.L. Orthodontic Traction of Impacted Upper Canines Using the VISTA Technique. J. Clin. Orthod. 2017, 51, 76–85. [Google Scholar]
- Liou, E.J.; Huang, C. Rapid canine retraction through distraction of the periodontal ligament. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 372–382. [Google Scholar] [CrossRef]
- Impellizzeri, A.; Palaia, G.; Horodynski, M.; Pergolini, D.; Vernucci, R.A.; Romeo, U.; Galluccio, G. Co2 laser for surgical exposure of impacted palatally canines. Dent. Cadmos. 2020. [Google Scholar] [CrossRef]
- Pellegrino, G.; Grande, F.; Ferri, A.; Pisi, P.; Gandolfi, M.G.; Marchetti, C. Three-Dimensional Radiographic Evaluation of the Malar Bone Engagement Available for Ideal Zygomatic Implant Placement. Methods Protoc. 2020, 3, 52. [Google Scholar] [CrossRef]
- Kuzniak, N.B.; Fedoniuk, L.Y.; Pryshlyak, A.M.; Skyba, O.I.; Yarema, O.M.; Dovgalyuk, A.I.; Penteleichuk, N.P.; Smiianov, V.A. Morphogenesis of maxillary sinuses in infants, during early and first childhood. Wiad. Lek. 2020, 73, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Kocsis, A.; Seres, L. Orthodontic screw to extrude impacted maxillary canines. J. Orofac. Orthop. 2011, 73, 19–27. [Google Scholar] [CrossRef]
- Nardi, C.; Talamonti, C.; Pallotta, S.; Saletti, P.; Calistri, L.; Cordopatri, C.; Colagrande, S. Head and neck effective dose and quantitative assessment of image quality: A study to compare cone beam CT and multislice spiral CT. Dentomaxillofac. Radiol. 2017, 46, 20170030. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, A.; Horodynski, M.; Serritella, E.; Romeo, U.; Barbato, E.; Galluccio, G. Three-dimensional evaluation of dental movement in orthodontics. Dent. Cadmos 2020, 88, 182–190. [Google Scholar] [CrossRef]
- Chang, H.N.; Su, C.W.; Hsu, Y.L.; Roberts, E.W. Soft tissue considerations for the management of impactions. Int. J. Orthod. Implantol. 2011, 24, 50–59. [Google Scholar]
- Chang, C.H.; Roberts, W.E. Orthodontics, 3Di-Orthoencyclopedia; Newton’s A Ltd.: Taipei, Taiwan, 2012. [Google Scholar]
- Kokich, V.G. Surgical and orthodontic management of impacted maxillary canines. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 278–283. [Google Scholar] [CrossRef]
- Chapokas, A.R.; Almas, K.; Schincaglia, G.P. The impacted maxillary canine: A proposed classification for surgical exposure. Oral surgery, oral medicine. Oral Pathol. Oral Radiol. 2012, 113, 222–228. [Google Scholar] [CrossRef]
- Fickl, S.; Kebschull, M.; Schupbach, P.; Zuhr, O.; Schlagenhauf, U.; Hurzeler, M.B. Bone loss after full-thickness and partial-thickness flap elevation. J. Clin. Periodontol. 2011, 38, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Crescini, A.; Nieri, M.; Rotundo, R.; Pini Prato, G.P. Orthodontic treatment of impacted maxillary canines: An appraisal of prognostic factors. Prog. Orthod. 2007, 8, 6–15. [Google Scholar]
- Skidmore, K.J.; Brook, K.J.; Thomson, W.M.; Harding, W.J. Factors influencing treatment time in orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, A.; Midulla, G.; Romeo, U.; La Monaca, C.; Barbato, E.; Galluccio, G. Delayed Eruption of Permanent Dentition and Maxillary Contraction in Patients with Cleidocranial Dysplasia: Review and Report of a Family. Int. J. Dent. 2018, 2018, 6591414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Impellizzeri, A.; Giannantoni, I.; Polimeni, A.; Barbato, E.; Galluccio, G. Epidemiological characteristic of Orofacial clefts and its associated congenital anomalies: Retrospective study. BMC Oral Health 2019, 19, 290. [Google Scholar] [CrossRef] [Green Version]
- Cassina, C.; Papageorgiou, S.N.; Eliades, T. Open versus closed surgical exposure for permanent impacted canines: A systematic review and meta-analyses. Eur. J. Orthod. 2018, 40, 1–10. [Google Scholar] [CrossRef] [PubMed]
- El, H.; Stefanovic, N.; Palomo, J.M.; Palomo, L. Strategies for Managing the Risk of Mucogingival Changes during Impacted Maxillary Canine Treatment. Turk. J. Orthod. 2020, 33, 123–132. [Google Scholar] [CrossRef]
- Incerti-Parenti, S.; Checchi, V.; Ippolito, D.R.; Gracco, A.; Alessandri-Bonetti, G. Periodontal status after surgical-orthodontic treatment of labially impacted canines with different surgical techniques: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 463–472. [Google Scholar] [CrossRef] [PubMed]
- La Monaca, G.; Cristalli, M.P.; Pranno, N.; Galluccio, G.; Annibali, S.; Pippi, R. First and second permanent molars with failed or delayed eruption: Clinical and statistical analyses. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Calasso, S.; Cassetta, M.; Galluccio, G.; Barbato, E. Impacted lower second molars. Dent. Cadmos 2008, 76, 41–54. [Google Scholar]
- Cavuoti, S.; Matarese, G.; Isolac, G.; Abdolreza, J.; Femiano, F.; Perillo, L. Combined orthodontic-surgical management of a transmigrated mandibular canine. Angle Orthod. 2016, 86, 4. [Google Scholar] [CrossRef] [Green Version]
- Ren, A.; Lv, T.; Kang, N.; Zhao, B.; Chen, Y.; Bai, D. Rapid orthodontic tooth movement aided by alveolar surgery in beagles. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 160.e1–160.e10. [Google Scholar] [CrossRef] [PubMed]
- Fu, T.; Liu, S.; Zhao, H.; Cao, M.; Zhang, R. Effectiveness and Safety of Minimally Invasive Orthodontic Tooth Movement Acceleration: A Systematic Review and Meta-analysis. J. Dent. Res. 2019, 98, 1469–1479. [Google Scholar] [CrossRef] [PubMed]
- Darwiche, F.; Khodari, E.; Aljehani, D.; Gujar, A.N.; Baeshen, H.A. Comparison of Effectiveness of Corticotomy-assisted Accelerated Orthodontic Treatment and Conventional Orthodontic Treatment: A Systematic Review. J. Contemp. Dent. Pract. 2020, 21, 701–709. [Google Scholar] [PubMed]
- Kamal, A.T.; Malik, D.E.S.; Fida, M.; Sukhia, R.H. Does periodontally accelerated osteogenic orthodontics improve orthodontic treatment outcome? A systematic review and meta-analysis. Int. Orthod. 2019, 17, 193–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jedliński, M.; Romeo, U.; Del Vecchio, A.; Palaia, G.; Galluccio, G. Comparison of the effects of photobiomodulation with different lasers on orthodontic movement and reduction of the treatment time with fixed appliances in novel scientific reports: A systematic review with meta-analysis(Review). Photobiomodulation Photomed. Laser Surg. 2020, 38, 455–465. [Google Scholar] [CrossRef]
- Impellizzeri, A.; Horodynski, M.; Fusco, R.; Palaia, G.; Polimeni, A.; Romeo, U.; Barbato, E.; Galluccio, G. Photobiomodulation therapy on orthodontic movement: Analysis of preliminary studies with a new protocol. Int. J. Environ. Res. Public Health 2020, 17, 3547. [Google Scholar] [CrossRef]
| Advantages | Disadvantages |
|---|---|
| Maximum Anchoring: The use of a miniscrew, when possible, allows for a maximum anchoring, minimizing side effects. Compliance: The use of TADs and closed NiTi springs requests only a minimum compliance from the patient. Periodontal Advantages: Distant incision reduces the possibility of traumatizing the gingiva of treated teeth; a critical point is the careful subperiosteal dissection, which reduces gingival margin tension during coronal advancement while maintaining integrity and anatomy of the interdental papillae. The placement of the initial incision and the periosteal tunnel causes almost no visible scarring, helping to maximize the aesthetic outcome in this delicate area. Comfort for the Patient: As it is a flapless technique, it is minimally invasive. The patient is also placed in conditions of maintaining proper oral hygiene, given the absence of vestibular orthodontic equipment | Complications Related to the Use of TADS: Disadvantages can be related to failure with the loss of the miniscrew, inflammation of the soft tissue, ulceration, root injury, fracture of the miniscrew, pain, and insensitivity. Second Surgical Phase: Once the impacted tooth has been distalized, a second surgical phase is required to remove the traction devices (closed NiTi spring and miniscrew). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galluccio, G.; Impellizzeri, A.; Pietrantoni, A.; De Stefano, A.; La Monaca, G.; Pippi, R. The VISTA Approach in Canine Disimpaction. Methods Protoc. 2021, 4, 57. https://doi.org/10.3390/mps4030057
Galluccio G, Impellizzeri A, Pietrantoni A, De Stefano A, La Monaca G, Pippi R. The VISTA Approach in Canine Disimpaction. Methods and Protocols. 2021; 4(3):57. https://doi.org/10.3390/mps4030057
Chicago/Turabian StyleGalluccio, Gabriella, Alessandra Impellizzeri, Alessandra Pietrantoni, Adriana De Stefano, Gerardo La Monaca, and Roberto Pippi. 2021. "The VISTA Approach in Canine Disimpaction" Methods and Protocols 4, no. 3: 57. https://doi.org/10.3390/mps4030057
APA StyleGalluccio, G., Impellizzeri, A., Pietrantoni, A., De Stefano, A., La Monaca, G., & Pippi, R. (2021). The VISTA Approach in Canine Disimpaction. Methods and Protocols, 4(3), 57. https://doi.org/10.3390/mps4030057







