The Switch from Patented Medicine to the Generic One: An Option or a Necessity?
Highlights
- This paper concludes that the switch between original medication with a generic one is rather a necessity than an option.
- The pharmaceutical market is currently confronted with some deficiencies related to information and/ or collaboration between physicians, pharmacists and patients.
Abstract
Highlights
- ✓ This paper concludes that the switch between original medication with a generic one is rather a necessity than an option.
- ✓ The pharmaceutical market is currently confronted with some deficiencies related to information and/ or collaboration between physicians, pharmacists and patients.
Introduction
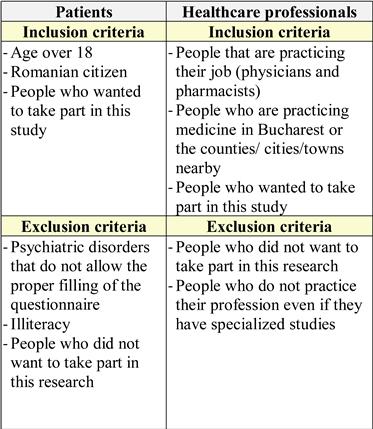
Materials and Methods
- The difference between original and generic drug (if they did not know, they were informed when given the questionnaire).
- The observed differences in health status after switching from the original drug to the generic one.
- The effective use of generic drugs in their treatment.
- The primary source of information to be taken into account when purchasing medication.
- The importance of medical advice when buying medicine.
- The influence of the drug’s cost when choosing between an original and generic medication.
- The problem of failing to purchase a specific drug that the patient is using in their treatment.
- Whether the switch from the original prescription to the generic one is based on the recommendation of the specialists or on other sources of information.
- The differences between an original drug and a generic one.
- The therapeutic efficacy and incidence of adverse reactions of the original vs. generic drug.
- The safety profile of a generic drug.
- The previous medicines given to their patients and their efficacy.
- The financial situation of the patient and guidance to use generic drugs.
- The relationship with the medical representative and its influence when choosing to prescribe a certain medication.
- The cooperation with the pharmacist when specifying or switching from the original drug to the generic one and their knowledge about the lack of medicines in the market.
- The previous experience concerning patient attitudes regarding the use of the generic drug.
- The differences between an original drug and a generic one.
- The therapeutic efficacy and incidence of adverse reactions of the original vs. generic drug.
- Previous experience concerning the patient's preferences regarding the use of an original vs. generic drug.
- The importance of the physician's recommendation when dispensing the medical prescription and the previous treatment received by the patient and its efficacy.
- The influence of the patient's financial situation when administering the original medicine and their counseling on alternatives to original medicines.
- The relationship between the medical representative and the pharmacy’s financial profit, and influence of these factors on drug release.
- The lack of original drugs in the pharmaceutical market, the impact of this lack, and how the relationship between the pharmacist and the patient is affected.
Results
The quantitative analysis of the answers given by the evaluated people
Discussions
Comparative analysis of the responses across the three groups
Conclusions
Conflicts of Interest
References
- Iorga, M.; Sztankovszky, L.Z.; Soponaru, C.; Gardikiotis, I. Pharmacists’ attitude and practices about drug dispensing in Romania. Farmacia. 2015, 63, 601–6. [Google Scholar]
- Lloyd, C.E.; Brown, F.J. Depression and diabetes. Curr Womens Health Rep. 2002, 2, 188–93. [Google Scholar] [PubMed]
- Maftei Aron, N.; Boev, M.; Bahrim, G. Probiotics and therapeutic effect in clinical practice – Review. Romanian Biotechnological Letters. 2015, 20, 10162–75. [Google Scholar]
- Thakkar, K.; Billa, G. The concept of Generic drugs and patented drugs vs brand name drugs and non-proprietary (generic) name drugs. Front Pharmacol. 2013, 4, 113. [Google Scholar] [CrossRef] [PubMed]
- Davit, B.M.; Nwakama, P.E.; Buehler, G.J.; Conner, D.P.; Haidar, S.H.; Patel, D.T.; Yang, Y.; Yu, L.X.; Woodcock, J. Comparing generic and innovator drugs: a review of 12 years of bioequivalence data from the United States Food and Drug Administration. Ann Pharmacother. 2009, 43, 1583–97. [Google Scholar] [CrossRef] [PubMed]
- Kesselheim, A.S.; Misono, A.S.; Lee, J.L.; Stedman, M.R.; Brookhart, M.A.; Choudhry, N.K.; Shrank, W.H. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008, 300, 2514–26. [Google Scholar] [CrossRef] [PubMed]
- Perry, C. Conflicts of interest and the physician's duty to inform. Am J Med. 1994, 96, 375–80. [Google Scholar] [PubMed]
- Rosner, F. Pharmaceutical industry support for continuing medical education programs: a review of current ethical guidelines. Mt Sinai J Med. 1995, 62, 427–30. [Google Scholar] [PubMed]
- Crisan, O.; Iacob, S. Patients’ rights in pharmacy legislation. Farmacia. 2014, 62, 444–450. [Google Scholar]
- Ciuhu, A.N.; Rahnea-Nita, A.; Popescu, M.; Badiu, C.D.; Pantea Stoian, A.; Lupuliasa, D.; Gherghiceanu, F.; Diaconu, C.C.; Rahnea-Nita, G. Evidence of strong opioid therapy for palliation of breathlessness in cancer patients. Farmacia. 2017, 65, 173–178. [Google Scholar]
- Georgescu, S.R.; Tampa, M.; Paunica, S.; Balalau, C.; Constantin, V.; Paunica, G.; Motofei, I. Distribution of post-finasteride syndrome in men with androgenic alopecia. J Investig Dermatol. 2015, 135, S40–S40. [Google Scholar]
- Pantea Stoian, A.; Pituru, S.M.; Hainarosie, R.; Andronache, L.F.; Ginghina, O.; Serafinceanu, C. Testosterone therapy, new opportunities in diabetes mellitus. Farmacia. 2018, 66, 1–7. [Google Scholar]
- Nitipir, C.; Barbu, M.A.; Orlov, C.; Stanciu, A.E.; Popa, A.M.; Hainarosie, R.; Pituru, S.; Arsene, A.L.; Pantea Stoian, A. Type II Diabetes Mellitus - Associated Risk Factor in the Onset and Evolution of Digestive Tract Carcinoma. Romanian Biotechnological Letters 2018, 10. [Google Scholar] [CrossRef]
- Rowland, D.L.; Motofei, I.G.; Popa, F.; Constantin, V.D.; Vasilache, A.; Păunică, I.; Bălălău, C.; Păunică, G.P.; Banu, P.; Păunică, S. The postfinasteride syndrome; an overview. J Mind Med Sci. 2016, 3, 99–107. [Google Scholar]
- Niculescu, D.A.; Dusceac, R.; Galoiu, S.A.; Capatina, C.A.M.; Poiana, C. Serial changes of liver function tests before and during methimazole treatment in thyrotoxic patients. Endocrine Practice. 2016, 22, 974–9. [Google Scholar] [CrossRef] [PubMed]
- Vlasceanu, A.M.; Baconi, D.L.; Galateanu, B.; Stan, M.; Balalau, C. Comparative cytotoxicity study of nicotine and cotinine on MRC-5 cell line. J Mind Med Sci. 2018, 5, 117–122. [Google Scholar] [CrossRef]
- Niculescu, D.A.; Baciu, I.F.; Capatina, C.; Galoiu, S.A.; Gheorghiu, M.L.; Radian STrifanescu, R.A.; Caragheorgheopol, A.; Coculescu, M.; Poiana, C. Acromegaly treatment in Romania. How close are we to disease control? Endokrynol Pol. 2017, 68, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Timofte, D.; Ciuntu, B.; Bulgaru, I.D.; Hainarosie, R.; Pantea Stoian, A.; Mocanu, V. Laparoscopic Sleeve Gastrectomy is associated with Reduced Depressive Symptoms: a One-Year Follow-Up Study. Revista de Cercetare si Interventie Sociala. 2018, 61, 147–154. [Google Scholar]
- Tuchila, C.; Baconi, D.L.; Pirvu, C.D.; Balalau, D.O.; Vlasceanu, A.M.; Stan, M.; Balalau, C. Therapeutic drug monitoring and methods of quantitation for carbamazepine. J Mind Med Sci. 2017, 4, 100–114. [Google Scholar] [CrossRef]
- Ştef, D.S.; Gergen, I.; Traşcă, T.I.; Rivis, A.; Ştef, L.; Romeo, C.; Druga, M.; Pet, I. Assessing the influence of various factors on antioxidant activity of medicinal herbs. Romanian Biotechnological Letters. 2017, 22, 12842–6. [Google Scholar]
- Trofin, F.; Ciobica, A.; Honceriu, C.; Cojocaru, S.I.; Stoica, B.; Cojocaru, D.; Ciornea, E.; Timofte, D. Modulatory effects of vitamin C on the relation between physical exercising and oxidative stress at young smokers. Romanian Biotechnological Letters. 2017, 22, 12439–47. [Google Scholar]
© 2008 by the author. 2008 Dan Nicolae Păduraru, Daniel Ion, Adriana Elena Nica, Florentina Coman, Marius Coțofană, Dumitru Cristinel Badiu, Valentin Titus Grigorean, Alexandra Bolocan and Octavian Andronic
Share and Cite
Păduraru, D.N.; Ion, D.; Nica, A.E.; Coman, F.; Coțofană, M.; Badiu, D.C.; Grigorean, V.T.; Bolocan, A.; Andronic, O. The Switch from Patented Medicine to the Generic One: An Option or a Necessity? J. Mind Med. Sci. 2018, 5, 230-235. https://doi.org/10.22543/7674.52.P230235
Păduraru DN, Ion D, Nica AE, Coman F, Coțofană M, Badiu DC, Grigorean VT, Bolocan A, Andronic O. The Switch from Patented Medicine to the Generic One: An Option or a Necessity? Journal of Mind and Medical Sciences. 2018; 5(2):230-235. https://doi.org/10.22543/7674.52.P230235
Chicago/Turabian StylePăduraru, Dan Nicolae, Daniel Ion, Adriana Elena Nica, Florentina Coman, Marius Coțofană, Dumitru Cristinel Badiu, Valentin Titus Grigorean, Alexandra Bolocan, and Octavian Andronic. 2018. "The Switch from Patented Medicine to the Generic One: An Option or a Necessity?" Journal of Mind and Medical Sciences 5, no. 2: 230-235. https://doi.org/10.22543/7674.52.P230235
APA StylePăduraru, D. N., Ion, D., Nica, A. E., Coman, F., Coțofană, M., Badiu, D. C., Grigorean, V. T., Bolocan, A., & Andronic, O. (2018). The Switch from Patented Medicine to the Generic One: An Option or a Necessity? Journal of Mind and Medical Sciences, 5(2), 230-235. https://doi.org/10.22543/7674.52.P230235



