Introduction
Periodontal disease, a chronic inflammatory condition affecting the supporting structures of the teeth and vitamin D deficiency, a common nutritional insufficiency, have both been extensively studied. However, evidence suggests a potential interplay between these two entities, implicating vitamin D deficiency as a potential risk factor for the development and progression of periodontal disease. This study aims to high-light the relationship between periodontal disease and vitamin D deficiency, exploring the underlying mechanisms and clinical implications. Recent scientific findings suggest that a deficiency in Vitamin D (25(OH)D) may potentially contribute to the onset of periodontitis [
1]. Garcia et al. [
2] have demonstrated that supplementation with calcium and vitamin D could potentially decrease the severity of periodontal disease. In the progression of periodontitis, Vitamin D plays a beneficial role due to its direct impact on bone metabolism. In addition to maintaining calcium and bone balance, Vitamin D may also inhibit inflammatory mediators that contribute to periodontal da-mage through its antibiotic effects on periodontopathogens [
2].
Vitamin D, a fat-soluble hormone, is primarily obtained through sunlight exposure, as well as dietary sources and supplements in young adults not sufficiently exposed to sunlight, and patients suffering from malabsorption, consumption of vitamin D supplements or vitamin D fortified foods are required to meet the daily need, approximately 2000 IU/day to maintain serum 25(OH)D levels greater than 30 ng/mL [
3]. Dietary intake contributes around 20% of the required vitamin D amount [
4]. There are two main forms of Vitamin D: Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol). Vitamin D2 mainly comes from plants and can be synthetically produced, while Vitamin D3 is synthesized in human skin from 7-dehydrocholesterol upon sun-light exposure. Both forms remain inactive until undergoing enzymatic hydroxylation [
5,
6]. Numerous studies highlight the diverse biological functions of Vitamin D: facilitating calcium absorption, maintaining optimal serum calcium and phosphate levels for healthy bone mineralization, reducing inflammation, and regulating immune, neuromuscular, and metabolic functions [
7,
8,
9].
Since 2016, the medical community has been increasingly concerned about Vita-min D deficiency, especially in Europe, where roughly 40% of the population is deficient [
10]. Recent studies link low Vitamin D levels to the development of various chronic diseases [
11]. The etiology of Vitamin D deficiency is complex, involving fac-tors such as inadequate intake of Vitamin D-rich foods, limited sun exposure, body mass index, age, gender, clothing choices, race, and socioeconomic status [
11].
The serum level of 25(OH)D is the best indicator of Vitamin D status, as it represents the primary circulating form with a half-life of two to three weeks [
12,
13]. The World Health Organization defines Vitamin D deficiency as a serum 25(OH)D level below 20 ng/mL (50 nmol/L), insufficiency as 20–29 ng/mL (52–72.5 nmol/L), and sufficiency as 30 ng/mL (75 nmol/L) or higher [
14,
15].The findings of a meta-analysis con-ducted in 2022, which comprised 1455 patients, revealed that individuals with periodontitis exhibit lower serum Vitamin D levels in comparison to the general population[
16]. Scaling and root planning (SRP) combined with Vitamin D supplementation has been shown to significantly improve periodontal clinical parameters [
16].
Periodontal disease is an inflammatory condition affecting the gingiva and alveolar bone. It is primarily initiated by the accumulation of dental plaque, leading to inflammation, tissue destruction, and ultimately tooth loss if left untreated. Despite advances in prevention and treatment, periodontal disease remains highly prevalent globally, posing significant public health challenges [
1]. The global impact of oral diseases like caries and severe periodontitis is significant, affecting billions of individuals worldwide and placing a considerable burden on public health systems. According to the European Federation of Periodontology (EFP) and The Economist Impact's new white paper, caries impacts approximately 2 billion individuals, while severe periodontitis affects around 1 billion people [
17]. These conditions not only cause physical discomfort but also pose significant challenges to overall well-being and healthcare systems. The World Health Organization (WHO) emphasizes the urgency of addressing these oral health issues in its Global Oral Health Status Report, high-lighting the need for universal health coverage for oral health by 2030. Recognizing the widespread impact of caries and periodontitis, concerted efforts are required to mitigate their prevalence and provide accessible, comprehensive oral healthcare for all [
18].
Chronic periodontitis significantly impacts the quality of life for affected individuals compared to those with good periodontal health. The disease progressively da-mages gingival and the supportive tissues of the teeth, including the alveolar bone, cementum, and periodontal ligament [
19,
20]. While various microorganisms contribute, toxins from gram-negative bacteria play a key role by triggering the release of pro-inflammatory mediators and inducing both local and systemic inflammation [
21,
22]. Considering inflammation as a common factor, a potential link between Vita-min D deficiency and the onset and progression of periodontal disease is plausible. Socioeconomic disparities correlate with diminished awareness of oral hygiene practices, heightened consumption of sugary food and beverages exacerbating these ailments, elevated rates of malnutrition, and limited access to personal preventive measures and products like toothbrushes, dental floss, interdental brushes, and fluoride-based oral care items. Additionally, these vulnerable groups face significant hurdles in accessing adequate treatment options. Developing countries experience a higher prevalence of moderate and severe periodontitis compared to wealthier nations [
23,
24,
25].
Moreover, also other factors contribute to the onset and progression of periodontal disease. These factors include behaviors such as alcohol consumption and smoking, which have been widely recognized as detrimental to overall health and are linked to increased susceptibility to various diseases, including periodontal and systemic conditions [
1]. Notably, poor oral hygiene plays a crucial role in the development of periodontal disease. Inadequate brushing, flossing, and regular dental check-ups can lead to the accumulation of plaque and tartar, providing a favorable environment for the proliferation of pathogenic bacteria and subsequent inflammation of the gums [
17]. Also stress, a prevalent factor in modern lifestyles, has been associated with immune dysregulation and inflammation, potentially exacerbating the severity of both periodontal disease and systemic conditions such as rheumatoid arthritis, chronic disorders, diabetes, and osteoporosis [
17,
22,
23].
Signs of periodontal disease development include gingival bleeding, suppuration, halitosis, plaque accumulation (bacterial biofilm), calculus formation, and loss of alveolar bone [
18]. Several physiological pathways have been proposed to elucidate the potential link between vitamin D deficiency and periodontal disease. Vitamin D receptors (VDRs) are expressed in various oral tissues, including gingival epithelial cells, fibroblasts, and immune cells, suggesting a direct regulatory role in periodontal health [
1,
2,
3,
4,
5]. Vitamin D deficiency may compromise the host's immune response to periodontal pathogens, leading to dysregulated inflammation and tissue destruction. Moreover, vitamin D insufficiency has been associated with impaired wound healing and com-promised bone remodeling, exacerbating periodontal tissue damage [
10,
11,
12,
13,
14,
15].
Despite the existing knowledge gaps, recognizing the potential link between periodontal disease and vitamin D deficiency holds clinical implications for oral healthcare professionals. Routine assessment of vitamin D status and supplementation in at-risk populations may offer adjunctive benefits in the management of periodontal disease, particularly in individuals with concurrent risk factors such as smoking, diabetes, or immune disorders.
Case Presentation
For this study, 2 representative cases were selected, both with advanced periodontitis and vitamin D deficiency. Following laboratory analysis, case 1 exhibited a value of 24.5 ng/mL, while case 2 showed 7.4 ng/mL. Both patients do not present associated systemic diseases. They have been referred to the Department of Periodontology, Faculty of Dental Medicine, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania, for periodontal evaluation by a general practitioner.
The evaluated clinical parameters were bleeding upon probing (BOP), plaque index score (according to O’Leary et al.) [
26], probing depth (PD) and radiographic bone loss (BL). All measurements were conducted by the same examiner using a periodontal probe (North Carolina 15 mm probe), assessing six sites for each tooth. The periodontal clinical examination was also complemented by radiological examination.
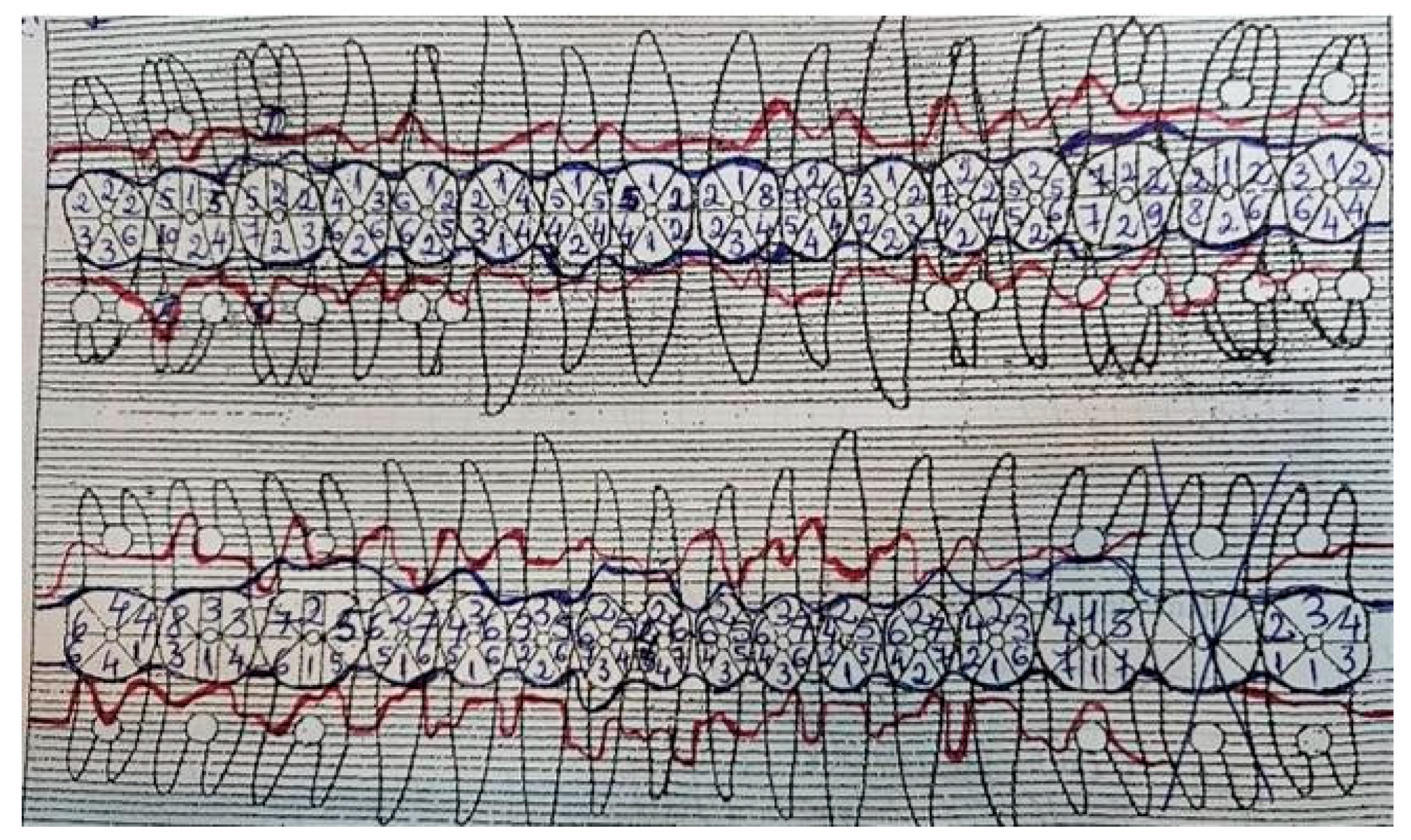
Case 1 was a 22-year-old male (
Figure 1), without of known illnesses or systemic risk factors such as diabetes or hematological disorders, non-smoker, and not under any medication regimen.
From the routine medical analyses conducted, a deficiency of vitamin D was observed, without recommended treatment. The initial visit was prompted by concerns about tooth mobility that had developed over the past 2 years, poor aesthetic appearance of the gums and tooth misalignment. The initial examination revealed deep probing pocket depths, tooth mobility, bleeding upon probing, gum recession, and signs of gingival inflammation (
Figure 1 and
Figure 2).
The plaque index score registered were 76%, radiographic bone loss 55% (more than half of the tooth's root) The bleeding upon probing index (BOP) measured at 45%. The probing depth (PD) was 8 mm for both maxillary incisors and 7 mm for the mandibular first molars and premolars. Tooth mobility, assessed using the Miller Classification, was categorized as class 1 for both maxillary and mandibular incisors, and class 2 for the left mandibular lateral incisor (
Figure 2).
Among the local predisposing factors contributing to periodontal disease, observations included dental malposition of the maxillary and mandibular central and lateral incisors, deep bite malocclusion, and the presence of deep and advanced carious lesions in both maxillary and mandibular molars and premolars. The diagnosis was periodontitis stage III, grade C. Stage III of periodontitis in this case, was defined based on the severity and complexity of management. The grade of periodontitis was estimated with direct or indirect evidence of % bone loss/age > 1.0 and destruction exceeding biofilm deposits (suggestive of rapid progression and early onset disease) [
27,
28]. The orthodontic diagnostic was class II, division 1 malocclusion (Angle classification).
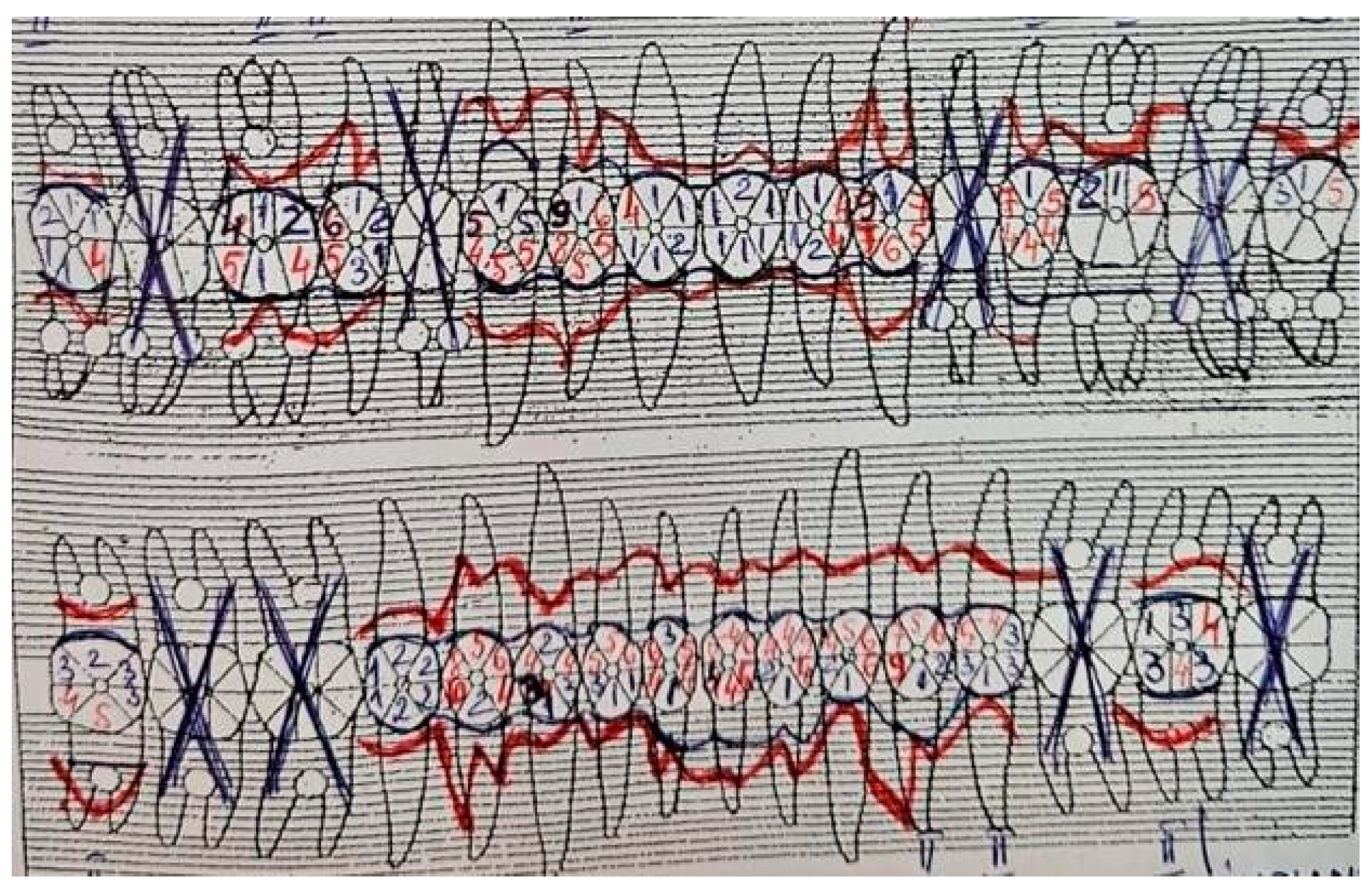
The patient has no history of periodontal treatment. The periodontal changes are also encountered in the case 2 of a 47-year-old woman (
Figure 3). Medical analyses revealed a deficiency of vitamin D, which was also noted to be untreated. Serum calcium levels remained unchanged. The first appointment was prompted by similar concerns as in case 1, regarding the poor aesthetic appearance of the gums, tooth mobility, and misalignment, along with additional issues related to chewing difficulties.
The initial examination revealed deep probing pocket depths, tooth mobility, bleeding upon probing, radiographic bone loss, gum recession, and signs of gingival inflammation (
Figure 3 and
Figure 4). The plaque index score registered were 23%, radiographic bone loss 65% (more than half of the tooth's root) and bleeding upon probing index (BOP) were 68%. The initial probing depth (PD) was 8 mm at the both maxillary canine and incisors and 9 mm at the mandibular canine and first premolars. The tooth mobility (Miller Classification) was class 2 for maxillary first premolar and molar and class 3 for right maxillary lateral incisor. The diagnosis was periodontitis stage III, grade C. Stage III of periodontitis, in this case, was defined based on the severity (radiographic bone loses extending to the apical third of the root) and probing depth > 6 mm, vertical and horizontal bone loss). The grade of periodontitis was estimated with evidence of bone loss/age > 1.0 [
25,
26].
The patient had a history of periodontal treatment. The diagnosis of periodontal disease was made six years ago during the initial visit by a general dentist. The treatment followed, consisted of initial periodontal therapy including antimicrobial treatment, subgingival debridement and additional a composite splint was applied to the lower mandibular incisors due to increased mobility Additionally, the patient presented with fixed prosthetic supported by dental abutments in the maxilla as well as dental and implant support in the mandible, which were performed 4-5 years ago.
Treatment
Both patients accepted the proposed periodontal treatment plan and signed the informed consent form.
The initial treatment commenced with the removal of supragingival plague, supragingival and subgingival tartar associated with antiseptics irrigation (chloramine solution 3‰ and hydrogen peroxide solution 3%) [
29,
30] and local antibiotics (prescription prepared at the pharmacy and consisted of Tetracycline and Metronidazole in equal amounts, along with Vaseline as a vehicle. This mixture was applied into the periodontal pocket using a special syringe, under isolation and administered with a seven-day interval between applications. The quadrant subgingival debridement was carried out using hand instruments (Gracey curettes). Also, the patient was instructed on how to improve his oral hygiene and recommended to use, at home, an adjuvant topical antimicrobial product after oral hygiene and to applied it with a small piece of gauze in 8-10 circular motions from the base to the tip of the papilla and in linear motions along the gingival margin. This topical antimicrobial product was a mixture of two antibiotics (neomycin and metronidazole), hydrocortisone acetate, Stamycin, and vitamin A, with glycerol as the vehicle [
30].
This initial antimicrobial treatment was performed in two treatment sessions with a one-week interval between them. Tetracycline has anti-collagenolytic properties that inhibit the MMPs (matrix metalloproteinases), has an antioxidant role, and as metronidazole, it can be administered locally with minimal secondary effects [
31,
32]. SRPs were performed in multiple sessions, due to persistent inflammatory gingival signs. In addition to periodontal treatment, both patients were recommended by the general medicine specialist to start vitamin D supplements therapy. In case 1, the patient initially underwent treatment with 2000 IU of vitamin D for one month. Subsequently, following clinical and laboratory examinations and upon the recommendation of the general practitioner, the patient continued long-term treatment with a vitamin D supplement of 10000 IU. In case 2 treatment for vitamin D started with supplementation of 4000 IU daily for eight months, followed by regular visits to the general practitioner for monitoring. Both patients remain under specialized medical supervision.
After 3 months from the antimicrobial phase I periodontal treatment and vitamin D supplementation during follow-up consultations, improvement in the gingival and periodontal status was observed in both patients. Plaque index, probing depth and bleeding on probing were reduced, and the gingiva acquired a clinically healthy aspect. Improvement was noted also in areas where mobility was classified as Miller Class I. The patients no longer reported discomfort or other subjective clinical manifestations. After this treatment, the patients were able to improve their dental hygiene, as the teeth were splinted with composite resin.
Following this periodontal treatment, at the one-month follow-up appointment, a reduction in clinical indicators of inflammation was observed in both cases. The plaque index decreased to 18 % for case 1 and to 10% for case 2. Additionally, the bleeding on probing index decreased to 11% for case 1 and to 17% for case 2. A decrease in probing depth of periodontal pockets to 4-5 mm was observed, with the exception of maxillary molars for case 1 and mandibular canines for case 2. For these teeth, a gingival probing depth of 6 mm was maintained, but without bleeding or other signs of inflammation. The serum vitamin D level remained unchanged for case 2, but in case 1, as a result of interrupting vitamin D treatment, at the 6-month evaluation from baseline, the vitamin D level decreased to 12 ng/mL. Therefore, continuous monitoring of vitamin D alongside periodontal status evaluation is necessary to reduce the risk of exacerbating periodontal disease.
Discussions
Vitamin D deficiency has been linked to compromised immune function, making it crucial for overall health and disease prevention. Adequate levels of vitamin D play a vital role in supporting the immune system's ability to fight off infections and maintain optimal function. Insufficient vitamin D levels may increase susceptibility to various illnesses and impair the body's ability to mount an effective immune response. Therefore, maintaining adequate vitamin D levels through supplementation or sun exposure is essential for bolstering immune function and reducing the risk of infections and other health issues [
3].
There are few studies in the literature regarding the role of vitamin D on marginal periodontitis. Serum vitamin D determinations are not part of routine investigations. It is often recommended to investigate especially in postmenopausal women with signs of osteoporosis. Another reason is the high cost of this investigation. In the specialized literature, numerous microbiological, immunological, and genetic studies have been conducted to investigate the correlation between vitamin D deficiency and periodontal disease. A study (Madi M. et al. in 2021) [
32] examined how vitamin D levels influence the composition and diversity of oral microbial flora among patients with periodontal disease. They found that vitamin D deficiency is associated with significant changes in oral microbial flora, which may contribute to the progression of periodontal disease [
32]. Liang et al. investigated the effects of vitamin D supplementation on the immune response in inflamed periodontal tissues. Their results suggested that vitamin D can modulate the inflammatory response of the immune system, thereby reducing gingival inflammation and improving periodontal health [
33]. Du Fulan et al. (2022) examined the association between genetic polymorphisms involved in vitamin D metabolism and predisposition to periodontal disease. They identified certain genetic variations that can influence vitamin D levels and susceptibility to periodontal disease, highlighting a possible genetic component in this relationship [
34].
These studies provide a deeper understanding of the mechanisms through which vitamin D may influence periodontal diseases, underscoring the importance of assessing and correcting vitamin D deficiencies in the management and treatment of these conditions. The association between vitamin D deficiency and periodontal disease has gained attention in recent years. Vitamin D plays a crucial role in maintaining oral health by modulating the immune response, regulating inflammatory pathways, and promoting calcium homeostasis in periodontal tissues [1-5]. Research suggests that inadequate vitamin D levels may exacerbate periodontal inflammation and compromise periodontal tissue integrity. Low vitamin D status is associated with increased pro-inflammatory cytokine production, impaired antimicrobial peptide synthesis, and dysregulated osteoclast activity, contributing to periodontal tissue breakdown and bone resorption [
9,
10].
Furthermore, vitamin D deficiency may influence the host response to periodontal pathogens, leading to heightened susceptibility to periodontal infections and delayed wound healing. Studies have shown a negative correlation between serum vitamin D levels and periodontal disease severity, highlighting the potential therapeutic implications of vitamin D supplementation in periodontal management. Periodontitis has been correlated with vitamin D deficiency, unlike gingivitis and individuals with healthy gum tissues. Additionally, the severity of periodontitis has been found to be associated with the levels of vitamin D present in an individual's bloodstream [
35]. The interplay between vitamin D status and periodontal health is complex and multifactorial. Factors such as age, gender, ethnicity, sun exposure, dietary intake, genetic predisposition, and systemic comorbidities can influence vitamin D metabolism and periodontal disease susceptibility [
36,
37].
In these clinical cases, several factors contributed to the onset and progression of periodontal disease: occlusal trauma resulting from teeth misalignment, untreated edentulous areas (resulting from the progression of periodontal disease and advanced carious lesions), deep bite malocclusion, and multiple carious lesions.
Additionally, the patient's age must be factored into the decision-making process when devising a treatment plan.
Both cases were diagnosed with advanced periodontitis and presented the same local predisposing factors. They only differ in two risk indicators: age and gender. Both patients had good socio-economic conditions, a balanced diet, without other restrictions. The first case involves a young male patient with a milder severity of periodontal involvement but with a pattern of rapidly progressive aggressive periodontitis compared to the second case, where clinical signs of periodontitis were more advanced in an older woman, indicating a potentially slower progression of the disease. Moreover, the deficiency in vitamin D was significantly more pronounced in the second case and could be correlated with the more advanced periodontal issues compared to the first case. It’s noteworthy that the patient in the first case did not undergo periodontal treatment, whereas the patient in the second case did receive such treatment. Consequently, in the absence of periodontal intervention in the second case, the clinical signs of periodontal affection would likely have been much more advanced [
38,
39].
The reassessment of serum vitamin D levels shows that correction in the short term is quite challenging, requiring regular monitoring over time intervals, collaboration with the general practitioner, and, last but not least, patient compliance. Thus, the combination of local antiseptics and antibiotic therapy, both in-office and at home, in patients with advanced periodontitis and vitamin D deficiency has proven to be beneficial, especially in cases where the immune response is compromised [
40].
This underscores the importance of timely intervention and adherence to treatment protocols in managing periodontal disease, especially in cases where vitamin D deficiency exacerbates the condition. It also highlights the potential role of vitamin D supplementation as an adjunctive therapy in periodontal treatment, particularly in cases where deficiency is severe. Our study confirms these findings, showing that patients with a more severe vitamin D deficiency exhibited more advanced and severe periodontal disease compared to those with moderate deficiency. Also, the current study underscores the importance of evaluating vitamin D levels in the context of assessing and managing periodontal disease [
41].
Furthermore, our observations are consistent with the hypothesis that interventions to correct vitamin D deficiency could be beneficial in managing periodontal disease. Vitamin D supplementation or controlled sun exposure may play a significant role in reducing gingival inflammation and slowing the progression of periodontal disease among deficient patients.