Abstract
Umbilical hernia is one of the types of ventral hernias of the abdominal wall and it represents the externalization of a part of the abdominal contents through a defect of the anterior abdominal wall located in the umbilical region. It is estimated that more than 20 million abdominal wall hernia surgeries are performed worldwide each year. The paper presents a retrospective study on the patients diagnosed with umbilical hernia and admitted to the First and Second Surgery Departments of the Sibiu County Emergency Clinical Hospital. The study includes 82 cases diagnosed with umbilical hernias over a period of 4 years, between 1 January 2017 and 31 December 2020. Open and laparoscopic surgical techniques are compared in terms of outcomes and postoperative complications. Most cases of umbilical hernia were within the age group 51–70 years, with a slightly higher incidence in males. Arterial hypertension and obesity were the most frequent comorbidities. The alloplastic, classic or laparoscopic procedure became the most widely used due to benefits such as: rapid socio-professional reintegration, short-term hospitalization and low incidence of relapses and postoperative complications. The current trend is for the IPOM laparoscopic procedure to become the gold standard in the treatment of umbilical hernias.
Introduction
Umbilical hernias are the second most common forms of hernia in adults, after inguinal hernias, and they represent 6% -14% of all hernias of the abdominal wall [1,2,3]. Approximately 10% of all primary hernias include umbilical and epigastric hernias [4]. Although it is a very common condition among children, about 90% of the umbilical hernias in adults are acquired, without a history of umbilical hernia in childhood. The incidence of umbilical hernia in the general adult population is 2%, being much more common in obese women, multiparous or in patients with cirrhosis. The risk factors are the same as in the case of other hernias of the abdominal wall, causing an increase in the intra-abdominal pressure and/ or a decrease in parietal resistance. The repetitive action on the abdominal wall due to the increased intra-abdominal pressure favors the stretching of the abdominal muscles and the presence of adipose tissue acts by separating the fascicles and muscle layers, weakening the aponeurosis and favoring the appearance of umbilical hernias [5,6].
Generally, umbilical hernias in men are most often incarcerated, while women are more likely to have an asymptomatic reducible hernia. However, 70% of the hernia defects are performed on men [6]. The evolution of ventral hernia repairs has a long history, starting from ancient Egypt from the recognition of ventral hernias to their current management, with significant contributions from various authors [7]. In 1899, Mayo described his famous transverse overlap technique for umbilical hernia, which was adopted by many surgeons for hernia repair. Others, such as Witzel, Goepel, and Bartlett, have described the repair of the hernia by continuous sutures of the fascia of the external oblique. This encouraged surgeons to explore alternative techniques for strengthening the abdominal wall. Advances in surgery have led to more cases of ventral hernia formation, and this has required the development of new techniques and new materials for the management of ventral hernias [8]. In 1890, T. Billroth suggested that the ideal way to repair hernias was to use a prosthetic material to close the hernia defect. Many materials were used, but all failed due to infections, rejection by the body and recurrences [9]. Marlex was one of the first synthetic meshes made of polypropylene that revolutionized hernia repairs and contributed substantially to the introduction of the “tension-free” concept [10].
The surgical treatment of ventral hernias has changed dramatically in recent decades with the introduction of laparoscopy and prosthetic biomaterials to strengthen the abdominal wall [11]. Laparoscopic ventral hernia repair was first described in 1992 by Karl Leblanc. By performing the IPOM procedure, he reported a shorter hospitalization period, a lower recurrence rate and fewer complications compared to classical techniques. The laparoscopic repair of ventral hernia is based on the principles of the technique described by Rives and Stoppa, which states the importance of placing preperitoneal or intraperitoneal prostheses to ensure a uniform distribution of force, which can lead to higher resistance and lower recurrence rates [12,13].
If the s-IPOM procedure is performed, the parietal defect is left open, and if the IPOM-plus procedure is used, the parietal defect will be closed with a continuous intraperitoneal thread or with separate threads passed transparietally, a procedure which, if so, decreases recurrence.
This paper aims at presenting the outcomes of the 2 alloplastic procedures (classic alloplastic and laparoscopic procedure) compared to the classic anatomical one, in the treatment of umbilical hernias in terms of efficacy, applicability and performance. Also, the study aims at following the aspects and the results obtained in laparoscopic procedures (IPOM and IPOM-plus) depending on the particularities of the patients.
Materials and Methods
This is a retrospective study on the patients diagnosed with umbilical hernia and admitted to the 1st and 2nd Departments of Surgery in Sibiu County Emergency Clinical Hospital. The study includes 82 cases operated on for umbilical hernias over a period of 4 years, between 01.01.2017 and 31.12.2020. All the patients over 14 years of age who underwent surgery in a chronic and acute regimen, for primary or recurrent umbilical hernias, were included. Young patients under the age of 14 and those who were not operated on were excluded. The statistical data processing was performed using Microsoft Office Excel 2016.
The data collection and integration were performed from sources that were extracted from the database of Sibiu County Emergency Clinical Hospital. These results were correlated with the current data from the international literature on umbilical hernias.
The parameters followed in the evaluation of the patients included in the study group are: the age, the sex of the patients, the environment, the distribution by year of cases diagnosed with umbilical hernia, the associated comorbidities, the type of umbilical hernia (primary or recurrent), the type of surgical procedure performed (classic or laparoscopic), the type of anesthesia performed, the period of hospitalization depending on the type of the surgical procedure performed and the postoperative complications.
The description of the surgical techniques used
During the anatomical procedure, an elliptical incision is made, which circumscribes the umbilical scar, involving the skin, the subcutaneous cellular tissue, up to the level of the anterior aponeurosis, completely isolating the hernia sac circumferentially. Subsequently, the hernia sac is isolated by viscerolysis from the adjacent tissues, a stage followed by its opening, after making sure that we removed the saccular contents in the peritoneum.
The next operative time consists in closing the sac, with the resection of the saccular surplus up to the level of the aponeurotic edges. To close the wall, the Mayo technique was used in a single plane or in a double layer, on the lapel, with wires placed transversely, at a distance of 1 cm. As technical variants, in terms of incisions, there can be: smaller or larger, in relation to the parietal dehiscence; longitudinal or bypassing the umbilical scar [14].
In the cases in which we used the classic alloplastic procedure, we made the incision at the level of the skin, supra- and sub-umbilical, with the sectioning of the subcutaneous tissue and the circular isolation of the sac, its dissection and its subsequent opening. After the reduction of the viscera in the peritoneal cavity and their viscerolysis, the hernia sac is partially resected and closed. A retromuscular properitoneal prosthesis was placed according to the Rives-Stoppa procedure, circularly overcoming the defect on a length of 5 cm.
The fixation of the prosthesis is practiced at a distance from the edges of the defect, with several separate wires that cross the structures at the lateral edge of the right abdominal muscles. In order to close the sheaths of the right abdomen, a Biopro 3.0 Sourjet type of thread was used. The skin suture and the wound dressing conclude the operative act [15,16].
The (IPOM) procedure were performed under general anesthesia and involved performing pneumoperitoneum, either openly or with the help of the Veress needle in the Palmer point (the left subcostal space). The first 10 mm trocar was inserted in the Palmer point most of the time. A 30º laparoscope is used to check the entire peritoneal cavity and visualize all parietal defects.
Two 5 mm and 10/ 12mm working trocars are inserted, on the same side of the abdomen. In case of large defects, one or two trocars can be inserted on the opposite side, in order to facilitate the fixation of the prosthesis at the level of the anterior abdominal wall. The next operative time is to reduce the hernia content in the peritoneal cavity, viscerolysis of the adhesions and release on an area of at least 5 cm circular around the parietal defect of the adhesions.
The hernia sac is not resected in the laparoscopic procedure. The defect can be left open - s-IPOM procedure or, it can be closed using continuous intraperitoneal thread or separate wires passed transparietally - IPOM-plus procedure, which has the advantages of decreasing recurrence [17,18].
The mesh is then inserted into the peritoneal cavity through the 12 mm trocar. The mesh has 4 pre-assembled wires in the 4 cardinal points. With the help of the Reverdin needle, the 4 transfixing threads are removed through small incisions in the skin. With these threads, the mesh is fixed, the knots being buried in the subcutaneous tissue. Subsequently, the mesh is fixed on the inside with the help of plastic staples applied with the help of the ProTack. The mesh used is a Parietex ™ Optimized Composite Mesh made of polyester with absorbable collagen layers and pre- placed sutures that prevent the adhesion of the small intestine into it.
Results
The analysis of the distribution of the cases in the period between 2017 and 2020 shows that the number of hospitalizations for umbilical hernias was constantly increasing in the first 2 years included in the study, registering a peak in 2018, with 30 cases (37%). Subsequently, there is a slight decrease in the number of hospitalizations for this pathology with 17 cases in 2020 (21%). This can be explained by the pandemic of Coronavirus (SARS-CoV-2) and the low addressability of patients to medical services during this period.
The mean age in the study group was of 62.3+/-7.4 years. The age distribution revealed a predominance of the number of the cases observed in the age group 51-70 years, representing a percentage of 52% for 43 cases, followed by the age group over 70 years with 21 patients (26%) and the 41-50 age group with 14 cases (17%). The fewest cases were registered in the age group 31-40 years, representing only 5% of the whole studied group.

Table 1.
The characteristics of the patients included in the study group.
Table 1.
The characteristics of the patients included in the study group.
| No of patients (%) | |
| Age (years) | 62.3+-7.4 |
| Urban area | 54 (66%) |
| Rural area | 34 (34%) |
| Sex: | |
| 43 (52%) 39 (48%) |
| Comorbidities: | |
| 53 (64%) 15 (18%) 29 (35%) 47 (57%) |
| Type of umbilical hernia: | |
| 70 (85%) 12 (15%) |
Type of surgery:
| 36 (44%) 34 (41%) 12 (15%) |
Type of anesthesia
| 42 (51%) 40 (49%) |
Most patients came from urban areas (66%). The higher incidence of cases in urban areas can be explained by better accessibility and addressability to specialized medical services and a more developed health education, compared to patients from rural areas. Patients from rural areas often arrive at our clinic for an emergency, with complicated umbilical hernias, precisely due to the lack of easy access to specialized consultations.
There was no statistically significant difference regarding the patients’ gender, with 52% males vs. 48% females.
Out of the total number of patients included in the study, the most frequently encountered comorbidities were arterial hypertension (64%) and obesity (57%). Hepatopathies were present in 29 patients, representing 35% and type II diabetes and associated lung pathologies were associated with umbilical hernias to a lesser extent, namely 15 patients for each pathology.
The analysis of the distribution of cases, depending on the type of umbilical hernias shows that the number of hospitalizations for primary umbilical hernias had a much higher incidence (85%) as opposed to recurrent ones (15%). In addition, all patients with recurrent umbilical hernia were hospitalized for emergency surgery.
An important aspect that is worth mentioning is that all the patients hospitalized with the diagnosis of recurrent umbilical hernia have previously benefited from classic surgical treatment using the anatomical procedure.
In our departments, during the 4 years included in the study, three types of procedures were performed for the surgical treatment of umbilical hernia. The most frequently used procedure was the classic anatomical one (44%), followed by the classic procedure with textile allograft performed (41%) and IPOM laparoscopic procedure (15%). However, an important aspect to mention is the progressive annual increase in the use of laparoscopy in umbilical hernias. If in 2017, only one intervention was performed using this procedure, in 2020, 6 patients benefited from the IPOM procedure.
There is no significant difference in terms of the general vs. the spinal anesthesia used in the study group (51% vs. 49%). However, choosing the type of anesthesia was related to the type of hospitalization (acute/ chronic), the type of surgical procedure, but also to comorbidities. Patients who underwent the IPOM procedure benefited only from general anesthesia with oral intubation.
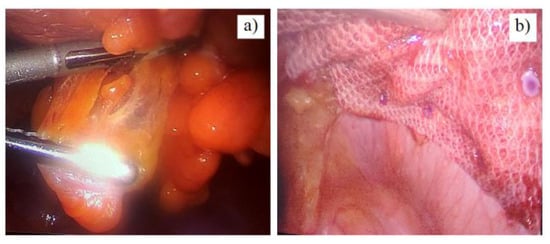
Figure 1.
Laparoscopic umbilical hernia repair: a) the dissection of the hernia sac; b) the fixation of the textile mesh—final aspect.
Another important parameter in the patients included in the study is the duration of their postoperative hospitalization, depending on the type of procedure used. Although the number of IPOM type surgeries was lower, a significant decrease in the number of hospitalization days can be observed in the patients who used this procedure.
Umbilical hernia surgery is generally considered a type of surgery with a low risk of morbidity. However, a number of postoperative complications can occur with more or less serious consequences. They can lead to both increased morbidity and costs through prolonged hospitalization. During the 4 years included in this study, no major postoperative complications or deaths occurred. The most common complications were: seroma (5%), followed by hematoma and wound infection (2.4%) (Table 2).

Table 2.
Postoperative outcomes in patients included in the study group.
These complications occurred after classical surgeries using anatomical or alloplastic procedures. There were no immediate postoperative complications among the patients undergoing the IPOM procedure.
Discussion
The results on the age group distribution in the present study are similar to the results of other research, thus showing an increased prevalence of umbilical hernias in patients over 40 years of age. A study conducted in Saudi Arabia in 2020, on a group of 500 participants, showed a maximum prevalence in the age group 40-59 years, followed by the age group> 60 years with a semi- significantly increased prevalence [19]. Another study showed a higher prevalence of umbilical hernias in men, aged between 60 and 70 years [20]. On the hand, other authors found umbilical hernias to be significantly more prevalent in females than in males, indicating that pregnancy is a significant etiological influence [21,22]. Obesity is another import risk factor, by different pathogenic pathways: the musculature can be overburdened through increased food intake, the visceral adiposity leads to a permanent increased abdominal pressure, but also adipose tissue will react to separate muscle bundles and layers, weaken aponeuroses, and it can have the appearance of abdominal hiatus and direct inguinal hernias [21]. On the other hand, intense physical effort is also associated with an increased risk of umbilical hernia, and this might be an explanation for the higher prevalence in males observed in some studies [23]. We noticed a slightly higher incidence in males, but not statically significant. Several studies show different results, some authors finding that a rate of umbilical hernia is up to five times more common in women [24], while others found an incidence of umbilical hernia repair twice as high in males as well in females [6]. The same study, however, mentions a variability in the results obtained, depending on the association of risk factors in people within the study group [6]. Another study conducted in 2017 showed a higher frequency of abdominal hernias in females, being associated with risk factors such as obesity, multiparity, history of abdominal surgery, personal history of abdominal hernias or history of abdominal trauma [21].
The chronic distension of the abdominal wall, with increasing intra-abdominal pressure during pregnancy in women, obesity, ascites or peritoneal dialysis cause the stretching of abdominal muscle fibers, the history of trauma and weakening of connective tissue being risk factors for hernia of the abdominal walls [11,25,26,27,28]. Asolati et al. [29] found that type 2 diabetes, hyperlipidemia, and the presence of human immunodeficiency virus (HIV) may be risk factors for the recurrence of umbilical hernias. Obesity, with a BMI> 30, has also been associated with higher recurrence rates. A recent study found that patients with a history of another form of abdominal hernia also have an increased risk of recurrence [5,30]. In addition, 20% of the patients with cirrhosis of the liver complicated by ascites have an umbilical hernia. Many recent studies have shown that the presence of ascites and associated liver disease increase the rate of intra- and postoperative complications in patients with umbilical hernias [31,32].
As more and more laparoscopic surgeries are being performed nowadays, umbilical port hernia is also an emerging disease, with an incidence estimated between 0.38% and 5.4%. The risk factors are the size of the trocar, the inadequate closing of the fascia, the male sex, obesity and connective tissue disorders [33,34].
Previous studies confirm the high recurrence rate in this procedure between 15 and 40% [35]. While the classic anatomical procedure will likely continue to be used to repair small umbilical hernias, mesh should be considered when the goal is to reduce recurrence in the repair of primary umbilical hernia. In the recurrence of this type of umbilical hernia, the alloplastic mesh should be the first choice for repair [35]. The anatomical procedure is widely used for umbilical hernia defects smaller than 2 cm, but when the defects are larger than 4 cm, this technique has been associated with high recurrence rates. The introduction of the alloplastic procedure reduced the risk of recurrence compared to the anatomical closure in the elective repair of the umbilical hernias, without any significant difference in terms of chronic postoperative pain [36].
The use of alloplastic mesh has proven to be beneficial in repairing incisional and inguinal hernias, and its use has become the gold standard in repairing both types of hernias [37,38]. However, the technique of elective surgical repair of umbilical hernias in adults using suture or mesh has been widely debated and the rates of reported complications related to both methods of repair differ from one study to another [39]. A study by Kaufmann et al. evaluated the efficacy of the alloplastic vs. anatomical procedure in terms of recurrence of umbilical hernia in hernia defects between 1 and 4 cm. The results showed a significantly lower recurrence rate in patients who benefited from the alloplastic procedure. A complex meta-analysis of several randomized controlled trials suggests that the use of the alloplastic procedure is associated with a reduced risk of recurrence, with no additional risk of wound infection, hematoma and seroma formation, and therefore open repair with textile allograft should be the preferred method of repairing the umbilical hernia [40,41].
Recently, an increasing number of laparoscopic surgeries have been performed for the treatment of umbilical hernias, due to the multiple benefits it can offer, such as: rapid socio-professional reintegration, short-term hospitalization and low incidence of recurrences. A recently published meta-analysis, which includes 3 randomized studies and 7 retrospective cohort studies, which enrolled a total of 16,549 patients, showed that alloplastic laparoscopic repair was associated with a significant reduction in recurrence rate, length of hospital stay, wound dehiscence and wound infection [42,43]. The results of the specialized studies coincide with the results obtained in the current study regarding the constant increase of laparoscopic procedures in the minimally invasive surgical treatment of umbilical hernias.
Spinal and general anesthesia have been shown to be effective anesthetic methods for patients undergoing open surgery for umbilical hernia repair, but both techniques are associated with some complications and side effects. The safety of the procedure should prevail based on the patient’s associated risk factors, the type of surgery and whether the patient is hospitalized or treated in an ambulatory care setting or in day-care centers [44,45]. Laparoscopic approaches impose the need for general anesthesia, which may be challenging in elderly patients, due to the frailty of the elderly [46]. Spinal anesthesia causes hypotension, urinary retention and prolonged motor recovery and all these may limit its routine use in outpatient surgery and in the geriatric population. On the other hand, spinal anesthesia provides excellent sensory and motor blockage, prolonged postoperative analgesia and significantly lower costs, being therefore a more appropriate and cost-effective alternative to general anesthesia. The results of a prospective study have shown that spinal anesthesia provides safe and reliable surgical anesthesia in adult patients undergoing surgical treatment of ventral hernia. Although general anesthesia has a more stable hemodynamic profile, spinal anesthesia provided fewer side effects and better control of postoperative pain [47].
During the Covid-19 pandemic, we observed an increased proportion of cases with umbilical hernias admitted to the emergency room. This may be correlated with the regulations during the lockdown periods, but also with the patients’ fear of Sars-cov-2 infection and self- isolation. In the patients admitted to the emergency room, the ischemic sufferance of the herniated bowel loop may be a trigger factor for systemic inflammation and sepsis. A careful perioperative approach is necessary especially in diabetic patients, associating cardiovascular diseases. Fluid and metabolic rebalance and infection control are associated with lower complications in the postoperative period [48,49,50]. By targeting inflammation in diabetic patients, physicians become able to improve insulin sensitivity and glucose control, thus relieving the risk of cardiovascular complications [51].
Postoperative adhesions after abdominal or pelvic surgery remain an important clinical problem causing infertility, pain and bowel obstruction. Minimally invasive techniques are associated with decreased peritoneal aggression and adherences formation. A comparative study conducted in Italy on a group of 523 patients diagnosed with ventral hernia aimed at establishing the safety profile, efficacy and feasibility of laparoscopy using composite mesh and tacks compared to the open alloplastic technique. Among the analyzed criteria, the following are worth mentioning: the duration of surgery, postoperative complications, the duration of the analgesic therapy, the restoration of the intestinal function, the average length of hospitalization, the mortality and recurrence rate at one year postoperatively. The results of the study highlighted the superiority of laparoscopy over open classical procedures. In the group that underwent laparoscopy with textile allograft, the duration of the operation was shorter, the rate of postoperative complications was 5% (compared to 14% in the other group), the restoration of the intestinal function was faster, there was less postoperative pain and a short-term analgesic therapy. The average length of the hospital stay was significantly reduced in the group that benefited from the laparoscopic procedure. The rate of postoperative complications was higher in the group that benefited from the classic procedure compared to the laparoscopic group, but the mortality rate was 0% for both techniques. At the postoperative reassessment after one year, a recurrence rate of 7% was observed for the classic open procedure and 4% for the laparoscopic procedure. Therefore, the laparoscopic procedure is an efficient and safe variant, with very low rates of morbidity and recurrence with multiple advantages compared to open procedures, related to the reduction of overall complications and the period of hospitalization with better patient comfort [50,51,52,53,54].
The use of a variety of prosthetic materials for the repair of umbilical hernias has led to a low recurrence rate compared to that of classical anatomical procedures. Subsequent studies on the type of surgery to repair the umbilical hernia have led surgeons to start using the laparoscopic procedure, as there is growing evidence that the use of laparoscopy in the surgical treatment of umbilical hernias is superior to the open alloplastic procedure in terms of postoperative complications, postoperative chronic pain, morbidity and overall mortality [55,56,57].
Composite meshes are the preferred materials in most cases to avoid the risk of visceral adhesion to the mesh, and laparoscopy also allows the identification of several previously undiagnosed hernia defects. In a recent series, the laparoscopic repair of the umbilical hernia using a two- layer polypropylene mesh and transfascial sutures significantly reduced wound infections, the length of the hospital stay, and the costs compared to the open alloplastic procedure [57,58,59].
Highlights
- ✓ The umbilical hernia is the second most common form of hernia in adults, after inguinal hernia, most frequently encountered in males aged between 51 and 70 years of age.
- ✓ The current trend is for the IPOM laparoscopic procedure, with its IPOM plus variant, to become a gold standard in the treatment of umbilical hernias, due to its minimum postoperative complications and quick recovery.
Conclusions
The umbilical hernia is a surgical condition that is more and more common nowadays. More than 10% of all operated hernias are umbilical and epigastric hernias. The alloplastic, classical or laparoscopic procedure has become the most used due to the benefits, such as: rapid socio- professional reintegration, short-term hospitalization and low incidence of relapses and postoperative complications. The current trend is for the IPOM laparoscopic procedure to become a gold standard in the treatment of umbilical hernias.
Conflicts of Interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
References
- Muysoms, F.E.; Miserez, M.; Berrevoet, F.; Campanelli, G.; Champault, G.G.; Chelala, E.; Dietz, U.A.; Eker, H.H.; El Nakadi, I.; Hauters, P.; et al. Classification of primary and incisional abdominal wall hernias. Hernia 2009, 13, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Kulacoglu, H. Current options in umbilical hernia repair in adult patients. Turk. J. Surg. 2015, 31, 157–161. [Google Scholar] [CrossRef]
- Kingsnorth, A.; LeBlanc, K. Hernias: Inguinal and incisional. Lancet 2003, 362, 1561–1571. [Google Scholar] [CrossRef]
- Klinge, U.; Prescher, A.; Klosterhalfen, B.; Schumpelick, V. Entstehung und Pathophysiologie der Bauchwanddefekte. Der Chir. 1997, 68, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Shankar, D.A.; Itani, K.M.F.; O’brien, W.J.; Sanchez, V.M. Factors Associated With Long-term Outcomes of Umbilical Hernia Repair. JAMA Surg. 2017, 152, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Dabbas, N.; Adams, K.; Pearson, K.; Royle, G. Frequency of abdominal wall hernias: Is classical teaching out of date? JRSM Short Rep. 2011, 2, 1–6. [Google Scholar] [CrossRef]
- Faylona, J.M. Evolution of ventral hernia repair. Asian J. Endosc. Surg. 2017, 10, 252–258. [Google Scholar] [CrossRef]
- Savlovschi, C.; Brănescu, C.; Serban, D.; Tudor, C.; Găvan, C.; Shanabli, A.; Comandaşu, M.; Vasilescu, L.; Borcan, R.; Dumitrescu, D.; et al. Amyand’s hernia—A clinical case. Chirurgia (Bucharest, Romania: 1990) 2010, 105, 409–414. [Google Scholar]
- Baylón, K.; Rodríguez-Camarillo, P.; Elías-Zúñiga, A.; Díaz-Elizondo, J.A.; Gilkerson, R.; Lozano, K. Past, Present and Future of Surgical Meshes: A Review. Membranes 2017, 7, 47. [Google Scholar] [CrossRef]
- Uysal, E.; Kırdak, T.; Sarkut, P.; Kaya, E.; Korun, N. Is the frequency of simultaneous umbilical hernia repairs in laparoscopic and open cholecystectomy similar? J. Clin. Investig. Surg. 2021, 6, 153–156. [Google Scholar] [CrossRef]
- Dumitrescu, D.; Savlovschi, C.; Borcan, R.; Pantu, H.; Serban, D.; Gradinaru, S.; Smarandache, G.; Trotea, T.; Branescu, C.; Musat, L.; et al. [Clinical case--voluminous diaphragmatic hernia--surgically acute abdomen: Diagnostic and therapeutical challenges]. Chirurgia (Bucur) 2011, 106, 657–660. [Google Scholar]
- A LeBlanc, K.; Booth, W.V. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: Preliminary findings. Surg Laparosc Endosc. 1993, 3, 39–41. [Google Scholar] [PubMed]
- Kumar, D. Outcome of four years experience in laparoscopic ventral hernia repair. Pak. J. Med Sci. 1969, 31, 987–990. [Google Scholar] [CrossRef]
- Radu, N.; Voicescu, M.; Radu, E.; Tanasescu, C. Biomaterial with antioxidant and antifungal activities, obtained from romanian indigenous plants. Mol. Cryst. Liq. Cryst. 2017, 655, 243–249. [Google Scholar] [CrossRef]
- Colavita, P.D.; Belyansky, I.; Walters, A.L.; Zemlyak, A.Y.; Lincourt, A.E.; Heniford, B.T.; Augenstein, V.A. Umbilical hernia repair with mesh: Identifying effectors of ideal outcomes. Am. J. Surg. 2014, 208, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Tanasescu, C.; Moisin, A.; Mihetiu, A.; Serban, D.; Costache, A.; Bratu, D.G. The use of polypropylene mesh in inguinal hernia surgery: A retrospective study. Exp. Ther. Med. 2021, 22, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Voeller, G.R.; Chin, A.K.; A LeBlanc, K. Novel Technique for Full-Thickness Abdominal Wall Closure in Laparoscopic Ventral Hernia Repair. Surg Technol Int. 2019, 35, 123–128. [Google Scholar]
- Bernardi, K.; Olavarria, O.A.; Holihan, J.L.; Kao, L.S.; Ko, T.C.; Roth, J.S.; Tsuda, S.; Vaziri, K.; Liang, M.K. Primary Fascial Closure During Laparoscopic Ventral Hernia Repair Improves Patient Quality of Life. Ann. Surg. 2020, 271, 434–439. [Google Scholar] [CrossRef]
- Mahfouz, M.E.M.; Al-Juaid, R.S. Prevalence and risk factors of abdominal hernia among Saudi population. J. Fam. Med. Prim. Care 2021, 10, 3130–3136. [Google Scholar] [CrossRef]
- Burcharth, J.; Pedersen, M.S.; Pommergaard, H.-C.; Bisgaard, T.; Pedersen, C.B.; Rosenberg, J. The prevalence of umbilical and epigastric hernia repair: A nationwide epidemiologic study. Hernia 2015, 19, 815–819. [Google Scholar] [CrossRef]
- Alsharif, M.M.; Hussain, M.A.; Alenezi, N.G.; Alenazi, A.A.; Almadani, S.A.; Alanazi, N.H.; Alshammari, J.H.; Altimyat, A.O.; Alanazi, T.H. Prevalence, risk factors and character of abdominal hernia in Arar City, Northern Saudi Arabia in 2017. Electron. Physician 2017, 9, 4806–4811. [Google Scholar] [CrossRef]
- Rutkow, I.M. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg. Clin. North Am. 2003, 83, 1045–1051. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Wang, H.; Zhou, J. Prevalence and Risk Factors of Hernia in Patients With Rectus Abdominis Diastasis: A 10-Year Multicenter Retrospective Study. Front. Surg. 2021, 8, 730875. [Google Scholar] [CrossRef]
- Khan, H.M.; Patwari, T.R. A comparative study of Desarda’s mesh free inguinal hernia repair with modified Bassini’s repair. J. Clin. Investig. Surg. 2021, 6, 104–115. [Google Scholar] [CrossRef]
- Celdrán, A.; Bazire, P.; A Garcia-Ureña, M.; Marijuán, J.L. H-hernioplasty: A tension-free repair for umbilical hernia. Br. J. Surg. 1995, 82, 371–372. [Google Scholar] [CrossRef] [PubMed]
- Radu, N.; Roman, V.; Bostan, M.; Radu, E.; Tanasescu, C. Influence of some spice food based bioproducts on human monocytic cells line type THP-1. Mol. Cryst. Liq. Cryst. 2017, 655, 114–123. [Google Scholar] [CrossRef]
- Popoiag, R.-E.; Stoian, A.; Suceveanu, A.; Mazilu, L.; Parepa, I.; Serban, L.; Paunica, M.; Motofei, C.; Braticevici, C. The relationship between gut microbiota and spontaneous bacterial peritonitis in patients with liver cirrhosis—A literature review. J. Mind Med Sci. 2019, 6, 26–30. [Google Scholar] [CrossRef]
- Asolati, M.; Huerta, S.; Sarosi, G.; Harmon, R.; Bell, C.; Anthony, T. Predictors of recurrence in Veteran patients with umbilical hernia: Single center experience. Am. J. Surg. 2006, 192, 627–630. [Google Scholar] [CrossRef]
- A Chatzizacharias, N.; Bradley, J.A.; Harper, S.; Butler, A.; Jah, A.; Huguet, E.; Praseedom, R.K.; Allison, M.; Gibbs, P. Successful surgical management of ruptured umbilical hernias in cirrhotic patients. World J. Gastroenterol. 2015, 21, 3109–3113. [Google Scholar] [CrossRef]
- Marsman, H.A.; Heisterkamp, J.; Halm, J.A.; Tilanus, H.W.; Metselaar, H.J.; Kazemier, G. Management in patients with liver cirrhosis and an umbilical hernia. Surgery 2007, 142, 372–375. [Google Scholar] [CrossRef]
- Aslani, N.; Brown, C.J. Does mesh offer an advantage over tissue in the open repair of umbilical hernias? A systematic review and meta-analysis. Hernia 2010, 14, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Socea, B.; Carap, A.; Bratu, O.G.; Diaconu, C.C.; Dimitriu, M.; Socea, L.I.; Bobic, S.; Constantin, V.D. The Role of the Composite and Biologic Meshes in the Trocar Site Hernia Repair Following Laparoscopic Surgery. Mater. Plast. 2018, 55, 146–148. [Google Scholar] [CrossRef]
- Sharma, R. The Earliest Presenting Umbilical Port Site Hernia Following Laparoscopic Cholecystectomy: A Case Report. J. Clin. Diagn. Res. 2016, 10, PD18–9. [Google Scholar] [CrossRef] [PubMed]
- Madsen, L.J.; Oma, E.; Jorgensen, L.N.; Jensen, K.K. Mesh versus suture in elective repair of umbilical hernia: Systematic review and meta-analysis. BJS Open 2020, 4, 369–379. [Google Scholar] [CrossRef]
- Tănăsescu, C.; Faur, M.; Sabău, D. Day-case Surgery in the Context of Inguinal Hernia Repair by the Modified Lichtenstein Technique - A Single Centre Experience. Chirurgia 2019, 114, 115–120. [Google Scholar] [CrossRef]
- van Veen, R.N.; Wijsmuller, A.R.; Vrijland, W.W.; Hop, W.C.; Lange, J.F.; Jeekel, J. Long-term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br. J. Surg. 2007, 94, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Winsnes, A.; Haapamäki, M.M.; Gunnarsson, U.; Strigård, K. Surgical outcome of mesh and suture repair in primary umbilical hernia: Postoperative complications and recurrence. Hernia 2016, 20, 509–516. [Google Scholar] [CrossRef]
- Kaufmann, R.; A Halm, J.; Eker, H.H.; Klitsie, P.J.; Nieuwenhuizen, J.; van Geldere, D.; Simons, M.P.; van der Harst, E.; Riet, M.v. '.; van der Holt, B.; et al. Mesh versus suture repair of umbilical hernia in adults: A randomised, double-blind, controlled, multicentre trial. Lancet 2018, 391, 860–869. [Google Scholar] [CrossRef]
- Shrestha, D.; Shrestha, A.; Shrestha, B. Open mesh versus suture repair of umbilical hernia: Meta-analysis of randomized controlled trials. Int. J. Surg. 2019, 62, 62–66. [Google Scholar] [CrossRef]
- Gonzalez, R.; Mason, E.; Duncan, T.; Wilson, R.; Ramshaw, B.J. Laparoscopic Versus Open Umbilical Hernia Repair. JSLS 2003, 7, 323–328. [Google Scholar]
- Hajibandeh, S.; Sreh, A.; Khan, A.; Subar, D.; Jones, L. Laparoscopic versus open umbilical or paraumbilical hernia repair: A systematic review and meta-analysis. Hernia 2017, 21, 905–916. [Google Scholar] [CrossRef] [PubMed]
- Șerban, D.; Brăneașcu, C.; Smarandache, G.; Tudor, C.; Tănăsescu, C.; Tudosie, M.; Stana, D.; Dascălu, A.; Spătaru, R. Safe Surgery in Day Care Centers: Focus on Preventing Medical Legal Issues. Romanian J. Leg. Med. 2021, 29, 60–64. [Google Scholar] [CrossRef]
- Diaconu, C.; Paraschiv, B.; Stanescu, A.M.A.; Pantea Stoian, A.; Nitipir, C.; Socea, B.; Bratu, O. Arterial Hypertension, a Frequent Comorbidity in Diabetes: The Perioperative Management. Proceedings of the 35th Balkan Medical Week. 35th Balkan Medical Week on Healthy Ageing An Endless Challenge. Athens, Greece, Sep 25-27, 2018. pp.15-20.
- Serban, D.; Socea, B.; Balasescu, S.A.; Badiu, C.D.; Tudor, C.; Dascalu, A.M.; Vancea, G.; Spataru, R.I.; Sabau, A.D.; Sabau, D.; et al. Safety of Laparoscopic Cholecystectomy for Acute Cholecystitis in the Elderly: A Multivariate Analysis of Risk Factors for Intra and Postoperative Complications. Medicina 2021, 57, 230. [Google Scholar] [CrossRef] [PubMed]
- Krobot, R.; Premuzic, J. Comparison of general and spinal anaesthesia in patients undergoing open ventral hernia repair. Periodicum Biologorum. 2013, 115, 225–229. [Google Scholar]
- Manea, M.; Hospital, B.E.U.C.M.; Marcu, D.; Motofei, I.; Socea, B.; Stoian, A.P.; Bratu, O.G.; Gaman, M.-A.; Gaman, A.M.; Stanescu, A.M.A.; et al. Cardiovascular risk in patients with inflamma-tory bowel diseases: A review. Romanian Biotechnol. Lett. 2019, 24, 366–373. [Google Scholar] [CrossRef]
- Hainaroșie, R.; Zainea, V.; Rusescu, A.; O Iana, R.; Ghindea, T.; Suceveanu, A.P.; Ștefanescu, D.C.; Ionita, I.G.; Pietroșanu, C.; Stoian, A.P.; et al. Management of infectious complications in diabetes mellitus patients. Romanian J. Mil. Med. 2019, 122, 46–51. [Google Scholar] [CrossRef]
- Ardeleanu, V.; Chicos, S.; Tutunaru, D.; Georgescu, C. A rare case of acute abdomen: Garengeot hernia. Chirurgia (Bucur) 2013, 108, 896–899. [Google Scholar]
- Helvacioglu, C.; Ekin, M.; Yasar, L. Comparing quality-of-life scores on patients with sacrospinal ligament fixation versus LeFort colpoclesis for pelvic organ prolapse. J. Clin. Investig. Surg. 2020, 5, 39–42. [Google Scholar] [CrossRef]
- Suceveanu, A.-I.; Mazilu, L.; Katsiki, N.; Parepa, I.; Voinea, F.; Pantea-Stoian, A.; Rizzo, M.; Botea, F.; Herlea, V.; Serban, D.; et al. NLRP3 Inflammasome Biomarker—Could Be the New Tool for Improved Cardiometabolic Syndrome Outcome. Metabolites 2020, 10, 448. [Google Scholar] [CrossRef]
- Fometescu, S.G.; Costache, M.; Coveney, A.; Oprescu, S.M.; Serban, D.; Savlovschi, C. Peritoneal fibrinolytic activity and adhesiogenesis. Chirurgia (Bucur) 2013, 108, 331–340. [Google Scholar]
- Fabozzi, M.; Allieta, R.; Grimaldi, L.; Reggio, S.; Amato, B.; Danzi, M. Open vs laparoscopic repair of abdominal hernia: A case control study in over 60 years old patients. BMC Surg. 2013, 13, A19. [Google Scholar] [CrossRef]
- Roman, M.D.; Fleaca, R.S.; Boicean, A.; Bratu, D.; Birlutiu, V.; Rus, L.L.; Tantar, C.; Mitariu, S.I.C. Assesment of Synovial Fluid pH in Osteoarthritis of the HIP and Knee. Rev. Chim. 2017, 68, 1242–1244. [Google Scholar] [CrossRef]
- Stoian, A.; Hainarosie, R.; Pietrosanu, C.; Rusescu, A.; Andronache, L.; Paunica, S.; Balalau, C.; Pituru, T. Modern concepts in non-surgical esthetics; a review. J. Mind Med Sci. 2019, 6, 190–195. [Google Scholar] [CrossRef]
- Radu, N.; Roman, V.; Tănăsescu, C. Biomaterials obtained from probiotic consortia of microorganisms. Potential applications in regenerative medicine. Mol. Cryst. Liq. Cryst. 2016, 628, 115–123. [Google Scholar] [CrossRef]
- Rezaei, F.; Hassan, H.; Fallahi, A.; Gheshlagh, R.; Sadeghi, S.; Fallahi, P.; Nemat, B. The relationship between spiritual health and social trust among students. J. Mind Med Sci. 2021, 8, 100–107. [Google Scholar] [CrossRef]
- Abhinava, D.M.; Shashidhara, N.C.; Seshagiri, R.K.; Santhosh, C.S.; Mallikarjuna, N.M.; Niranjan, N. A clinical study of laparoscopic versus open umbilical hernia repair. Surgical Update: Int J Surg Orthop. 2017, 3, 157–161. [Google Scholar]
- Cofaru, N.F.; Roman, M.D.; Cofaru, I.I.; Oleksik, V.S.; Fleaca, S.R. Medial Opening Wedge High Tibial Osteotomy in Knee Osteoarthritis—A Biomechanical Approach. Appl. Sci. 2020, 10, 8972. [Google Scholar] [CrossRef]
- Tollens, T.; Struyve, D.; Aelvoet, C.; Vanrijkel, J.P. Introducing the Proceed Ventral Patch as a new device in surgical management of umbilical and small ventral hernias: Preliminary results. Surg Technol Int. 2010, 19, 99–103. [Google Scholar]
© 2022 by the author. 2022 Andrei Moisin, Mihai Faur, Carmen Popa, Claudia Diana Gherman, Victor Dumitrescu, Denisa Tanasescu, Adrian Boicean, Simona Balasescu, Meda Comandasu, Dan Dumitrescu, Anca Zgura, Calin Mohor