Exploring Patient Views and Acceptance of Multiparametric Magnetic Resonance Imaging for the Investigation of Suspected Prostate Cancer (the PACT Study): A Mixed-Methods Study Protocol
Abstract
1. Introduction
1.1. Multiparametric Prostate MRI
1.2. Patient Perceptions of Prostate mpMRI
1.3. Uncertainties of Prostate mpMRI
2. Experimental Design
2.1. Background
2.2. Research Question
2.3. Aims
- Examine the views of men on the mpMRI diagnostic pathway, including its acceptability and associated risks, as compared to the traditional approach of random TRUS-guided biopsy.
- Explore the opinions of men on how clinically significant prostate cancer is currently defined.
2.4. Objectives
- Ascertain the level of acceptability of the mpMRI pathway to men referred with suspected prostate cancer.
- Investigate the extent to which men with suspected prostate cancer are willing to tolerate the current false negative rate associated with mpMRI.
- Describe the factors that may affect whether patients are willing to accept the drawbacks of the modern mpMRI pathway, over those of the traditional systematic TRUS-guided biopsy approach.
- Explore men’s perceptions of different prostate biopsy strategies.
- Elucidate men’s views on what constitutes clinically significant prostate cancer, describing this from a patient perspective.
- Identify potential areas for the development of patient education and support materials, in light of these findings.
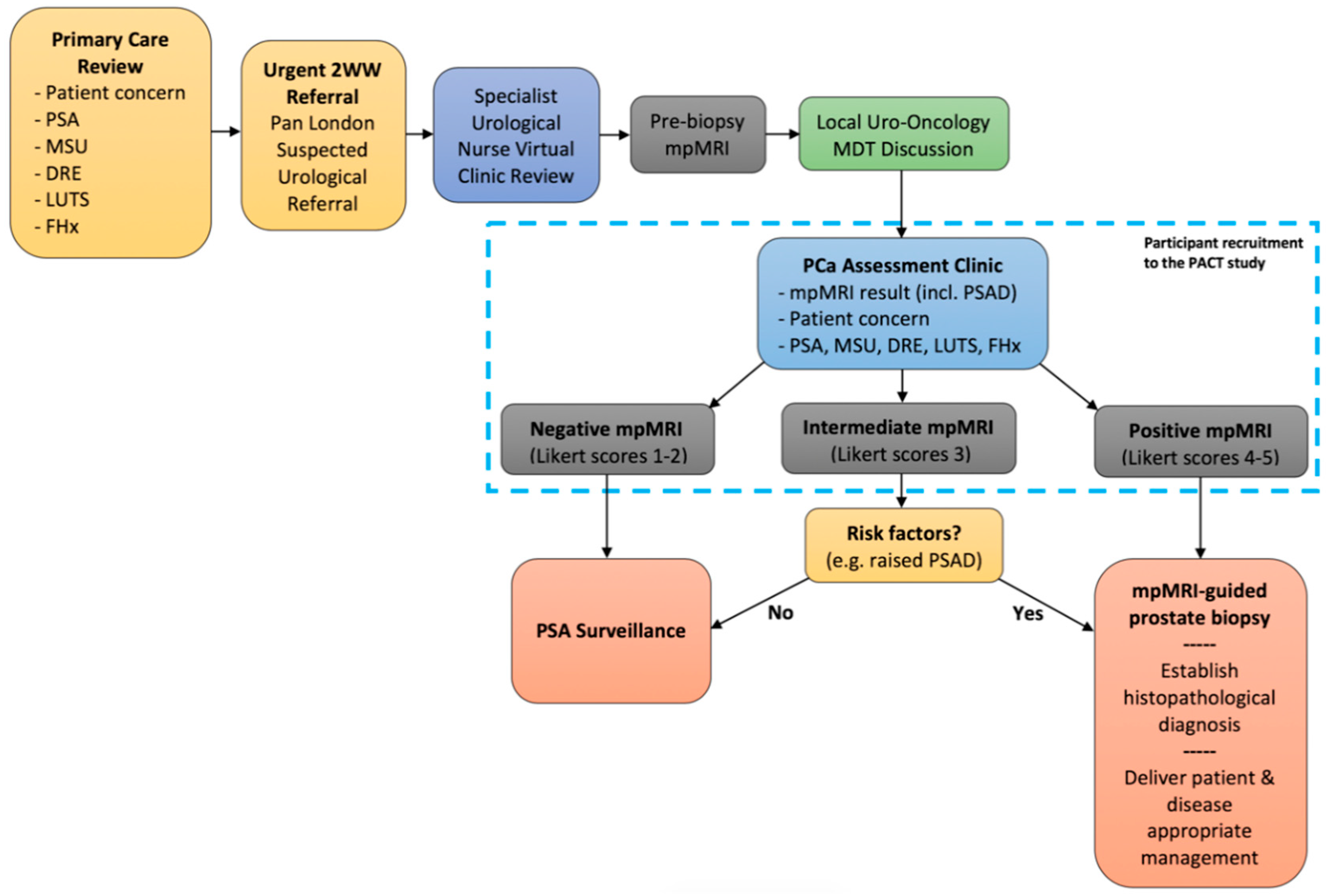
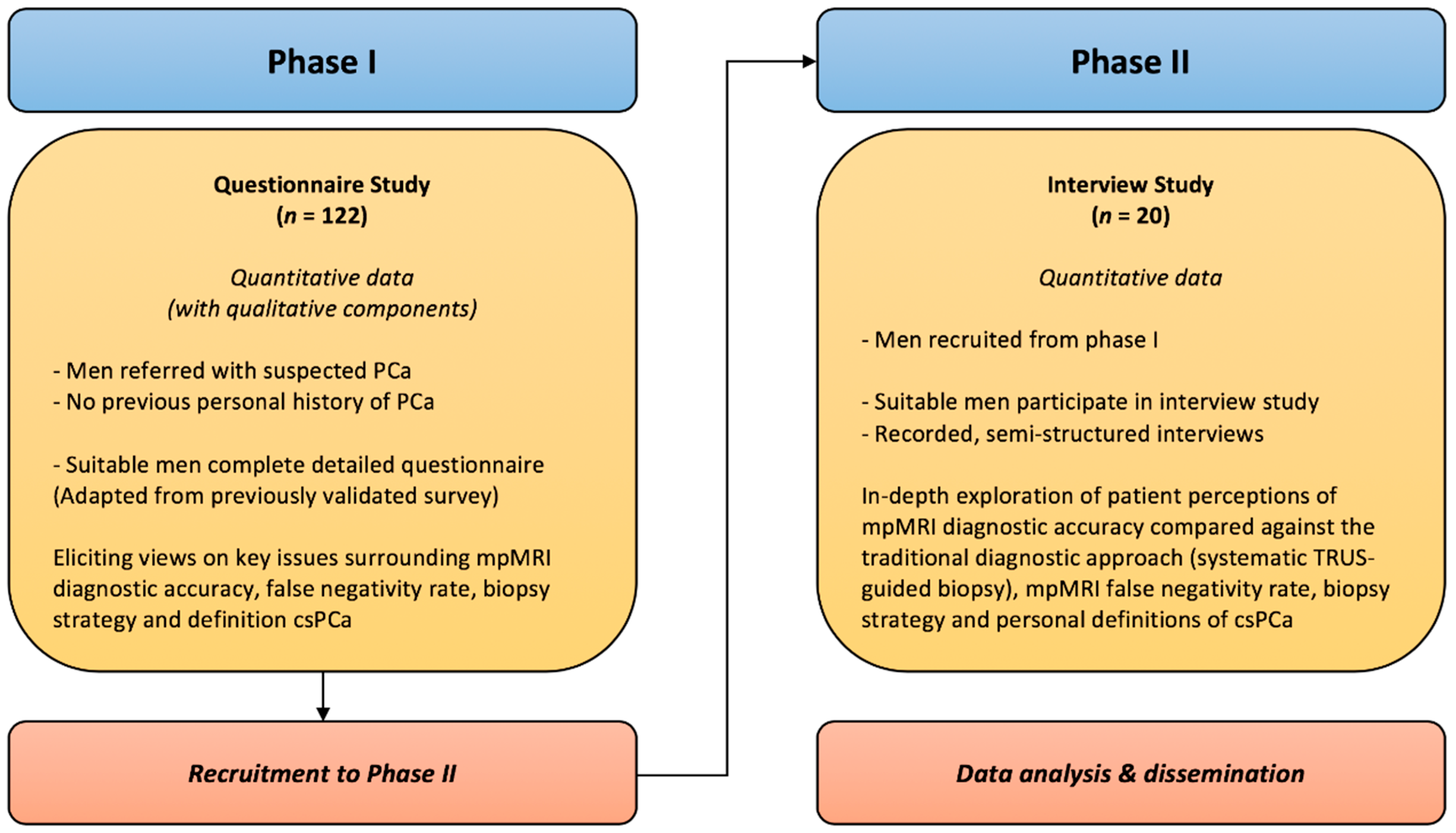
3. Procedure
3.1. Phase I: Questionnaire Study
3.1.1. Inclusion Criteria
- Adult male patients (over 18-years-old).
- Referred with suspected prostate cancer.
- Undergone prostate mpMRI.
- Informed consent given to complete questionnaire.
3.1.2. Exclusion Criteria
- Unable to read, write or understand English.
- Previous diagnosis of prostate cancer.
3.1.3. Recruitment
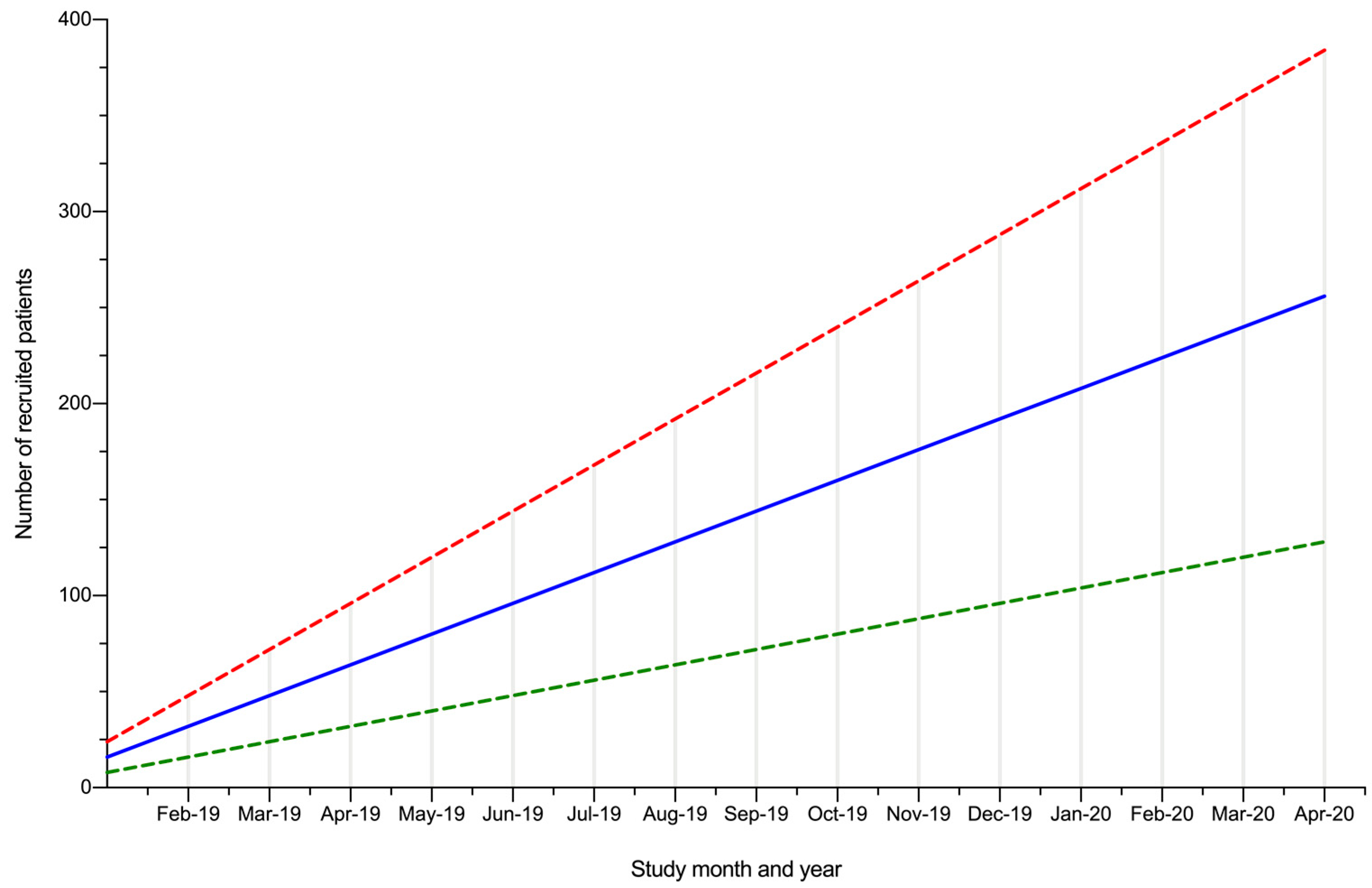
3.1.4. Data Collection
3.2. Phase II: Interview Study
3.2.1. Inclusion Criteria
- Adult male patients (over 18-years-old).
- Referred with suspected prostate cancer.
- Undergone prostate mpMRI.
- Successful completion of the questionnaire in phase I, with informed consent given to be interviewed in phase II.
3.2.2. Exclusion Criteria
- Unable speak or understand English.
- Previous diagnosis of prostate cancer.
- No contact details given during questionnaire completion.
3.2.3. Recruitment
3.2.4. Data Collection
3.3. Data Analysis
3.3.1. Quantitative Analysis
3.3.2. Qualitative Analysis
- Step 1: Transcripts will be read whilst re-listening to audio recordings to check accuracy and build dataset familiarity.
- Step 2: Transcripts will be coded to identify aspects of the data relevant to research objectives.
- Step 3: Codes will be collated into themes.
- Step 4: Themes will be reviewed with the broader research team to ensure code consistency within themes and to avoid overlap between themes.
- Step 5: A thematic map will be developed by refining themes and analysing their relationships.
- Step 6: The qualitative results will be collated and published using the words of participants to illustrate areas of agreement, as well as divergences of views.
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ahmed, H.U.; El-Shater Bosaily, A.; Brown, L.C.; Gabe, R.; Kaplan, R.; Parmar, M.K.; Collaco-Moraes, Y.; Ward, K.; Hindley, R.G.; Freeman, A.; et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): A paired validating confirmatory study. Lancet 2017, 389, 815–822. [Google Scholar] [CrossRef]
- Kasivisvanathan, V.; Rannikko, A.S.; Borghi, M.; Panebianco, V.; Mynderse, L.A.; Vaarala, M.H.; Briganti, A.; Budäus, L.; Hellawell, G.; Hindley, R.G.; et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N. Engl. J. Med. 2018, 378, 1767–1777. [Google Scholar] [CrossRef] [PubMed]
- Wise, J. NICE recommends MRI for suspected prostate cancer to reduce biopsies. BMJ 2018, 363, k5290. [Google Scholar] [CrossRef] [PubMed]
- Loeb, S.; Bjurlin, M.A.; Nicholson, J.; Tammela, T.L.; Penson, D.F.; Carter, H.B.; Carroll, P.; Etzioni, R. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 2014, 65, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- Ukimura, O.; Coleman, J.A.; De la Taille, A.; Emberton, M.; Epstein, J.I.; Freedland, S.J.; Giannarini, G.; Kibel, A.S.; Montironi, R.; Ploussard, G.; et al. Contemporary role of systematic prostate biopsies: Indications, techniques, and implications for patient care. Eur. Urol. 2013, 63, 214–230. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, F.C.; Donovan, J.L.; Lane, J.A.; Mason, M.; Metcalfe, C.; Holding, P.; Davis, M.; Peters, T.J.; Turner, E.L.; Martin, R.M.; et al. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N. Engl. J. Med. 2016, 375, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- Skouteris, V.M.; Crawford, E.D.; Mouraviev, V.; Arangua, P.; Metsinis, M.P.; Skouteris, M.; Zacharopoulos, G.; Stone, N.N. Transrectal ultrasound-guided versus transperineal mapping prostate biopsy: Complication comparison. Rev. Urol. 2018, 20, 19–25. [Google Scholar] [PubMed]
- Wade, J.; Rosario, D.J.; Macefield, R.C.; Avery, K.N.; Salter, C.E.; Goodwin, M.L.; Blazeby, J.M.; Lane, J.A.; Metcalfe, C.; Neal, D.E.; et al. Psychological impact of prostate biopsy: Physical symptoms, anxiety, and depression. J. Clin. Oncol. 2013, 31, 4235–4241. [Google Scholar] [CrossRef] [PubMed]
- Tooker, G.M.; Truong, H.; Pinto, P.A.; Siddiqui, M.M. National survey of patterns employing targeted MRI/US guided prostate biopsy in the diagnosis and staging of prostate cancer. Curr. Urol. 2018, 12, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Bukavina, L.; Tilburt, J.C.; Konety, B.; Shah, N.D.; Gross, C.P.; Yu, J.B.; Schumacher, F.; Kutikov, A.; Smaldone, M.C.; Kim, S.P. Perceptions of prostate MRI and fusion biopsy of radiation oncologists and urologists for patients diagnosed with prostate cancer: Results from a national survey. Eur. Urol. Focus. 2020, 6, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Manley, B.J.; Brockman, J.A.; Raup, V.T.; Fowler, K.J.; Andriole, G.L. Prostate MRI: A national survey of Urologist’s attitudes and perceptions. Int. Braz. J. Urol. 2016, 42, 464–471. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ullrich, T.; Schimmöller, L.; Oymanns, M.; Blondin, D.; Dietzel, F.; Kirchner, J.; Arsov, C.; Rabenalt, R.; Albers, P.; Antoch, G.; et al. Current utilization and acceptance of multiparametric MRI in the diagnosis of prostate cancer. A regional survey. Rofo 2018, 190, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Tallon, D.; Chard, J.; Dieppe, P. Relation between agendas of the research community and the research consumer. Lancet 2000, 355, 2037–2040. [Google Scholar] [CrossRef]
- Rossi, S.H.; Fielding, A.; Blick, C.; Handforth, C.; Brown, J.E.; Stewart, G.D. Setting research priorities in partnership with patients to provide patient-centred urological cancer care. Eur. Urol. 2019, 75, 891–893. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Kazer, M.W.; Bailey, D.E., Jr.; Chipman, J.; Psutka, S.P.; Hardy, J.; Hembroff, L.; Regan, M.; Dunn, R.L.; Crociani, C.; Sanda, M.G.; et al. Uncertainty and perception of danger among patients undergoing treatment for prostate cancer. BJU Int. 2013, 111, E84–E91. [Google Scholar] [CrossRef] [PubMed]
- Sakpal, T.V. Sample size estimation in clinical trial. Perspect. Clin. Res. 2010, 1, 67–69. [Google Scholar] [PubMed]
- Schönenberger, E.; Schnapauff, D.; Teige, F.; Laule, M.; Hamm, B.; Dewey, M. Patient acceptance of noninvasive and invasive coronary angiography. PLoS ONE 2007, 2, e246. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
| Background | Pathway Comparison | Biopsy Strategy | Cancer Significance | Education |
|---|---|---|---|---|
| We have begun using MRI scans to help diagnose prostate cancer and would value your thoughts on this. | Previously, men with suspected prostate cancer would normally have prostate samples taken through the back-passage, without an MRI being performed – this approach could miss up to 50% of important cancers. Today, MRI scans are more readily available and can help us to detect around 80–90% of important tumours (if the MRI is performed before samples are taken). | When we take a prostate sample, we can choose to sample only cancers that we “see” on the MRI scan. This targeted approach has the advantage of diagnosing more “significant cancers” and fewer “insignificant” cancers; however, this does risk missing cancers elsewhere in the prostate. Alternatively, we can choose to sample the “whole prostate” (in addition to sampling the ‘target’) but this has a higher risk of detecting non-harmful cancer, bleeding, retention of urine and discomfort. | There is still no consensus definition of what makes prostate cancer ‘significant.’ However, some cancers are “more aggressive” than others and can spread around the body – these generally benefit from treatment. Others are “less aggressive” and do not spread or cause harm – these generally do not benefit from treatment and treating these cancers may cause more harm than the cancers themselves. | There are lots of information sources for patients and we would value your thoughts on these. |
| Can you tell me what experience you have had of MRI scanning? What do you understand about the use of MRI scans to detect prostate cancer? Are there particular aspects of MRI scanning that appeal to you? Are there any aspects of MRI scanning that you might have a concern about? Would you like to clarify these issues before proceeding? | Any new approach has drawbacks and benefits and the new MRI approach can miss 10–20% of prostate cancers – what do you think of this? How far does this risk worry you? With this in mind, how do you feel about not taking tissue samples at all when the MRI scan appears to be “normal” or shows “no cancer”? Can you tell me how you feel about this compared to the traditional approach? When comparing these two approaches (using MRI or not) which do you think is more appealing? And, why? From your point of view, are there any aspects of either of these approaches that would especially concern you? Given your own experience to date, can you think of any changes or improvements to these two pathway options that you would like to see being made? | Can you tell me, what experience you have had, if any, of prostate biopsy? Do you have any thoughts on which of the two major types of biopsy do you think that you would prefer? And, why is this? If you had an MRI scan that showed possible prostate cancer, would you wish to have: - Only a “target biopsy” (in which around 3–5 samples taken from the suspicious area shown on the MRI scan)? - Or, would you rather have a “targeted and systematic biopsy” (in which approximately 12 other samples are also taken from the rest of the prostate at the same time)? And why would you feel this way? As a related question, what proportion of important cancers would you be willing to miss? | If you were diagnosed with prostate cancer, which aspect of the cancer would be most important to you? Would you be more concerned about the effect on your quality of life (e.g., developing unpleasant symptoms, such as problems with urination) or your life expectancy (how long you might live for)? And, why might you feel this way? If you had prostate cancer, do you think you would you like to know about the potential danger posed by your cancer? In what way could we best provide such information to you? Do you think you would want to know about every single cancer that is present in your prostate (even “less aggressive” cancers) or do you think you would only want to know only about “more aggressive” cancers? Why would you feel this way? | What format is normally best for you when it comes to information about your health? Are there any aspects of this topic that you would like to have more information on? Can you summarise any key lessons for us about your diagnostic experience to date? |
| MRI magnetic resonance imaging. | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Norris, J.M.; Kasivisvanathan, V.; Allen, C.; Ball, R.; Freeman, A.; Ghei, M.; Kirkham, A.; Whitaker, H.C.; Kelly, D.; Emberton, M. Exploring Patient Views and Acceptance of Multiparametric Magnetic Resonance Imaging for the Investigation of Suspected Prostate Cancer (the PACT Study): A Mixed-Methods Study Protocol. Methods Protoc. 2020, 3, 26. https://doi.org/10.3390/mps3020026
Norris JM, Kasivisvanathan V, Allen C, Ball R, Freeman A, Ghei M, Kirkham A, Whitaker HC, Kelly D, Emberton M. Exploring Patient Views and Acceptance of Multiparametric Magnetic Resonance Imaging for the Investigation of Suspected Prostate Cancer (the PACT Study): A Mixed-Methods Study Protocol. Methods and Protocols. 2020; 3(2):26. https://doi.org/10.3390/mps3020026
Chicago/Turabian StyleNorris, Joseph M., Veeru Kasivisvanathan, Clare Allen, Rhys Ball, Alex Freeman, Maneesh Ghei, Alex Kirkham, Hayley C. Whitaker, Daniel Kelly, and Mark Emberton. 2020. "Exploring Patient Views and Acceptance of Multiparametric Magnetic Resonance Imaging for the Investigation of Suspected Prostate Cancer (the PACT Study): A Mixed-Methods Study Protocol" Methods and Protocols 3, no. 2: 26. https://doi.org/10.3390/mps3020026
APA StyleNorris, J. M., Kasivisvanathan, V., Allen, C., Ball, R., Freeman, A., Ghei, M., Kirkham, A., Whitaker, H. C., Kelly, D., & Emberton, M. (2020). Exploring Patient Views and Acceptance of Multiparametric Magnetic Resonance Imaging for the Investigation of Suspected Prostate Cancer (the PACT Study): A Mixed-Methods Study Protocol. Methods and Protocols, 3(2), 26. https://doi.org/10.3390/mps3020026






