Long-Term Neurological Outcomes of Adult Patients with Phenylketonuria before and after Newborn Screening in Japan
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NBS | newborn screening |
| PKU | phenylketonuria |
| PAH | phenylalanine hydroxylase |
| Phe | phenylalanine |
| BH4 | tetrahydrobiopterin |
| HPA | hyperphenylalaninemia; |
| IQ | intelligence quotient |
References
- Mitchell, J.J.; Trakadis, Y.J.; Scriver, C.R. Phenylalanine hydroxylase deficiency. Genet. Med. 2011, 13, 697–707. [Google Scholar] [CrossRef]
- Ozalp, I.; Coşkun, T.; Tokatli, A.; Kalkanoğlu, H.S.; Dursun, A.; Tokol, S.; Köksal, G.; Ozgüc, M.; Köse, R. Newborn PKU screening in Turkey: At present and organization for future. Turk. J. Pediatr. 2001, 43, 97–101. [Google Scholar] [PubMed]
- Vockley, J.; Andersson, H.C.; Antshel, K.M.; Braverman, N.E.; Burton, B.K.; Frazier, D.M.; Mitchell, J.; Smith, W.E.; Thompson, B.H.; Berry, S.A. Phenylalanine hydroxylase deficiency: Diagnosis and management guideline. Genet. Med. 2014, 16, 188–200. [Google Scholar] [PubMed]
- Shibata, N.; Hasegawa, Y.; Yamada, K.; Kobayashi, H.; Purevsuren, J.; Yang, Y.; Dung, V.C.; Khanh, N.N.; Verma, I.C.; Bijarnia-Mahay, S.; et al. Diversity in the incidence and spectrum of organic acidemias, fatty acid oxidation disorders, and amino acid disorders in Asian countries: Selective screening vs. expanded newborn screening. Mol. Genet. Metab. Rep. 2018, 16, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Aoki, K. Long term follow-up of patients with inborn errors of metabolism detected by the newborn screening program in Japan. Southeast Asian J. Trop. Med. Public Health 2003, 34 (Suppl. S3), 19–23. [Google Scholar] [PubMed]
- Lord, J.; Thomason, M.J.; Littlejohns, P.; Chalmers, R.A.; Bain, M.D.; Addison, G.M.; Wilcox, A.H.; Seymour, C.A. Secondary analysis of economic data: A review of cost-benefit studies of neonatal screening for phenylketonuria. J. Epidemiol. Community Health 1999, 53, 179–186. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dhondt, J.L.; Farriaux, J.P.; Sailly, J.C.; Lebrun, T. Economic evaluation of cost-benefit ratio of neonatal screening procedure for phenylketonuria and hypothyroidism. J. Inherit. Metab. Dis. 1991, 14, 633–639. [Google Scholar] [CrossRef]
- Koch, R.; Burton, B.; Hoganson, G.; Peterson, R.; Rhead, W.; Rouse, B.; Scott, R.; Wolff, J.; Stern, A.M.; Guttler, F.; et al. Phenylketonuria in adulthood: A collaborative study. J. Inherit. Metab. Dis. 2002, 25, 333–346. [Google Scholar] [CrossRef] [PubMed]
- Moyle, J.J.; Fox, A.M.; Arthur, M.; Bynevelt, M.; Burnett, J.R. Meta-analysis of neuropsychological symptoms of adolescents and adults with PKU. Neuropsychol. Rev. 2007, 17, 91–101. [Google Scholar] [CrossRef]
- Waisbren, S.E.; Noel, K.; Fahrbach, K.; Cella, C.; Frame, D.; Dorenbaum, A.; Levy, H. Phenylalanine blood levels and clinical outcomes in phenylketonuria: A systematic literature review and meta-analysis. Mol. Genet. Metab. 2007, 92, 63–70. [Google Scholar] [CrossRef]
- Burton, B.K.; Leviton, L.; Vespa, H.; Coon, H.; Longo, N.; Lundy, B.D.; Johnson, M.; Angelino, A.; Hamosh, A.; Bilder, D. A diversified approach for PKU treatment: Routine screening yields high incidence of psychiatric distress in phenylketonuria clinics. Mol. Genet. Metab. 2013, 108, 8–12. [Google Scholar] [CrossRef]
- Antshel, K.M. ADHD, learning, and academic performance in phenylketonuria. Mol. Genet. Metab. 2010, 99 (Suppl. S1), S52–S58. [Google Scholar] [CrossRef] [PubMed]
- Aoki, K.; Ohwada, M.; Kitagawa, T. Long-term follow-up study of patients with phenylketonuria detected by the newborn screening programme in Japan. J. Inherit. Metab. Dis. 2007, 30, 608. [Google Scholar] [CrossRef] [PubMed]
- Aoki, K.; Wada, Y. Outcome of the patients detected by newborn screening in Japan. Acta Paediatr. Jpn. 1988, 30, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Trefz, F.; Maillot, F.; Motzfeldt, K.; Schwarz, M. Adult phenylketonuria outcome and management. Mol. Genet. Metab. 2011, 104, S26–S30. [Google Scholar] [CrossRef] [PubMed]
- Burlina, A.P.; Lachmann, R.H.; Manara, R.; Cazzorla, C.; Celato, A.; van Spronsen, F.J.; Burlina, A. The neurological and psychological phenotype of adult patients with early-treated phenylketonuria: A systematic review. J. Inherit. Metab. Dis. 2019, 42, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Nardecchia, F.; Manti, F.; Chiarotti, F.; Carducci, C.; Carducci, C.; Leuzzi, V. Neurocognitive and neuroimaging outcome of early treated young adult PKU patients: A longitudinal study. Mol. Genet. Metab. 2015, 115, 84–90. [Google Scholar] [CrossRef]
- Van Wegberg, A.M.J.; MacDonald, A.; Ahring, K.; Bélanger-Quintana, A.; Blau, N.; Bosch, A.M.; Burlina, A.; Campistol, J.; Feillet, F.; Giżewska, M.; et al. The complete European guidelines on phenylketonuria: Diagnosis and treatment. Orphanet J. Rare Dis. 2017, 12, 162. [Google Scholar] [CrossRef]
- Hofman, D.L.; Champ, C.L.; Lawton, C.L.; Henderson, M.; Dye, L. A systematic review of cognitive functioning in early treated adults with phenylketonuria. Orphanet J. Rare Dis. 2018, 13, 150. [Google Scholar] [CrossRef]
- Owada, M.; Aoki, K.; Kitagawa, T. Taste preferences and feeding behaviour in children with phenylketonuria on a semisynthetic diet. Eur. J. Pediatr. 2000, 159, 846–850. [Google Scholar] [CrossRef]
- Bilder, D.A.; Kobori, J.A.; Cohen-Pfeffer, J.L.; Johnson, E.M.; Jurecki, E.R.; Grant, M.L. Neuropsychiatric comorbidities in adults with phenylketonuria: A retrospective cohort study. Mol. Genet. Metab. 2017, 121, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.J.; Leuzzi, V. White matter pathology in phenylketonuria. Mol. Genet. Metab. 2010, 99 (Suppl. S1), S3–S9. [Google Scholar] [CrossRef] [PubMed]
- Ilgaz, F.; Pinto, A.; Gökmen-Özel, H.; Rocha, J.C.; van Dam, E.; Ahring, K.; Bélanger-Quintana, A.; Dokoupil, K.; Karabulut, E.; MacDonald, A. Long-Term Growth in Phenylketonuria: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2070. [Google Scholar] [CrossRef]
- Demirkol, M.; Giżewska, M.; Giovannini, M.; Walter, J. Follow up of phenylketonuria patients. Mol. Genet. Metab. 2011, 104, S31–S39. [Google Scholar] [CrossRef] [PubMed]
- Mazzucato, M.; Visonà Dalla Pozza, L.; Minichiello, C.; Manea, S.; Barbieri, S.; Toto, E.; Vianello, A.; Facchin, P. The Epidemiology of Transition into Adulthood of Rare Diseases Patients: Results from a Population-Based Registry. Int. J. Environ. Res. Public Health 2018, 15, 2212. [Google Scholar] [CrossRef] [PubMed]
- Mütze, U.; Roth, A.; Weigel, J.F.; Beblo, S.; Baerwald, C.G.; Bührdel, P.; Kiess, W. Transition of young adults with phenylketonuria from pediatric to adult care. J. Inherit. Metab. Dis. 2011, 34, 701–709. [Google Scholar] [CrossRef]
| NBS Group (n = 68) | Pre-NBS Group (n = 17) | ||
|---|---|---|---|
| Sex | |||
| male | 34 | 7 | |
| female | 33 | 10 | |
| unknown | 1 | 0 | |
| Median age (range) [years] | 28.5 (20.5–38.2) | 43.9 (37.7–50.8) | |
| 20–24 | 22 | 0 | |
| 25–29 | 19 | 0 | |
| 30–34 | 14 | 0 | |
| 35–39 | 13 | 3 | |
| 40–44 | 0 | 7 | |
| 45–49 | 0 | 6 | |
| 50- | 0 | 1 | |
| Clinical form | |||
| classic | 54 | 16 | |
| mild HPA | 6 | 0 | |
| BH4-responsive | 2 | 0 | |
| BH4 defect | 0 | 0 | |
| unknown | 6 | 1 | |
| Follow-up department | |||
| pediatrics | 66 | 16 | |
| internal medicine | 1 | 1 | |
| gynecology | 1 | 0 | |
| treatment interruption | 21 | 5 | |
| Reasons for Discontinuation (Number of Patients with the Same Comment) | Reasons for Restarting (Number of Patients with the Same Comment) |
|---|---|
| Economic problems (7) Self-judgment/personal circumstances (7) Unpleasant taste of the special formula (6) Recommendation of the attending physicians (5) Changes in one’s environment (3) | Pregnancy (8) Improvement of the medical subsidy system (4) Appearance of psychiatric abnormalities (3) Spontaneously restarted (2) |
| NBS Group (n = 68) | Pre-NBS Group (n = 17) | |||||||
|---|---|---|---|---|---|---|---|---|
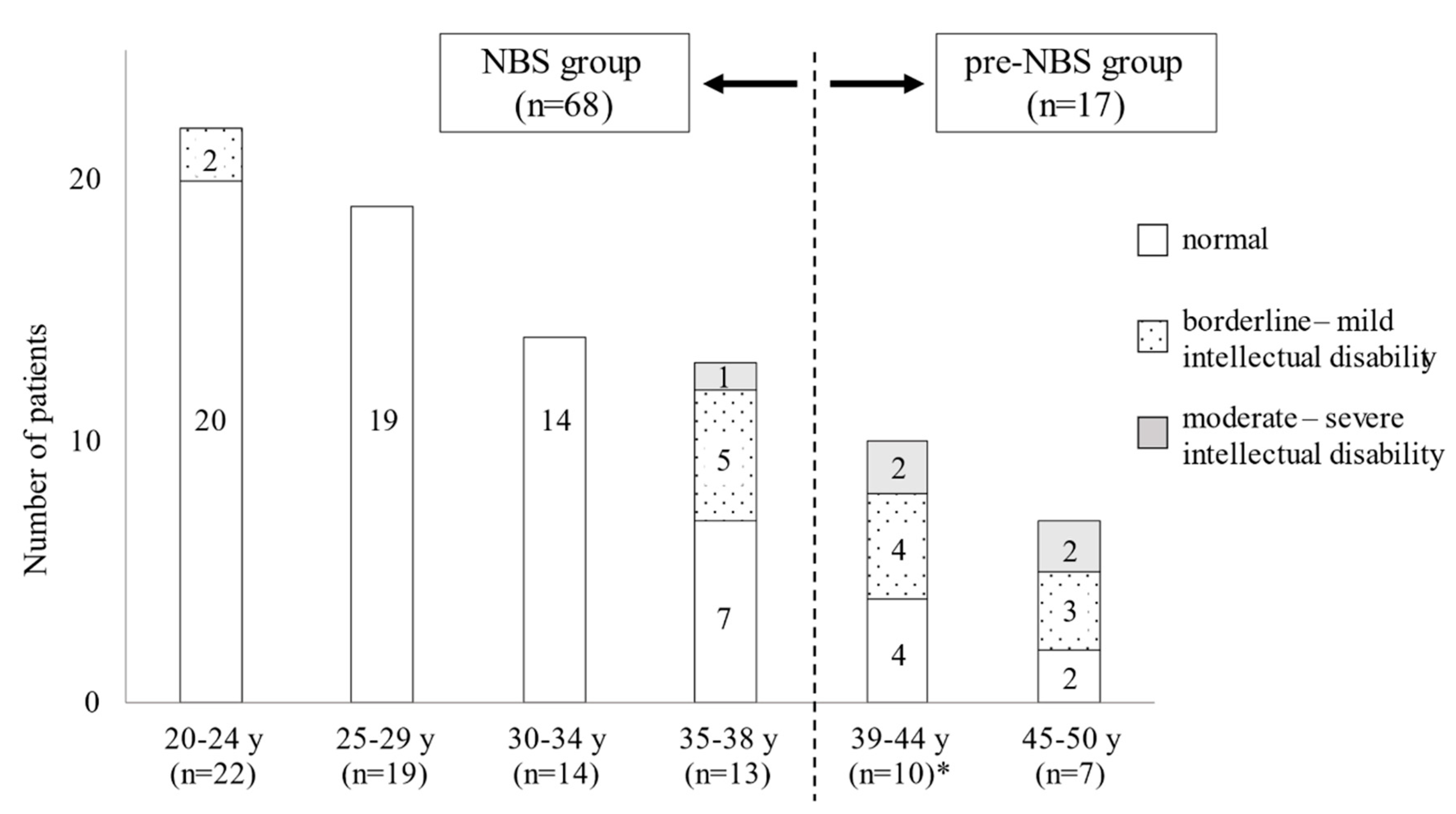
| 20–24 y (n = 22) | 25–29 y (n = 19) | 30–34 y (n = 14) | 35–38 y (n = 13) | Total (%) | 39–44 (n = 10) * | 45–50 y (n = 7) | Total (%) | |
| Psychiatric status | ||||||||
| normal | 20 | 19 | 13 | 12 | 64 (94%) | 7 | 4 | 11 (65%) |
| transient impairment during treatment interruption | 2 | 0 | 1 | 0 | 3 (4%) | 0 | 0 | 0 (0%) |
| psychiatric disability | 0 | 0 | 0 | 1 | 1 (1%) | 3 | 3 | 6 (35%) |
| Physical characteristics | ||||||||
| normal | 19 | 13 | 14 | 11 | 57 (84%) | 5 | 7 | 12 (71%) |
| short stature | 1 | 0 | 0 | 0 | 1 (1%) | 1 | 0 | 1 (6%) |
| obesity | 2 | 3 | 0 | 1 | 6 (9%) | 2 | 0 | 2 (12%) |
| obesity and short stature | 0 | 2 | 0 | 0 | 2 (3%) | 0 | 0 | 0 (0%) |
| leanness | 0 | 1 | 0 | 1 | 2 (3%) | 1 | 0 | 1 (6%) |
| unknown | 0 | 0 | 0 | 0 | 0 (0%) | 1 | 0 | 1 (6%) |
| Education status | ||||||||
| university | 9 | 10 | 3 | 4 | 26 (38%) | 1 | 1 | 2 (12%) |
| technical school | 3 | 5 | 3 | 0 | 11 (16%) | 1 | 0 | 1 (6%) |
| high school # | 10 | 2 | 4 | 2 | 18 (26%) | 2 | 2 | 4 (24%) |
| junior high school | 0 | 0 | 0 | 1 | 1 (1%) | 0 | 0 | 0 (0%) |
| school for individuals with a disability | 0 | 0 | 0 | 1 | 1 (1%) | 3 | 2 | 5 (30%) |
| unknown | 0 | 2 | 4 | 5 | 11 (16%) | 3 | 2 | 5 (30%) |
| Employment status | ||||||||
| attending school | 4 | 1 | 0 | 0 | 5 (7%) | 0 | 0 | 0 (0%) |
| employed | 18 | 17 | 14 | 12 | 61 (90%) | 3 | 4 | 7 (41%) |
| unemployed | 0 | 1 | 0 | 1 | 2 (3%) | 4 | 1 | 5 (30%) |
| living in a house for individuals with a disability | 0 | 0 | 0 | 0 | 0 (0%) | 3 | 2 | 5 (30%) |
| unknown | 0 | 0 | 0 | 0 | 0 (0%) | 0 | 0 | 0 (0%) |
| Marital status | ||||||||
| married | 0 | 4 | 9 | 6 | 19 (28%) | 2 | 0 | 2 (12%) |
| unmarried or divorce | 14 | 8 | 4 | 5 | 31 (46%) | 8 | 5 | 13 (76%) |
| unknown | 8 | 7 | 1 | 2 | 18 (26%) | 0 | 2 | 2 (12%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, K.; Yamaguchi, S.; Yokoyama, K.; Aoki, K.; Taketani, T. Long-Term Neurological Outcomes of Adult Patients with Phenylketonuria before and after Newborn Screening in Japan. Int. J. Neonatal Screen. 2021, 7, 21. https://doi.org/10.3390/ijns7020021
Yamada K, Yamaguchi S, Yokoyama K, Aoki K, Taketani T. Long-Term Neurological Outcomes of Adult Patients with Phenylketonuria before and after Newborn Screening in Japan. International Journal of Neonatal Screening. 2021; 7(2):21. https://doi.org/10.3390/ijns7020021
Chicago/Turabian StyleYamada, Kenji, Seiji Yamaguchi, Kazunori Yokoyama, Kikumaro Aoki, and Takeshi Taketani. 2021. "Long-Term Neurological Outcomes of Adult Patients with Phenylketonuria before and after Newborn Screening in Japan" International Journal of Neonatal Screening 7, no. 2: 21. https://doi.org/10.3390/ijns7020021
APA StyleYamada, K., Yamaguchi, S., Yokoyama, K., Aoki, K., & Taketani, T. (2021). Long-Term Neurological Outcomes of Adult Patients with Phenylketonuria before and after Newborn Screening in Japan. International Journal of Neonatal Screening, 7(2), 21. https://doi.org/10.3390/ijns7020021






