Abstract
Breast reconstruction after breast cancer surgery represents a positive step in restoring a women’s idea of self by reestablishing her feminine features and confidence, thus improving essential aesthetic and emotional aspects. Regarded as the cornerstone in breast cancer management, the surgical treatment has come a long way since 1884 when W.S. Halsted performed the first radical mastectomy- a disfiguring procedure which was conducted until the late 70s when owing to contemporary advancements it was surpassed by modified radical mastectomies and other far less invasive approaches. Either performed in an immediate or a delayed fashion breast reconstruction can be achieved not only through alloplastic procedures using expander/ implant prosthesis but also through autologous tissue transfers wisely harvested from different parts of the body or through methods that combine the two. When planning a breast reconstruction, after the oncologist formally rules out any form of residual cancer, one must take into consideration several critical factors that will eventually condition the technique election process for example the possible local or systemic adjuvant therapy. Although a “one size fits all” breast reconstruction procedure has yet to prevail, the extensive volume of published literature regarding this matter enables a well-experienced plastic surgeon to proceed with careful procedural selection allowing for the best possible results.
Introduction
Alongside the introduction of national breast cancer screening programs of the female population in well-developed countries, breast malignancies are currently considered to have the highest rate of diagnosis among all types of neoplasia encountered in women. Regarded as the main cancer-related cause of death for this particular group, breast cancer has constantly determined doctors worldwide to elaborate and improve on its management algorithm, thereby presently allowing not only for a complete disease free status after its completion,but also for the possibility of breast reconstruction in an immediate or later state [1].
Cancer has a huge psychological impact on the newly diagnosed patientsby itself, let alone the mutilating mandatory surgical treatment, which comprises partial or total removal of the mammary gland, likely accompanied by radio-, chemo-, hormonal or immunotherapy, which further alters both self-confidence and mental health [2]
Breast reconstruction after breast cancer surgery represents a positive step in restoring a women’s idea of self by reestablishing her feminine features and confidence, thus improving essential aesthetic and emotional aspects.
Discussion
Acknowledged as the keystone in breast cancer management, the surgical treatment has come a long way since 1884 when W.S. Halsted performed the first radical mastectomy, removing both the pectoralis major and minor along with the entire mammary gland and axillary lymph nodes, in order to fully eradicate a breast tumor [3]. This disfiguring procedure was routinely conducted on women presenting with various breast masses that were deemed malignant in nature until the late 70s, when owing to contemporary advancements in tumor histology and grading systems, it was surpassed by modified radical mastectomies described by Madden or Patey and other far less invasive approaches, adapted in accordance with tumor characteristics [4].
Today’s recent introduction of gene mapping as part of the breast cancer protocol for high-risk patients has set the stage for an innovative means of handling some specific situations [5]. The positive BRCA1/ BRCA2 gene status, encountered in female patients with a personal or a strong family history of breast or ovarianneoplasia, will significantly increase their lifetime risk of developing breast cancer, determining most of them to undergo prophylactic mastectomies, therefore lowering the incidence of future cancer below 10% [6,7].
Either performed in an immediate or a delayed fashion, according to possible necessary adjuvant local or systemic therapies, breast reconstruction can be achievednot only through alloplastic procedures using expander/implant prosthesis but also through autologous tissue transfers wisely harvested from different parts of the body or through methods that combine the two [8].
Irrespective of the method of choice, the main goal of breast reconstruction is restoring proper shape and size to the breast mound, aiming forthe most natural aspect that can be achieved when nude and a normally appearing breast when clothed [2,9].
Although no single procedure outshines the others, careful patient selection plays a key role in obtaining the best possible relative outcome. When planning a breast reconstruction, after the oncologist formally rules out any form of residual cancer, one must take into consideration several critical factors that will eventually condition the technique election process [9]. Radiotherapy, if employed, exerts a cruel effect on the post-mastectomy skin flaps, rendering them prone to developing local necrosis (Figure 1), hyperpigmentation (Figure 2), increased fibrosis or important edema. This guides the plastic surgeon towards an autologous breast reconstruction procedure rather than the use expander/ implants, hence eluding dreaded complications such as implant extrusion or delayed wound healing with possible infection. The shortcomings of radiotherapy are evident even if radiation is applied after breast reconstruction is performed, taking into account capsular contracture and less favorable aesthetic results for alloplastic procedures, and significant fat necrosis or seroma when usingone’s own tissue [10].

Figure 1.
Radiation therapy complications Isle of skin necrosis managed by means of local skin flaps.

Figure 2.
Radiotherapy complications - Periareolar incision hyperpigmentation.
Recent oncoplastic surgical trends advocate for immediate breast reconstruction following mastectomy (Figure 3) rather than reconstruction performed in a delayed manner, obviously shouldthe situation permit it. Advantages such as having a pre-established inframammary fold, a generous skin envelope over the former breast tissue and more importantly it being a one-stage procedure, therefore undergoing general anesthesia only once, has turned this type of reconstruction technique into a method of choice [2].
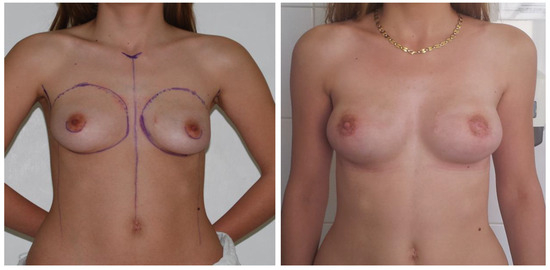
Figure 3.
Immediate breast reconstruction using breast implants following a prophylacticnipple sparring mastectomy – before and after aspects.
Given the more than reasonable results, especially when aiming to achieve breast symmetry in bilateral breast reconstructions, all this with less time spent in the operating room and without having to worry about any donor site comorbidities, breast reconstruction using alloplastic materials (Figure 4) benefits from a far greater popularity than its counterpart in both Europe and the US [11].

Figure 4.
Immediate breast reconstruction using breast implants/expanders following a skin-sparing mastectomy.
Setting aside the obviously necessarybreast prosthetics, which can either be saline or silicone- filled, other recently introduced alloplastic materials that are vastly gaining recognition are the acellular dermal matrix products (ADM) (Figure 5). Designed as additional coverage between the lower part of the implant and the subcutaneous tissue, where muscle coverage alone would not suffice, ADMs prove themselves reliable in such situations, thus replacing the use of muscle flap transpositions or free flap transfers in the attempt of proper implant shielding [12].
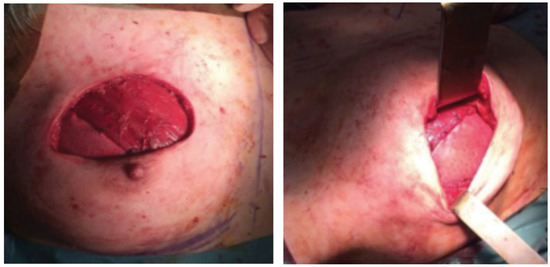
Figure 5.
Acellular dermal matrix used for soft tissue replacement in breast reconstruction procedures.
Breast reconstruction using autologous tissue, though less popular, certainly comes with its own advantages. Regardless of the timing, replacing “self with self”gives both a more natural feel and the possibility of becoming whole again without using any foreign materials, therefore having a hugely positive psychological effect [2].
Presently considered the standard of care in autologous breast reconstruction, the transverse rectus abdominis muscle flap (TRAM) was introduced in 1982 by Hartrampf et al. Based on the superior epigastric vessels, the TRAM flap (Figure 6) provides adequate soft tissue, harvested on muscular perforators arising from the underlying rectus abdominis muscle, for creating a suitable breast mound, whilst simultaneously making the lower abdominal fat disappear, feature that most women find very tempting [13]. This specific aspectimplies certain drawbacks, such as the possibility of developing abdominal wall weaknesses, hernias or unaesthetic asymmetries, thus urging for the correct positioning of a prolene mesh to be considered in order to prevent these unwanted outcomes [14]. Another, almost equally important pedicled flap is the latissimusdorsimyocutaneous flap. Based on the thoracodorsal vascular pedicle, this type of flap may be used either alone, in its extended version,with additional adipose tissue being harvested with the typical skin island or for implant coverage in hybrid procedures that use both autologous tissue and alloplastic materials [15].

Figure 6.
Right breast reconstruction using a pedicled TRAM flap.
Recent advances in the microsurgical field have provided additional meansfor the surgeon when autologous breast reconstruction is envisaged. The free TRAM flap, the deep inferior epigastric perforator flap (DIEP) and the superficial inferior epigastric artery flap (SIEA) are harvested on the inferior epigastric vessels, whichever deep or superficial, and transferred as free flaps to be anastomosed to the internal mammary artery or thoracodorsal artery. Other less popular free flaps used in breast reconstruction such as the superior and the inferior gluteal artery perforator flaps or the profundafemorisartery perforator flap harvest tissue from the hip, buttocks or thigh regions [16].
Breast reconstruction can sometimes be achieved through autologous fat tissue grafting procedures, where fat may be harvested from various parts of the bodyby means of liposuction [17].
Conclusion
Although a “one size fits all” breast reconstruction procedure has yet to prevail, the extensive volume of published literature regarding this matter enables a well-experienced plastic surgeon to proceed with careful procedural selection allowing for the best possible results [2]. However, despite the advances in the reconstruction technique, care should be taken to guide the patients into developing realistic expectations, taking into account the unavoidable visible incision lines on the reconstructed breast and on the donor site should the procedure require one, the different sensation of the reconstructed breast and the imperfect symmetry, especially when unilateral breast reconstruction is performed [9].
Disclosure
No authors involved in the production of this article have any commercial associations that might pose or create a conflict of interest with information presented herein.
References
- Lucas, D.J.; Sabino, J.; Shriver, C.D.; Pawlik, T.M.; Singh, D.P.; Vertrees, A.E. Doing More: Trends in Breast Cancer Surgery, 2005 to 2011. 2015, 81, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Serletti, J.M.; Fosnot, J.; Nelson, J.A.; Disa, J.J.; Bucky, L.P. Breast reconstruction after breast cancer, Plast. Reconstr. Surg. 2011, 127, 124e–135e. [Google Scholar] [CrossRef] [PubMed]
- Ghossain, A.; Ghossain, M.A. History of mastectomy before and after Halsted. J Med Liban 2009, 57, 65–71. [Google Scholar] [PubMed]
- Young, R.E. The history of breast cancer surgery: Halsted’s radical mastectomy and beyond, Australian Medical Student Journal 2013, 4, 53.
- Soltanian, H.; Okada, H. Understanding genetic analysis for breast cancer and its implications for plastic surgery. Aesthet. Surg. J. 2008, 28, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, A.; Pharoah, P.D.; Narod, S.; Risch, H.A.; Eyfjord, J.E.; Hopper, J.L.; Loman, N.; Olsson, H.; Johannsson, O.; Borg, A.; Pasini, B.; Radice, P.; Manoukian, S.; Eccles, D.M.; Tang, N.; Olah, E.; Anton- Culver, H.; Warner, E.; Lubinski, J.; Gronwald, J.; Gorski, B.; Tulinius, H.; Thorlacius, S.; Eerola, H.; Nevanlinna, H.; Syrjäkoski, K.; Kallioniemi, O.P.; Thompson, D.; Evans, C.; Peto, J.; Lalloo, F.; Evans, D.G.; Easton, D.F. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003, 72, 1117–1130. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, L.C.; Sellers, T.A.; Schaid, D.J.; Frank, T.S.; Soderberg, C.L.; Sitta, D.L.; Frost, M.H.; Grant, C.S.; Donohue, J.H.; Woods, J.E.; McDonnell, S.K.; Vockley, C.W.; Deffenbaugh, A.; Couch, F.J.; Jenkins, R.B. Efficacy of bilateral prophylactic mastectomy in BRCA1 and BRCA2 gene mutation carriers. J Natl Cancer Inst. 2001, 93, 1633–1637. [Google Scholar] [CrossRef] [PubMed]
- Nahabedian, M.Y. Breast reconstruction: A review and rationale for patient selection. Plast Reconstr Surg. 2009, 124, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Guyomard, V.; Leinster, S.; Wilkinson, M. Systematic review of studies of patients’ satisfaction with breast reconstruction after mastectomy. Breast 2007, 16, 547–567. [Google Scholar] [CrossRef] [PubMed]
- Kronowitz, S.J.; Robb, G.L. Radiation therapy and breast reconstruction with postmastectomy radiation therapy: Current issues. Plast Reconstr Surg 2004, 114, 395–408. [Google Scholar] [CrossRef]
- Collis, N.; Sharpe, D.T. Breast reconstruction by tissue expansion: A retrospective technical review of 197 two-stage delayed reconstructions following mastectomy for malignant breast disease in 189 patients. Br J Plast Surg. 2000, 53, 37–41. [Google Scholar] [PubMed]
- Sbitany, H.; Sandee, S.N.; Amalfi, A.N.; Davenport, M.S.; Langstein, H.N. Acellular dermis-assisted prosthetic breast reconstruction versus complete submuscular coverage: A head-to-head comparison of outcomes. Plast Reconstr Surg. 2009, 124, 1735–1740. [Google Scholar] [CrossRef] [PubMed]
- DeBono, R.; Stevenson, J.H.; Thompson, A. Immediate versus delayed free TRAM breast reconstruction: an analysis of perioperative factors and complications. British Journal of Plastic Surgery 2002, 55, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Man, L.X.; Selber, J.C.; Serletti, J.M. Abdominal wall following free TRAM or DIEP flap reconstruction: A meta-analysis and critical review. Plast Reconstr Surg. 2009, 124, 752–764. [Google Scholar] [PubMed]
- Hammond, D.C. Latissimus Dorsi Flap Breast Reconstruction. Plast Reconstr Surg. 2009, 124, 1055–1063. [Google Scholar] [CrossRef] [PubMed]
- Avraham, T.; Clavin, N.; Mehrara, B.J. Microsurgical Breast Reconstruction. Cancer Journal 2008, 14, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Missana, M.C.; Laurent, I.; Barreau, L.; Balleyguier, C. Autologous fat transfer in reconstructive breast surgery: Indications, technique and results. European journal of surgical oncology 2007, 33, 685–690. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the author. 2015 Jecan Cristian Radu, Hernic Alexandru Daniel, Filip Iulia Cristina, Răducu Laura