Abstract
Objectives. Up to 20% of patients with biliary lithiasis have bile duct stones, which are asymptomatic in 50% of cases. The aim of the study was to evaluate the role of choledoscopy in extracting stones from the main bile ducts. Materials and Methods. This is a retrospective study (January 2014–December 2024) on 2309 patients who underwent a laparoscopic cholecystectomy. Laparoscopic choledoscopy was performed in 32 cases. Of the 32 patients with complete clearance, none had residual common bile duct stones (CBDS) at 1 year postoperatively. Results. The ideal approach in our study was the transcystic approach, with the shortest hospital stays (mean 3 days) transcholedochal approach; it was only feasible in 7 patients. All patients had transcystic drainage that was removed after 10 days (mean operative time 105 min). The transcholedochal approach was demanding from a technical point of view. Primary ductal closure was performed in 5 patients. Ductal closure with transcystic drain was in 9 patients. A total of 14 patients had a T-tube and a longer operative time (on average 170 min). Conversion to open surgery was performed in 4 cases, due to difficult dissection at the level of the hepatic porta. Conclusions. LCBDE for previously documented or discovered CBDS during LC is a safe and feasible procedure. The technique is technically demanding, and requires advanced laparoscopic skills. Patient selection is very important, but the transcystic approach for LCBDE when possible is optimal.
Introduction
The first direct visual exploration of the main biliary duct was obtained in 1880 by the use of a magnifying glass. In the year 1923, an optical device with a proximal placed mirror with reflective properties was used to reflect the light from a headlamp placed on the surgeon’s head [1]. In 1941 the first choledochoscope was offered by modifying a cystoscope [2]. In the year 1953, Wildegans presents a modified version of the rigid choledochoscope which was also marketed in the year 1958 [3]. In the year 1970, Hopkins offered a refined and embedded lens mounted in a Karl Stortz choledochoscope [4]. The flexible choledochoscope was introduced late in 1965 [5].
The advantage of the flexible system over the rigid choledochoscope was the better maneuverability, but the optical image was inferior in quality. From then until now, the flexible choledochoscope is constantly evolving. Most flexible modern choledochoscopes can provide good images when compared to the rigid ones. Also, they have a working shaft in which instruments are introduced to reach the biliary tract. Flexible choledochoscopes with a diameter between 0.8 and 2 mm are now manufactured. They did not incorporate a working channel for tools. Choledochoscopes with working channels had a diameter between 3 and 5 mm [6,7,8].
The choledoscope is introduced through a cannula placed in the right subcostal midclavicular line. In the present, the preferred treatment for main bile duct stones is sequential, ERCP being initially performed and the bile duct stones are extracted. After 24-72h a laparoscopic cholecystectomy is performed. Complications related to this procedure occur in 5-10% of cases and consist of duodenal perforation, bleeding from sphincterotomy, acute pancreatitis, residual lithiasis. It has a general mortality of the 0.4-0.7% [9,10].
The main disadvantages of this method are related to the loss of the oddian sphincter function, to the inherent morbidity of this technique and higher costs. Although choledoscopy has no specific contraindications or risks, but it is expensive. The price of a complete line of video-choledoscopy can exceed 40,000 Euro [7,11].
From the point of reliability, cholangioscopy performs the most effective direct evaluation of the biliary tract. Choledoscopy reduces the percentage of residual lithiasis to values between 0 and 2.3%. It is less reliable in terms of ductal and ampullary functional assessment, cholangio-graphy being the imaging method of choice for assessing bilio-ampullary functional status [12].
Data evidence suggests that the associated endoscopic-laparoscopic approach requires an increased number of procedures while choledoscopy is associated with shorter hospital stay, with similar or lower ductal clearance and similar morbidity [13,14]. The reoperation rate after choledoscopy is comparable to postoperative ERCP [15].
The aim of our study was to evaluate how and when cholecystectomized patients needed and benefited from choledochoscopy.
Materials and Methods
We conducted a retrospective descriptive study over 16 years (January 2014–January 2024). The study includes a group of 2,309 patients who underwent laparoscopic cholecystectomy within the general surgery clinic of the Emergency Clinical Hospital “Prof. Dr. Agrippa Ionescu”, Bucharest. The processed data were obtained from the patient observation sheet. The technical devices with which the imaging investigations were carried out were evaluated to obtain the images. The inclusion criteria were the laparoscopic cholecystectomy. In addition, the following variables were collected: gender, age, intraoperative diagnosis, type of surgery performed, imaging methods of the main biliary tract.
Technique
Laparoscopic surgery was performed using the AESCULAP HD laparoscopy line. To perform intra-operative cholangiofibroscopy, the OLYMPUS P60 model cholangiofibroscope was used: VISERA-OTV S7. The angular angle of the distal segment, controllable by the lever located in the proximal segment which can be rotated approximately 290 degrees in a single plane. A wider field of view is obtained by associating the instrument rotation.
This maneuverability of the flexible choledochoscope ensures better access to the biliary tree. It can reach the intrahepatic ducts of the second or third ramification. The diameter is about 3-5 mm and allows the operator to explore the entire biliary tree to the level of the intrahepatic third order biliary branches. It is equipped with 3 separate channels: illumination, optics and working channel. The distal segment of the main biliary tract can be explored without the surgical mobilization of the duodenum. The toolset used, via the working channel, includes basket probes (Dormia type), curettes, biopsy pens and "grasp" type retractors, balloon catheters, mechanical lithotripters, hydraulic, ultrasonic or laser devices for fragmentation or tumor drilling [16,17,18].
Choledoscopy involves operation in a liquid environment, which is obtained by continuous irrigation of the main biliary tract through the instrument’s irrigation and working channel. We use physiological serum in containers of 500-1000 mL, adapted through a sterile tubing to the valve of the instrument and directing the flow for irrigation through the working channel. A cold (halogen) light source, an image processing unit and a video monitor are required for viewing. The video monitor can be common with the laparoscopy line if it has two video inputs (line A and B), and the system also includes a video mixer. We use two monitors for increased magnification.
When adopting the surgical procedure, the anatomical and clinical form of the main bile duct stones needs to be taken into account. Thus, in favorable cases, a choledochotomy was performed with the extraction of stones by choledocholithotomy, followed by external biliary drainage with a T-tube. In complex forms, however, major operations such as choledochoduodenostomy or specific ones such as transduodenal oddian sphincterotomy are often required. In malignant forms, a bilio-jejunal anastomosis is necessary. Access to stones should be obtained by multiple methods, such as those described below.
Transcystic approach
The following conditions must be met for transcystic approach: the cystic duct must be wide, freestones, and implanted on the right side of the bile duct. The investigation will be carried out by putting in tension the cystic duct that was previously dissected and clipped to interrupt the communication with the gallbladder.
A small transverse breach will be created in the cystic duct, through which a cannula is inserted to perform the laparoscopic cholagioscopy (Figure 1). The cholangio-fibroscope is inserted through cannula no. 3 (located on the midclavicular line below the rib margin) in the abdomen and will be guided into the cystic duct by means of an atraumatic clamp (Figure 2). If the cystic duct is not wide enough, it will be dilated using a catheter equipped with a balloon which has a diameter of 5-7 mm (cholangio-fibroscope has a diameter of 3-5 mm) (Figure 2). During this time, the operator must simultaneously observe the information provided by the two monitors: the laparoscope and the cholangiofibroscope. If the local anatomy also allows and the cystic duct is short and perpendicular to the common hepatic bile duct, the operator can use the fiberscope to ascend to the level of the intrahepatic branches of order 2 even 3. The investigation will be concluded either by the external drainage of the cystic duct that serves to extract any residual gallstones or by its ligation/clipping. For an experienced surgical team, the exploration does not exceed 15 min.
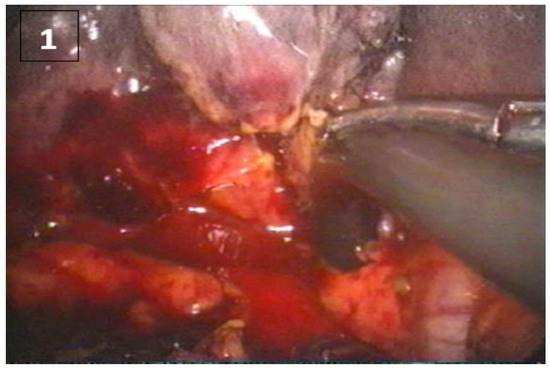
Figure 1.
Main bile duct stone extracted through a transcystic approach (part 1).
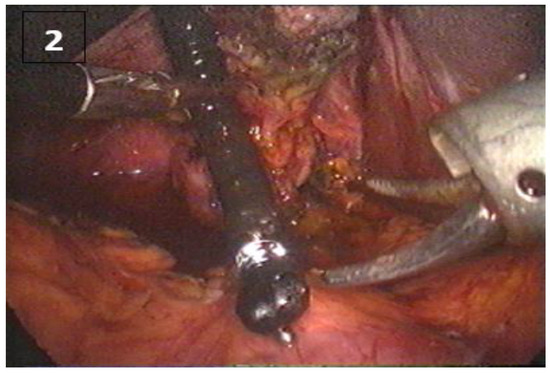
Figure 2.
Main bile duct stone extracted through a transcystic approach (part 2).
The transcholedochal approach
In this situation, the main bile duct approach is performed by choledochotomy, but for the investigation to be carried out in complete safety for the patient, the choledoscope must have a diameter of minimum 7 mm and a maximum of 14 mm. Cholecystectomy will be performed at the end of the intervention, as the gallbladder offers a traction point to expose the bile ducts. The choledochotomy will be performed on a length of approximately 1 cm and the laparoscopic scissors will be used. Later the breach will be increased with fine scissors and the cholangiofibroscope will be introduced, which is initially directed to the papilla and then proximally to the left and right hepatic ducts (Figure 3). The investigation will be concluded either by performing a biliojejunal anastomosis or by installing external biliary drainage: T-tube or transcystic, but in the latter situation, choledorafy will be required. The investigation is limited by the size of the choledochal duct, which must be at least 7 mm. Choledochotomy can be performed with a laparoscopic scalpel or laparoscopic scissors. It is not recommended to use the electrocautery or another type of laser. Access to the lumen can be done either by the incision of the cystic duct in the long axis prolonged to the main bile duct until an access path of sufficient size is obtained or by the longitudinal incision on the anterior surface of the main bile duct (Figure 3 and Figure 4). Traction wires are not needed on the sides of the choledochotomy, which can start in the cystic duct and extend into the main bile duct. This technique inquires a more difficult closure by suture.
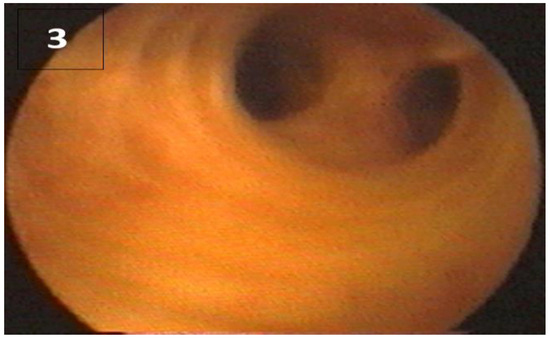
Figure 3.
Choledoscopy—(left and right main biliary ducts), proximal view.
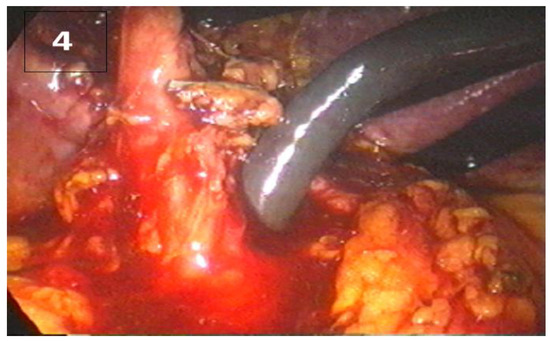
Figure 4.
Choledochotomy and cholangioscope.
Cholangioscopy via choledochotomy allows the complete exploration of the main biliary tract, the orientation starting from the retropancreatic segment with visualization of the papilla and then proximal, visualizing the upper biliary confluence, the right and left hepatic channels and the first segmental branches (Figure 3). The operation may continue with an endoscopic or instrumental clearing of the bile duct, or it can be converted to open surgery (Figure 5). If the procedure is finished via laparoscopy, an external biliary drainage type T-tube or transcystic (with choledocoraphy) can be left in place. If the local anatomy allows it, ideal choledocoraphy can be performed.
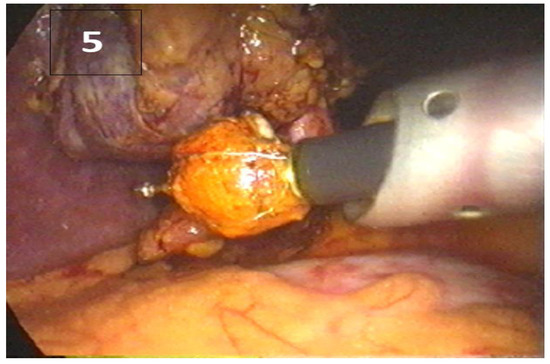
Figure 5.
Main bile duct stone extracted in a Dormia basket.
Special mention must be made in this paragraph about the possibility of undiagnosed choledochal diverticula which are not observed during exploration. Perforation of such a diverticulum, located retropancreatic or juxta-papillary, causes pancreatic or pancreaticoduodenal lesions, which lead to severe consequences if they are not immediately recognized and corrected intraoperatively.
The aspiration of saline solution used for irrigation has been reported in the literature in two cases. The accident can be avoided by shortening the exploration time and maintaining an intraoperative nasogastric tube. The possibility of exploration is conditioned only by the ratio between the dimensions of the main biliary tract and those of the instrument.
Results
The main preoperative diagnosis for patients undergoing laparoscopic cholecystectomy was chronic cholecystitis, n = 1184. A number of two patients were operated under the diagnosis of cholecysto-choledochial fistula. A number of 5 cases had gallbladder cancer diagnosed following the histopathological examination.
The patients hospitalized and operated under the diagnosis of acute cholecystitis were also the ones who had the most problems intraoperatively regarding the dissection of the hepatic pedicle due to the local inflammatory changes. Of great use in the situations mentioned above was laparoscopic ultrasound, which allowed the differentiation of anatomical structures without the need for prior dissection.

Table 1.
Patient distribution regarding the underlying disease.
Table 1.
Patient distribution regarding the underlying disease.
| Pathology | No. |
|---|---|
| Acute cholecystitis | 1184 |
| Chrnoic cholecystitis | 1281 |
| Scleroatrofic cholecystitis | 91 |
| Gallbladder tumor | 5 |
| Gallbladder bud | 6 |
| Biliary fistula | 2 |
Main bile duct stones were diagnosed preoperatively in a number of n = 46 patients (3.71%). The majority of these consisted of females, n = 32.
The exploration and diagnosis of the main bile duct are one of the major objectives of the surgeon who addresses the biliary tree in surgery.

Table 2.
Distribution of genders regarding the preoperative diagnosis of main bile duct stones.
Table 2.
Distribution of genders regarding the preoperative diagnosis of main bile duct stones.
| Preoperative diagnosis of main bile duct stones | Male | Female |
|---|---|---|
| Yes | 14 | 32 |
| No | 716 | 1793 |
| Total | 730 | 1825 |
Around 2%, n=49, of all the patients who had undergone cholecystectomy also received choledochoscopy. From these, in n=33 of the cases the choledoscope was inserted through a transcystic approach, while in n=16 the approach was through the choledochal duct.

Table 3.
Transcystic approach – gender distribution.
Table 3.
Transcystic approach – gender distribution.
| Transcystic approach | Male | Female |
|---|---|---|
| Yes | 9 | 24 |
| No | 721 | 1801 |
| Total | 730 | 1825 |
The transcystic (anatomical) approach of the main bile ducts was chosen in the majority of the explorations, n = 33 cases (67%).

Table 4.
Transcholedochal approach – gender distribution.
Table 4.
Transcholedochal approach – gender distribution.
| Transcholedochal | Male | Female |
|---|---|---|
| Yes | 6 | 10 |
| No | 724 | 1815 |
| Total | 730 | 1825 |
In the case of n = 16 (33%) patients, due to local anatomy (difficult implantation of the cystic duct, small size of the cystic duct < 3 mm, proximal location of stones above the cystic-hepatic junction or their size > 7 mm, which is the maximum diameter that could be obtained by dilation with a balloon) it was necessary to perform a choledochotomy. It was preferred to limit the use of the transcholedochal approach of the main bile duct due to postoperative complications such as biliary fistula or strictures.
Choledoscopy has proven to be very useful when using the trans-choledochal approach in exploring the left and right main bile ducts. This scan was performed in 2 patients for whom intraoperatively numerous choledochal stones with a diameter < 2 mm were identified and their upward migration into the intrahepatic bile ducts was suspected. The main hepatic ducts were found to be free in both cases.
Discussions
Laparoscopic choledochoscopy was developed to facilitate the performance of cholangiography. When used together, these two methods can increase the percentage of identified biliary duct stones [19,20].
During a laparoscopic cholecystectomy when bile duct stones are encountered, in most cases the patient is referred to an ERCP, while direct intraoperative laparoscopic exploration of the bile duct is avoided.
This attitude is due both to the increased operative time required to perform a choledoscopy and to the high complexity of this procedure [21].
Among the indications of laparoscopic cholangiofibroscopy we can mention the following: inconclusive results after regarding the state of the main bile duct after cholangiography or ultrasonography, endoluminal biopsy when bile duct tumors are suspected, luminal deobstruction by drilling (laser, ultrasound, diathermy) or instrumentation [22,23,24].
As demonstrated in our group, cholangiofibroscopy was performed on a number of 49 patients (2%) and the main biliary duct was completely freed of stones in 35 of them (71%). The average duration of the intervention was 120 min, but according to Gough et al. (depending on the complexity of the case) this can be extended up to 350 min [9].
Transcystic approach of the biliary tree is ideal but and was preferred in 33 (67%) cases, thus avoiding extensive dissection of the bile duct thus reducing the risk of iatrogenic ductal and vascular lesions [25].
To perform this approach, the cystic duct must accommodate the fiberscope, be stone-free, and implanted on the right side of the main bile duct.
Lyass and Phillips mention the following indications for a transcystic approach: stones with a diameter below 10 mm, under 9 stones in the choledoc, the existence of a choledochal tumor that causes lumen obstruction [10].
The transcholedochal approach of the biliary tract was practiced in 16 cases (33%). Among the indications for this approach, we mention the following: an non-dilated cystic duct, preoperative investigations that identified a large bile duct stone that could not be extracted through the cystic duct, as well as the need to explore the intrahepatic bile ducts (this last indication motivated the 2 of our transcholedochal approaches, and in both cases exploration of 2nd and 3rd order intrahepatic ramifications was achieved). In these cases, proximal migration of duct stones was suspected. The main contraindication of the transcholedochal approach is related to the diameter of the main bile duct, which must be at least 7 mm, otherwise it will not be possible to allow exploratory maneuvers and the size of the duct stones [26,27,28].
Various complications may occur during this procedure: hemorrhagic accidents (when the cystic duct is cut, when the colodeus is prepared for incision or because of mucosal rupture on exploration), mechanical accidents (cystic duct tears, rupture of the bile ducts walls, trauma of the papilla) [29,30].
Cholangiofibroscopy has been shown to be very useful in the management of patients with choledochal lithiasis in a single-stage surgical intervention without the need for a subsequent endoscopic sphincterotomy (ERCP) [31,32].
Thus, the additional costs were reduced without further increasing morbidity and mortality.
Limits. The study is retrospective and thus we could not verify and control how the data were entered and stored. The study is monocentric and can be biased to the respective center technique and indications. Also, the data was obtained from multiple surgeons with different learning curves which can alter the quality of the results.
Conclusions
Cholangiofibroscopy is a cost-effective method that allows the exploration of the biliary tree and resolves main bile duct lithiasis within the same laparoscopic intervention. The use of the transcystic approach is ideal but not always possible; the transcholedochal approach associates external or internal biliary drainage.
Whenever possible, where the necessary technique and a trained team exist, it is preferred to approach the main bile duct stones in the same laparoscopic intervention by cholangiofibroscopy.
Institutional Review Board Statement
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- Dimov, R.S.; Kantchev, R.I.; Boev, B.G.; et al. Laparoscopic exploration of bile ducts in patients with calculosis. Indications, methods and first results. Folia Med (Plovdiv). 2013, 55, 33–38. [Google Scholar] [CrossRef]
- Piñeres, G.; Yamakawa, T.; Kasugai, H.; et al. Common bile duct stones: Management strategies in the laparoscopic era. J Hepatobiliary Pancreat Surg. 1998, 5, 97–103. [Google Scholar] [CrossRef]
- Vindal, A.; Chander, J.; Lal, P.; Mahendra, B. Comparison between intraoperative cholangiography and choledochoscopy for ductal clearance in laparoscopic CBD exploration: A prospective randomized study. Surg Endosc. 2015, 29, 1030–1038. [Google Scholar] [CrossRef]
- Nassar, A.H.M.; Gough, V.; Ng, H.J.; et al. Utilization of Laparoscopic Choledochoscopy During Bile Duct Exploration and Evaluation of the Wiper Blade Maneuver for Transcystic Intrahepatic. Access Ann Surg. 2023, 277, e376–e383. [Google Scholar] [CrossRef]
- Fang, L.; Huang, J.; Zheng, H.; et al. Laparoscopic transcystic common bile duct exploration in patients with a nondilated common bile duct. Ann Palliat Med. 2021, 10, 12845–12856. [Google Scholar] [CrossRef]
- Carroll, B.J.; Fallas, M.J.; Phillips, E.H. Laparoscopic transcystic choledochoscopy. Surg Endosc. 1994, 8, 310–314. [Google Scholar] [CrossRef]
- Urbach, D.R.; Khajanchee, Y.S.; Jobe, B.A.; Standage, B.A.; Hansen, P.D.; Swanstrom, L.L. Cost-effective management of common bile duct stones: A decision analysis of the use of endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography, and laparoscopic bile duct exploration. Surg Endosc. 2001, 15, 4–13. [Google Scholar] [CrossRef]
- Kenny, R.; Richardson, J.; McGlone, E.R.; Reddy, M.; Khan, O.A. Laparoscopic common bile duct exploration versus pre or post-operative ERCP for common bile duct stones in patients undergoing cholecystectomy: Is there any difference? Int J Surg. 2014, 12, 989–993. [Google Scholar] [CrossRef]
- Gough, V.; Stephens, N.; Ahmed, Z.; Nassar, A.H. Intrahepatic choledochoscopy during trans-cystic common bile duct exploration; technique, feasibility and value. Surg Endosc. 2012, 26, 3190–3194. [Google Scholar] [CrossRef]
- Lyass, S.; Phillips, E.H. Laparoscopic transcystic duct common bile duct exploration. Surg Endosc 2006, 20 Suppl 2, S441–S445. [Google Scholar] [CrossRef]
- Carroll, B.J.; Phillips, E.H.; Daykhovsky, L.; et al. Laparoscopic choledochoscopy: An effective approach to the common duct. J Laparoendosc Surg. 1992, 2, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Bekheit, M.; Smith, R.; Ramsay, G.; Soggiu, F.; Ghazanfar, M.; Ahmed, I. Meta-analysis of laparoscopic transcystic versus transcholedochal common bile duct exploration for choledocholithiasis. BJS Open. 2019, 3, 242–251, Published 2019 Jan 23. [Google Scholar] [CrossRef]
- Bar-Meir, S.; Rotmensch, S. A comparison between peroral choledochoscopy and endoscopic retrograde cholangiopancreatography. Gastrointest Endosc. 1987, 33, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Kroh, M.; Chand, B. Choledocholithiasis, endoscopic retrograde cholangiopancreatography, and laparoscopic common bile duct exploration. Surg Clin North Am. 2008, 88, 1019–vii. [Google Scholar] [CrossRef]
- Phillips, E.H.; Carroll, B.J.; Pearlstein, A.R.; Daykhovsky, L.; Fallas, M.J. Laparoscopic choledochoscopy and extraction of common bile duct stones. World J Surg. 1993, 17, 22–28. [Google Scholar] [CrossRef]
- Campagnacci, R.; Baldoni, A.; Baldarelli, M.; et al. Is laparoscopic fiberoptic choledochoscopy for common bile duct stones a fine option or a mandatory step? Surg Endosc. 2010, 24, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N. Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J Gastrointest Surg. 2016, 8, 376–381. [Google Scholar] [CrossRef]
- Kelley, W.E., Jr.; Sheridan, V.C. Laparoscopic choledochoscopy with a small-caliber endoscope. A safe and effective technique for laparoscopic common bile duct exploration. Surg Endosc. 1995, 9, 293–296. [Google Scholar] [CrossRef]
- Topal, B.; Aerts, R.; Penninckx, F. Laparoscopic common bile duct stone clearance with flexible choledochoscopy. Surg Endosc. 2007, 21, 2317–2321. [Google Scholar] [CrossRef]
- Wang, H.; Lu, W.; Yang, G.; Zhu, J. Safety and feasibility analysis of combination therapy of laparoscopic left hepatectomy and choledochoscopy for calculus of the left intrahepatic duct. Minerva Chir. 2019, 74, 115–120. [Google Scholar] [CrossRef]
- Stoker, M.E.; Leveillee, R.J.; McCann, J.C., Jr.; Maini, B.S. Laparoscopic common bile duct exploration. J Laparoendosc Surg. 1991, 1, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Arregui, M.E.; Davis, C.J.; Arkush, A.M.; Nagan, R.F. Laparoscopic cholecystectomy combined with endoscopic sphincterotomy and stone extraction or laparoscopic choledochoscopy and electrohydraulic lithotripsy for management of cholelithiasis with choledocholithiasis. Surg Endosc. 1992, 6, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Sun, D.; Sun, Y.; Bai, J.; Zhao, H.; Miao, Y. Primary closure following laparoscopic common bile duct exploration combined with intraoperative cholangiography and choledochoscopy. World J Surg. 2012, 36, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Silaghi, A.; Socea, B.; Banu, P.; Baleanu, V.D.; Epistatu, D.; Paunica, I.; Constantin, V.D. Acute lithiasis cholecystitis; particularities of diagnosis and treatment in the elderly. J Mind Med Sci. 2023, 10, 121–130. [Google Scholar] [CrossRef]
- Yuan, H.; Dong, G.; Zhang, N.; Sun, X.; Zhao, H. Minimally invasive strategy for type I choledochal cyst in adult: Combination of laparoscopy and choledochoscopy. Surg Endosc. 2021, 35, 1093–1100. [Google Scholar] [CrossRef]
- Platt, T.E.; Smith, K.; Sinha, S.; et al. Laparoscopic common bile duct exploration; a preferential pathway for elderly patients. Ann Med Surg (Lond). 2018, 30, 13–17. [Google Scholar] [CrossRef]
- Navaratne, L.; Martinez Isla, A. Transductal versus transcystic laparoscopic common bile duct exploration: An institutional review of over four hundred cases. Surg Endosc. 2021, 35, 437–448. [Google Scholar] [CrossRef]
- Giacometti, M.; Battafarano, F.; Geraci, O.; Zonta, S. Laparoscopic trans-cystic common bile duct exploration and treatment of choledocholithiasis in a patient with Roux-en-Y reconstruction after gastrectomy: Report of an emergency case. J Surg Case Rep. 2021, 2021, rjab144. [Google Scholar] [CrossRef]
- Giurgiu, D.I.; Margulies, D.R.; Carroll, B.J.; et al. Laparoscopic common bile duct exploration: Long-term outcome. Arch Surg. 1999, 134, 839–844. [Google Scholar] [CrossRef]
- Smith, P.C.; Clayman, R.V.; Soper, N.J. Laparoscopic cholecystectomy and choledochoscopy for the treatment of cholelithiasis and choledocholithiasis. Surgery. 1992, 111, 230–233. [Google Scholar]
- Zhu, Y.; Li, J.; Xie, M.; Jin, J.; Lou, J. Clinical application of laparoscopy combined with choledochoscopy in patients with bilioenteric anastomotic stricture with access via the jejunal loops. J Int Med Res. 2021, 49, 3000605211034542. [Google Scholar] [CrossRef] [PubMed]
- Tokumura, H.; Umezawa, A.; Cao, H.; et al. Laparoscopic management of common bile duct stones: Transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg. 2002, 9, 206–212. [Google Scholar] [CrossRef] [PubMed]
© 2024 by the authors. 2024 Iulian Slavu, Raluca Tulin, Ileana Dima, Alexandru Dogaru, Florin Filipoiu, Bogdan Socea, Anca Monica Oprescu-Macovei, Adrian Tulin.