Non-Uptake of Newborn Screening in Planned Homebirth Is Associated with Preventive Health Practices for Infants: A Retrospective Case-Control Study
Abstract
1. Introduction
2. Methods
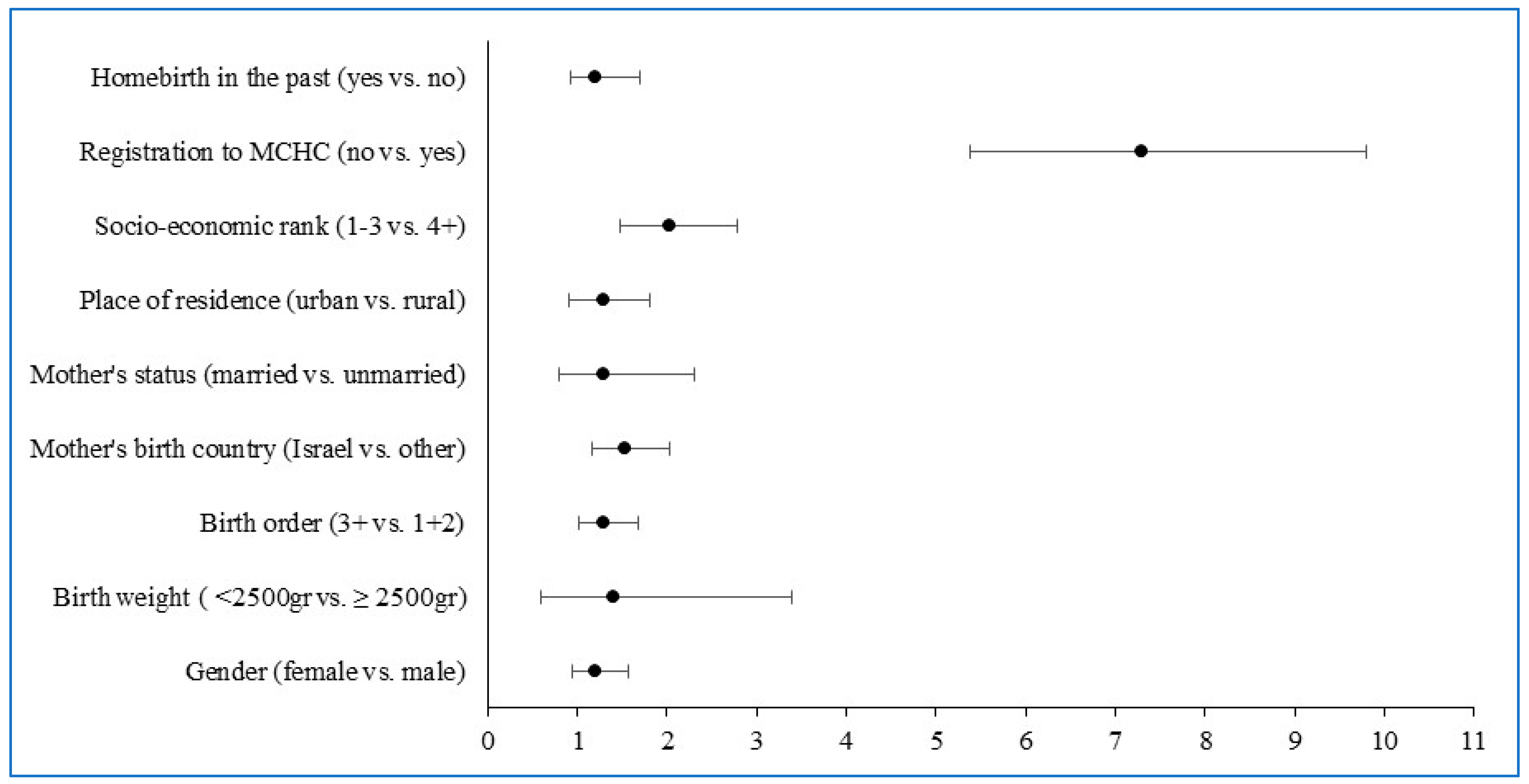
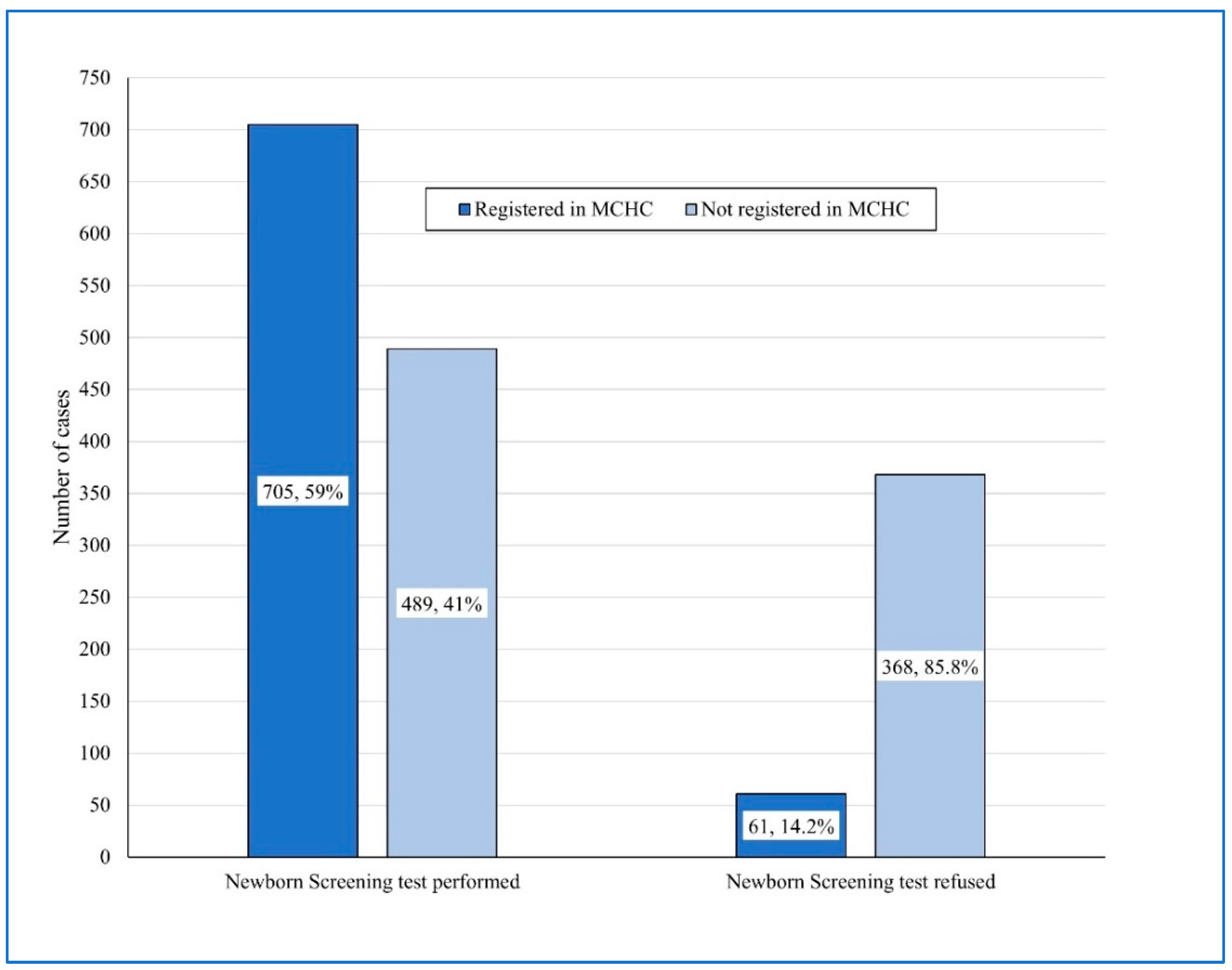
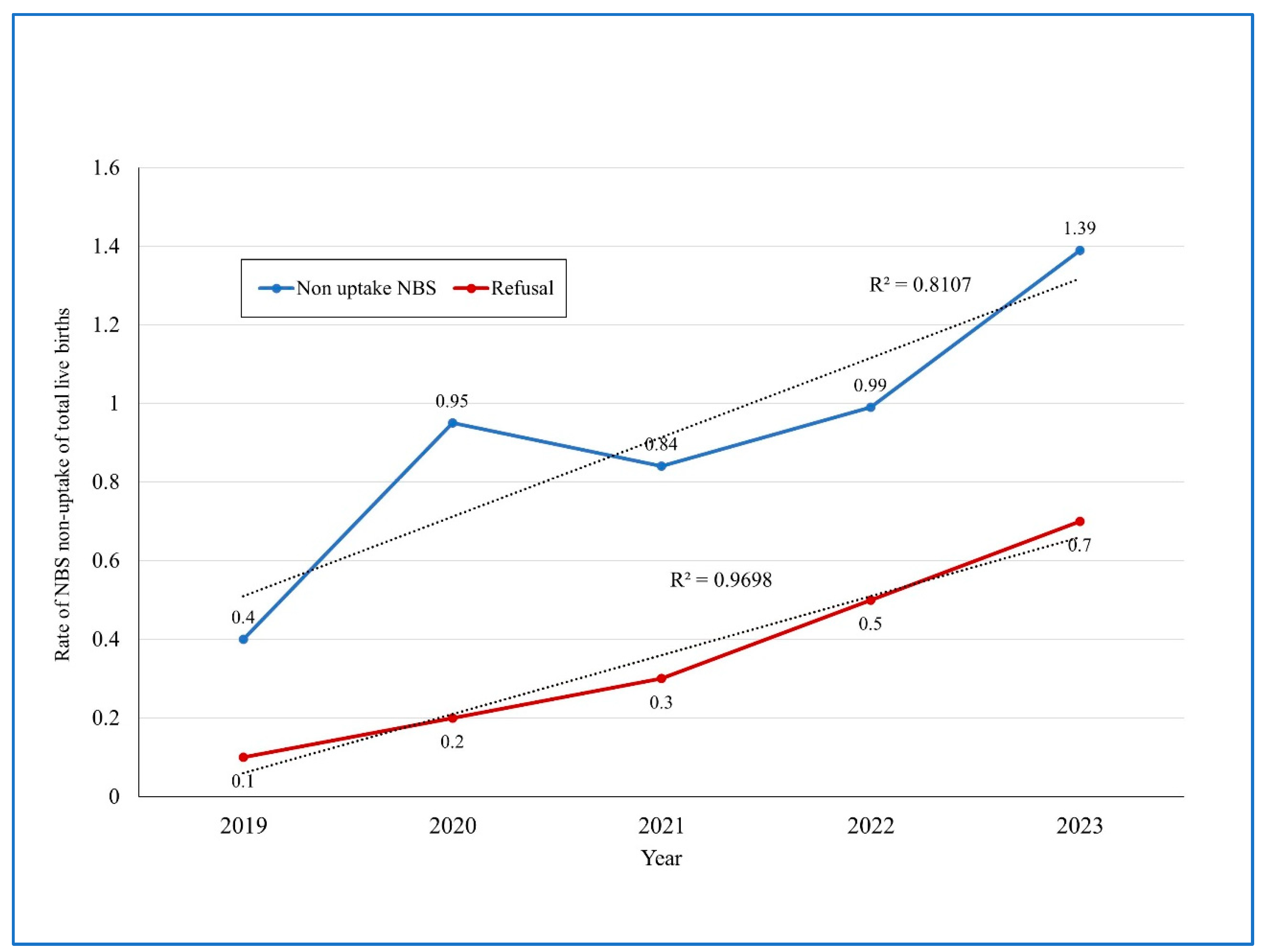
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NBS | Newborn Screening |
| MCHC | Mother and Child Health Clinics |
| JD | Jerusalem District |
| MoH | Ministry of Health |
| ID | Identification Number |
| WHO | World Health Organization |
| STROBE | Strengthening Reporting of Observational Studies in Epidemiology |
| NIHP | Israel National Institute for Health Policy and Health Services Research |
References
- Therrell, B.L.; Padilla, C.D.; Borrajo, G.J.C.; Khneisser, I.; Schielen, P.C.J.I.; Knight-Madden, J.; Malherbe, H.L.; Kase, M. Current Status of Newborn Bloodspot Screening Worldwide 2024: A Comprehensive Review of Recent Activities (2020–2023). Int. J. Neonatal Screen. 2024, 10, 38. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.S.; Lloyd-Puryear, M.A.; Howell, R.R. The Progress and Future of US Newborn Screening. Int. J. Neonatal Screen. 2022, 8, 41. [Google Scholar] [CrossRef]
- Sikonja, J.; Groselj, U.; Scarpa, M.; la Marca, G.; Cheillan, D.; Kölker, S.; Zetterström, R.H.; Kožich, V.; Le Cam, Y.; Gumus, G.; et al. Towards Achieving Equity and Innovation in Newborn Screening across Europe. Int. J. Neonatal Screen. 2022, 8, 31. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). CDC Grand Rounds: Newborn screening and improved outcomes. MMWR Morb. Mortal. Wkly. Rep. 2012, 61, 390–393. [Google Scholar]
- Loeber, J.G.; Platis, D.; Zetterström, R.H.; Almashanu, S.; Boemer, F.; Bonham, J.R.; Borde, P.; Brincat, I.; Cheillan, D.; Dekkers, E.; et al. Neonatal Screening in Europe Revisited an ISNS Perspective on the Current State and Developments Since 2010. Int. J. Neonatal Screen. 2021, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- Pollitt, R.J. Different Viewpoints: International Perspectives on Newborn Screening. J. Med. Biochem. 2015, 34, 18–22. [Google Scholar] [CrossRef][Green Version]
- Njau, G.; Odoi, A. Investigation of Predictors of Newborn Screening Refusal in a Large Birth Cohort in North Dakota, USA. Matern. Child Health J. 2019, 23, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Sahni, V.; Lai, F.Y.; MacDonald, S.E. Neonatal vitamin K refusal and nonimmunization. Pediatrics 2014, 134, 497–503. [Google Scholar] [CrossRef]
- GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1160–1203. [Google Scholar] [CrossRef] [PubMed]
- United Nations, Department of Economic and Social Affairs, Population Division (2022). World Population Prospects 2022. Available online: https://population.un.org/wpp/ (accessed on 15 October 2024).
- Thomasson, M.A.; Treber, J. From home to hospital: The evolution of childbirth in the United States, 1928–1940. Explor. Econ. Hist. 2008, 45, 76–99. [Google Scholar] [CrossRef]
- McCool, W.F.; Simeone, S.A. Birth in the United States: An overview of trends past and present. Nurs. Clin. N. Am. 2002, 37, 735–746. [Google Scholar] [CrossRef]
- Walker, J.J. Planned home birth. Best. Pract. Res. Clin. Obstet. Gynaecol. 2017, 43, 76–86. [Google Scholar] [CrossRef]
- Montagu, D.; Sudhinaraset, M.; Diamond-Smith, N.; Campbell, O.; Gabrysch, S.; Freedman, L.; Kruk, M.E.; Donnay, F. Where women go to deliver: Understanding the changing landscape of childbirth in Africa and Asia. Health Policy Plan. 2017, 32, 1146–1152. [Google Scholar] [CrossRef] [PubMed]
- Campbell, O.M.; Calvert, C.; Testa, A.; Strehlow, M.; Benova, L.; Keyes, E.; Donnay, F.; Macleod, D.; Gabrysch, S.; Rong, L.; et al. The scale, scope, coverage, and capability of childbirth care. Lancet 2016, 388, 2193–2208. [Google Scholar] [CrossRef]
- Hernández-Vásquez, A.; Chacón-Torrico, H.; Bendezu-Quispe, G. Prevalence of home birth among 880,345 women in 67 low- and middle-income countries: A meta-analysis of Demographic and Health Surveys. SSM Popul. Health 2021, 16, 100955. [Google Scholar] [CrossRef] [PubMed]
- Galková, G.; Böhm, P.; Hon, Z.; Heřman, T.; Doubrava, R.; Navrátil, L. Comparison of Frequency of Home Births in the Member States of the EU Between 2015 and 2019. Glob. Pediatr. Health 2022, 9, 2333794X211070916. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.; Romanis, E.C. The Medicalisation of Childbirth and Access to homebirth in the UK: COVID-19 and Beyond. Med. Law. Rev. 2021, 29, 661–687. [Google Scholar] [CrossRef]
- MacDorman, M.F.; Barnard-Mayers, R.; Declercq, E. United States community births increased by 20% from 2019 to 2020. Birth 2022, 49, 559–568. [Google Scholar] [CrossRef]
- Gregory, E.C.; Osterman, M.J.; Valenzuela, C.P. Changes in Home Births by Race and Hispanic Origin and State of Residence of Mother: United States, 2019–2020 and 2020–2021. Natl. Vital Stat. Rep. 2022, 71, 1–10. [Google Scholar] [PubMed]
- Kuehn, B.M. Highest Rate of US Home Births in 3 Decades. JAMA 2022, 328, 2389. [Google Scholar] [CrossRef]
- The Central Bureau of Statistics (CBS), Israel. Live Births—Main Indicators. 2002. Available online: https://www.cbs.gov.il/en/subjects/Pages/Live-Births.aspx (accessed on 15 October 2024).
- Meroz, M.R.; Gesser-Edelsburg, A. Institutional and Cultural Perspectives on Home Birth in Israel. J. Perinat. Educ. 2015, 24, 25–36. [Google Scholar] [CrossRef] [PubMed][Green Version]
- The Knesset (Israel Parliament) Research and Information Center (RIC). Homebirths in Israel and in Other Countries (in Hebrew). July Jerusalem, Israel. Available online: https://fs.knesset.gov.il/globaldocs/MMM/854d6b58-e9f7-e411-80c8-00155d010977/2_854d6b58-e9f7-e411-80c8-00155d010977_11_8555.pdf (accessed on 15 October 2024).
- Brusa, M.; Barilan, Y.M.; Gobber, D. Childbirth in Israel: Home Birth and Newborn Screening. In Bioethics and Biopolitics in Israel: Socio-Legal, Political and Empirical Analysis; Boas, H., Hashiloni-Dolev, Y., Davidovitch, N., Filc, D., Lavi, S.J., Eds.; Cambridge University Press: Cambridge, UK, 2018; p. 180-2-1. [Google Scholar]
- Handelzalts, J.E.; Zacks, A.; Levy, S. The association of birth model with resilience variables and birth experience: Home versus hospital birth. Midwifery 2016, 36, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Israel. Postnatal Initial Care of the Newborn at the Hospital (8/2024). Jerusalem, Israel. Available online: https://me.health.gov.il/en/parenting/raising-children/after-childbirth/at-the-hospital/initial-care-for-newborn/?source=6839 (accessed on 15 October 2024).
- Ministry of Health, Israel. Home Births Guidelines (17/2012). May Jerusalem, Israel. Available online: https://www.gov.il/he/departments/policies/mr17-2012 (accessed on 15 October 2024).
- Almashanu, S.; Sela, B.A.; Zlotogora, J. The national program for neonatal screening. Isr. J. Pediatr. 2008, 65, 6–9. [Google Scholar]
- Zlotogora, J. Genetics and genomic medicine in Israel. Mol. Genet. Genomic Med. 2014, 2, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, D.R.; Verbov, G.; Edelstein, N.; Stein-Zamir, C. Preventive health services for young children in Israel: Historical development and current challenges. Isr. J. Health Policy Res. 2019, 8, 23. [Google Scholar] [CrossRef] [PubMed]
- The National Insurance, Israel. Birth Grants. Conditions of Entitlement. Jerusalem, Israel. Available online: https://www.btl.gov.il/English%20Homepage/Benefits/Pages/BirthGrant.aspx (accessed on 15 October 2024).
- Stein-Zamir, C.; Israeli, A.; Grotto, I. Immunization registry as a digital assessment tool during outbreaks. Clin. Microbiol. Infect. 2021, 27, 166–168. [Google Scholar] [CrossRef]
- Stein-Zamir, C.; Israeli, A. Timeliness and completeness of routine childhood vaccinations in young children residing in a district with recurrent vaccine-preventable disease outbreaks, Jerusalem, Israel. Euro Surveill. 2019, 24, 1800004. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Israel. Newborn Screening Tests. October Jerusalem, Israel. Available online: https://me.health.gov.il/en/parenting/raising-children/after-childbirth/at-the-hospital/genetic-tests/?source=7279 (accessed on 15 October 2024).
- Ministry of Health, Israel. Routine Vaccines for Babies and Children. October 2024. Jerusalem, Israel. Available online: https://me.health.gov.il/en/parenting/raising-children/immunization-schedule/immunization-schedule/ (accessed on 15 October 2024).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Nygaard, S.S.; Kesmodel, U.S. Home births—Where are we heading? Acta Obstet. Gynecol. Scand. 2018, 97, 1155–1156. [Google Scholar] [CrossRef] [PubMed]
- Verhoeven, C.J.M.; Boer, J.; Kok, M.; Nieuwenhuijze, M.; de Jonge, A.; Peters, L.L. More home births during the COVID-19 pandemic in the Netherlands. Birth 2022, 49, 792–804. [Google Scholar] [CrossRef]
- Marcewicz, L.H.; Clayton, J.; Maenner, M.; Odom, E.; Okoroh, E.; Christensen, D.; Goodman, A.; Warren, M.D.; Traylor, J.; Miller, A.; et al. Parental Refusal of Vitamin K and Neonatal Preventive Services: A Need for Surveillance. Matern. Child Health J. 2017, 21, 1079–1084. [Google Scholar] [CrossRef] [PubMed]
- Loyal, J.; Shapiro, E.D. Refusal of intramuscular vitamin K by parents of newborns: A review. Hosp. Pediatr. 2020, 10, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Rogers, T.P.; Fathi, O.; Sánchez, P.J. Neonatologists and vitamin K hesitancy. J. Perinatol. 2023, 43, 1067–1071. [Google Scholar] [CrossRef] [PubMed]
- Higgins, D.M.; Haynes, A.L.; Jensen, J.C.; O’Leary, S.T.; Moss, A.; Calonge, N. Planned Out-of-Hospital Birth as a Risk Factor for Nonreceipt of Hepatitis B Immunization. Pediatr. Infect. Dis. J. 2023, 42, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Kabra, S.K.; Sachdev, H.P.; Lodha, R. Home visits by community health workers to improve identification of serious illness and care seeking in newborns and young infants from low- and middle-income countries. J. Perinatol. 2016, 36 (Suppl. S1), S74–S82. [Google Scholar] [CrossRef] [PubMed]
- Watterberg, K.; AAP Committee on Fetus and Newborn. Providing Care for Infants Born at Home. Pediatrics 2020, 145, e20200626. [Google Scholar] [CrossRef] [PubMed]
- Olsen, O.; Clausen, J.A. Planned hospital birth compared with planned home birth for pregnant women at low risk of complications. Cochrane Database Syst. Rev. 2023, 3, CD000352. [Google Scholar] [PubMed]
- Grünebaum, A.; Chervenak, F.A. Why do women choose home births. J. Perinat. Med. 2024, 52, 575–585. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Israel. Director General’s Directive: Criteria for Operating Birth Centers in the Community. (5/2024). Jerusalem, Israel. Available online: https://www.gov.il/he/pages/mk03-2024 (accessed on 15 October 2024).
- Kemper, A.R.; Fant, K.E.; Clark, S.J. Informing parents about newborn screening. Public Health Nurs. 2005, 22, 332–338. [Google Scholar] [CrossRef]
- Odenwald, B.; Brockow, I.; Hanauer, M.; Lüders, A.; Nennstiel, U. Is Our Newborn Screening Working Well? A Literature Review of Quality Requirements for Newborn Blood Spot Screening (NBS) Infrastructure and Procedures. Int. J. Neonatal Screen. 2023, 9, 35. [Google Scholar] [CrossRef] [PubMed]
- Wilaiwongsathien, K.; Wattanasirichaigoon, D.; Rattanasiri, S.; Aonnuam, C.; Tangshewinsirikul, C.; Tim-Aroon, T. Parental Awareness, Knowledge, and Attitudes Regarding Current and Future Newborn Bloodspot Screening: The First Report from Thailand. Int. J. Neonatal Screen. 2023, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- Speechley, M.; Kunnilathu, A.; Aluckal, E.; Balakrishna, M.S.; Mathew, B.; George, E.K. Screening in Public Health and Clinical Care: Similarities and Differences in Definitions, Types, and Aims—A Systematic Review. J. Clin. Diagn. Res. 2017, 11, LE01–LE04. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman, S. Indifferent or Uninformed? Reflections of Health Professionals on Parental Education and Consent for Expanded Newborn Screening in Israel, 2008–2016. Int. J. Neonatal Screen. 2017, 3, 12. [Google Scholar] [CrossRef]


| Variable | Study Group n = 1623 | Control Group n = 1623 | OR (95%CI) | p-Value |
|---|---|---|---|---|
| Gender | ||||
| Male | 806 (49.7%) | 826 (50.9%) | 0.95 (0.83–1.09) | NS |
| Female | 817 (50.3%) | 797 (49.1%) | ||
| Birth Weight | ||||
| <2500 gr | 28 (1.8%) | 86 (5.3%) | 0.31 (0.2–0.49) | 0.001 |
| Birth weight (gr) mean ± SD | 3335 ± 444 | 3288 ± 499 | 0.006 | |
| Birth weight median (gr) | 3330 | 3300 | NS | |
| Birth order | ||||
| 1 and 2 | 872 (53.7%) | 965 (59.5%) | ||
| 3+ | 751 (46.3%) | 658 (40.5%) | 1.26 (1.1–1.46) | 0.001 |
| Mother’s age (years) | ||||
| Mean ± SD | 31.6 ± 5.6 | 29.5 ± 5.9 | 0.001 | |
| Median | 32 | 29 | 0.001 | |
| Mother’s birth country | ||||
| Israel | 1087 (67%) | 1401 (86.3%) | 0.3 (0.26–0.38) | 0.0001 |
| Other | 536 (33%) | 222 (13.7%) | ||
| Mother’s status | ||||
| Unmarried | 153 (9.4%) | 28 (1.7%) | 5.93 (3.9–9.3) | 0.0001 |
| Married | 1470 (90.6%) | 1595 (98.3%) | ||
| Place of residence | ||||
| Rural | 544 (33.5%) | 155 (9.6%) | 4.77 (3.9–5.84) | 0.0001 |
| Urban | 1079 (66.5%) | 1468 (90.4%) | ||
| Maternal education (years) | ||||
| Mean ± SD | 14.7 ± 2.4 | 13.6 ± 2.1 | 0.001 | |
| Median | 15 | 12 | 0.001 | |
| Ethnicity | ||||
| Jewish | 1623 (100%) | 1332 (82.1%) | 0.0001 | |
| Arab | 0 (0%) | 291 (17.9%) | ||
| Socio-economic rank of place of residence | ||||
| 1–3 | 704 (43.4%) | 1169 (72%) | ||
| 4+ | 919 (56.6%) | 454 (28%) | 3.36 (2.89–3.9) | 0.0001 |
| Mean ± SD | 4.3 ± 2.5 | 2.8 ± 2.1 | 0.001 | |
| Median | 5 | 2 | 0.001 | |
| Homebirth in the past | ||||
| Yes | 772 (47.6%) | ------- | 0.0001 | |
| No | 851 (52.4%) | 1623 (100%) |
| Performed Newborn Screening Test | |||||
|---|---|---|---|---|---|
| Variable | Total | No | Yes | OR (95%CI) | p-Value |
| n = 429 (26.4%) | n = 1194 (73.6%) | ||||
| Gender | |||||
| Male | 806 | 193 (45%) | 613 (51.3%) | 0.78 (0.62–0.97) | 0.014 |
| Female | 817 | 236 (55%) | 581 (48.7%) | ||
| Birth weight | |||||
| <2500 gr | 28 | 12 (2.8%) | 16 (1.4%) | 2.08 (0.89–4.73) | 0.047 |
| Birth weight (gr) mean ± SD | 3335 ± 444 | 3284 ± 443 | 3353 ± 444 | 0.006 | |
| Birth weight median (gr) | 3330 | 3300 | 3350 | NS | |
| Birth order | |||||
| 1 and 2 | 872 | 205 (47.8%) | 667 (55.9%) | 0.72 (0.58–0.91) | 0.002 |
| 3+ | 751 | 224 (52.2%) | 527 (44.1%) | ||
| Mother’s age (years) | |||||
| Mean ± SD | 31.6 ± 5.6 | 31.2 ± 6 | 31.7 ± 5.5 | NS | |
| Median | 32 | 32 | 32 | NS | |
| Mother’s birth country | |||||
| Israel | 1087 | 316 (73.7%) | 771 (64.6%) | 1.5 (1.19–1.98) | 0.0001 |
| other | 536 | 113 (26.3%) | 423 (35.4%) | ||
| Mother’s status | |||||
| Unmarried | 153 | 21 (4.9%) | 132 (11.1%) | 0.41 (0.24–0.67) | 0.0001 |
| Married | 1470 | 408 (95.1%) | 1062 (88.9%) | ||
| Homebirth in the past | |||||
| Yes | 772 | 231 (53.8%) | 541 (45.3%) | 1.4 (1.12–177) | 0.001 |
| No | 851 | 198 (46.2%) | 653 (54.7%) | ||
| Place of residence | |||||
| Rural | 544 | 90 (21%) | 454 (38%) | 0.43 (0.33–0.56) | 0.0001 |
| Urban | 1079 | 339 (79%) | 740 (62%) | ||
| Maternal education (years) | |||||
| Mean ± SD | 14.6 ± 2.4 | 13.6 ± 1.9 | 15.04 ± 2.4 | <0.001 | |
| Median | 15 | 12 | 15 | <0.001 | |
| Socio-economic rank of place of residence | |||||
| 1–3 | 704 | 271 (63.2%) | 433 (36.3%) | 3.01 (2.38–3.82) | 0.0001 |
| 4+ | 919 | 158 (36.8%) | 761 (63.7%) | ||
| Mean ± SD | 4.3 ± 2.5 | 3.2 ± 2.4 | 4.7 ± 2.4 | <0.001 | |
| Median | 5 | 2 | 6 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Society for Neonatal Screening. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stein-Zamir, C.; Shoob, H.; Katan, S.; Verbov, G.; Almashanu, S. Non-Uptake of Newborn Screening in Planned Homebirth Is Associated with Preventive Health Practices for Infants: A Retrospective Case-Control Study. Int. J. Neonatal Screen. 2025, 11, 15. https://doi.org/10.3390/ijns11010015
Stein-Zamir C, Shoob H, Katan S, Verbov G, Almashanu S. Non-Uptake of Newborn Screening in Planned Homebirth Is Associated with Preventive Health Practices for Infants: A Retrospective Case-Control Study. International Journal of Neonatal Screening. 2025; 11(1):15. https://doi.org/10.3390/ijns11010015
Chicago/Turabian StyleStein-Zamir, Chen, Hanna Shoob, Sandra Katan, Gina Verbov, and Shlomo Almashanu. 2025. "Non-Uptake of Newborn Screening in Planned Homebirth Is Associated with Preventive Health Practices for Infants: A Retrospective Case-Control Study" International Journal of Neonatal Screening 11, no. 1: 15. https://doi.org/10.3390/ijns11010015
APA StyleStein-Zamir, C., Shoob, H., Katan, S., Verbov, G., & Almashanu, S. (2025). Non-Uptake of Newborn Screening in Planned Homebirth Is Associated with Preventive Health Practices for Infants: A Retrospective Case-Control Study. International Journal of Neonatal Screening, 11(1), 15. https://doi.org/10.3390/ijns11010015





