Abstract
Myelolipomas are described as small tumors, with some authors referring to sizes less than 4 cm in diameter. However, when greater than 10 cm, myelolipomas are labeled as giant tumors and thus, have a definite indication for surgical resection. Myelolipomas represent a small percentage of adrenal tumors. Giant myelolipomas are usually discovered incidentally during imaging studies performed for other conditions. They are often slow-growing and may reach sizes that significantly distort the anatomy of the affected area. Despite their large size, they are usually benign and do not spread to other parts of the body. Adrenal myelolipoma is a benign tumor with a scarce number of detailed cases reported in literature. It is frequently discovered by chance, covering a variety of differential diagnoses. Imaging techniques and histopathological examinations are of great importance in the differential diagnosis of adrenal gland lesions, including retroperitoneal lipoma and liposarcoma, adrenal myelolipoma, adrenal lymphoma, adrenal adenoma, adrenocortical carcinoma, pheochromocytoma or metastasis. We performed a comprehensive review on PubMed of all cases of giant adrenal myelolipoma reported in literature with more than 10 cm in diameter, in order to estimate the incidence, diagnosis and treatment of giant myelolipoma. So far, only 15 cases of truly giant adrenal myelolipoma have been reported between 1981 and 2023.
Introduction
Adrenal myelolipoma is a benign, generally unilateral tumor, composed of mature adipose and hematopoietic tissue. They typically occur in the adrenal gland and can grow to significant sizes, sometimes weighing several kilograms [1].
This type of tumors was described for the first time in 1905 by Gierke. In 1929, Oberling named this type of tumors “myelolipomas” because of its histological components: cortico-adrenal tissue, adipose tissue and multiple hematopoietic sites [2,3]. Literature review reports 420 cases between 1957-2017, with very few references on a comprehensive analysis of this incidentaloma [4].
Myelolipomas are described as small tumors, with some authors referring to sizes less than 4 cm in diameter, and others to 7 cm. However, when greater than 10 cm, myelolipomas are labeled as giant tumors and thus, have a solid indication for surgical resection. The largest myelolipoma reported so far was 31 cm x 24.5 cm x 11.5 cm, and weighted 6 kg. Most of cases reported in literature are small non-symptomatic myelolipoma, not bigger than 10 cm in diameter [5,6]. Because the lack of symptoms, most of these tumors are incidentally detected. Adrenal myelolipoma is commonly found between the fifth and seventh decades [7].
The etiology of this type of tumor is not completely understood, however, several theories have been advanced. One of the most credited, cited by Meaglia and Schmidt, embraces the metaplasia of the reticuloendothelial cells in the adrenal capillaries in response to necrosis, infection, stress or long-term ACTH stimulation, as potential factors [8,9].
Due to their size and potential for symptoms, surgical removal is often recommended. The surgery can be challenging due to the tumor's large size and its proximity to important structures like the kidneys, blood vessels, and other organs. However, with advancements in surgical techniques and preoperative imaging, successful removal is achievable in most cases [9,10].
The aim of this study has been to review all cases of giant adrenal myelolipoma reported in literature with more than 10 cm in diameter, in order to estimate the incidence of giant myelolipoma. Only few cases of truly giant adrenal myelolipoma (>10 cm diameter) have been reported.
We performed a systematic review of all giant myelolipoma reported on PubMed between 1981-2023 and we found 15 cases of giant myelolipoma (>10 cm diameter), including one patient with giant myelolipoma found in on the surgery department of Brasov Emergency Clinical County Hospital (female, 53 years old). The female to male ratio of the 15 cases was 1.5:1 and the age range was between 26 to 72 years, with an average of 53 years.
Discussions
The real incidence of adrenal myelolipomas remains unknown. Prior to the widespread use of imaging techniques, the incidence was cited below 1%, mostly based on autopsy reports. Later studies, based on imaging techniques revealed a higher level, between 10-15% [11].
Furthermore, the type of imaging technique employed, has greatly influenced the diagnosis of this pathology. Moreover, their use is strongly intertwined. Ultrasound can differentiate between renal and adrenal tissue. A CT description of a well circumscribed round or elliptical hypodense, heterogenous mass is highly suggestive for a myelolipoma, while structural components can be better described based on MRI, with the latter being more expensive and time consuming. Because of the wide use of such diagnostic imaging methods, with CT being the most widespread technique to examine the adrenal glands, these tumors can be discovered incidentally, during routine checkups. Additional methods of distinguishing myelolipoma from other entities include the use of Tc- albumin nanocolloid scintigraphy [12,13].
The hyperechoic mass detected by US and the hypodense, heterogenous retroperitoneal mass detected on abdominal CT were highly suggestive for myelolipoma, that usually presents with density <0 HU on non-contrast CT, due to its lipid content. In comparison, adrenocortical adenomas are typically smaller in size, well defined and homogenous in attenuation, with a density between 10-30 HU. Adrenal metastasis, adrenocortical carcinomas, pheochromocytomas and lymphomas usually have densities greater than 10 HU. This diagnosis was later confirmed by the histopathological examination [14,15].
There are no general patterns in terms of a patient profile for myelolipomas. Literature review cites no gender prevalence and a growth rate <0.2 cm/year. It is difficult to estimate the actual growth rate in our patient because the lack of previous imaging studies. Literature review reports that tumor growth > 1 cm is associated with larger myelolipoma and hemorrhagic changes [16,17].
Adrenal myelolipoma is commonly found between the fifth and seventh decades, as in our patient. The indication for surgical resection is based on volume, compression, risk of rupture and hemorrhage. Thus, each patient must be individually assessed, especially since they can coexist with other endocrine or hematological disorders [18,19].
Although usually unilateral, when bilateral, the left myelolipomas tend to be greater than the ones on the right side, mainly due to anatomical space limitations [20,21]. When unilateral, literature review cites a greater incidence of right sided myelolipomas compared to left, as outlined in this patient’s case [2].
Myelolipomas are usually found in the adrenal gland, although pleural, lung, mediastinum, thoracic spine, iliac fossa, hepatic, splenic and, more often, presacral sites have also been cited in literature. This tumor is predominantly asymptomatic, but depending on the size, patients can experience abdominal or low back pain due to compression, or rupture with hemorrhagic shock [22]. Thus, imaging techniques are paramount for the diagnosis and follow-up of myelolipomas. Adrenal myelolipomas are generally non-functioning tumors. However, literature review reports 25 cases of hormone secreting myelolipomas. These tumors are described as intra or extra glandular. Following surgical removal such tumors generally do not reoccur [21].
An association between insulin resistance and adrenal incidentalomas has been established. However, the pathophysiological link between these two conditions remains incompletely characterized. Insulin resistance, hyperinsulinemia, and the anabolic effects on adrenal gland tissue, which have insulin and insulin-like growth factor-1 receptors, offer possible pathophysiological links [23].
People with benign adrenal tumors are at higher risk for type 2 diabetes and high blood pressure than previously understood, according to new research from the University of Birmingham in the U.K. A, Mild autonomous cortisol secretion (MACS) is a regularly diagnosed cardiometabolic risk condition which predominantly affects women and warrants regular assessment for hypertension and type 2 diabetes [24]. In this context, it is more than explainable why diabetes induced by adrenal tumor activity can cause hypertension by affecting the peripheral arterial system [25].
Although CT and MRI examinations have been described as being a very sensitive, histopathological evaluation is compulsory for a definitive diagnosis [26].
Diagnostic and surgical management
Similar to most myelolipomas cases, the main symptoms for which our patient presented to the hospital was moderate abdominal pain and discomfort, without any other significant ones. Also, our patient presented intermittent, non-radiating right upper quadrant dull pain, 5/10 in intensity, with occasional nausea and vomiting, without associated weight or appetite changes. The vital signs were within normal range and the patient was in no acute distress, presenting a soft distended abdomen, right upper quadrant tenderness without rebound or guarding and a large palpable tumor in the right abdomen [27,28].
All patients included in the study had a non-related medical history such as hypertension (only 6 patients) and type 2 diabetes (only 3 patients). Our patient medical history included stage 3 hypertension (diagnosed 7 years earlier), type 2 diabetes (diagnosed 8 years earlier) and chronic cholecystitis with lithiasis. Surgical history included traumatic leg amputations 2 years prior.
The specific literature noted that for all the cases the main imagistic investigation was the contrast enhanced computed tomography (CT) scan, ultrasonography (US), and additionally Magnetic Resonance (MRI) being performed only in 2 cases [26].
Related to the diagnostic procedures, in 11 cases of myelolipoma, the CT scan revealed a right suprarenal mass in contact with the right hepatic lobe, inferior vena cava and dislodging the right kidney. In the other 4 cases the mass was situated in the left suprarenal gland. All studied patients had tumors with the maximum diameter greater than 10 cm. The maximum diameter varied between 10-31 cm [29,30].
In our patient, the CT scan demonstrated a 25 cm x 17 cm x 21 cm well-delimitated, heterogenic, non-iodophil retroperitoneal tumor (Figure 1) in close contact with the right hepatic lobe, inferior vena cava, ascendant and transverse colon. The right kidney was medially and inferiorly displaced by the tumor volume (approx. 0,9 dm3).
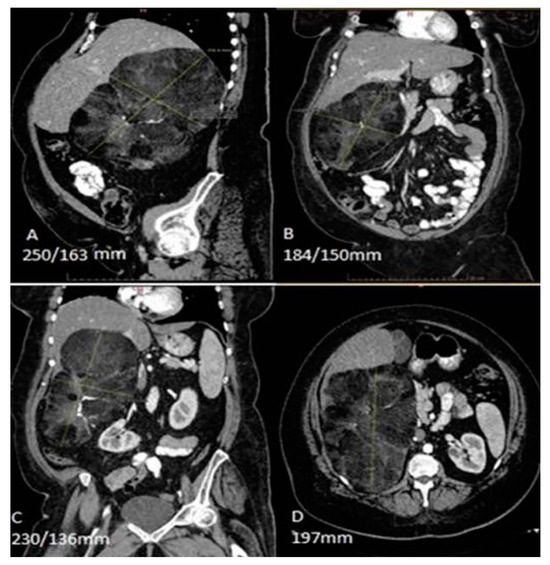
Figure 1.
Abdominal computed tomography scan demonstrating a 25 cm x 17 cm x 21 cm, mass in close contact with the right hepatic lobe, the inferior vena cava, the ascendant and transverse colon, and the diaphragm, and a medially and inferiorly displaced right kidney.
Because the CT investigation was sufficient for a comprehensive diagnosis, an additional MRI scan was not performed. All routine laboratory workup, including hormonal assessment, were within normal range, except a mild inflammatory syndrome (ESR: 26 mm/h) and hyperglycemia (Glucose: 126 mg/dl).
It is well known that CT and MRI imaging techniques are of paramount importance in the differential diagnosis, yet US and nuclear medicine tests are commonly used for adrenal lesion assessment. Diagnosis confirmation requires histopathological examination. Depending on their biological behavior, adrenal gland lesions can be classified into malignant or benign. Incidentally discovered, adrenocortical adenoma is the most common lesion of the adrenal gland. It presents as a small, solid, well-defined lesion with hemorrhagic or cystic changes. Pheochromocytoma is typically larger than adenoma and usually symptomatic, presenting with new onset secondary malignant hypertension, flushing, hypermetabolism, hyperglycemia, hyperhidrosis, headache and palpitations. Adrenocortical carcinomas are typically large masses, with early detection due to their hormonally functional behavior such as Cushing syndrome, primary aldosteronism or abnormal sexuality. Primary or secondary adrenal lymphomas are large, malignant homogenous lesions presenting with adrenal insufficiency, fever, weight loss, night sweats [14,29,30,31].
The surgical intervention was planned based on tumor size and compression, given the risk of a spontaneous retroperitoneal hemorrhage following a potential tumor rupture and the proximity to the inferior vena cava. The CT scan revealed predominantly fatty regions interspersed with areas of higher attenuation. The tissue density varied between -70 Hounsfield (HU) and -30 HU.
Because in the surgical hospital departments wound infection is one of the most common and dreaded complications, the colonization and contamination of the patient’ skin was controlled from the first moment. In this context, knowing the bacteriological status at admission ensures the distinction between the colonization and infection processes and could help to manage in an efficient way the fight against bacterial pathogen infections from the beginning [32].
Also, since the patient was admitted to hospital during the COVID-19 pandemic, an additional screening for SARS- CoV-2 infection was performed to prevent future complications, predictable in such an epidemiological context and knowing the pathologic conditions of the patient, represented by hypertension and type 2 diabetes [33].
The preferred surgical approach in most cases was open surgery [14], only one case was resolved by laparoscopic approach. In 12 cases, a medial subxiphoid-suprapubic incision was performed, and in 2 cases a Kocher incision was preferred. In our case a medial subxiphoid-pubic incision was performed (Figure 2).
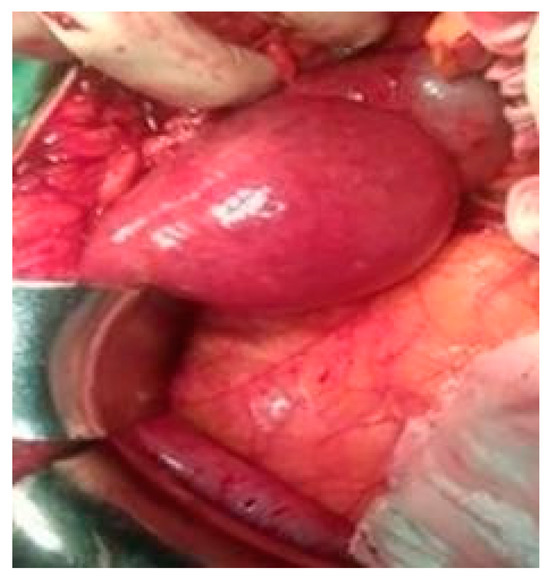
Figure 2.
Intraoperative view of the tumor.
The surgical approach also included a retrograde cholecystectomy. The mass was dissected from the upper pole of the right kidney, the right hepatic lobe and the inferior vena cava. Gross examination revealed a thin encapsulated mass with firm, mixed consistency (Figure 3).
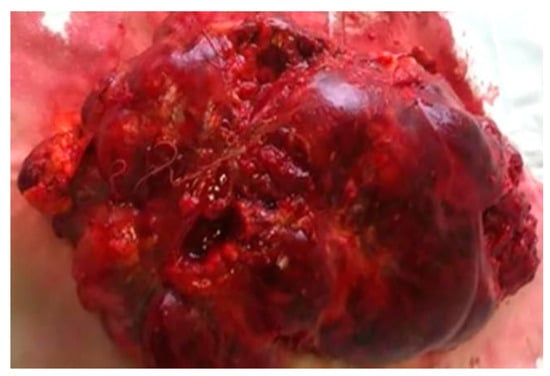
Figure 3.
Macroscopic structure of the specimen, presenting a thin capsule.
The microscopic examination revealed in all cases cortico-adrenal and adipose tissue and multiple hematopoietic sites (Figure 4). The histological examination concluded adrenal myelolipoma. Also, the microscopic tumor examination of our patient revealed the same elements.
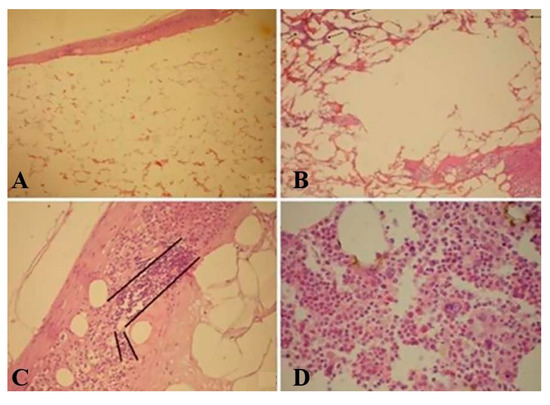
Figure 4.
Microscopic view; Hematoxylin and eosin stain of the resected tissue. A: Overview of the tumor (magnification x4). Mature adipose tissue, many capillaries and cortico-adrenal gland capsule. B: Overview (magnification x10): Mature adipose tissue and many hematopoietic sites. C: Detail (magnification x20): Hematopoietic site under the corticoadrenal capsule. D: Detail (magnification x40): Hematopoietic tissue with all blood forming cells.
All reported patients had an uneventful hospitalization with full recovery.
Conclusions
Despite their benign biology, these tumors are difficult to diagnose as a result of a low threshold of suspicion. Our patient matched the literature suggested profile between the fifth and seventh decades of life, right side, well circumscribed hypodense, heterogenous, <0 HU, retroperitoneal mass, with nonspecific signs and symptoms [34,35].
The differential diagnosis should include retroperitoneal lipoma and liposarcoma, pheochromocytoma, adrenal lymphoma, adrenal adenoma and adrenocortical carcinoma, as well as metastasis and even mass-forming extramedullary hematopoiesis in patients with hematologic disorders [29,30].
Advancements in medical imaging technology and increased awareness among healthcare providers may contribute to more accurate diagnosis and reporting of these rare tumors in the future. Collaborative efforts among medical professionals and researchers worldwide are essential for further understanding and addressing the challenges associated with giant myelolipomas [35,36].
Surgery for giant myelolipomas can be challenging due to their size and location, but with appropriate preoperative planning and surgical expertise, favorable outcomes can be achieved in many cases [10,37].
Compliance with Ethical Standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript. Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- Alvarez, J.F.; Goldstein, L.; Samreen, N.; Beegle, R.; Carter, C.; Shaw, A.; Ben-David, K. Giant adrenal myelolipoma. J Gastrointest Surg. 2014, 18, 1716–1718. [Google Scholar] [CrossRef]
- Gautam, S.; Raafat, H.; Sriganesh, S.; Zaffar, I.; Olude, I.; Komolafe, F.; Qazi, F. Giant adrenal myelolipoma. Qatar Med J. 2013, 2013, 7–11, Published 2013 Nov 1. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mhammedi, W.A.; Ouslim, H.; Ouraghi, A.; Irzi, M.; Elhoumaidi, A.; Chennoufi, M.; Mokhtari, M.; Elmouden, A.; Barki, A. Adrenal myelolipoma: From tumorigenesis to management. Pan Afr Med J. 2019, 34, 180, Published 2019 Dec 5. [Google Scholar] [CrossRef] [PubMed]
- Nikumbh, D.B.; Kshirsagar, A.Y.; Desai, S.R.; Shrigondekar, P.A.; Mali, R.K.; Wader, J.V. Giant adrenal myelolipoma. The American Journal of Case Reports. 2011, 12, 83–86. [Google Scholar] [CrossRef]
- Fernandes, G.C.; Gupta, R.K.; Kandalkar, B.M. Giant adrenal myelolipoma. Indian J Pathol Microbiol. 2010, 53, 325–326. [Google Scholar] [CrossRef]
- Akamatsu, H.; Koseki, M.; Nakaba, H.; Sunada, S.; Ito, A.; Teramoto, S.; Miyata, M. Giant adrenal myelolipoma: Report of a case. Surg Today. 2004, 34, 283–285. [Google Scholar] [CrossRef]
- Adapa, S.; Naramala, S.; Gayam, V.; Gavini, F.; Dhingra, H.; Hazard, F.K.G.; Aeddula, N.R.; Konala, V.M. Adrenal Incidentaloma: Challenges in Diagnosing Adrenal Myelolipoma. J Investig Med High Impact Case Rep. 2019, 7, 2324709619870311. [Google Scholar] [CrossRef]
- Répássy, D.L.; Csata, S.; Sterlik, G.; Iványi, A. Giant adrenal myelolipoma. Pathol Oncol Res. 2001, 7, 72–73. [Google Scholar] [CrossRef]
- Rafiq, B.; El Mghari, G. Myélolipome de la surrénale: À propos d’un cas [Adrenal myelolipoma: About a case]. Pan Afr Med J. 2017, 28, 153. [Google Scholar] [CrossRef]
- Daneshmand, S.; Quek, M.L. Adrenal myelolipoma: Diagnosis and management. Urol, J. 2006, 3, 71–74. [Google Scholar]
- D’Addosio, R.; Rojas, J.; Bermúdez, V.; Ledesma, F.; Hoedebecke, K. Case Report: An incidentaloma that catches your eye—Adrenal myelolipoma. F1000Res. 2017, 6, 1140, Published 2017 Jul 18. [Google Scholar] [CrossRef] [PubMed]
- Guillaume, L.; Borght, T.V.; Bertrand, C.; Dupont, M.; Krug, B. Presacral Myelolipoma: The Usefulness of a 99mTc-Albumin Nanocolloid Scintigraphy. Clin Nucl Med. 2021, 46, 38–39. [Google Scholar] [CrossRef]
- Yildiz, L.; Akpolat, I.; Erzurumlu, K.; Aydin, O.; Kandemir, B. Giant adrenal myelolipoma: Case report and review of the literature. Pathol Int. 2000, 50, 502–504. [Google Scholar] [CrossRef] [PubMed]
- Xin, H.; Li, H.; Yu, H.; Zhang, J.; Peng, W.; Peng, D. MR imaging to detect myelolipomas of the liver: A case report and literature review. Medicine 2019, 98, e16497. [Google Scholar] [CrossRef]
- Brogna, A.; Scalisi, G.; Ferrara, R.; Bucceri, A.M. Giant secreting adrenal myelolipoma in a man: A case report. J Med Case Rep. 2011, 5, 298, Published 2011 Jul 9. [Google Scholar] [CrossRef] [PubMed]
- Rahoui, M.; Ouanes, Y.; Chaker, K.; Dali, K.M.; Bibi, M.; Sellami, A.; Ben Rhouma, S.; Nouira, Y. Giant adrenal myelolipoma in a young female patient: A case report. J Surg Case Rep. 2022, 2022, rjac213. [Google Scholar] [CrossRef]
- Lamont, J.P.; Lieberman, Z.H.; Stephens, J.S. Giant adrenal myelolipoma. Am Surg. 2002, 68, 392–394. [Google Scholar] [CrossRef]
- Şavlovschi, C.; Comandaşu, M.; Şerban, D. Particularities of Diagnosis and Treatment in Synchronous Colorectal Cancers (SCC). Chirurgia 2013, 108, 43–45. [Google Scholar]
- Hamidi, O.; Raman, R.; Lazik, N.; Iniguez-Ariza, N.; McKenzie, T.J.; Lyden, M.L.; Thompson, G.B.; Dy, B.M.; Young, W.F.; Bancos, I. Clinical course of adrenal myelolipoma: A long-term longitudinal follow-up study. Clin Endocrinol 2020, 93, 11–18. [Google Scholar] [CrossRef]
- Ramesh, R.; Roger, B.; Dhali, A.; Dsouza, C. Giant Bilateral Adrenal Myelolipoma: Case Report. Indian J Endocrinol Metab. 2020, 24, 551–553. [Google Scholar] [CrossRef]
- Gupta, S.S.; Kupfer, Y. Giant Bilateral Adrenal Myelolipoma. Balkan Med, J. 2017, 34, 476–477. [Google Scholar] [CrossRef] [PubMed]
- Nitz, J.A.; Huckleby, J.; Hwang, E.H.; Medina, M.G.; Pera, S.J.; Orcutt, S.T. Symptomatic Extra-Adrenal Myelolipoma in the Spleen. Case Rep Surg. 2020, 2020, 8839178. [Google Scholar] [CrossRef] [PubMed]
- Higgs, J.A.; Quinn, A.P.; Seely, K.D.; Richards, Z.; Mortensen, S.P.; Crandall, C.S.; Brooks, A.E. Pathophysiological Link between Insulin Resistance and Adrenal Incidentalomas. Int J Mol Sci. 2022, 23, 4340, Published 2022 Apr 14. [Google Scholar] [CrossRef]
- Prete, A.; Subramanian, A.; Bancos, I.; Chortis, V.; Tsagarakis, S.; Lang, K.; Macech, M.; Delivanis, D.A.; Pupovac, I.D.; Reimondo, G.; et al. Cardiometabolic Disease Burden and Steroid Excretion in Benign Adrenal Tumors: A Cross- Sectional Multicenter Study. Ann Intern Med. 2022, 175, 325–334. [Google Scholar] [CrossRef]
- Toader, S.; Pavel, O.; Barsan, S.; Olariu, R.; Grigorescu, D.O.; Penciu, M.; Nagy, A.L.; Georgescu, A.V.; Baldea, B.I. The influence of diabetes mellitus on survival of abdominal perforator flaps: An experimental study in rats with slowly induced diabetes mellitus. J Reconstr Microsurg. 2015, 31, 145–153. [Google Scholar] [CrossRef][Green Version]
- Wang, F.; Liu, J.; Zhang, R.; Bai, Y.; Li, C.; Li, B.; Liu, H.; Zhang, T. CT and MRI of adrenal gland pathologies. Quant Imaging Med Surg. 2018, 8, 853–875. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.H.; Mandaliya, R.; Liang, J.; Patel, M. A case report of symptomatic presacral myelolipoma. Medicine 2018, 97, e0337. [Google Scholar] [CrossRef]
- Ramdani, A.; Aissaoui, A.; Bouhout, T.; Bennani, A.; Latrech, H.; Serji, B.; El Harroudi, T. Giant symptomatic adrenal myelolipoma: A case report. Ann Med Surg 2022, 75, 103333, Published 2022 Feb 9. [Google Scholar] [CrossRef]
- Cho, J.; Kinsey, D.; Kimchi, E.T.; O'Carroll, K.S.; Nguyen, V.; Alsabbagh, M.; Gaballah, A. Retroperitoneal extra-adrenal myelolipoma misdiagnosed as liposarcoma: A case report. Radiol Case Rep. 2020, 16, 364–368. [Google Scholar] [CrossRef]
- Reginelli, A.; Vacca, G.; Belfiore, M.; Sangiovanni, A.; Nardone, V.; Vanzulli, A.; Grassi, R.; Cappabianca, S. Pitfalls and differential diagnosis on adrenal lesions: Current concepts in CT/MR imaging: A narrative review. Gland Surg. 2020, 9, 2331–2342. [Google Scholar] [CrossRef]
- Jun, J.H.; Ahn, H.J.; Lee, S.M.; Kim, J.A.; Park, B.K.; Kim, J.S.; Kim, J.H. Is Preoperative Biochemical Testing for Pheochromocytoma Necessary for All Adrenal Incidentalomas? Medicine 2015, 94, e1948. [Google Scholar] [CrossRef] [PubMed]
- Mateescu, M.-C.; Grigorescu, S.; Socea, B.; Bloanca, V.; Grigorescu, O.-D. Contribution to the Personalized Management of the Nosocomial Infections: A New Paradigm Regarding the Influence of the Community Microbial Environment on the Incidence of the Healthcare-Associated Infections (HAI) in Emergency Hospital Surgical Departments. J Pers Med. 2023, 13, 210, Published 2023 Jan 25. [Google Scholar] [CrossRef]
- Grigorescu, S.; Cazan, A.-M.; Rogozea, L.; Grigorescu, D.O. Predictive Factors of the Burnout Syndrome Occurrence in the Healthcare Workers During the COVID-19 Pandemic. Front. Med. 2022, 9, 842457. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.J.; Obasi, M.; Wu, B.; Corwin, M.T.; Fananapazir, G. The radiographically diagnosed adrenal myelolipoma: What do we really know? Endocrine 2017, 58, 289–294. [Google Scholar] [CrossRef]
- Allison, K.H.; Mann, G.N.; Norwood, T.H.; Rubin, B.P. An unusual case of multiple giant myelolipomas: Clinical and pathogenetic implications. Endocr Pathol. 2003, 14, 93–100. [Google Scholar] [CrossRef]
- Doddi, S.; Singhal, T.; Leake, T.; Sinha, P. Management of an incidentally found large adrenal myelolipoma: A case report. Cases J. 2009, 2, 8414, Published 2009 Sep 3. [Google Scholar] [CrossRef]
- Decmann, Á.; Perge, P.; Tóth, M.; Igaz, P. Adrenal myelolipoma: A comprehensive review. Endocrine. 2018, 59, 7–15. [Google Scholar] [CrossRef]
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).