Co-Designing an Intervention to Increase HIV Testing Uptake with Women from Indonesia At-Risk of HIV: Protocol for a Participatory Action Research Study
Abstract
:1. Introduction
2. Aims and Objectives
- Identify and assess the pathways and enablers to HIV testing among women from Indonesia
- Record and synthesize the use of a co-design process in developing an intervention
- Determine the critical elements of a co-designed intervention to increase HIV testing uptake among women from Indonesia
- Implement and evaluate a co-designed intervention to increase HIV testing uptake among women from Indonesia
- Review the utility of a participatory action research approach in addressing HIV with women from Indonesia
- Synthesize findings of the intervention and provide recommendations on appropriate strategies to prevent and manage HIV among women from Indonesia.
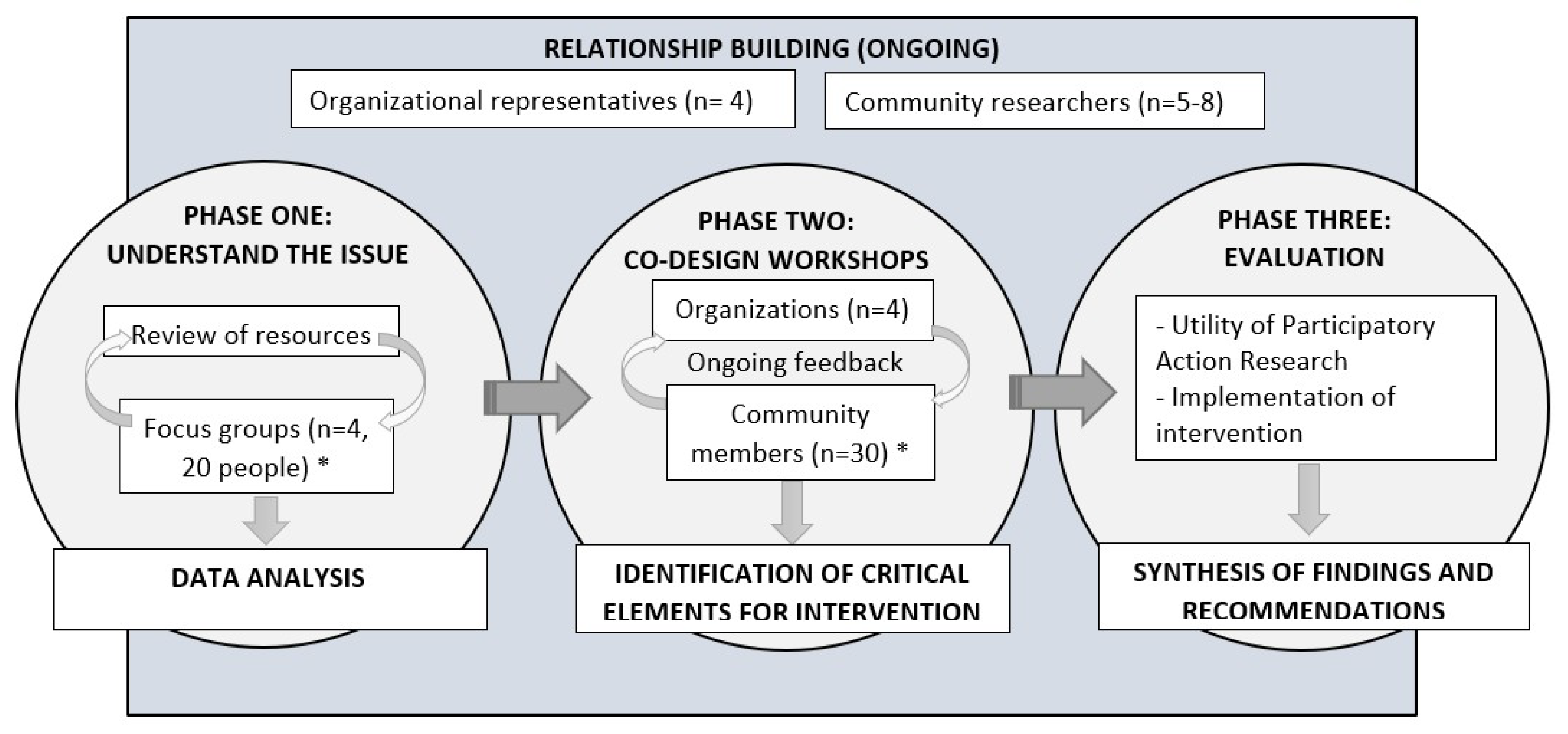
3. Methods and Analysis
Partnerships
4. Phase One
4.1. Review of Resources
4.2. Focus Groups
4.2.1. Data Collection
4.2.2. Data Analysis
5. Phase Two
5.1. Sampling Strategy and Participants
5.2. Data Collection and Analysis
6. Phase Three
Sampling Strategy and Participants
7. Ethical Considerations
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- The Kirby Institute. HIV, Viral Hepatitis and Sexually Transmissible Infections in Australia, Annual Surveillance Report 2017; The Kirby Institute, UNSW Sydney: Sydney, Australia, 2017. [Google Scholar]
- The Kirby Institute. HIV, Viral Hepatitis and Sexually Transmissible Infections in Australia, Annual Surveillance Report 2014; The Kirby Institute, UNSW Sydney: Sydney, Australia, 2014. [Google Scholar]
- Crawford, G.; Lobo, R.; Brown, G.; Langdon, P. HIV and Mobility in Australia: Road Map for Action; Western Australian Centre for Health Promotion Research and Australian Research Centre in Sex, Health and Society: Perth, Australia, 2014. [Google Scholar]
- United Nations Department of Economic and Social Affairs Population Division. International Migration Report 2017: Highlights (ST/ESA/SER.A/404); United Nations: New York, NY, USA, 2017. [Google Scholar]
- Australian Bureau of Statistics. 3412.0—Migration, Australia, 2016-17. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/3412.0/ (accessed on 5 March 2019).
- Carrington, K.; McIntosh, A.; Walmsley, J. The Social Costs and Benefits of Migration into Australia; Commonwealth of Australia: Canberra, Australia, 2007. [Google Scholar]
- Lee, E.S. A theory of migration. Demography 1966, 3, 47–57. [Google Scholar] [CrossRef]
- Wickramage, K.; Vearey, J.; Zwi, A.B.; Robinson, C.; Knipper, M. Migration and health: A global public health research priority. BMC Public Health 2018, 18, 987. [Google Scholar] [CrossRef] [PubMed]
- Viruell-Fuentes, E.A.; Miranda, P.Y.; Abdulrahim, S. More than culture: Structural racism, intersectionality theory, and immigrant health. Soc. Sci. Med. 2012, 75, 2099–2106. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Health of Migrants—The Way Forward; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Caperchione, C.M.; Kolt, G.S.; Mummery, W.K. Physical Activity in Culturally and Linguistically Diverse Migrant Groups to Western Society. Sports Med. 2012, 39, 167–177. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Migration. HIV and Population Mobility; IOM: Grand Saconne, Switzerland, 2010. [Google Scholar]
- Haour-Knipe, M.; Zalduondo, B.; Samuels, F.; Molesworth, K.; Sehgal, S. HIV and “People on the Move”: Six Strategies to Reduce Risk and Vulnerability during the Migration Process. Int. Migr. 2014, 52, 9–25. [Google Scholar] [CrossRef]
- International Organization for Migration. IOM Position Paper on HIV/AIDS and Migration; IOM: Grand Saconne, Switzerland, 2002. [Google Scholar]
- Palmer, R.; Lemoh, C.; Tham, R.; Hakim, S.; Biggs, B. Sudanese women living in Victoria, Australia: Health-information-seeking behaviours and the availability, effectiveness and appropriateness of HIV/AIDS information. Divers. Health Care 2009, 6, 109–120. [Google Scholar]
- Xiridou, M.; van Veen, M.; Coutinho, R.; Prins, M. Can migrants from high-endemic countries cause new HIV outbreaks among heterosexuals in low-endemic countries? AIDS 2010, 24, 2081–2088. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-del Arco, D.; Monge, S.; Azcoaga, A.; Rio, I.; Hernando, V.; Gonzalez, C.; Alejos, B.; Caro, A.M.; Perez-Cachafeiro, S.; Ramirez-Rubio, O.; et al. HIV testing and counselling for migrant populations living in high-income countries: A systematic review. Eur. J. Public Health 2013, 23, 1039–1045. [Google Scholar] [CrossRef]
- Zhou, Y.R.; Coleman, W.D.; Huang, Y.; Sinding, C.; Wei, W.; Gahagan, J.; Micollier, E.; Su, H.H. Exploring the Intersections of Transnationalism, Sexuality and HIV Risk. Cult. Health Sex. 2017, 19, 645–652. [Google Scholar] [CrossRef]
- Mullens, A.B.; Kelly, J.; Debattista, J.; Phillips, T.M.; Gu, Z.; Siggins, F. Exploring HIV risks, testing and prevention among sub-Saharan African community members in Australia. Int. J. Equity Health 2018, 17, 62. [Google Scholar] [CrossRef]
- McGregor, S.; Mlambo, E.; Gunaratnam, P.; Wilson, D.; Guy, R. HIV Knowledge, Risk Behaviour and Testing: A Community Survey in People from Culturally and Linguistically Diverse (CALD) Backgrounds in NSW, Australia; The Kirby Institute, UNSW Sydney: Sydney, Australia, 2017. [Google Scholar]
- Llácer, A.; Zunzunegui, M.V.; del Amo, J.; Mazarrasa, L.; Bolůmar, F. The contribution of a gender perspective to the understanding of migrants’ health. J. Epidemiol. Community Health 2007, 61, ii4–ii10. [Google Scholar] [CrossRef]
- Hach, M. Common Threads: The Sexual and Reproductive Health Experiences of Immigrant and Refugee Women in Australia; Multicultural Centre for Women’s Health: Melbourne, Australia, 2012. [Google Scholar]
- Rade, D.; Crawford, G.; Lobo, R.; Gray, C.; Brown, G. Sexual Health Help-Seeking Behavior among Migrants from Sub-Saharan Africa and South East Asia living in High Income Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 1311. [Google Scholar] [CrossRef]
- Mengesha, Z.B.; Dune, T.; Perz, J. Culturally and linguistically diverse women’s views and experiences of accessing sexual and reproductive health care in Australia: A systematic review. Sex. Health 2016, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Mengesha, Z.B.; Perz, J.; Dune, T.; Ussher, J. Refugee and migrant women’s engagement with sexual and reproductive health care in Australia: A socio-ecological analysis of health care professional perspectives. PLoS ONE 2017, 12, e0181421. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M. Late diagnosis of HIV infection: Major consequences and missed opportunities. Curr. Opin. Infect. Dis. 2008, 21, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Department of Health Australian Government. Eighth National HIV Strategy 2018–2022; Commonwealth of Australia: Canberra, Australia, 2018. [Google Scholar]
- Blondell, S.J.; Kitter, B.; Griffin, M.P.; Durham, J. Barriers and facilitators to HIV testing in migrants in high-income countries: A systematic review. AIDS Behav. 2015, 19, 2012–2024. [Google Scholar] [CrossRef]
- Aung, E.; Blondell, S.J.; Durham, J. Interventions for Increasing HIV Testing Uptake in Migrants: A Systematic Review of Evidence. AIDS Behav. 2017. [Google Scholar] [CrossRef]
- Körner, H. ‘If I Had My Residency I Wouldn’t Worry’: Negotiating Migration and HIV in Sydney, Australia. Ethn. Health 2007, 12, 205–225. [Google Scholar] [CrossRef] [PubMed]
- Persson, A.; Brown, G.; McDonald, A.; Körner, H. Transmission and prevention of HIV among heterosexual populations in Australia. AIDS Educ. Prev. 2014, 26, 245–255. [Google Scholar] [CrossRef]
- Durand, M.-A.; Carpenter, L.; Dolan, H.; Bravo, P.; Mann, M.; Bunn, F.; Elwyn, G. Do Interventions Designed to Support Shared Decision-Making Reduce Health Inequalities? A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e94670. [Google Scholar] [CrossRef] [PubMed]
- Quay, T.A.; Frimer, L.; Janssen, P.A.; Lamers, Y. Barriers and facilitators to recruitment of South Asians to health research: A scoping review. BMJ Open 2017, 7. [Google Scholar] [CrossRef]
- Elam, G.; Fenton, K. Researching sensitive issues and ethnicity: Lessons from sexual health. Ethn. Health 2003, 8, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Agu, J.; Lobo, R.; Crawford, G.; Chigwada, B. Migrant Sexual Health Help-Seeking and Experiences of Stigmatization and Discrimination in Perth, Western Australia: Exploring Barriers and Enablers. Int. J. Environ. Res. Public Health 2016, 13, 485. [Google Scholar] [CrossRef] [PubMed]
- Persson, A.; Newman, C. Making monsters: Heterosexuality, crime and race in recent Western media coverage of HIV. Sociol. Health Illn. 2008, 30, 632–646. [Google Scholar] [CrossRef] [PubMed]
- Ganann, R. Opportunities and challenges associated with engaging immigrant women in participatory action research. J. Immigr. Minor. Health 2013, 15, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Do, B. Health needs of migrant Vietnamese women in South-West Brisbane: An exploratory study. Aust. J. Soc. Issues 2003, 38, 247. [Google Scholar]
- Drummond, P.; Mizan, A.; Brocx, K.; Wright, B. Barriers to Accessing Health Care Services for West African Refugee Women Living in Western Australia. Health Care Women Int. 2011, 32, 206–224. [Google Scholar] [CrossRef]
- Wilson, D.; Neville, S. Culturally safe research with vulnerable populations. Contemp. Nurse 2009, 33, 69–79. [Google Scholar] [CrossRef]
- Cole, E.R. Intersectionality and research in psychology. Am. Psychol. 2009, 64, 170–180. [Google Scholar] [CrossRef]
- Reeders, D. Double Trouble? The Health Needs of Culturally Diverse MSM; Centre for Culture, Ethnicity & Health: Melbourne, Australia, 2010. [Google Scholar]
- George, M.A.; Daniel, M.; Green, L.W. Appraising and Funding Participatory Research in Health Promotion. Int. Q. Community Health Educ. 2006, 26, 171–187. [Google Scholar] [CrossRef]
- Baum, F.; Macdougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Health 2006, 60, 854. [Google Scholar] [CrossRef]
- Baum, F.E. Power and glory: Applying participatory action research in public health. SciELO Public Health 2016. [Google Scholar] [CrossRef] [PubMed]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of community-based research: Assessing partnership approaches to improve public health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef] [PubMed]
- Eyles, H.; Jull, A.; Dobson, R.; Firestone, R.; Whittaker, R.; Te Morenga, L.; Goodwin, D.; Mhurchu, C.N. Co-design of mHealth Delivered Interventions: A Systematic Review to Assess Key Methods and Processes. Curr. Nutr. Rep. 2016, 5, 160–167. [Google Scholar] [CrossRef]
- Thabrew, H.; Fleming, T.; Hetrick, S.; Merry, S. Co-design of eHealth Interventions with Children and Young People. Front. Psychiatry 2018, 9. [Google Scholar] [CrossRef]
- Leask, C.F.; Sandlund, M.; Skelton, D.A.; Altenburg, T.M.; Cardon, G.; Chinapaw, M.J.M.; De Bourdeaudhuij, I.; Verloigne, M.; Chastin, S.F.M.; on behalf of the GrandStand, S.S.; et al. Framework, principles and recommendations for utilising participatory methodologies in the co-creation and evaluation of public health interventions. Res. Involv. Engagem. 2019, 5, 2. [Google Scholar] [CrossRef]
- Potvin, L.; Cargo, M.; McComber, A.M.; Delormier, T.; Macaulay, A.C. Implementing participatory intervention and research in communities: Lessons from the Kahnawake Schools Diabetes Prevention Project in Canada. Soc. Sci. Med. 2003, 56, 1295–1305. [Google Scholar] [CrossRef]
- Te Morenga, L.; Pekepo, C.; Corrigan, C.; Matoe, L.; Mules, R.; Goodwin, D.; Dymus, J.; Tunks, M.; Grey, J.; Humphrey, G. Co-designing an mHealth tool in the New Zealand Māori community with a “Kaupapa Māori” approach. AlterN. An Int. J. Indig. Peoples 2018, 14, 90–99. [Google Scholar] [CrossRef]
- McIntyre, A. Participatory Action Research; Sage Publications: Saunders Oaks, CA, USA, 2007. [Google Scholar]
- Liamputtong, P. Researching the Vulnerable: A Guide to Sensitive Research Methods; Sage Publications: London, UK, 2006. [Google Scholar]
- Kindon, S.; Pain, R.; Kesby, M. Participatory Action Research Approaches and Methods: Connecting People, Participation and Place; Routledge: Abington, Thames, UK, 2007. [Google Scholar]
- Minkler, M. Using Participatory Action Research to build Healthy Communities. Public Health Rep. 2000, 115, 191. [Google Scholar] [CrossRef]
- Minkler, M.; Wallerstein, N. Community Based Participatory Research for Health/Edited by Meredith Minkler and Nina Wallerstein; Foreword by Budd Hall; Jossey-Bass: San Francisco, CA, USA, 2003. [Google Scholar]
- International HIV/AIDS Alliance and the Global Network of People Living with HIV. Greater Involvement of People Living with HIV; International HIV/AIDS Alliance: Brighton, UK, 2010. [Google Scholar]
- Salway, S.; Chowbey, P.; Such, E.; Ferguson, B. Researching health inequalities with Community Researchers: Practical, methodological and ethical challenges of an ‘inclusive’ research approach. Res. Involv. Engagem. 2015, 1, 9. [Google Scholar] [CrossRef]
- Stringer, E.T. Action Research/Ernest T. Stringer, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2007. [Google Scholar]
- Kaphingst, K.A.; Kreuter, M.W.; Casey, C.; Leme, L.; Thompson, T.; Cheng, M.-R.; Jacobsen, H.; Sterling, R.; Oguntimein, J.; Filler, C.; et al. Health Literacy INDEX: Development, Reliability, and Validity of a New Tool for Evaluating the Health Literacy Demands of Health Information Materials. J. Health Commun. 2012, 17, 203–221. [Google Scholar] [CrossRef] [PubMed]
- Orel, N.A.; Spence, M.; Steele, J. Getting the Message Out to Older Adults: Effective HIV Health Education Risk Reduction Publications. J. Appl. Gerontol. 2005, 24, 490–508. [Google Scholar] [CrossRef]
- Katchmarchi, A.B.; Taliaferro, A.R.; Kipfer, H.J. A document analysis of drowning prevention education resources in the United States. Int. J. Inj. Control Saf. Promot. 2018, 25, 78–84. [Google Scholar] [CrossRef]
- Yin, R.K. Qualitative Research from Start to Finish; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Tajfel, H.; Turner, J.C. An integrative theory of intergroup conflict. Soc. Psychol. Intergr. Relat. 1979, 33, 74. [Google Scholar]
- Cox, C.M.; Babalola, S.; Kennedy, C.E.; Mbwambo, J.; Likindikoki, S.; Kerrigan, D. Determinants of concurrent sexual partnerships within stable relationships: A qualitative study in Tanzania. BMJ Open 2014, 4, e003680. [Google Scholar] [CrossRef]
- Culley, L.; Hudson, N.; Rapport, F. Using focus groups with minority ethnic communities: Researching infertility in British South Asian communities. Qual. Health Res. 2007, 17, 102–112. [Google Scholar] [CrossRef]
- Dias, S.; Gama, A.; Rocha, C. Immigrant women’s perceptions and experiences of health care services: Insights from a focus group study. J. Public Health 2010, 18, 489–496. [Google Scholar] [CrossRef]
- Collaboration for Evidence Research and Impact in Public Health. “I Want to Test But I’m Afraid”: Barriers to HIV Testing among People Born in South. East. Asia and Sub-Saharan Africa: Final Report; Curtin University: Perth, Australia, 2018. [Google Scholar]
- Forrest, J.I.; Stevenson, B.; Rich, A.; Michelow, W.; Pai, J.; Jollimore, J.; Raymond, H.F.; Moore, D.; Hogg, R.S.; Roth, E.A. Community mapping and respondent-driven sampling of gay and bisexual men’s communities in Vancouver, Canada. Cult. Health Sex. 2014, 16, 288–301. [Google Scholar] [CrossRef]
- Amsden, J.; VanWynsberghe, R. Community mapping as a research tool with youth. Action Res. 2005, 3, 357–381. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Tetui, M.; Coe, A.-B.; Hurtig, A.-K.; Bennett, S.; Kiwanuka, S.N.; George, A.; Kiracho, E.E. A participatory action research approach to strengthening health managers’ capacity at district level in Eastern Uganda. Health Res. Policy Syst. 2017, 15, 110. [Google Scholar] [CrossRef]
- QSR International Pty Ltd. NVivo qualitative data analysis Software, Version 11; QSR International Pty Ltd.: Doncaster, Australia, 2016. [Google Scholar]
- Bazeley, P. Analysing qualitative data: More than ‘identifying themes’. Malays. J. Qual. Res. 2009, 2, 6–22. [Google Scholar]
- Lin, I.B.; O’Sullivan, P.B.; Coffin, J.A.; Mak, D.B.; Toussaint, S.; Straker, L.M. Disabling chronic low back pain as an iatrogenic disorder: A qualitative study in Aboriginal Australians. BMJ Open 2013, 3. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Jackson, C.; Shaw, S.; Janamian, T. Achieving Research Impact through Co-creation in Community-Based Health Services: Literature Review and Case Study. Milbank Q. 2016, 94, 392–429. [Google Scholar] [CrossRef]
- Choudhry, U.K.; Jandu, S.; Mahal, J.; Singh, R.; Sohi-Pabla, H.; Mutta, B. Health Promotion and Participatory Action Research with South Asian Women. J. Nurs. Scholarsh. 2002, 34, 75–81. [Google Scholar] [CrossRef]
- Crane, P.; O’Regan, M. On PAR: Using participatory action research to improve early intervention; Department of Families, Housing, Community Services and Indigenous Affairs: Canberra, Australia, 2010. [Google Scholar]
- Kelly, P.J. Practical Suggestions for Community Interventions Using Participatory Action Research. Public Health Nurs. 2005, 22, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Collie, P.; Liu, J.; Podsiadlowski, A.; Kindon, S. You can’t clap with one hand: Learnings to promote culturally grounded participatory action research with migrant and former refugee communities. Int. J. Intercult. Relat. 2010, 34, 141–149. [Google Scholar] [CrossRef]
- Morisky, D.E.; Ang, A.; Coly, A.; Tiglao, T.V. A model HIV/AIDS risk reduction programme in the Philippines: A comprehensive community-based approach through participatory action research. Health Promot. Int. 2004, 19, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Orsmond, G.I.; Cohn, E.S. The distinctive features of a feasibility study: Objectives and guiding questions. OTJR Occup. Particip. Health 2015, 35, 169–177. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Ridde, V. Need for more and better implementation science in global health. BMJ Glob. Health 2016, 1. [Google Scholar] [CrossRef]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm. Policy Ment. Health 2011, 38, 65–76. [Google Scholar] [CrossRef]
- Tetui, M.; Coe, A.-B.; Hurtig, A.-K.; Ekirapa-Kiracho, E.; Kiwanuka, S.N. Experiences of using a participatory action research approach to strengthen district local capacity in Eastern Uganda. Glob. Health Action 2017, 10, 1346038. [Google Scholar] [CrossRef]
- Van Staa, A.; Jedeloo, S.; Latour, J.M.; Trappenburg, M.J. Exciting but exhausting: Experiences with participatory research with chronically ill adolescents. Health Expect. Int. J. Public Particip. Health Care Health Policy 2010, 13, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.M.; D’Antoine, H.A.; France, K.E.; McKenzie, A.E.; Henley, N.; Bartu, A.E.; Elliott, E.J.; Bower, C. Collaborating with consumer and community representatives in health and medical research in Australia: Results from an evaluation. Health Res. Policy Syst. 2011, 9, 18. [Google Scholar] [CrossRef]
- Butterfoss, F.D. Process evaluation for community participation. Annu. Rev. Public Health 2006, 27, 323–340. [Google Scholar] [CrossRef] [PubMed]
- Hergenrather, K.C.; Rhodes, S.D.; Cowan, C.A.; Bardhoshi, G.; Pula, S. Photovoice as a community-based participatory research: A qualitative review. Am. J. Health Behav. 2009, 33, 686–698. [Google Scholar] [CrossRef]
- Heslop, C.W.; Burns, S.; Lobo, R.; McConigley, R. Developing a framework for community-based sexual health interventions for youth in the rural setting: Protocol for a participatory action research study. BMJ Open 2017, 7, e013368. [Google Scholar] [CrossRef]
- Chen, S.; Poland, B.; Skinner, H.A. Youth voices: Evaluation of participatory action research. Can. J. Program. Eval. 2007, 22, 125. [Google Scholar]
- Plumb, M.; Collins, N.; Cordeiro, J.N.; Kavanaugh-Lynch, M. Assessing process and outcomes: Evaluating community-based participatory research. Prog. Community Health Partnersh. Res. Educ. Action 2008, 2, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Fenton, K.A.; Chinouya, M.; Davidson, O.; Copas, A.; Team, M.S. HIV testing and high risk sexual behaviour among London’s migrant African communities: A participatory research study. Sex. Transm. Infect. 2002, 78, 241–245. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gray, C.; Crawford, G.; Lobo, R.; Maycock, B. Co-Designing an Intervention to Increase HIV Testing Uptake with Women from Indonesia At-Risk of HIV: Protocol for a Participatory Action Research Study. Methods Protoc. 2019, 2, 41. https://doi.org/10.3390/mps2020041
Gray C, Crawford G, Lobo R, Maycock B. Co-Designing an Intervention to Increase HIV Testing Uptake with Women from Indonesia At-Risk of HIV: Protocol for a Participatory Action Research Study. Methods and Protocols. 2019; 2(2):41. https://doi.org/10.3390/mps2020041
Chicago/Turabian StyleGray, Corie, Gemma Crawford, Roanna Lobo, and Bruce Maycock. 2019. "Co-Designing an Intervention to Increase HIV Testing Uptake with Women from Indonesia At-Risk of HIV: Protocol for a Participatory Action Research Study" Methods and Protocols 2, no. 2: 41. https://doi.org/10.3390/mps2020041
APA StyleGray, C., Crawford, G., Lobo, R., & Maycock, B. (2019). Co-Designing an Intervention to Increase HIV Testing Uptake with Women from Indonesia At-Risk of HIV: Protocol for a Participatory Action Research Study. Methods and Protocols, 2(2), 41. https://doi.org/10.3390/mps2020041





