Hepatocarcinoma with Tumor Thrombus Occupying the Right Atrium and Portal Vein in a Patient with Hereditary Hemochromatosis and Liver Cirrhosis
Highlights
- Hepatocellular carcinoma with right atrium invasion is a rare condition, especially in hereditary hemochromatosis.
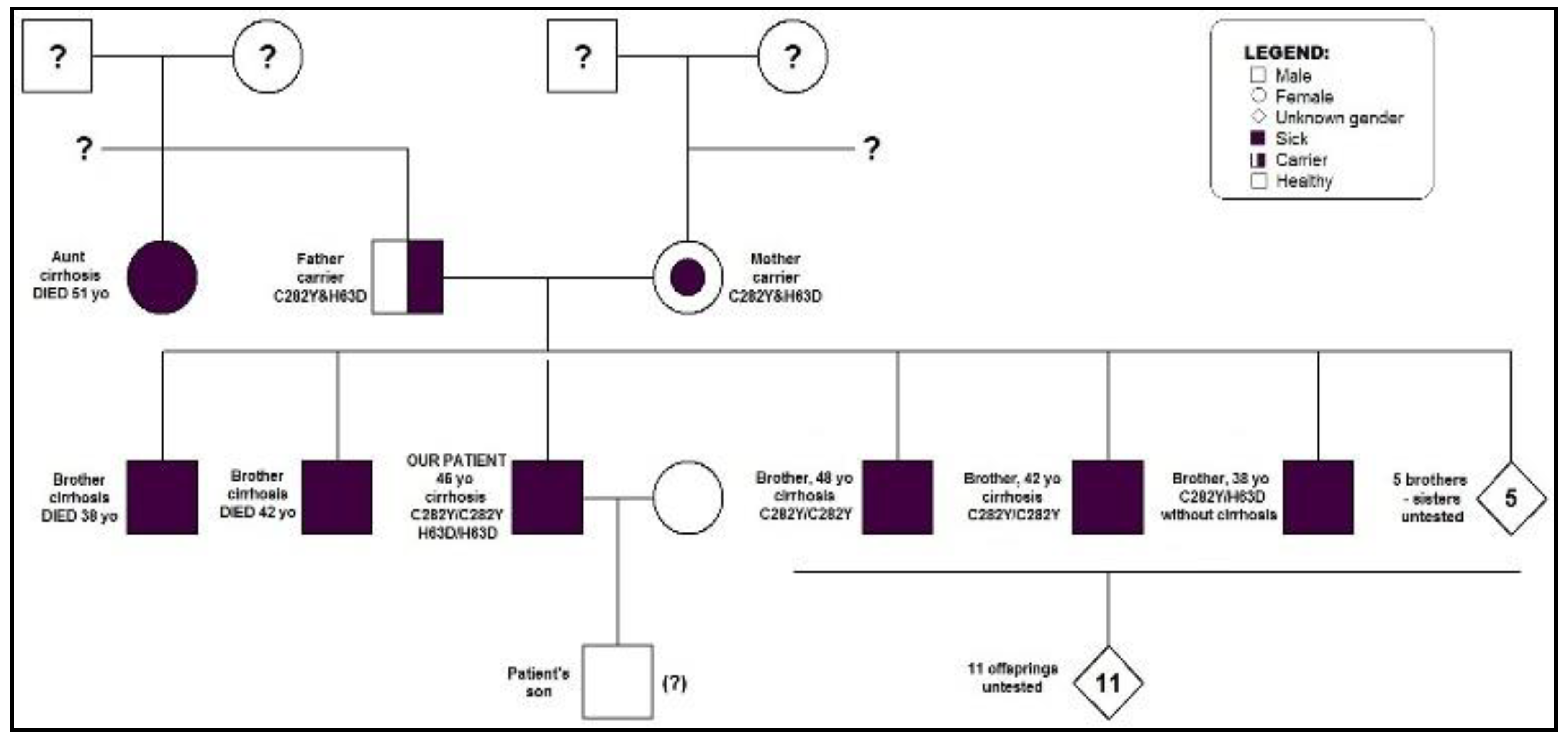
- All first-degree relatives of a patient diagnosed with type 1 hereditary hemochromatosis should be genetically tested for HFE mutations and monitored in order to prevent iron overload.
Highlights
- Hepatocellular carcinoma with right atrium invasion is a rare condition, especially in hereditary hemochromatosis.
- All first-degree relatives of a patient diagnosed with type 1 hereditary hemochromatosis should be genetically tested for HFE mutations and monitored in order to prevent iron overload.
Abstract
Introduction
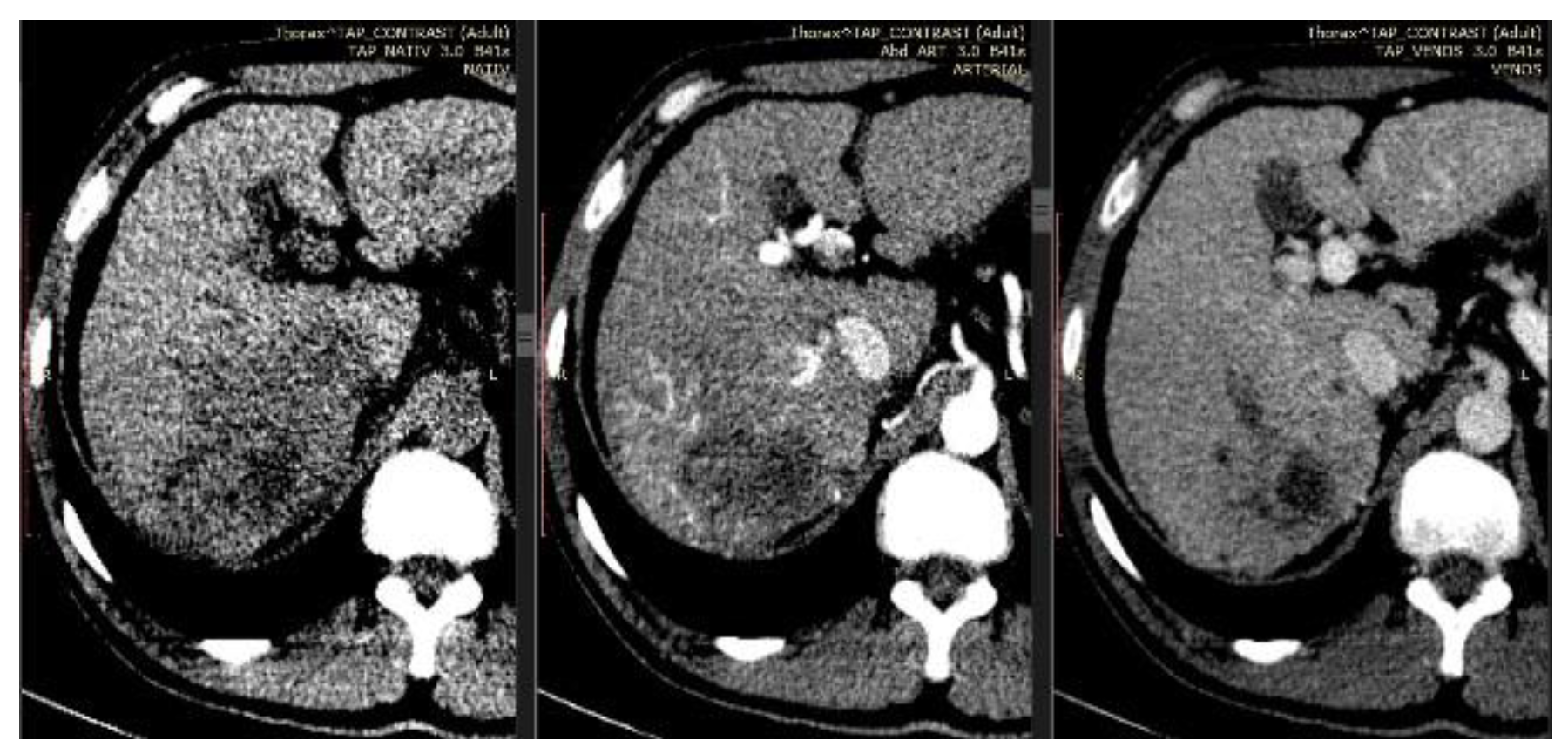
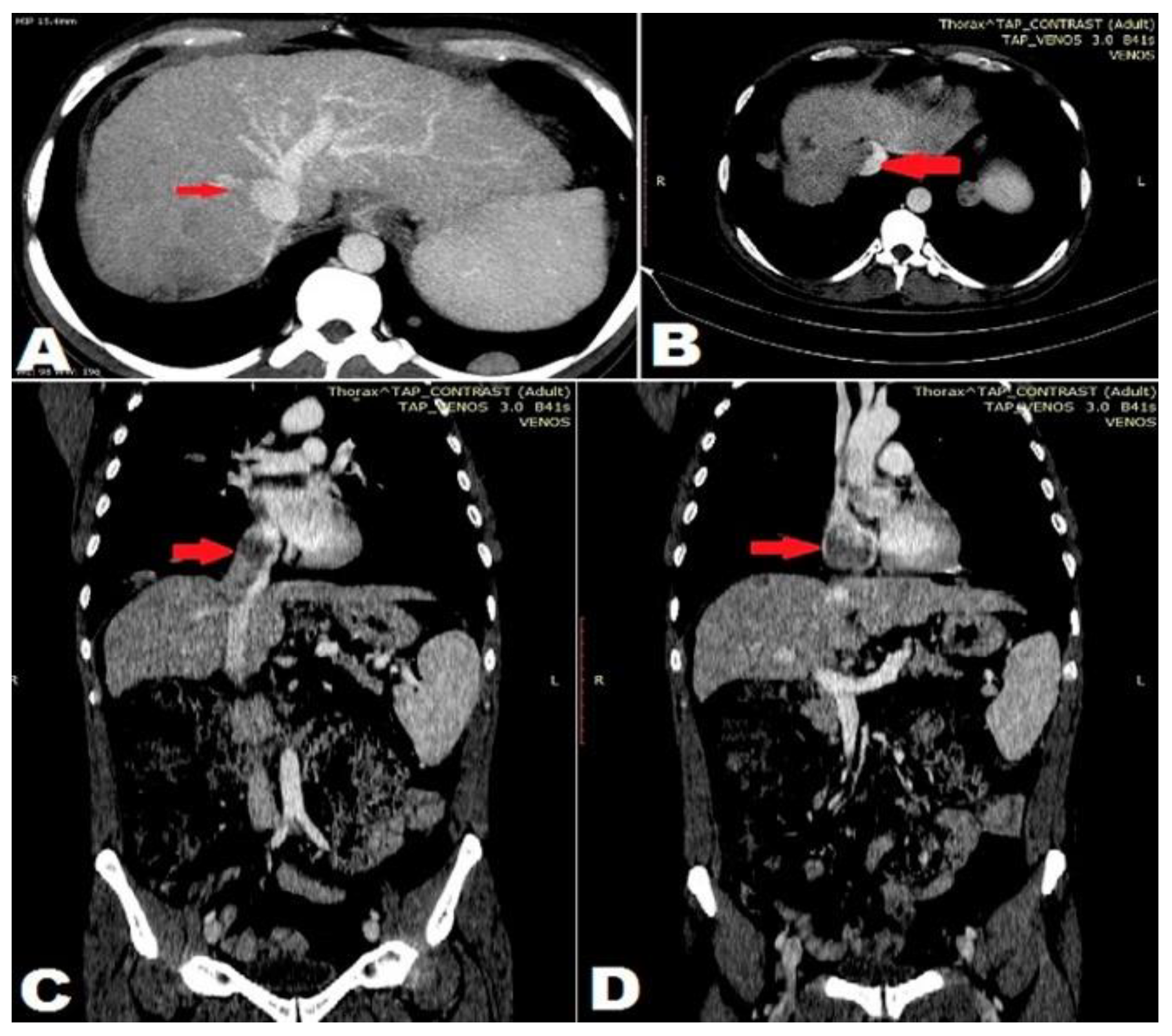
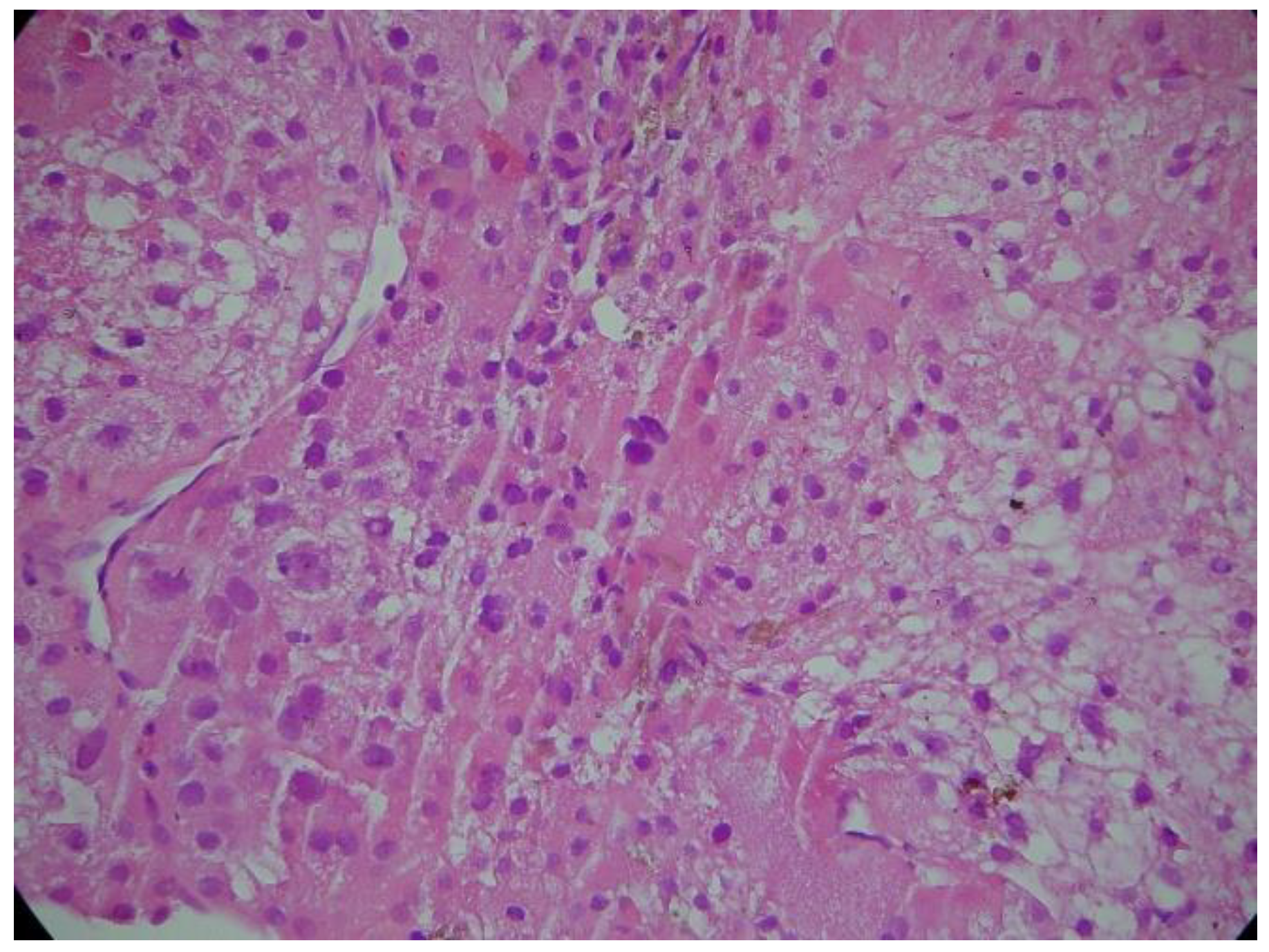
Case report
Discussion
Conclusions
References
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef] [PubMed]
- Okuda, K. Hepatocellular carcinoma: clinicopathological aspects. J Gastroenterol Hepatol. 1997, 12, S314–318. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Zhang, B.; Dong, S.; Zhang, B.; Chen, X. Hepatocellular carcinoma with tumor thrombus occupying the right atrium and portal vein. A case report and literature review. Medicine. 2015, 94, e1049. [Google Scholar] [CrossRef] [PubMed]
- Balaceanu, A.; Diaconu, C.; Aron, G. Budd-Chiari syndrome as an initial presentation of hepatocellular carcinoma – a case report. Med Ultrason. 2014, 16, 172–174. [Google Scholar] [CrossRef] [PubMed]
- Beutler, E.; Gelbart, T.; West, C.; Lee, P.; Adams, M.; Blackstone, R.; Pockros, P.; Kosty, M.; Venditti, C.P.; Phatak, P.D.; Seese, N.K.; Chorney, K.A.; Ten Elshof, A.E.; Gerhard, G.S.; Chorney, M. Mutation analysis in hereditary hemochromatosis. Blood Cells Mol Dis. 1996, 22, 187–94. [Google Scholar] [CrossRef] [PubMed]
- Elmberg, M.; Hultcrantz, R.; Ekbom, A.; Brandt, L.; Olsson, S.; Olsson, R.; Lindgren, S.; Lööf, L.; Stål, P.; Wallerstedt, S.; Almer, S.; Sandberg-Gertzén, H.; Askling, J. Cancer risk in patients with hereditary hemochromatosis and in their first-degree relatives. Gastroenterology. 2003, 125, 1733–41. [Google Scholar] [CrossRef] [PubMed]
- Fracanzani, A.L.; Conte, D.; Fraquelli, M.; Taioli, E.; Mattioli, M.; Losco, A.; Fargion, S. Increased cancer risk in a cohort of 230 patients with hereditary hemochromatosis in comparison to matched control patients with non-iron-related chronic liver disease. Hepatology. 2001, 33, 647–51. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.; Qian, B.X.; Yin, W.L.; Wang, F.M.; Han, T. Association between the HFE C282Y, H63D polymorphisms and the risks of non-alcoholic fatty liver disease, liver cirrhosis and hepatocellular carcinoma: an updated systematic review and meta- analysis of 5,758 cases and 14,741 controls. PLOS One. 2016, 11, e0163423. [Google Scholar] [CrossRef] [PubMed]
- Diaconu, C.; Bălăceanu, A.; Moroşan, E. Sepsis biomarkers: past, present and future. Farmacia 2015, 63, 811–815. [Google Scholar]
- Wang, Y.; Yuan, L.; Ge, R.L.; Sun, Y.; Wei, G. Survival benefit of surgical treatment for hepatocellular carcinoma with inferior vena cava/right atrium tumor thrombus: results of a retrospective cohort study. Ann Surg Oncol. 2013, 20, 914–22. [Google Scholar] [CrossRef] [PubMed]


© 2018 by the author. 2018 Olga Hilda Orasan, Andreea Maria Stefan, Laura Urian, Anca Mihailov, Ovidiu Fabian, Flaviu Muresan, Iulia Breaban, Sorina Cezara Secara, Simina Tarmure Sarlea, Vasile Negrean, Dorel Sampelean, Angela Cozma
Share and Cite
Orasan, O.H.; Stefan, A.M.; Urian, L.; Mihailov, A.; Fabian, O.; Muresan, F.; Breaban, I.; Secara, S.C.; Tarmure Sarlea, S.; Negrean, V.; et al. Hepatocarcinoma with Tumor Thrombus Occupying the Right Atrium and Portal Vein in a Patient with Hereditary Hemochromatosis and Liver Cirrhosis. J. Mind Med. Sci. 2018, 5, 300-304. https://doi.org/10.22543/7674.52.P300304
Orasan OH, Stefan AM, Urian L, Mihailov A, Fabian O, Muresan F, Breaban I, Secara SC, Tarmure Sarlea S, Negrean V, et al. Hepatocarcinoma with Tumor Thrombus Occupying the Right Atrium and Portal Vein in a Patient with Hereditary Hemochromatosis and Liver Cirrhosis. Journal of Mind and Medical Sciences. 2018; 5(2):300-304. https://doi.org/10.22543/7674.52.P300304
Chicago/Turabian StyleOrasan, Olga Hilda, Andreea Maria Stefan, Laura Urian, Anca Mihailov, Ovidiu Fabian, Flaviu Muresan, Iulia Breaban, Sorina Cezara Secara, Simina Tarmure Sarlea, Vasile Negrean, and et al. 2018. "Hepatocarcinoma with Tumor Thrombus Occupying the Right Atrium and Portal Vein in a Patient with Hereditary Hemochromatosis and Liver Cirrhosis" Journal of Mind and Medical Sciences 5, no. 2: 300-304. https://doi.org/10.22543/7674.52.P300304
APA StyleOrasan, O. H., Stefan, A. M., Urian, L., Mihailov, A., Fabian, O., Muresan, F., Breaban, I., Secara, S. C., Tarmure Sarlea, S., Negrean, V., Sampelean, D., & Cozma, A. (2018). Hepatocarcinoma with Tumor Thrombus Occupying the Right Atrium and Portal Vein in a Patient with Hereditary Hemochromatosis and Liver Cirrhosis. Journal of Mind and Medical Sciences, 5(2), 300-304. https://doi.org/10.22543/7674.52.P300304


