Abstract
Introduction. The malfunction of the supporting pelvic system generates signs and symptoms that require various procedures. The aim of our study was to evaluate whether vaginal surgical interventions for genital prolapse or urinary incontinence have an impact on patients’ sexual quality of life. Materials and methods. We studied 40 eligible women who underwent vaginal surgical procedures in Saint John Hospital, Bucharest. Patients completed a questionnaire 6 months after the intervention. Results. Patients who underwent vaginal surgery for prolapse were 50-64 years of age. The most frequent vaginal surgical intervention was vaginal hysterectomy (32.5%), followed by anterior and posterior colporaphy (17.5%), and direct cystopexy (15.0%). Regarding their sexual life, 42.5% patients described improvement in sexual life, 22.5% described decreased libido after surgery, and 35% indicated no significant improvement. 57.5% of women indicated that they had no sexual discomfort (57.5%), whereas 27.5% had dyspareunia and 15% had dysuria. There was no negative impact on patients’ male partner quality of sexual intercourse after intervention. Conclusions. Vaginal surgical interventions for genital prolapse or urinary incontinence do not appear to lead to significant alteration of quality of sexual life in women.
Introduction
The dysfunction of the supporting pelvic system generates a multitude of signs and symptoms which, independent of their magnitude, usually have an anatomical correspondent. Regarding pelvic static disorders, however, the extent of the symptoms is not often directly proportional with the organic damage [1]. As a consequence, severe forms of prolapses may be accompanied by few symptoms such as urinary incontinence, whereas small changes not visible macroscopically, may generate alarming symptoms like incontinence, urinary imperiousness, or nycturia [2].
Any involuntary urine loss is defined as urinary incontinence, and it affects around 26-61% of women [3]. This pathology may be present in many cases for a long period of time without diagnosis or adequate treatment because of the patient’s embarrassment and fear of possible surgery. The most used diagnosis tools are clinical examination and ultrasound evaluation [4]. Epidemiologically, the urinary incontinence is associated with a sexual dysfunction in 26 to 47% cases [5]. Although it is not known which type of urinary incontinence is most correlated with severe sexual dysfunction, a recent study has highlighted that in emergency incontinence, vaginal lubrication is inadequate, whereas in mixed incontinence, sexual satisfaction is mainly affected [6].
The purpose of our study was to evaluate whether vaginal surgical procedures for genital prolapse or urinary incontinence have an impact on patients’ sexual quality of life (QoL).
Materials and Methods
The study was conducted in 2018, at Saint John Emergency Hospital in Bucharest. This pilot study retrospectively evaluated the quality of sexual life in patients who underwent vaginal surgery between 2015–2017 in our unit. We preferred an experimenter-derived questionnaire that could be adapted to the local and cultural conditions of the study. Patients were retrospectively enrolled and questionnaires were given via phone conversation in order to obtain immediate answers using “yes or no” responses. Each of the 40 patients completed the 12-item quality-of-life assessment, at least 6 months after the intervention.
The questionnaire included two types of items. The first section included epidemiologic and surgical data (age, environment, menopause status, type of surgical intervention, days of hospitalization). The second section included specific questions about quality of sexual life, including “Do you have vaginal dryness?”, “Did you have this symptom before the surgical intervention?”, “Did the vaginal surgical intervention affect your sexual life?”, “ If so, in what way?”, “How long until you had sexual contact after intervention?”, “ Do you have pain during sexual intercourse?”, “Did you have pain during sexual intercourse before operation?”, “Do you have other disturbing symptoms during sex?”, “Does your sexual partner report unpleasant symptoms during sexual intercourse after your vaginal intervention?”
Data were analyzed using SPSS version 20.0. Sample characteristics of the entire were evaluated using descriptive statistics and frequencies. Pearson correlations were used to investigate relationships among variable, using p < .05 for significance.
Results
Based on our patient database, 275 patients were identified for participation in the study. Of these, we were able to contact 126, and 47 agreed to complete the questionnaire. Of these, 7 women did not have sexual life after surgery, resulting in a count of 40 eligible participants.
Study group characteristics
The age distribution of the patients shows that most were 50-64 years of age, being followed on the second place by those between 35-49 years old. Taking into consideration that low socio-economic and cultural environment negatively influences the level of information and the openness of the patient-doctor relationship, we have taken into consideration the origin of the patient (urban or rural), with 62.5% of the patients from urban area. 30 (75%) out of 40 patients were menopausal, with only 10 (25%) premenopausal.
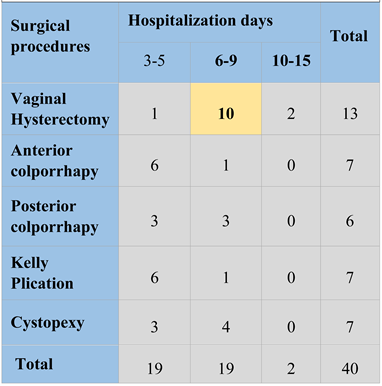
In Figure 1, distribution of surgical procedures is presented. The most frequent procedure (32.50%) was vaginal hysterectomy. Anterior and posterior colporraphy, associated with Kelly approach showed equal percentages (17.50%), followed by direct cystopexy (15%).
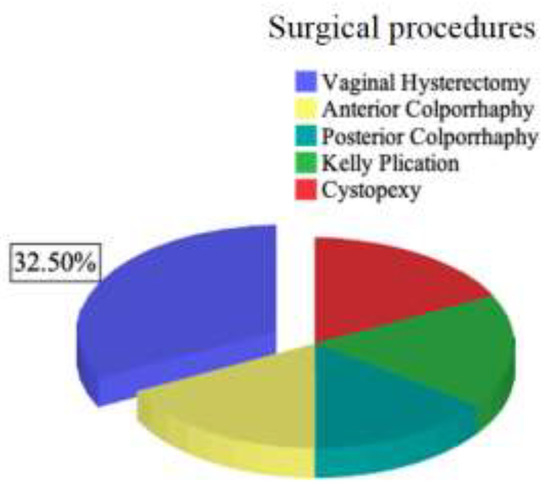
Figure 1.
Surgical procedures.
Each surgical procedure has its own particularities in terms of technique, recovery period, complete or partial remission of symptoms etc.
Table 1 shows how specific procedures affect the number of hospitalization days. As expected, vaginal hysterectomy requires the longest period for an adequate recovery (6-9 days).

Table 1.
Hospitalization days.
Considering that certain comorbidities have a major influence on the quality of sexual life, we analyzed their rates within our sample. 45.5% of patients had associated cardiovascular disease, 32.2 % had metabolic disorders (diabetes, obesity), 8.3% had neoplasia, 6.6% had chronic infections, and 7.4% had no comorbidities.
Quality of Life (QoL) evaluation
Figure 2 shows that surgical vaginal procedures did not have a negative impact on the sexual life quality of patients, where it can be noted that 9 patients reported an improvement and 14 patients report no change in their sexual life. Specifically, 42.5% patients described improvement of sexual life, 22.5% described decreased libido after surgery, whereas 35% of them answered that was no significant improvement.
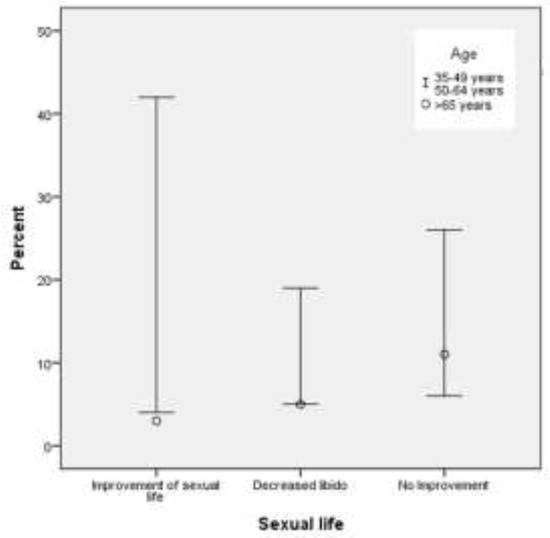
Figure 2.
The sexual life appreciation of the patients.
However, vaginal dryness was an issue, with 35% of patients reported this complaint before surgery but 55% reported it after surgery. However, 47.5% of patients described vaginal pain before surgery and 39.3% after surgery.
Patients’ sexual life was resumed in 3-5 months after operation for 47.5% patients 8.7% in 2 months, and 4.7% in 7 to 10 months. 57.5% of women enrolled in the study declared that they have no sexual discomfort, 27.5% had dyspareunia, and 15% described dysuria for few days after sexual intercourse.
When patients were interviewed about pleasure during sex, 72.5% confirmed experiencing sexual pleasure following surgical intervention. Regarding partner pleasure, 87.5% of men reported experiencing sexual pleasure with their partner after the partner’s surgery. There is a strong correlation between the pleasure of the patients after the surgical procedures with the partner’s pleasure (p < 0.01).
Discussions
The literature data often reports a high prevalence of sexual dysfunctions among women with pelvic static disorders, a condition that sometimes leads to decreased quality of sex life [7]. Studies have reported that women with symptomatic genital prolapse are much more likely to avoid sexual contact than the asymptomatic women, for different reasons [8].
Because quality-of-life issues are important for modern medicine, we investigated the physiological and psychological impact certain procedures have on the sexual life of female patients [9,10]. We noted that 75% of the patients in our study were post-menopausal women, who were prone to dryness and discomfort during sexual contact due to the low levels of vaginal estrogens.
Vaginal hysterectomy represents one of the most common treatment procedures for advanced genital prolapse. The impact of such surgery on Nepalese women with genital prolapse has recently been assessed. The results of the study showed that the quality of life improved for these women after surgery. Thus, vaginal hysterectomy is the best recommendation for the treatment of total pelvic prolapse in low-income countries [11]. The results of our study are similar, vaginal hysterectomy being the most common vaginal intervention applied among the interviewed women.
Different authors evaluated the role of native tissue used for vaginal apical prolapse repair with anti- incontinence surgery and the impact on women's sexual function, generally in a period of 24 months [12]. Another study assessed the surgical success of vaginal native tissue repair for rectocele and the impact on quality of life and sexual function. Vaginal native tissue repair proved to be a safe surgical procedure for symptomatic rectocele (with minimum complications), removing the symptoms of the genitals and improving the quality of life and sexual function [13].
Over time, studies have correlated different vaginal surgical approaches and their impact on women's quality of life. For example, to prevent vaginal vault prolapse after vaginal hysterectomy, modified McCall culdoplasty or Shull suspension was used in a retrospective study that included 414 patients who underwent vaginal hysterectomy for genital prolapse. The results of the study showed that both surgical procedures are effective in preventing vaginal vault prolapse, but the Shull technique is associated with better sexual function [14]. In parallel, other studies have shown effects on quality of life in women with apical pelvic organ prolapse treated with Vaginal Uphold™ System. This technique improves the quality of life among them, but the results showed that it worsened the sexual function postoperatively [15,16]. Meanwhile, vaginal mesh surgery may be the subject of a long debate because of the impact caused by mesh- related complications on patient's lives. Before surgery, patients should receive information from physicians about the potential adverse complications related to vaginal mesh surgery. But it is essential to present them that mesh-related side effects do not negatively affect quality of life regarding defecation, micturition, and sexual functioning [16,17,18]. In our study, women were beneficial of native tissue or mesh techniques for genital prolapse, in which there was no significant correlation between the impact of the surgical approach and the quality of life or sexual function.
Other authors evaluated the health-related quality of life after surgical removal of vaginally mesh used for pelvic organ prolapse, the authors trying to observe possible predictors of surgical management. Only half of the patients reported an overall improvement after the surgery, but with an insignificant improvement in dyspareunia. Patients who underwent complete mesh excision described notable improvement [19,20]. According to our results, there was no patient with altered quality of life due to mesh complications or removal during the study period.
Another surgical procedure for genital prolapse is the colpocleisis, which is considered a useful method for selected women. Its consequences on patients' postoperative quality of life have been studied very rarely. A recent study proved that colpocleisis has a good impact regarding the quality of life of the patients, but the major limiting condition is represented by selection criteria. It is recommended that the gynecologist discuss in detail with the elderly women about this type of vaginal obliterative surgery [21,22,23]. Even if colpocleisis is a frequent procedure performed in our clinic, we excluded those patients because we wouldn’t have the possibility to obtain answers about their sexual life.
There is usually a report on the need for additional treatments, symptoms, satisfaction and quality of life, one year after repair of vaginal and abdominal pelvic organ prolapse. It was observed that symptoms improve considerably, women are satisfied about the surgery result and quality of life, and approximately 25% of the interviewed women required additional therapy in the first year after the genital prolapse surgery [19,24]. Overall, there is a real need for studies to evaluate the effectiveness of a rigorous perioperative behavioral therapy program, with training of the pelvic muscles after a transvaginal reconstructive surgery for genital prolapse. However, perioperative muscle therapy performed in addition to vaginal surgery provided no additional improvement in quality of life or sexual function compared with usual procedure [20]. Women from our study did not mention any type of additional therapy for improving the quality or sexual life. The results are native, without any other treatment. We do not exclude this type of the therapy, even for this study group, but further evaluation may be considered in time [23,24,25].
There is a lack of data in literature regarding men’ satisfaction after their partner’s vaginal surgical intervention. Based on our results, the majority of partners of interviewed women described no negative impact on the sexual life caused by vaginal surgery. This subject may be a topic for further research, which should be performed in a large number of patients.
Highlights
- ✓
- The malfunction of the supporting pelvic system generates signs and symptoms that require various surgical procedures.
- ✓
- Vaginal surgical interventions for genital prolapse or urinary incontinence do not lead to significant alteration of quality of sexual life in women.
Conclusions
The patients who underwent a vaginal hysterectomy required longer hospitalization period compared with other vaginal procedures, and their sex life following vaginal surgery to a long time to recover. Vaginal dryness increases after the surgeries even in the premenopausal patients. However, overall, vaginal surgical interventions are not correlated to significant alteration of the quality of sexual life in the short term.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
References
- Herzog, A.R.; Diokno, A.C.; Brown, M.B.; Fultz, N.H.; Goldstein, N.E. Urinary incontinence as a risk factor for mortality. J Am Geriatr Soc. 1994, 42, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Yip, S.K.; Cardozo, L. Psychological morbidity and female urinary incontinence. Best Pract Res Clin Obstet Gynaecol. 2007, 21, 321–329. [Google Scholar] [CrossRef]
- Brown, J.S.; McGhan, W.F.; Chokroverty, S. Comorbidities associated with overactive bladder. Am J Manag Care. 2000, 6 (Suppl. S11), S574–S579. [Google Scholar]
- Ples, L.; Sima, R.M.; Stanescu, A.D.; et al. Transperineal Ultrasound Role for Pelvic Floor Dysfunction Evaluation. Proceeding of the paper for the 13th National Congress of Urogynecology, (UROGYN 2016; 2016; pp. 252–257. [Google Scholar]
- Serati, M.; Salvatore, S.; Uccella, S.; Nappi, R.E.; Bolis, P. Female urinary incontinence during intercourse: A review on an understudied problem for women's sexuality. J Sex Med. 2009, 6, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Motofei, I.G. A dual physiological character for sexual function: The role of serotonergic receptors. BJU Int. 2008, 101, 531–534. [Google Scholar] [CrossRef]
- Schumpf, L.F.; Theill, N.; Scheiner, D.A.; Fink, D.; Riese, F.; Betschart, C. Urinary incontinence and its association with functional physical and cognitive health among female nursing home residents in Switzerland. BMC Geriatr. 2017, 17, 17. [Google Scholar] [CrossRef] [PubMed]
- Elia, G.; Bergman, J.; Dye, T.D. Familial incidence of urinary incontinence. Am J Obstet Gynecol. 2002, 187, 53–55. [Google Scholar] [CrossRef]
- Bălălău, D.O.; Sima, R.M.; Bacalbașa, N.; Banu, P.; Bălălău, C.; Pleș, L.; Stănescu, A.D. High-grade cervical dysplasia in pregnancy–psychological and medical challenges. J Mind Med Sci. 2017, 4, 24–30. [Google Scholar] [CrossRef]
- Wood, L.N.; Anger, J.T. Urinary incontinence in women. BMJ. 2014, 349, g4531. [Google Scholar] [CrossRef]
- Radosa, J.C.; Meyberg-Solomayer, G.; Kastl, C.; et al. Influences of different hysterectomy techniques on patients' postoperative sexual function and quality of life. J Sex Med. 2014, 11, 2342–2350. [Google Scholar] [CrossRef]
- Poenaru, M.O.; Sima, R.M.; Dan, D.; et al. Comparison Between Classical and Protetic Surgical Intervention for Pelvic Floor Dysfunctions and Urinary Stress Incontinence. Proceeding of the paper for the 13th National Congress of Urogynecology. 2016 (UROGYN 2016); pp. 258–261.
- Dhital, R.; Otsuka, K.; Poudel, K.C.; Yasuoka, J.; Dangal, G.; Jimba, M. Improved quality of life after surgery for pelvic organ prolapse in Nepalese women. BMC Womens Health. 2013, 13, 22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Motofei, I.G.; Rowland David LBaconi, D.L.; et al. Therapeutic considerations related to finasteride administration in male androgenic alopecia and benign prostatic hyperplasia. Farmacia. 2017, 65, 660–666. [Google Scholar]
- Lukacz, E.S.; Warren, L.K.; Richter, H.E.; et al. Quality of Life and Sexual Function 2 Years After Vaginal Surgery for Prolapse. Obstet Gynecol. 2016, 127, 1071–1079. [Google Scholar] [CrossRef]
- Schiavi, M.C.; DʼOria, O.; Faiano, P.; et al. Vaginal Native Tissue Repair for Posterior Compartment Prolapse: Long-Term Analysis of Sexual Function and Quality of Life in 151 Patients. Female Pelvic Med Reconstr Surg. 2018, 24, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Schiavi, M.C.; Savone, D.; Di Mascio, D.; et al. Long-term experience of vaginal vault prolapse prevention at hysterectomy time by modified McCall culdoplasty or Shull suspension: Clinical, sexual and quality of life assessment after surgical intervention. Eur J Obstet Gynecol Reprod Biol. 2018, 223, 113–118. [Google Scholar] [CrossRef]
- Dimcevici Poesina, N.; Bălălău, C.; Bârcă, M.; et al. Testicular histopathological changes following sodium fluoride administration in mice. Rom J Morphol Embryol. 2013, 54, 1019–1024. [Google Scholar] [PubMed]
- Rahkola-Soisalo, P.; Altman, D.; Falconer, C.; Morcos, E.; Rudnicki, M.; Mikkola, T.S. Quality of life after Uphold™ Vaginal Support System surgery for apical pelvic organ prolapse-A prospective multicenter study. Eur J Obstet Gynecol Reprod Biol. 2017, 8, 86–90. [Google Scholar] [CrossRef]
- Motofei, I.G.; Rowland, D.L.; Popa, F.; et al. A Pilot Study on Tamoxifen Sexual Side Effects and Hand Preference in Male Breast Cancer. Arch Sex Behav. 2015, 44, 1589–1594. [Google Scholar] [CrossRef]
- Kowalik, C.R.; Lakeman, M.M.E.; de Kraker, A.T.; Roovers, J.P.W.R. Effects of mesh-related complications in vaginal surgery on quality of life. Int Urogynecol J. 2019, 30, 1083–1089. [Google Scholar] [CrossRef]
- Hokenstad, E.D.; El-Nashar, S.A.; Blandon, R.E.; et al. Health-related quality of life and outcomes after surgical treatment of complications from vaginally placed mesh. Female Pelvic Med Reconstr Surg. 2015, 21, 176–180. [Google Scholar] [CrossRef]
- Petcharopas, A.; Wongtra-Ngan, S.; Chinthakanan, O. Quality of life following vaginal reconstructive versus obliterative surgery for treating advanced pelvic organ prolapse. Int Urogynecol J. 2018, 29, 1141–1146. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.N.; Gruner, M.; Killinger, K.A.; et al. Additional treatments, satisfaction, symptoms and quality of life in women 1 year after vaginal and abdominal pelvic organ prolapse repair. Int Urol Nephrol. 2018, 50, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Weidner, A.C.; Barber, M.D.; Markland, A.; et al. Perioperative Behavioral Therapy and Pelvic Muscle Strengthening Do Not Enhance Quality of Life After Pelvic Surgery: Secondary Report of a Randomized Controlled Trial. Phys Ther. 2017, 97, 1075–1083. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the author. 2020 Maria Pană, Romina-Marina Sima, Oana-Denisa Bălălău, Anca-Daniela Stănescu, Liana Pleş, Mircea-Octavian Poenaru