When Myocardial Infarction Is Choosing Young Victims
Abstract
Introduction
Case Presentation
- Surgical coronary revascularization - double coronary bypass graft using left internal mammary artery–on the anterior descending artery and right internal—on the intermediate artery.
- Sub-occlusion of anterior descending artery and intermediate branch.
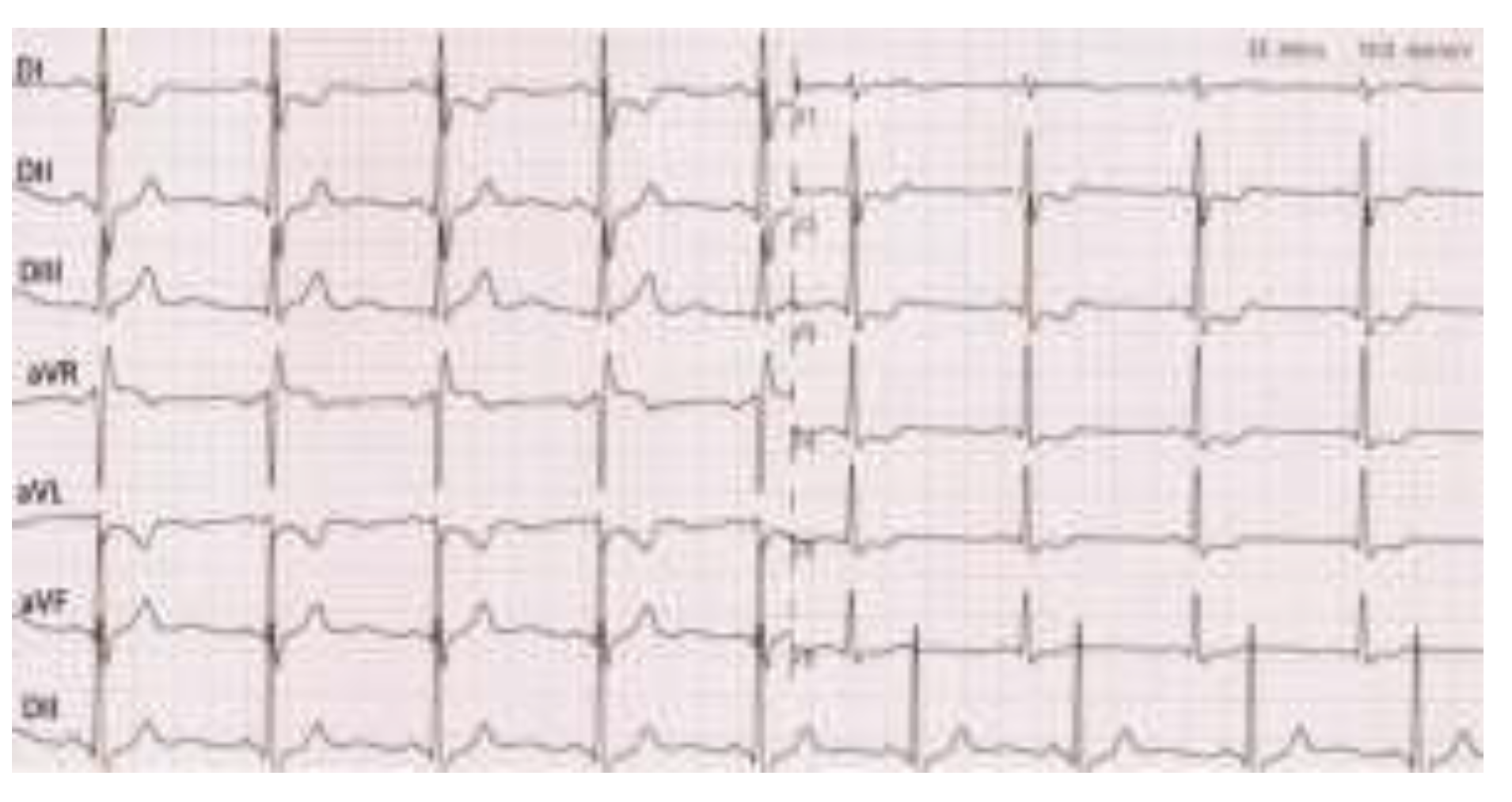
- Non-ST segment elevation myocardial infarction.
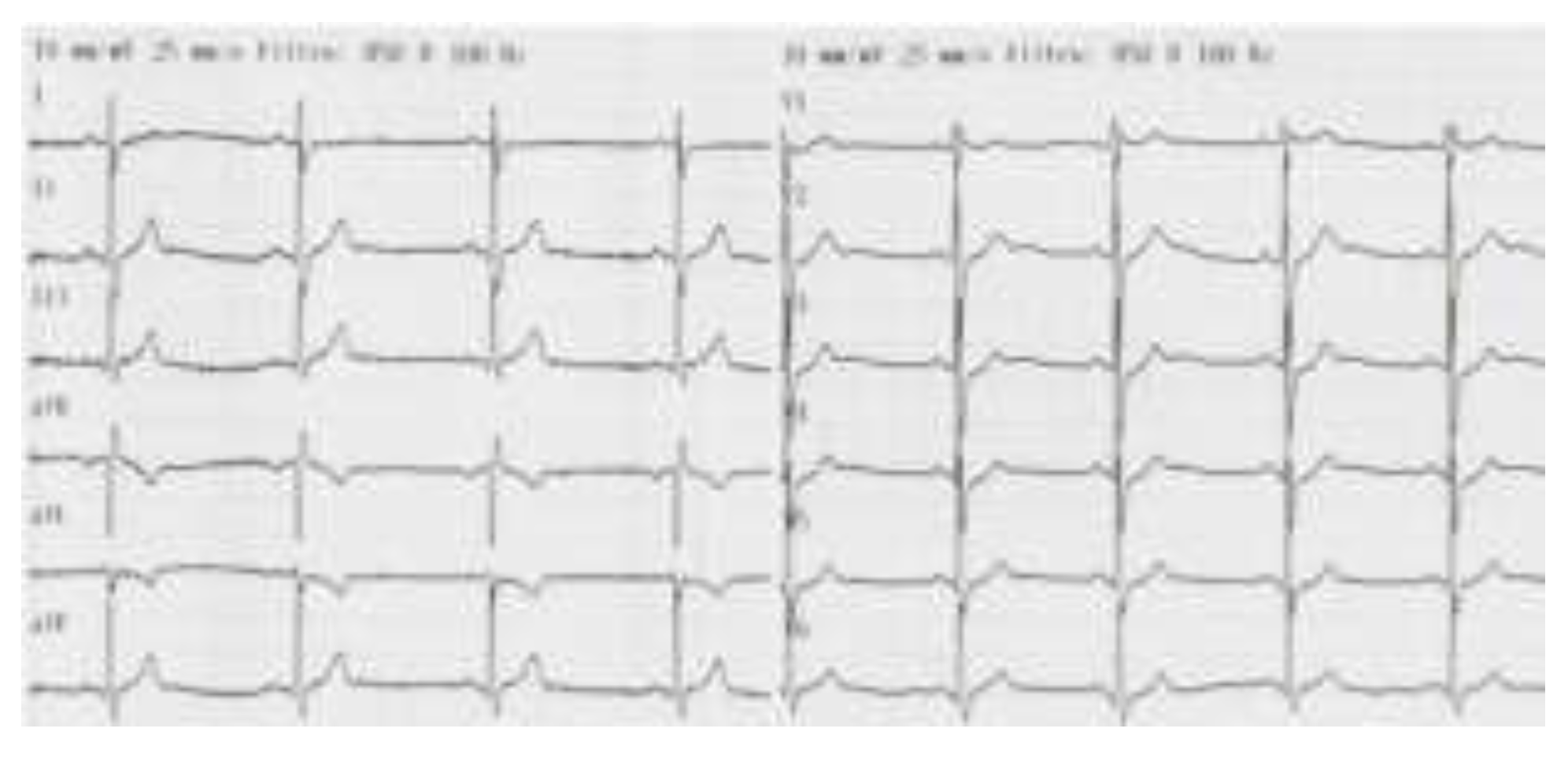
- Incomplete right bundle branch block.
Discussions
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
References
- Sanchis-Gomar, F.; Perez-Quilis, C.; Leischik, R.; Lucia, A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann Transl Med. 2016, 4, 256. [Google Scholar] [CrossRef] [PubMed]
- Yazdanyar, A.; Newman, A.B. The burden of cardiovascular disease in the elderly: Morbidity, mortality, and costs. Clin Geriatr Med. 2009, 25, 563-vii. [Google Scholar] [CrossRef]
- Egred, M.; Viswanathan, G.; Davis, G.K. Myocardial infarction in young adults. Postgrad Med J. 2005, 81, 741–745. [Google Scholar] [CrossRef]
- Innstrand, S.T.; Langballe, E.M.; Falkum, E.; Aasland, O.G. Exploring within- and between-gender differences in burnout: 8 different occupational groups. Int Arch Occup Environ Health. 2011, 84, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Kivimaki, M.; Nyberg, S.T.; Fransson, E.I.; Heikkila, K.; Alfredsson, L.; Casini, A.; et al. Associations of job strain and lifestyle risk factors with risk of coronary artery disease: A meta-analysis of individual participant data. CMAJ. 2013, 185, 763–769. [Google Scholar] [PubMed]
- Egred, M.; Viswanathan, G.; Davis, G.K. Myocardial infarction in young adults. Postgrad Med J. 2005, 81, 741–745. [Google Scholar] [CrossRef]
- Bhardwaj, R.; Kandoria, A.; Sharma, R. Myocardial infarction in young adults-risk factors and pattern of coronary artery involvement. Niger Med J. 2014, 55, 44–47. [Google Scholar] [CrossRef]
- Zimmerman, F.H.; Cameron, A.; Fisher, L.D.; Ng, G. Myocardial infarction in young adults: Angiographic characteristics, risk factors and prognosis, coronary artery surgery study register (CASS). J Am Coll Cardiol. 1995, 26, 654–61. [Google Scholar]
- Mukherjee, D.; Hsu, A.; Moliterno, D.J.; Lincoff, A.M.; Goormastic, M.; Topol, E.J. Risk factors for premature coronary artery disease and determinants of adverse outcomes after revascularization in patients less than 40 years old. Am J Cardiol. 2003, 92, 1465–7. [Google Scholar]
- Deshmukh, P.P.; Singh, M.M.; Deshpande, M.A.; Rajput, A.S. Clinical and angiographic profile of very young adults presenting with first acute myocardial infarction: Data from a tertiary care center in Central India. Indian Heart J. 2019, 71, 418–421. [Google Scholar] [CrossRef]
- Laslo, C.L.; Pantea Stoian, A.; Socea, B.; et al. New oral anticoagulants and their reversal agents. J Mind Med Sci. 2018, 5, 195–201. [Google Scholar] [CrossRef]
- Diaconu, C.; Paraschiv, B.; Stanescu, A.M.A.; et al. Arterial Hypertension, a Frequent Comorbidity in Diabetes: The Perioperative Management. In Proceedings of the 35th Balkan Medical Week on Healthy Ageing-An Endless Challenge, Athens, Greece, 25–27 September 2018; pp. 15–20. [Google Scholar]
- Cozma, M.A.; Gaman, M.A.; Dobrica, E.C.; et al. Beta-Blockers in the Treatment of Chronic Heart Failure: Did Gender Make a Difference? In Proceedings of the 35th Balkan Medical Week on Healthy Ageing-An Endless Challenge, Athens, Greece, 25–27 September 2018; pp. 21–26. [Google Scholar]
- Waller, B.F. Schlant, R.C., Alexander, R.W., O’Rourke, R.A., Roberts, R., Sonnenblick, E.H., Eds.; Nonatherosclerotic causes of coronary artery narrowing. In The Heart, 8th ed.; Mc Graw Hill, 1994; pp. 1239–1261. [Google Scholar]
- McGill, H.C., Jr.; McMahan, C.A.; Herderick, E.E.; Malcom, G.T.; Tracy, R.E.; Strong, J.P. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr. 2000, 72 (Suppl. S5), 1307S–1315S. [Google Scholar] [PubMed]
- Egred, M.; Viswanathan, G.; Davis, G.K. Myocardial infarction in young adults. Postgrad Med J. 2005, 81, 741–745. [Google Scholar]
- Chen, L.; Chester, M.; Kaski, J.C. Clinical factors and angiographic features associated with premature coronary artery disease. Chest 1995, 108, 364–369. [Google Scholar]
- Mazilu, L.; Stanculeanu, D.L.; Gheorghe, A.D.; Voinea, F.; et al. Incidenced of Chemotherapy Induced Paripheral Neuropathy in Cancer Patients in clinical Practice. Farmacia 2018, 66, 904–908. [Google Scholar]
- Tuta, L.A.; Iorga, I.; Azis, O.; Voinea, F. End-of-life Care in Erderly Patients with End-Stage Renal Disease–Ethical and Clinical Issues. In SGEM 2015, Book 1: Psychology and Psyhiatry, Sociology and Healthcare, Education Conference Proceedings; 2015; pp. 487–493. [Google Scholar]
- Ong, P.; Athanasiadis, A.; Hill, S.; Vogelsberg, H.; Voehringer, M.; Sechtem, U. Coronary artery spasm as a frequent cause of acute coronary syndrome: The CASPAR (Coronary Artery Spasm in Patients With Acute Coronary Syndrome) Study. J Am Coll Cardiol. 2008, 52, 523–527. [Google Scholar]
- Fulga, I.; Georgescu, C.; Ardeleanu, V. Single arterial trunk arising from the aortic arch with aortic coarctation. Report of a case. Embryological considerations. Rom J Morphol Embryol. 2014, 55, 165–169. [Google Scholar]
- Settineri, S.; Frisone, F.; Alibrandi, A.; Pino, G.; Lupo, N.J.; Merlo, E.M. Psychological Types and Learning Styles. Mediterr. J. Clin. Psychol. 2018, 6. [Google Scholar] [CrossRef]
- Suceveanu, A.I.; Mazilu, L.; Voinea, C.; Suceveanu, A.P. Concomitant Serum Presence of Hepatitis B Surface Antigen (HBsAg) and High Titers of Hepatitis B Surface Antibodies (Anti-HBsAb) in a Patient with Chronic Hepatitis B (HBV) Genotype D from Black Sea Coast Region: A Case Report. Hepat. Mon. 2018, 18, e60156. [Google Scholar]
- Tobaldini, E.; Fiorelli, E.M.; Solbiati, M.; Costantino, G.; Nobili, L.; Montano, N. Short sleep duration and cardiometabolic risk: From pathophysiology to clinical evidence. Nat Rev Cardiol. 2019, 16, 213–224. [Google Scholar] [CrossRef]
- Blieden, L.C.; Moller, J.H. Cardiac involvement in inherited disorders of metabolism. Prog Cardiovasc Dis. 1974, 16, 615–631. [Google Scholar] [CrossRef] [PubMed]
- Moraru, D.; Suceveanu, A.P.; Pantea Stoian, A.; Nitipir, C.; Pituru, S.; Voinea, F.; Timofte, D.; Suceveanu, A.I. Amyloidosis–the importance of an early diagnosis. In Proceeding of 35 Balkan Medical Week, Athens, Greece, 25–27 September; pp. 182–6.
- Leblebicioglu, H.; Arama, V.; Causse, X.; et al. Predictors associated with treatment initiation and switch in a real- world chronic hepatitis B population from five European countries. J Viral Hepat. 2014, 21, 662–670. [Google Scholar] [CrossRef] [PubMed]
- Suceveanu, A.I.; Mazilu, L.; Tomescu, D.; Ciufu, N.; Parepa, I.R.; Suceveanu, A.P. Screening of hepatopulmonary syndrome (HPS) with CEUS and pulse-oximetry in liver cirrhosis patients eligible for liver transplant. Chirurgia (Bucur). 2013, 108, 684–688. [Google Scholar]
- Tofolean, D.E.; Mazilu, L.; Stăniceanu, F.; et al. Clinical presentation of a patient with cutis laxa with systemic involvement: A case report. Rom J Morphol Embryol. 2015, 56, 1205–1210. [Google Scholar]
- Parepa, I.R.; Suceveanu, A.I.; Mazilu, L.; Mohamed, A.; Niţă, D.; Tuţă, L.A. Preventing cardiac complications after non-cardiac non-vascular surgery by using perioperative statin therapy–A prospective study in Constanţa County, Romania. Farmacia 2017, 65, 120–124. [Google Scholar]
- Motofei, I.G. A dual physiological character for cerebral mechanisms of sexuality and cognition: Common somatic peripheral afferents. BJU Int. 2011, 108, 1634–1639. [Google Scholar] [CrossRef]
- Brill, I.C.; Brodeur, M.T.H.; Oyama, A.A. Myocardial infarction in two sisters less than 20 years old. J Am Med Assoc. 1971, 217, 1345–1348. [Google Scholar]
- De Vente, W.; Olff, M.; Van Amsterdam, J.G.; Kamphuis, J.H.; Emmelkamp, P.M. Physiological differences between burnout patients and healthy controls: Blood pressure, heart rate, and cortisol responses. Occup Environ Med. 2003, 60 (Suppl. S1), i54–i61. [Google Scholar]
- Merlo, E.M. Opinion Article: The role of psychological features in chronic diseases, advancements and perspectives. Mediterr. J. Clin. Psychol. 2019, 7. [Google Scholar] [CrossRef]
- Bargellini, A.; Barbieri, A.; Rovesti, S.; Vivoli, R.; Roncaglia, R.; Borella, P. Relation between immune variables and burnout in a sample of physicians. Occup. Environ. Med. 2000, 57, 453–457. [Google Scholar] [CrossRef]
- Dimitriu, M.C.T.; Pantea-Stoian, A.; Smaranda, A.C.; et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. 2020, 144, 109972. [Google Scholar] [CrossRef] [PubMed]
- Mazilu, L.; Parepa, I.R.; Suceveanu, A.I.; Suceveanu, A.P.; Baz, R.; Catrinoiu, D. Venous thromboembolism: Secondary prevention with dabigatran vs. acenocumarol in patients with paraneoplastic deep vein thrombosis. Results from a small prospective study in Romania. Cardiovasc. Res. J. 2014, 103 (Suppl. S1), S39. [Google Scholar] [CrossRef][Green Version]
- Izawa, S.; Sugaya, N.; Yamamoto, R.; Ogawa, N.; Nomura, S. The cortisol awakening response and autonomic nervous system activity during nocturnal and early morning periods. Neuro Endocrinol Lett. 2010, 31, 685–689. [Google Scholar] [PubMed]
- Stefano, G.B.; Kream, R.M. Reciprocal regulation of cellular nitric oxide formation by nitric oxide synthase and nitrite reductases. Med Sci Monit. 2011, 17, RA221–RA226. [Google Scholar] [CrossRef]
- Esch, T.; Stefano, G.B.; Fricchione, G.L.; Benson, H. Stress-related diseases-a potential role for nitric oxide. Med Sci Monit. 2002, 8, RA103–RA118. [Google Scholar]
- Coco, H.; Oliveira, A.M. Endothelial Dysfunction Induced by Chronic Psychological Stress: A Risk Factor for Atherosclerosis. Cardiovasc. Pharmacol Open Access 2015, 4, 5. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, L.; Zhang, M.; et al. Relationship of depression, stress and endothelial function in stable angina patients. Physiol Behav. 2013, 118, 152–158. [Google Scholar] [CrossRef]
- Parepa, I.R.; Stoian, A.P.; Radulescu, A.M.; Tica, I.; Mazilu, L.; Stanculeanu, A.L.; Suceveanu, A.P.; Serafinceanu, C.; Suceveanu, A.I. Involvement of Adiponectin in Early Phase of Acute Myocardial Infarction with ST- Segment Elevation (STEMI). REV CHIM 2019, 70, 522–526. [Google Scholar] [CrossRef]
- Mazilu, L.; Suceveanu, A.I.; Tomescu, D.; et al. Optimizing the indication for breast-conservative surgery (BCS) in patients with locally-advanced breast cancer. Chirurgia 2013, 108, 478–481. [Google Scholar]
- Huang, C.J.; Webb, H.E.; Zourdos, M.C.; Acevedo, E.O. Cardiovascular reactivity, stress, and physical activity. Front Physiol. 2013, 4, 314. [Google Scholar] [CrossRef]

© 2020 by the author. 2020 Cristina Nedelcu, Mihaela Ionescu, Paris Ionescu, Paris Ionescu, Vitalie Morosanu, Gabriel Smarandache, Dumitru Cristinel Badiu, Florentina Gherghiceanu, Vlad Denis Constantin, Emanuele Maria Merlo, Daniel Niţă
Share and Cite
Nedelcu, C.; Ionescu, M.; Ionescu, P.; Morosanu, V.; Smarandache, G.; Badiu, D.C.; Gherghiceanu, F.; Constantin, V.D.; Merlo, E.M.; Niţă, D. When Myocardial Infarction Is Choosing Young Victims. J. Mind Med. Sci. 2020, 7, 233-238. https://doi.org/10.22543/7674.72.P233238
Nedelcu C, Ionescu M, Ionescu P, Morosanu V, Smarandache G, Badiu DC, Gherghiceanu F, Constantin VD, Merlo EM, Niţă D. When Myocardial Infarction Is Choosing Young Victims. Journal of Mind and Medical Sciences. 2020; 7(2):233-238. https://doi.org/10.22543/7674.72.P233238
Chicago/Turabian StyleNedelcu, Cristina, Mihaela Ionescu, Paris Ionescu, Vitalie Morosanu, Gabriel Smarandache, Dumitru Cristinel Badiu, Florentina Gherghiceanu, Vlad Denis Constantin, Emanuele Maria Merlo, and Daniel Niţă. 2020. "When Myocardial Infarction Is Choosing Young Victims" Journal of Mind and Medical Sciences 7, no. 2: 233-238. https://doi.org/10.22543/7674.72.P233238
APA StyleNedelcu, C., Ionescu, M., Ionescu, P., Morosanu, V., Smarandache, G., Badiu, D. C., Gherghiceanu, F., Constantin, V. D., Merlo, E. M., & Niţă, D. (2020). When Myocardial Infarction Is Choosing Young Victims. Journal of Mind and Medical Sciences, 7(2), 233-238. https://doi.org/10.22543/7674.72.P233238


