Functional Radical Cervical Dissection for Differentiated Thyroid Cancer: The Experience of a Single Center
Highlights
- Central and lateral neck dissections/ CLND is a feasible option for differentiated thyroid cancers, with a low complication rate.
- Berry picking of the enlarged lymph nodes should be avoided, due to the fact that the complication rate is similar to CLND and the recurrence rate of malignancy is higher.
Highlights
- Central and lateral neck dissections/ CLND is a feasible option for differentiated thyroid cancers, with a low complication rate.
- Berry picking of the enlarged lymph nodes should be avoided, due to the fact that the complication rate is similar to CLND and the recurrence rate of malignancy is higher.
Abstract
Introduction
Materials and Methods
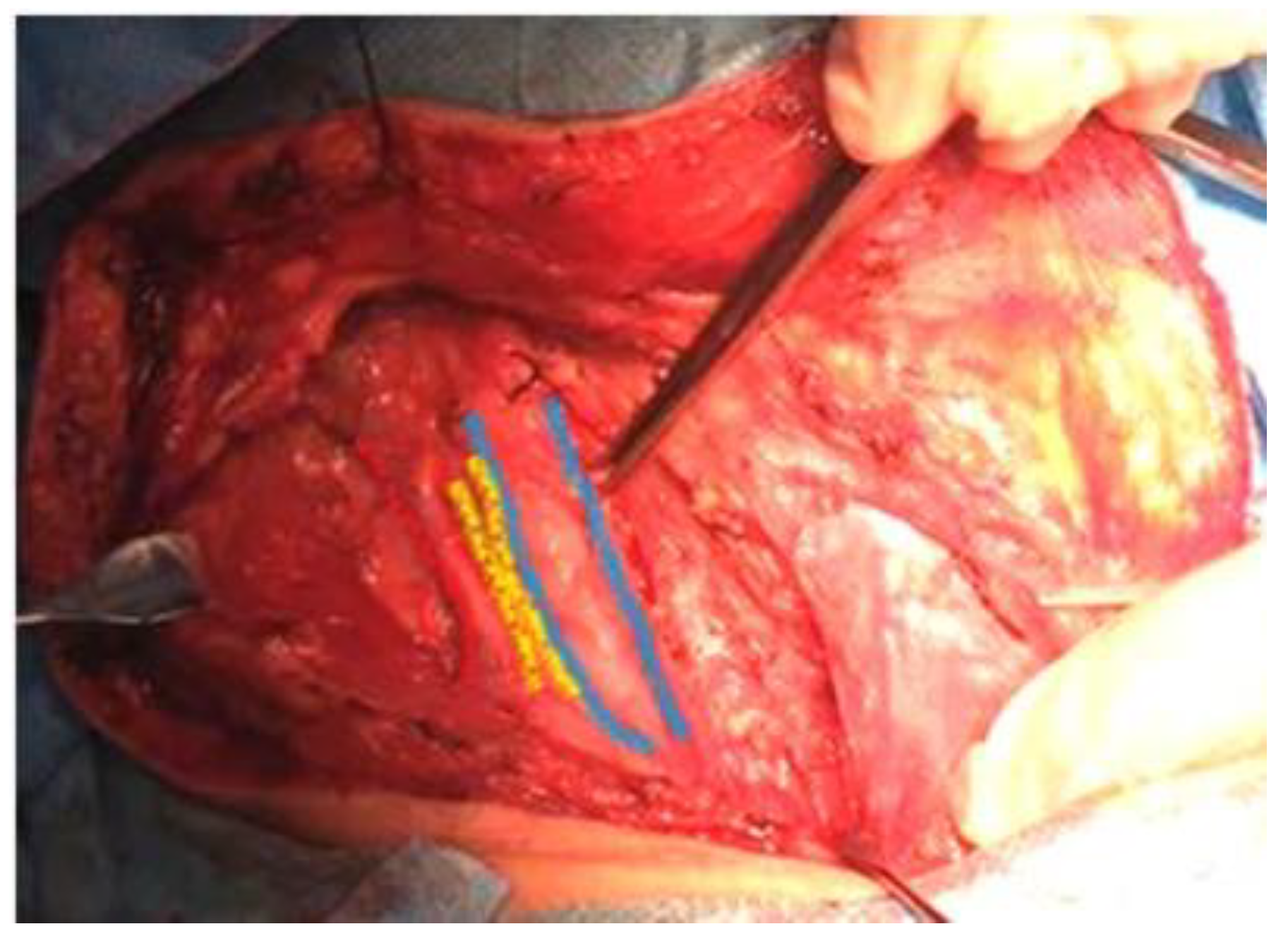
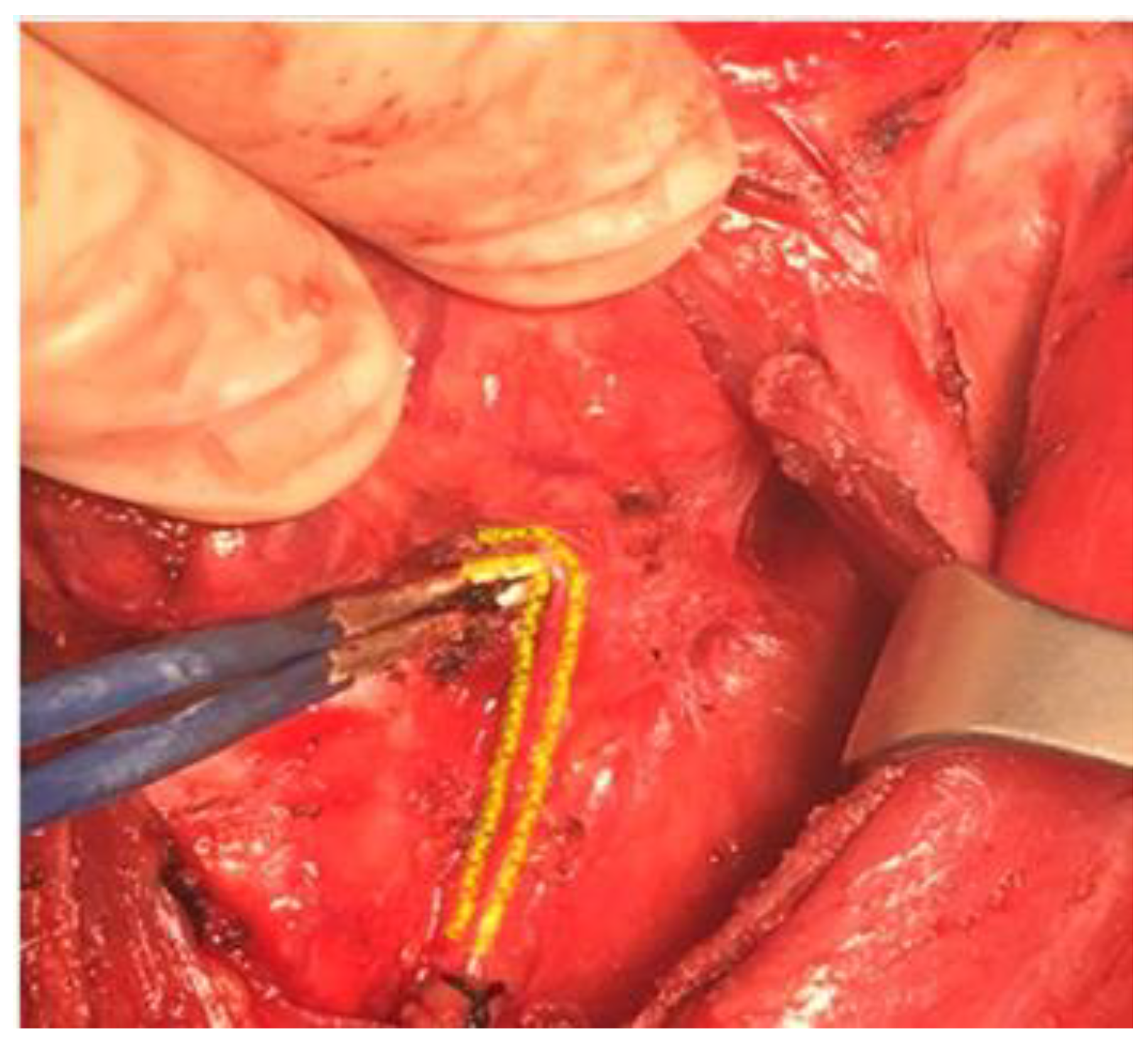
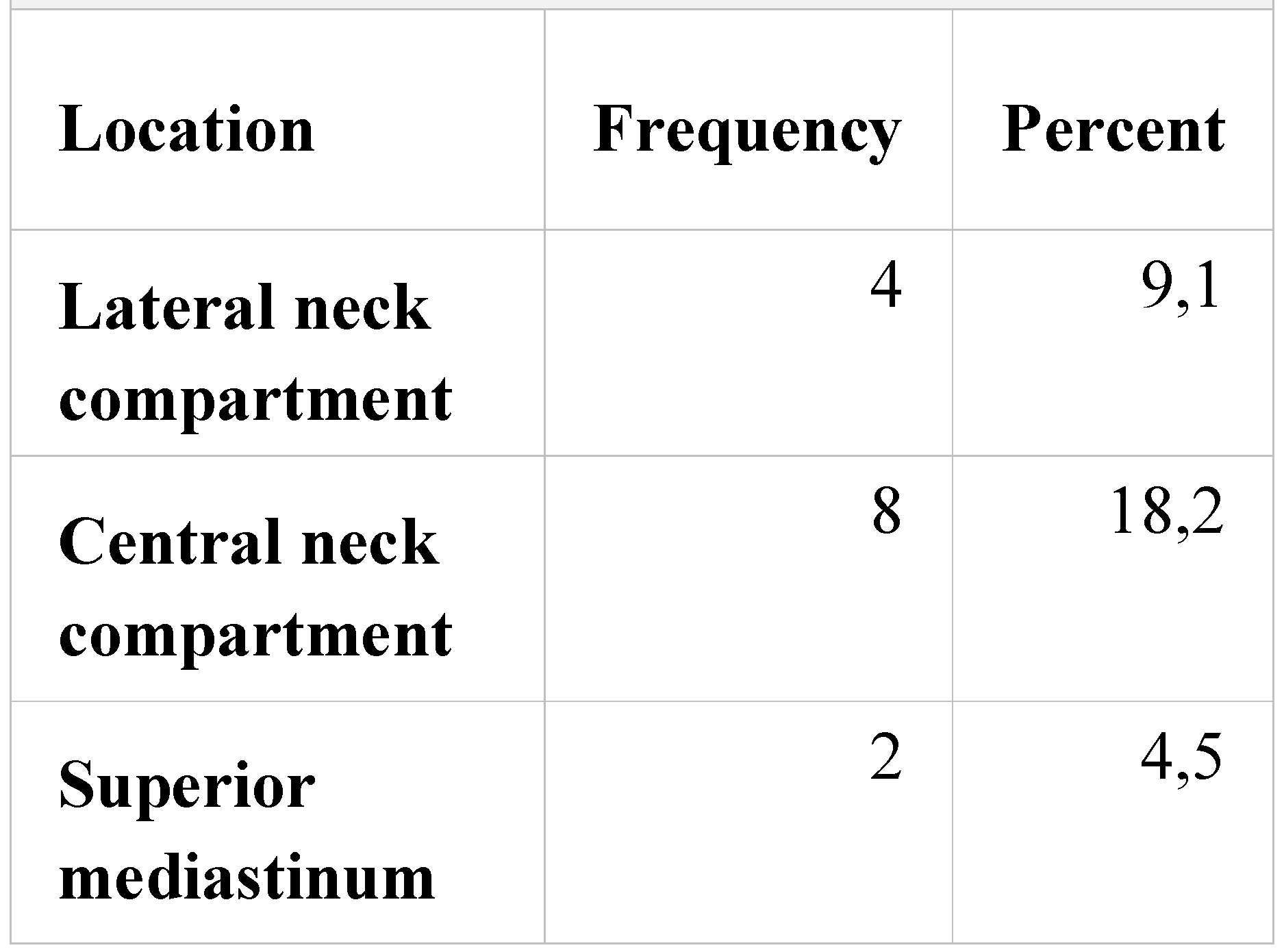
Results
 |
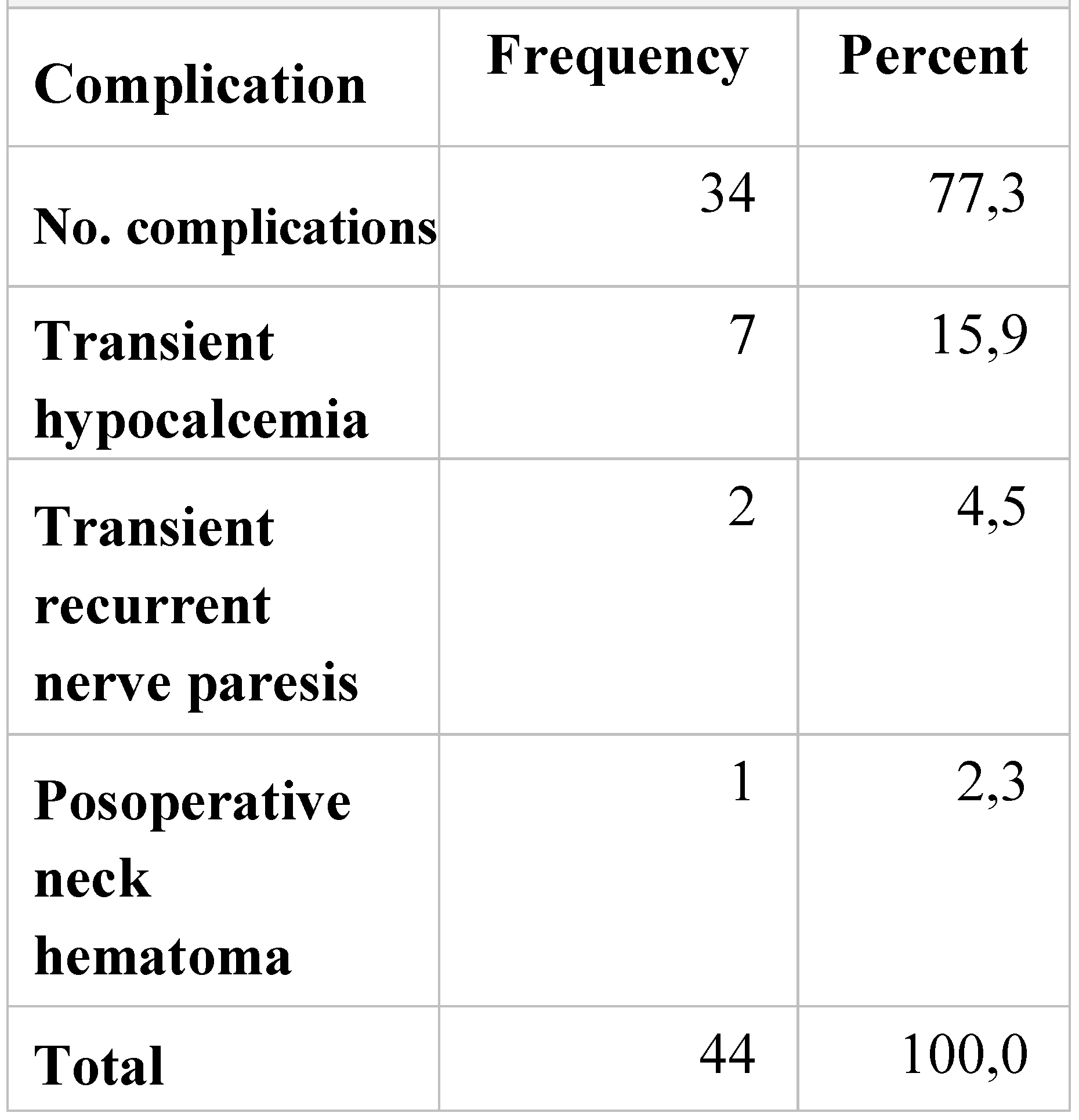 |
Discussions
Conclusions
Acknowledgments
Conflicts of Interest
References
- Kumar, V.; Abbas, A.K.; Astar, J.C. Robbins and Cotran Pathologic Basis of Disease, 9th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2014. [Google Scholar]
- Hundahl, S.A.; Fleming, I.D.; Fremgen, A.M.; et al. A national cancer data base report on 53,856 cases of thyroid carcinoma treated in the US, 1985-1995. Cancer 1998, 83, 2638–2648. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.Y.; Jemal, A.; Ward, E.M. Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer 2009, 115, 3801–3807. [Google Scholar] [CrossRef] [PubMed]
- Mirallie, E.; Visset, J.; Sagan, C.; Hamy, A.; Le Bodic, M.F.; Paineau, J. Localization of cervical node metastasis of papillary thyroid carcinoma. World J Surg. 1999, 23, 970–973. [Google Scholar] [CrossRef] [PubMed]
- McConahey, W.M.; Hay, I.D.; Woolner, L.B.; et al. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: Initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986, 61, 978–996. [Google Scholar] [CrossRef]
- Qubain, S.W.; Nakano, S.; Baba, M.; Takao, S.; Aikou, T. Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery. 2002, 131, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Tomoda, C.; Uruno, T.; et al. Preoperative ultrasonographic examination for lymph node metastases: Usefulness when designing lymph node dissection for papillary micro carcinoma of the thyroid. World J Surg. 2004, 28, 498–501. [Google Scholar] [CrossRef]
- Tisell, L.E.; Nilsson, B.; Molne, J.; et al. Improved survival of patients with papillary thyroid cancer after surgical microdissection. World J Surg. 1996, 20, 854–859. [Google Scholar] [CrossRef]
- Cooper, D.S.; Doherty, G.M.; Haugen, B.R.; Kloos, R.T.; Lee, S.L.; Mandel, S.J.; Mazzaferri, E.L.; McIver, B.; Sherman, S.I.; Tuttle, R.M.; American Thyroid Association Guidelines Taskforce. American Thyroid Association Guidelines Taskforce. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006, 16, 109–142. [Google Scholar] [CrossRef] [PubMed]
- Carty, S.E.; Cooper, D.S.; Doherty, G.M.; et al. American Thyroid Association Surgery Working Group; American Association of Endocrine Surgeons; American Academy of Otolaryngology-Head and Neck Surgery; American Head and Neck Society, Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 2009, 19, 1153–1158. [Google Scholar] [CrossRef]
- Cheah, W.K.; Arici, C.; Ituarte, P.H.; Siperstein, A.E.; Duh, Q.Y.; Clark, O.H. Complications of neck dissection for thyroid cancer. World J Surg. 2002, 26, 1013–1016. [Google Scholar] [CrossRef]
- Robbins, K.T.; Clayman, G.; Levine, P.A.; Medina, J.; Sessions, R.; Shaha, A.; Som, P.; Wolf, G.T.; American Head and Neck Society; American Academy of Otolaryngology-Head and Neck Surgery. Neck dissection classification update: Revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology. Arch Otolaryngol Head Neck Surg. 2002, 128, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Raffaelli, M.; De Crea, C.; Sessa, L.; Giustacchini, P.; Revelli, L.; Bellantone, C.; Lombardi, C.P. Prospective evaluation of total thyroidectomy versus ipsilateral versus bilateral central neck dissection in patients with clinically node-negative papillary thyroid carcinoma. Surgery. 2012, 152, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Hughes, D.T.; Doherty, G.M. Central neck dissection for papillary thyroid cancer. Cancer Control. 2011, 18, 83–88. [Google Scholar] [CrossRef]
- Giugliano, G.; Proh, M.; Gibelli, B.; Grosso, E.; Tagliabue, M.; De Fiori, E.; Maffini, F.; Chiesa, F.; Ansarin, M. Central neck dissection in differentiated thyroid cancer: Technical notes. Acta Otorhinolaryngol Ital. 2014, 34, 9–14. [Google Scholar] [PubMed]
- Raffaelli, M.; De Crea, C.; Sessa, L.; Giustacchini, P.; Bellantone, R.; Lombardi, C.P. Can intraoperative frozen section influence the extension of central neck dissection in cN0 papillary thyroid carcinoma? Langenbecks Arch Surg. 2013, 398, 383–388. [Google Scholar] [CrossRef]
- Raina, S.; Rocko, J.M.; Swaminathan, A.P.; Brief, D.K.; Lazaro, E.J. Current attitudes in the management of thyroid cancer. Am Surg. 1983, 49, 110–112. [Google Scholar]
- Nicolosi, A.; Malloci, A.; Esu, S.; Addis, E.; Tarquini, A. The role of node-picking lymphadenectomy in the treatment of differentiated carcinoma of the thyroid. Minerva Chir. 1993, 48, 459–463. [Google Scholar] [PubMed]
- Munacchio, M.J.; Kim, A.W.; Vijungco, J.D.; Prinz, R.A. Greater local recurrence occurs with “berry picking” than neck dissection in thyroid cancer. Am Surg. 2003, 69, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Zarnegar, R.; Brunaud, L.; Clark, O.H. Prevention, evaluation, and management of complications following thyroidectomy for thyroid carcinoma. Endocrinol Metab Clin North Am. 2003, 32, 483–502. [Google Scholar] [CrossRef] [PubMed]
- Wei, T.; Li, Z.; Jin, J.; Chen, R.; Gong, Y.; Du, Z.; Gong, R.; Zhu, J. Autotransplantation of inferior parathyroid glands during central neck dissection for papillary thyroid carcinoma: A retrospective cohort study. Int J Surg. 2014, 12, 1286–1290. [Google Scholar] [CrossRef]
- Hermann, M.; Hellebart, C.; Freissmuth, M. Neuromonitoring in Thyroid Surgery. Prospective Evaluation of Intraoperative Electrophysiological Responses for the Prediction of Recurrent Laryngeal Nerve Injury. Ann Surg. 2004, 240, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Paunica, M.; Manole, A.; Motofei, C.; Tanase, G.L. The Globalization in the actual Context of the European Union Economy. Proceedings of the international conference on business excellence. 2018, 12, 739–750. [Google Scholar] [CrossRef]
- van Wilgen, C.P.; Dijkstra, P.U.; van der Laan, B.F.; et al. Shoulder and neck morbidity in quality of life after surgery for head and neck cancer. Head Neck. 2004, 26, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, S.; Rodriguez, J.M.; Soria, T.; et al. Extrathyroid spread in papillary carcinoma of the thyroid: Clinicopathological and prognostic study. Otolaryngol Head Neck Surg. 2001, 124, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Gimm, O.; Rath, F.W.; Dralle, H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg. 1998, 85, 252–254. [Google Scholar] [CrossRef]
- Ciuhu, A.N.; Rahnea Niţă, R.A.; Popescu, M.; Dumitru Badiu, C.D.; Pantea Stoian, A.M.; Lupuliasa, D.; Gherghiceanu, F.; Diaconu, C.C.; Rahnea Niţă, G. Evidence of strong opioid therapy for palliation of breathlesness in cancer patients. Farmacia. 2017, 65, 173–178. [Google Scholar]
- Roh, J.L.; Park, J.Y.; Park, C.I. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: Pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg. 2007, 245, 604–610. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the author. 2018 Adrian Tulin, Lucian Alecu, Catalina Poiana, Luminita Tomescu, Iulian Slavu, Raluca Tulin, Silviu Pituru, Radu Jecan, Cristian Balalau, Anca Pantea Stoian, Razvan Hainarosie, Cornelia Nitipir
Share and Cite
Tulin, A.; Alecu, L.; Poiana, C.; Tomescu, L.; Slavu, I.; Tulin, R.; Pituru, S.; Orlov, C.; Jecan, R.; Balalau, C.; et al. Functional Radical Cervical Dissection for Differentiated Thyroid Cancer: The Experience of a Single Center. J. Mind Med. Sci. 2018, 5, 278-283. https://doi.org/10.22543/7674.52.P278283
Tulin A, Alecu L, Poiana C, Tomescu L, Slavu I, Tulin R, Pituru S, Orlov C, Jecan R, Balalau C, et al. Functional Radical Cervical Dissection for Differentiated Thyroid Cancer: The Experience of a Single Center. Journal of Mind and Medical Sciences. 2018; 5(2):278-283. https://doi.org/10.22543/7674.52.P278283
Chicago/Turabian StyleTulin, Adrian, Lucian Alecu, Catalina Poiana, Luminita Tomescu, Iulian Slavu, Raluca Tulin, Silviu Pituru, Cristina Orlov, Radu Jecan, Cristian Balalau, and et al. 2018. "Functional Radical Cervical Dissection for Differentiated Thyroid Cancer: The Experience of a Single Center" Journal of Mind and Medical Sciences 5, no. 2: 278-283. https://doi.org/10.22543/7674.52.P278283
APA StyleTulin, A., Alecu, L., Poiana, C., Tomescu, L., Slavu, I., Tulin, R., Pituru, S., Orlov, C., Jecan, R., Balalau, C., Stoian, A. P., Hainarosie, R., & Nitipir, C. (2018). Functional Radical Cervical Dissection for Differentiated Thyroid Cancer: The Experience of a Single Center. Journal of Mind and Medical Sciences, 5(2), 278-283. https://doi.org/10.22543/7674.52.P278283



