Obesity in Children: Systematic Review over a 6-Year Period, Including the COVID-19 Pandemic
Abstract
Introduction
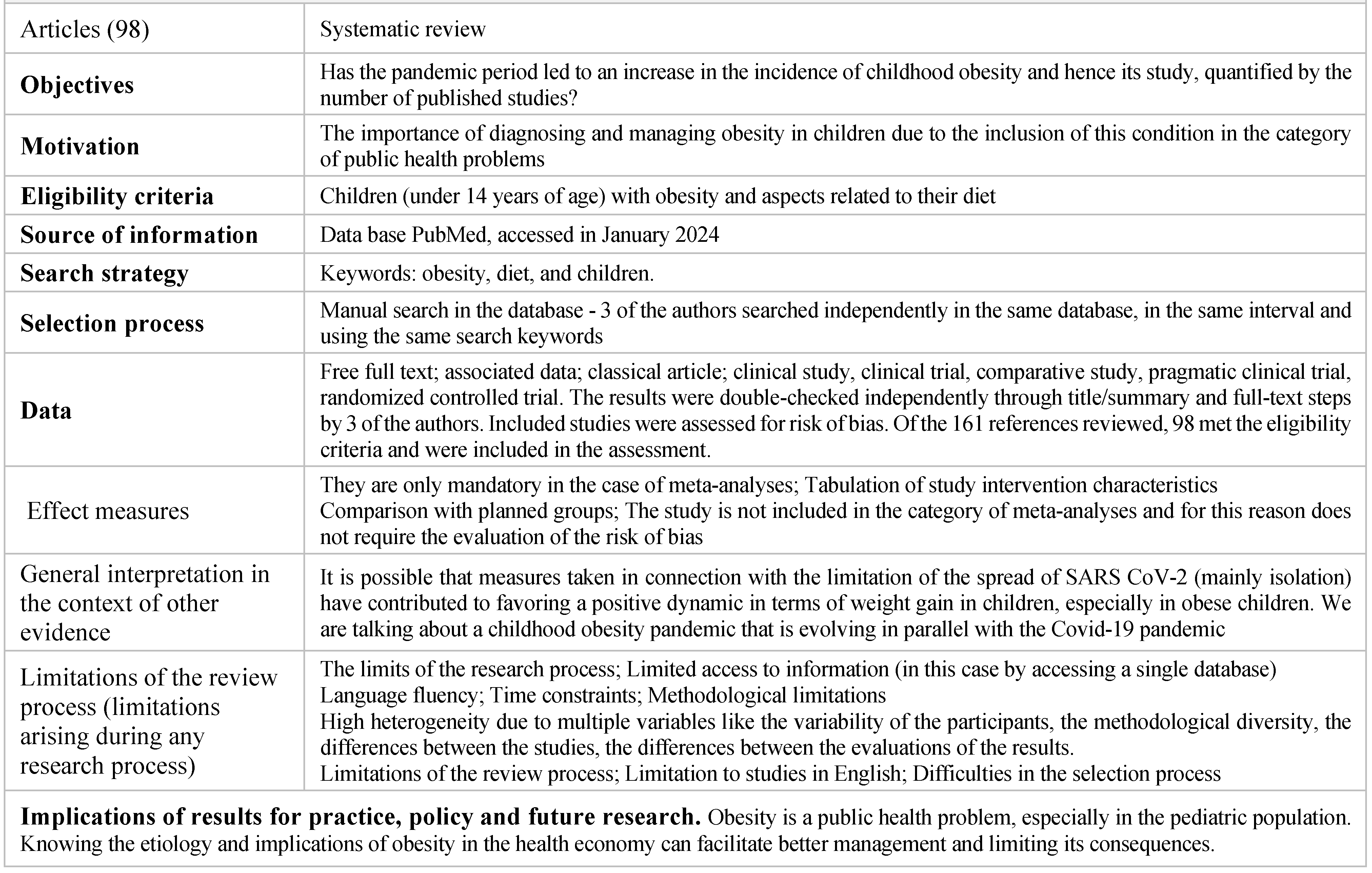
Materials and Methods
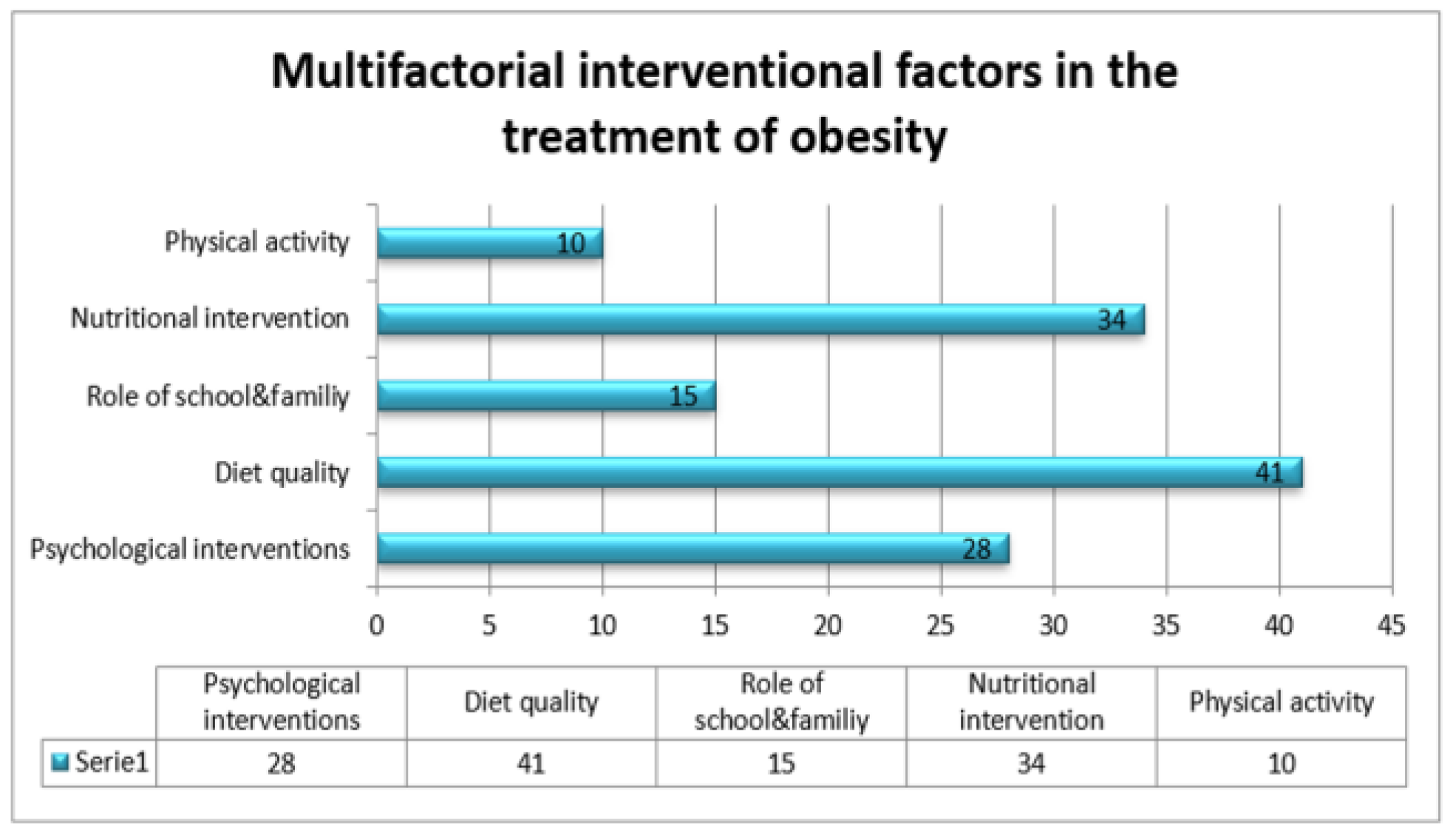
Results
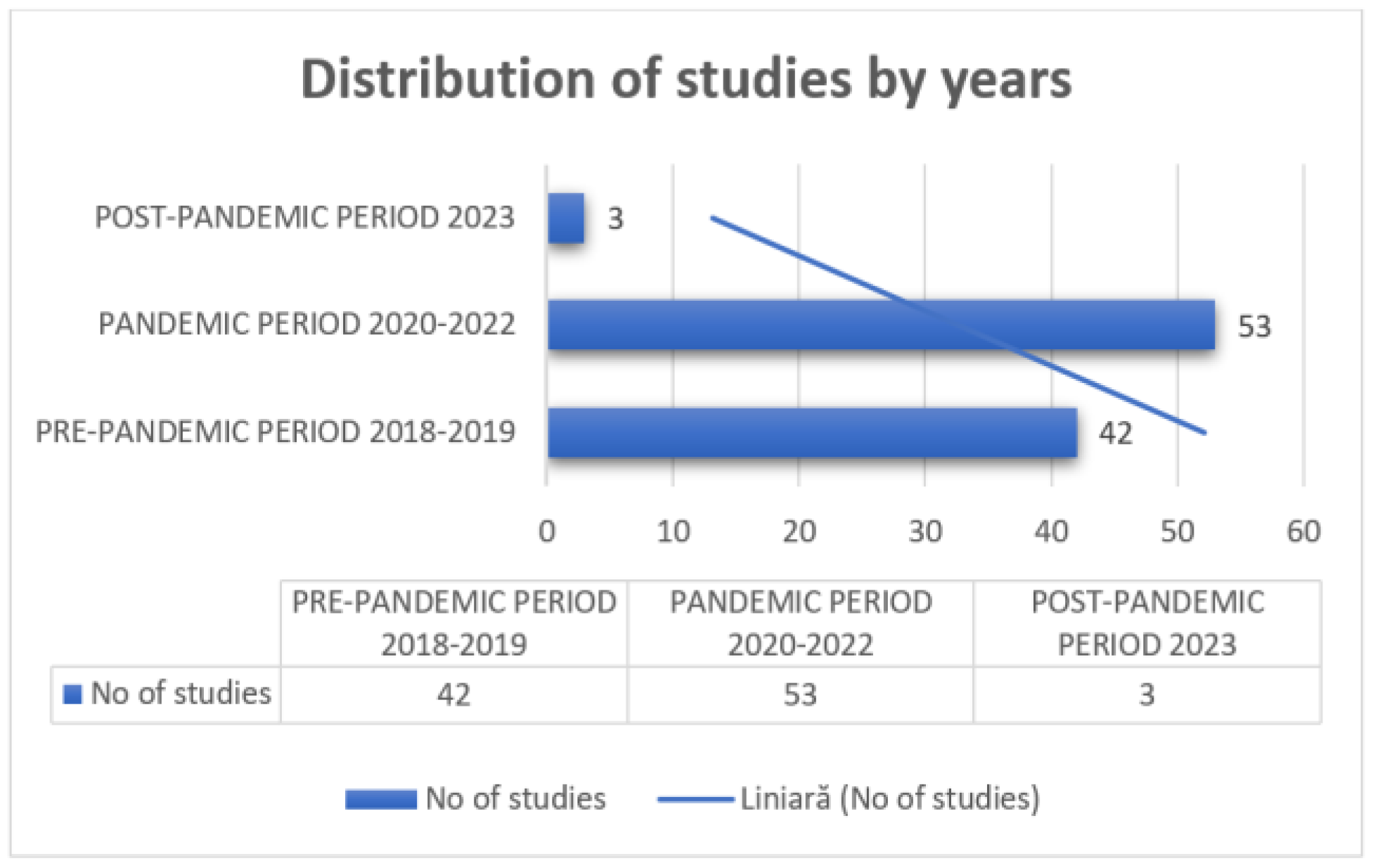
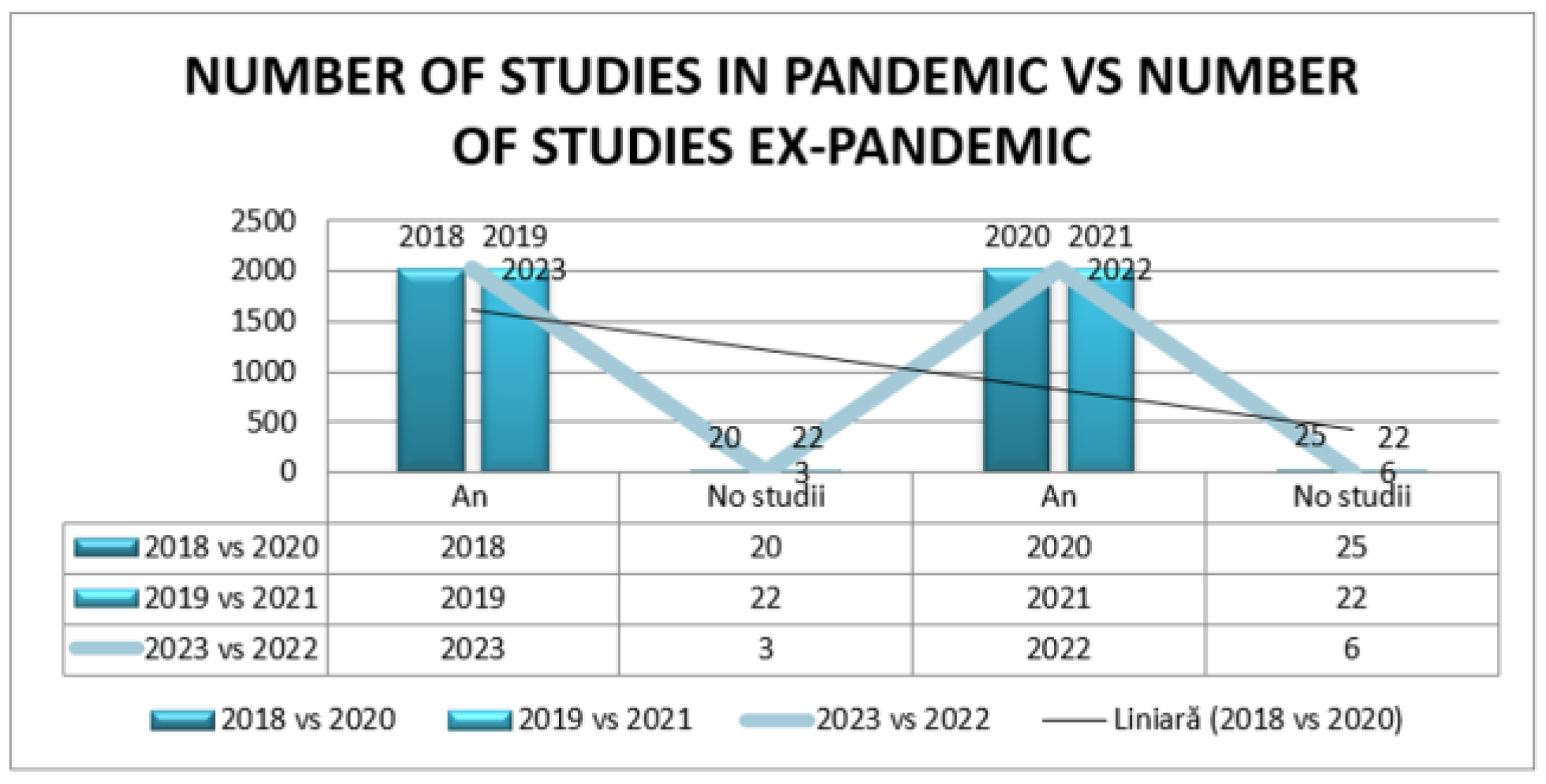
Systematic review of distribution of studies
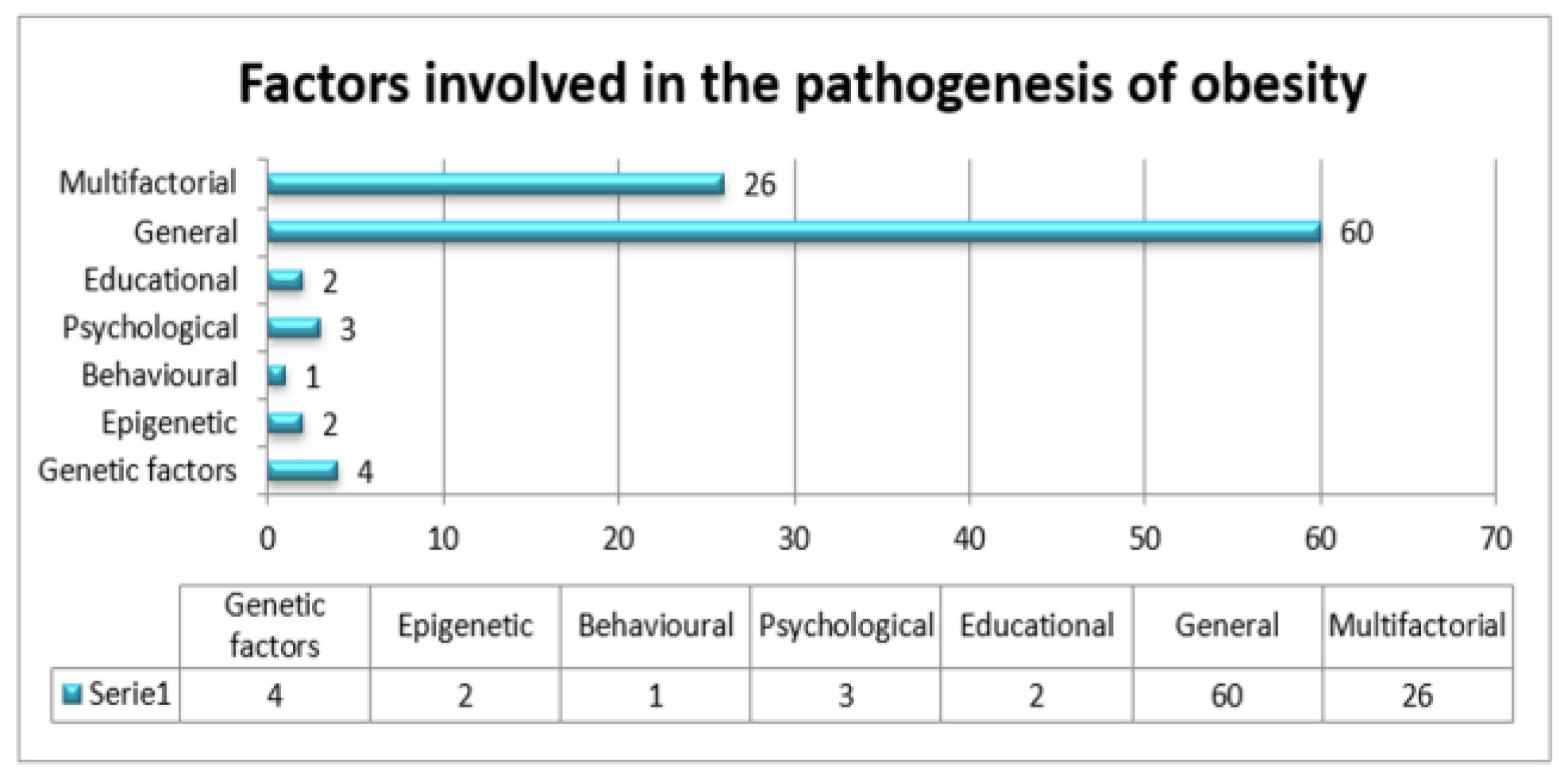
Factors involved in the pathogenesis of obesity
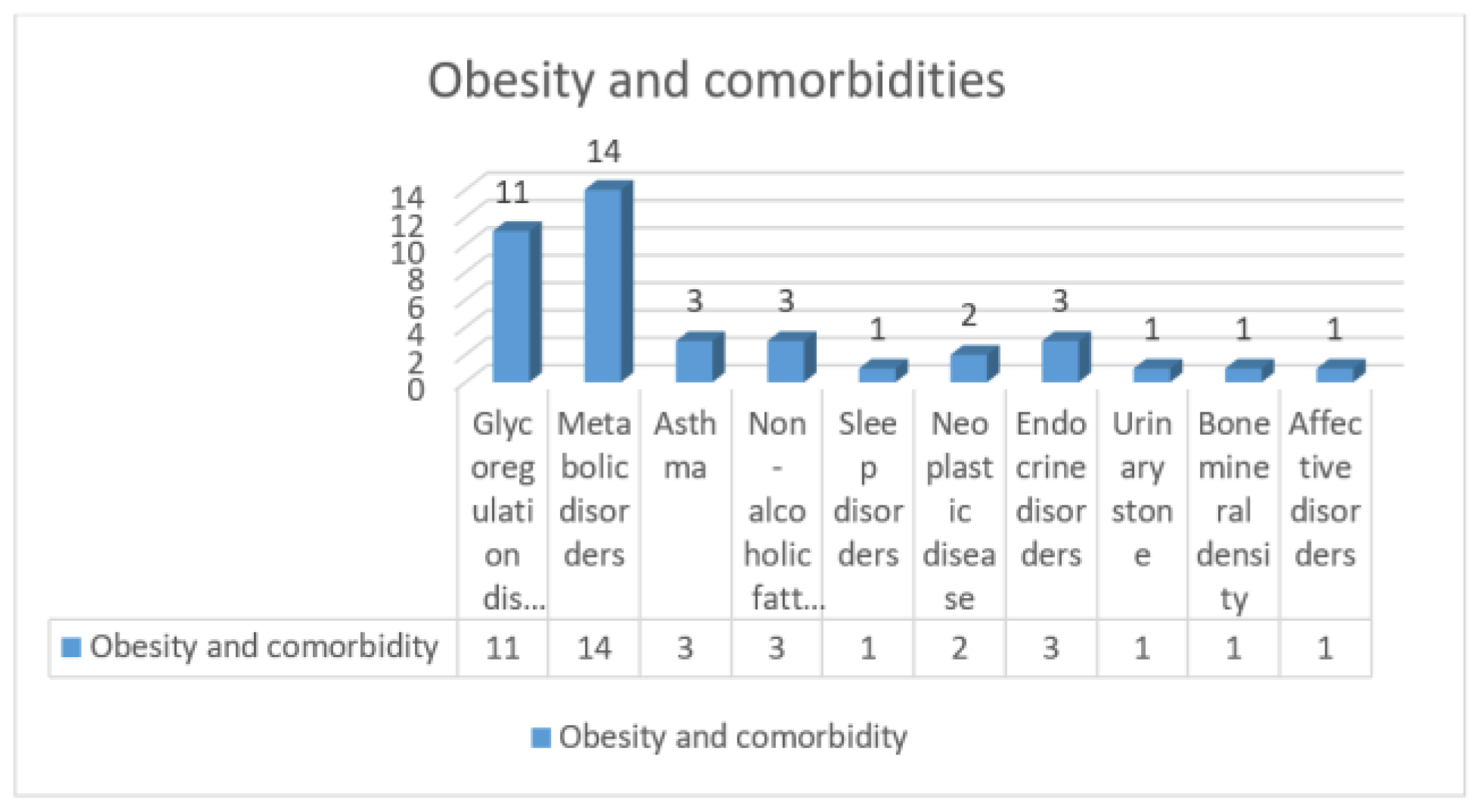
Discussions
Limitation of the study
Conclusions
Contributions
Compliance with ethical standards
Conflict of interest disclosure
References
- Dai, H.; Alsalhe, T.A.; Chalghaf, N.; Riccò, M.; Bragazzi, N.L.; Wu, J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020, 17, e1003198. [Google Scholar] [CrossRef] [PubMed]
- Gil-Rojas, Y.; Garzón, A.; Hernández, F.; et al. Burden of Disease Attributable to Obesity and Overweight in Colombia. Value Health Reg Issues. 2019, 20, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Vogel, M.; Geserick, M.; Gausche, R.; et al. Age-and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int J Obes (Lond). 2022, 46, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Nejadghaderi, S.A.; Grieger, J.A.; Karamzad, N.; et al. Burden of diseases attributable to excess body weight in the Middle East and North Africa region, 1990-2019. Sci Rep. 2023, 13, 20338. [Google Scholar] [CrossRef]
- Australian Burden of Disease Study 2018: Interactive data on risk factor burden. Australian Government, Australian Institute of Health and Welfare, Last updated 15 Aug 2023, https://www.aihw.gov.au/reports/burden-of-disease/abds-2018-interactive-data-risk-factors/contents/overweight-including-obesity.
- Zwemer, E.; Chen, F.; Beck Dallaghan, G.L.; et al. Reinvigorating an Academy of Medical Educators Using Ecological Systems Theory. Cureus. 2022, 14, e21640. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Aggarwal, P.; Bera, O.P.; et al. COVID-19 and childhood obesity (CO-BESITY) in the era of new normal life: A need for a policy research. J Public Health Res. 2021, 10, jphr20212673. [Google Scholar] [CrossRef]
- Fäldt, A.; Nejat, S.; Edvinsson Sollander, S.; Durbeej, N.; Holmgren, A. Increased incidence of overweight and obesity among preschool Swedish children during the COVID-19 pandemic. Eur J Public Health. 2023, 33, 127–131. [Google Scholar] [CrossRef]
- Higgins, J.P.T; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023), Cochrane, 2023. Available online: www.training.cochrane.org/handbook.
- Smith, J.D.; Fu, E.; Kobayashi, M.A. Prevention and Management of Childhood Obesity and Its Psychological and Health Comorbidities. Annu Rev Clin Psychol. 2020, 16, 351–378. [Google Scholar] [CrossRef]
- Pondel, N.; Liśkiewicz, D.; Liśkiewicz, A. Ketogenic diet – mechanism of action and perspectives for the use in the therapy: data from clinical studies. Postepy Biochem. 2020, 66, 270–286. [Google Scholar] [CrossRef]
- Ahmad, N.; Shariff, Z.M.; Mukhtar, F.; Lye, M.S. Effect of Family-Based REDUCE Intervention Program on Children Eating Behavior and Dietary Intake: Randomized Controlled Field Trial. Nutrients. 2020, 12, 3065. [Google Scholar] [CrossRef]
- Van Name, M.A.; Savoye, M.; Chick, J.M.; et al. A Low ω-6 to ω-3 PUFA Ratio (n-6:n-3 PUFA) Diet to Treat Fatty Liver Disease in Obese Youth. J Nutr. 2020, 150, 2314–2321. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.D.; Tang, Z.Z.; Chen, G.; et al. Soy food intake associates with changes in the metabolome and reduced blood pressure in a gut microbiota dependent manner. Nutr Metab Cardiovasc Dis. 2020, 30, 1500–1511. [Google Scholar] [CrossRef]
- Meng, Y.; Lohse, B.; Cunningham-Sabo, L. Sex modifies the association between the CLOCK variant rs1801260 and BMI in school-age children. PLoS One. 2020, 15, e0236991. [Google Scholar] [CrossRef] [PubMed]
- Dooley, J.; Lagou, V.; Goveia, J.; et al. Heterogeneous Effects of Calorie Content and Nutritional Components Underlie Dietary Influence on Pancreatic Cancer Susceptibility. Cell Rep. 2020, 32, 107880. [Google Scholar] [CrossRef]
- Diao, H.; Wang, H.; Yang, L.; Li, T. The impacts of multiple obesity-related interventions on quality of life in children and adolescents: a randomized controlled trial. Health Qual Life Outcomes. 2020, 18, 213. [Google Scholar] [CrossRef]
- Esquivel, M.K.; Higa, A.; Hitchens, M.; Shelton, C.; Okihiro, M. Keiki Produce Prescription (KPRx) Program Feasibility Study to Reduce Food Insecurity and Obesity Risk. Hawaii J Health Soc Welf. 2020, 79, 44–49. [Google Scholar] [PubMed]
- Garcia-Ribera, S.; Amat-Bou, M.; Climent, E.; et al. Specific Dietary Components and Gut Microbiota Composition are Associated with Obesity in Children and Adolescents with Prader-Willi Syndrome. Nutrients. 2020, 12, 1063. [Google Scholar] [CrossRef]
- Ge, L.; Sadeghirad, B.; Ball, G.D.C; et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ. 2020, 369, m696. [Google Scholar] [CrossRef]
- Ruiz, L.D.; Zuelch, M.L.; Dimitratos, S.M.; Scherr, R.E. Adolescent Obesity: Diet Quality, Psychosocial Health, and Cardiometabolic Risk Factors. Nutrients. 2019, 12, 43. [Google Scholar] [CrossRef]
- Holguin, F.; Grasemann, H.; Sharma, S.; et al. L-Citrulline increases nitric oxide and improves control in obese asthmatics. JCI Insight. 2019, 4, e131733. [Google Scholar] [CrossRef]
- Eneli, I.; Xu, J.; Tindall, A.; et al. Using a Revised Protein-Sparing Modified Fast (rPSMF) for Children and Adolescents with Severe Obesity: A Pilot Study. Int J Environ Res Public Health. 2019, 16, 3061. [Google Scholar] [CrossRef]
- Jebeile, H.; Gow, M.L.; Lister, N.B.; et al. Intermittent Energy Restriction Is a Feasible, Effective, and Acceptable Intervention to Treat Adolescents with Obesity. J Nutr. 2019, 149, 1189–1197. [Google Scholar] [CrossRef]
- Wrotniak, B.H.; Georger, L.; Hill, D.L.; et al. Association of dairy intake with weight change in adolescents undergoing obesity treatment. J Public Health (Oxf). 2019, 41, 338–345. [Google Scholar] [CrossRef]
- Lin, X.; Li, H. Obesity: Epidemiology, Pathophysiology, and Therapeutics. Front Endocrinol (Lausanne). 2021, 12, 706978. [Google Scholar] [CrossRef]
- Phillips, N.E.; Mareschal, J.; Schwab, N.; et al. The Effects of Time-Restricted Eating versus Standard Dietary Advice on Weight, Metabolic Health and the Consumption of Processed Food: A Pragmatic Randomised Controlled Trial in Community-Based Adults. Nutrients. 2021, 13, 1042. [Google Scholar] [CrossRef] [PubMed]
- O'Sullivan, B.P.; James, L.; Majure, J.M.; et al. Obesity-related asthma in children: A role for vitamin D. Pediatr Pulmonol. 2021, 56, 354–361. [Google Scholar] [CrossRef]
- Seo, Y.G.; Lim, H.; Kim, Y.; et al. Effects of circuit training or a nutritional intervention on body mass index and other cardiometabolic outcomes in children and adolescents with overweight or obesity. PLoS One. 2021, 16, e0245875. [Google Scholar] [CrossRef]
- Yu, J.; Zhu, H.; Taheri, S.; et al. Plant-Based Nutritional Supplementation Attenuates LPS-Induced Low-Grade Systemic Activation. Int J Mol Sci. 2021, 22, 573. [Google Scholar] [CrossRef]
- Li, T.; Yu, L.; Yang, Z.; et al. Associations of Diet Quality and Heavy Metals with Obesity in Adults: A Cross-Sectional Study from National Health and Nutrition Examination Survey (NHANES). Nutrients. 2022, 14, 4038. [Google Scholar] [CrossRef]
- Luo, Y.; Qiao, X.; Xu, L.; Huang, G. Irisin: circulating levels in serum and its relation to gonadal axis. Endocrine. 2022, 75, 663–671. [Google Scholar] [CrossRef]
- Filler, G.; Dave, S.; Ritter, V.; et al. In focus: perplexing increase of urinary stone disease in children, adolescent and young adult women and its economic impact. Front Med (Lausanne). 2023, 10, 1272900. [Google Scholar] [CrossRef]
- Thompson, D.; Mirabile, Y.; Islam, N.; et al. Diet Quality among Pre-Adolescent African American Girls in a Randomized Controlled Obesity Prevention Intervention Trial. Nutrients. 2023, 15, 2716. [Google Scholar] [CrossRef]
- Zhao, J.; Fan, B.; Huang, J.; et al. Environment-and epigenome-wide association study of obesity in 'Children of 1997' birth cohort. Elife. 2023, 12, e82377. [Google Scholar] [CrossRef]
- Ealey, K.N.; Phillips, J.; Sung, H.K. COVID-19 and obesity: fighting two pandemics with intermittent fasting. Trends Endocrinol Metab. 2021, 32, 706–720. [Google Scholar] [CrossRef]
- Pereira, A.R.; Oliveira, A. Dietary interventions to prevent childhood obesity: a literature review. Nutrients. 2021, 13, 3447. [Google Scholar] [CrossRef]
- Psota, T.L.; Tindall, A.M.; Lohse, B.; et al. The Weight Optimization Revamping Lifestyle using the Dietary Guidelines (WORLD) Study: Sustained Weight Loss Over 12 Months. Obesity (Silver Spring). 2020, 28, 1235–1244. [Google Scholar] [CrossRef]
- Kim, K.W.; Kim, S.J.; Kim, H.; et al. Clinical effects of slim-diet, with lifestyle modification for childhood obesity in community-based healthcare program: A case series. Medicine (Baltimore). 2020, 99, e20817. [Google Scholar] [CrossRef]
- Ludwig, D.S. The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed. J Nutr. 2020, 150, 1354–1359. [Google Scholar] [CrossRef]
- Peleli, M.; Ferreira, D.M.S; Tarnawski, L.; et al. Dietary nitrate attenuates high-fat diet-induced obesity via mechanisms involving higher adipocyte respiration and alterations in inflammatory status. Redox Biol. 2020, 28, 101387. [Google Scholar] [CrossRef]
- Jebeile, H.; Gow, M.L.; Baur, L.A.; Garnett, S.P.; Paxton, S.J.; Lister, N.B. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: A systematic review with meta-analysis. Obes Rev. 2019, 20, 1287–1298. [Google Scholar] [CrossRef]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015, 4, 187–192. [Google Scholar] [CrossRef]
- Kansra, A.R.; Lakkunarajah, S.; Jay, M.S. Childhood and Adolescent Obesity: A Review. Front Pediatr. 2021, 8, 581461. [Google Scholar] [CrossRef]
- Li, G.; Zhong, L.; Han, L.; et al. Genetic variations in adiponectin levels and dietary patterns on metabolic health among children with normal weight versus obesity: the BCAMS study. Int J Obes (Lond). 2022, 46, 325–332. [Google Scholar] [CrossRef]
- He, S.; Le, N.A.; Ramirez-Zea, M.; Martorell, R.; Narayan, K.M.V; Stein, A.D. Leptin partially mediates the association between early-life nutritional supplementation and long-term glycemic status among women in a Guatemalan longitudinal cohort. Am J Clin Nutr. 2020, 111, 804–813. [Google Scholar] [CrossRef]
- Ptomey, L.T.; Willis, E.A.; Sherman, J.R.; et al. Exploring the effectiveness of an 18-month weight management intervention in adults with Down syndrome using propensity score matching. J Intellect Disabil Res. 2020, 64, 221–233. [Google Scholar] [CrossRef]
- Li, H.; Wu, G.; Zhao, L.; Zhang, M. Suppressed inflammation in obese children induced by a high-fiber diet is associated with the attenuation of gut microbial virulence factor genes. Virulence. 2021, 12, 1754–1770. [Google Scholar] [CrossRef]
- Sanchez-Vaznaugh, E.V.; Matsuzaki, M.; Braveman, P.; et al. School nutrition laws in the US: do they influence obesity among youth in a racially/ethnically diverse state? Int J Obes (Lond). 2021, 45, 2358–2368. [Google Scholar] [CrossRef]
- Miller, A.L.; Miller, S.E.; Clark, K.M. Child, Caregiver, Family, and Social-Contextual Factors to Consider when Implementing Parent-Focused Child Feeding Interventions. Curr Nutr Rep. 2018, 7, 303–309. [Google Scholar] [CrossRef]
- So, S.Y.; Wu, Q.; Leung, K.S.; Kundi, Z.M.; Savidge, T.C.; El-Nezami, H. Yeast β-glucan reduces obesity-associated Bilophila abundance and modulates bile acid metabolism in healthy and high-fat diet mouse models. Am J Physiol Gastrointest Liver Physiol. 2021, 321, G639–G655. [Google Scholar] [CrossRef]
- Mustafa, A.E.M; Assery, A.A.A; Asiri, F.M.A; et al. Childhood obesity and its relation with dietary habits among children in Aseer region, Southern Saudi Arabia. J Family Med Prim Care. 2021, 10, 3760–3764. [Google Scholar] [CrossRef]
- Ferguson, J.F.; Roberts-Lee, K.; Borcea, C.; Smith, H.M.; Midgette, Y.; Shah, R. Omega-3 polyunsaturated fatty acids attenuate inflammatory activation and alter differentiation in human adipocytes. J Nutr Biochem. 2019, 64, 45–49. [Google Scholar] [CrossRef]
- Rangel-Huerta, O.D.; Pastor-Villaescusa, B.; Gil, A. Are we close to defining a metabolomic signature of human obesity? A systematic review of metabolomics studies. Metabolomics. 2019, 15, 93. [Google Scholar] [CrossRef]
- Sun, D.; Heianza, Y.; Li, X.; et al. Genetic, epigenetic and transcriptional variations at NFATC2IP locus with weight loss in response to diet interventions: The POUNDS Lost Trial. Diabetes Obes Metab. 2018, 20, 2298–2303. [Google Scholar] [CrossRef]
- Farabi, S.S.; Hernandez, T.L. Low-Carbohydrate Diets for Gestational Diabetes. Nutrients. 2019, 11, 1737. [Google Scholar] [CrossRef]
- de Castro, M.B.T; Cunha, D.B.; Araujo, M.C.; et al. High protein diet promotes body weight loss among Brazilian postpartum women. Matern Child Nutr. 2019, 15, e12746. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Cena, H.; et al. Polycystic Ovary Syndrome in Insulin-Resistant Adolescents with Obesity: The Role of Nutrition Therapy and Food Supplements as a Strategy to Protect Fertility. Nutrients. 2021, 13, 1848. [Google Scholar] [CrossRef]
- Ojeda-Rodríguez, A.; Zazpe, I.; Morell-Azanza, L.; Chueca, M.J.; Azcona-Sanjulian, M.C.; Marti, A. Improved Diet Quality and Nutrient Adequacy in Children and Adolescents with Abdominal Obesity after a Lifestyle Intervention. Nutrients. 2018, 10, 1500. [Google Scholar] [CrossRef]
- Albert Pérez, E.; Mateu Olivares, V.; Martínez-Espinosa, R.M.; Molina Vila, M.D.; Reig García-Galbis, M. New Insights about How to Make an Intervention in Children and Adolescents with Metabolic Syndrome: Diet, Exercise vs. Changes in Body Composition. A Systematic Review of RCT. Nutrients. 2018, 10, 878. [Google Scholar] [CrossRef]
- Stoica, R.A.; Diaconu, C.C.; Rizzo, M.; et al. Weight loss programmes using low carbohydrate diets to control the cardiovascular risk in adolescents (Review). Exp Ther Med. 2021, 21, 90. [Google Scholar] [CrossRef]
- Tung, J.Y.L; Poon, G.W.K; Du, J.; Wong, K.K.Y. Obesity in children and adolescents: Overview of the diagnosis and management. Chronic Dis Transl Med. 2023, 9, 122–133. [Google Scholar] [CrossRef]
- Dorenbos, E.; Drummen, M.; Adam, T.; et al. Effect of a high protein/low glycaemic index diet on insulin resistance in adolescents with overweight/obesity-A PREVIEW randomized clinical trial. Pediatr Obes. 2021, 16, e12702. [Google Scholar] [CrossRef]
- Chiu, S.; Siri-Tarino, P.; Bergeron, N.; Suh, J.H.; Krauss, R.M. A Randomized Study of the Effect of Replacing Sugar-Sweetened Soda by Reduced Fat Milk on Cardiometabolic Health in Male Adolescent Soda Drinkers. Nutrients. 2020, 12, 405. [Google Scholar] [CrossRef]
- Bekelman, T.A.; Ringham, B.M.; Sauder, K.A.; et al. Adherence to index-based dietary patterns in childhood and BMI trajectory during the transition to adolescence: the EPOCH study. Int J Obes (Lond). 2021, 45, 2439–2446. [Google Scholar] [CrossRef]
- Pauley, M.; Mays, C.; Bailes, J.R., Jr.; et al. Carbohydrate-Restricted Diet: A Successful Strategy for Short-Term Management in Youth with Severe Obesity-An Observational Study. Metab Syndr Relat Disord. 2021, 19, 281–287. [Google Scholar] [CrossRef]
- Raynor, H.A.; Mazzeo, S.E.; LaRose, J.G.; et al. Effect of a High-Intensity Dietary Intervention on Changes in Dietary Intake and Eating Pathology during a Multicomponent Adolescent Obesity Intervention. Nutrients. 2021, 13, 1850. [Google Scholar] [CrossRef]
- McMorrow, A.M.; Connaughton, R.M.; Magalhães, T.R.; et al. Personalized Cardio-Metabolic Responses to an Anti-Inflammatory Nutrition Intervention in Obese Adolescents: A Randomized Controlled Crossover Trial. Mol Nutr Food Res. 2018, 62, e1701008. [Google Scholar] [CrossRef]
- Ebbeling, C.B.; Knapp, A.; Johnson, A.; et al. Effects of a low-carbohydrate diet on insulin-resistant dyslipoproteinemia-a randomized controlled feeding trial. Am J Clin Nutr. 2022, 115, 154–162. [Google Scholar] [CrossRef]
- Eslick, S.; Jensen, M.E.; Collins, C.E.; Gibson, P.G.; Hilton, J.; Wood, L.G. Characterising a Weight Loss Intervention in Obese Asthmatic Children. Nutrients. 2020, 12, 507. [Google Scholar] [CrossRef]
- Slowik, V.; Wasserkrug, H.; Fischer, R.T.; et al. Readiness to Change and Prospective Effects of Weight Management Programs in Pediatric Nonalcoholic Fatty Liver Disease. Clin Transl Sci. 2021, 14, 582–588. [Google Scholar] [CrossRef]
- Caro-Sabido, E.A.; Larrosa-Haro, A. Efficacy of dietary intervention and physical activity in children and adolescents with nonalcoholic fatty liver disease associated with obesity: A scoping review. Rev Gastroenterol Mex (Engl Ed). 2019, 84, 185–194. [Google Scholar] [CrossRef]
- Nier, A.; Brandt, A.; Conzelmann, I.B.; Özel, Y.; Bergheim, I. Non-Alcoholic Fatty Liver Disease in Overweight Children: Role of Fructose Intake and Dietary Pattern. Nutrients. 2018, 10, 1329. [Google Scholar] [CrossRef]
- Odar Stough, C.; McCullough, M.B.; Robson, S.L.; et al. Are Preschoolers Meeting the Mark? Comparing the Dietary, Activity, and Sleep Behaviors of Preschoolers With Obesity to National Recommendations. J Pediatr Psychol. 2018, 43, 452–463. [Google Scholar] [CrossRef]
- Suárez González, M.; Díaz Martín, J.J.; Jiménez Treviño, S.; Bousoño García, C.A. Effect of healthy eating before intervention with a low FODMAP diet in pediatric patients with irritable bowel syndrome. Nutr Hosp. 2019, 36, 275–281. [Google Scholar] [CrossRef]
- Kim, J.; Lim, H. Nutritional Management in Childhood Obesity. J Obes Metab Syndr. 2019, 28, 225–235. [Google Scholar] [CrossRef]
- Marcos-Pasero, H.; Colmenarejo, G.; Aguilar-Aguilar, E.; Ramírez de Molina, A.; Reglero, G.; Loria-Kohen, V. Ranking of a wide multidomain set of predictor variables of children obesity by machine learning variable importance techniques. Sci Rep. 2021, 11, 1910. [Google Scholar] [CrossRef]
- Termes Escalé, M.; Martínez Chicano, D.; Egea Castillo, N.; Sánchez, A.G.; et al. Nutritional education in school-age children through Programa Nutriplato®. Nutr Hosp. 2021, 37, 47–51. [Google Scholar] [CrossRef]
- Bello, P.; Gallardo, P.; Pradenas, L.; Ferland, J.A.; Parada, V. Best compromise nutritional menus for childhood obesity. PLoS One. 2020, 15, e0216516. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Pascuzzi, M.C.; et al. Metabolic Derangement in Pediatric Patient with Obesity: The Role of Ketogenic Diet as Therapeutic Tool. Nutrients. 2021, 13, 2805. [Google Scholar] [CrossRef]
- Putnam, M.M.; Richmond, E.M.; Brunick, K.L.; et al. Influence of a Character-Based App on Children's Learning of Nutritional Information: Should Apps Be Served with a Side of Media Characters? Games Health J. 2018, 7, 121–126. [Google Scholar] [CrossRef]
- Kozioł-Kozakowska, A.; Kozłowska, M.; Jagielski, P. Assessment of diet quality, nutrient intake, and dietary behaviours in obese children compared to healthy children. Pediatr Endocrinol Diabetes Metab. 2020, 26, 27–38. [Google Scholar] [CrossRef]
- Sayer, R.D.; Peters, J.C.; Pan, Z.; Wyatt, H.R.; Hill, J.O. Hunger, Food Cravings, and Diet Satisfaction are Related to Changes in Body Weight During a 6-Month Behavioral Weight Loss Intervention: The Beef WISE Study. Nutrients. 2018, 10, 700. [Google Scholar] [CrossRef]
- Díez, J.; Gullón, P.; Valiente, R.; et al. Influence of home/school environments on children's obesity, diet, and physical activity: the SUECO study protocol. Gac Sanit. 2022, 36, 78–81. [Google Scholar] [CrossRef]
- Brown, C.L.; Pratt, K.; Martin, S.; Hulshult, H.; Skelton, J.A. Weight Control Practices in Children of Parents Participating in Weight Management Programs. Child Obes. 2019, 15, 451–8. [Google Scholar] [CrossRef]
- Kim, H.S.; Park, J.; Ma, Y.; Im, M. What are the barriers at home and school to healthy eating?: overweight/obese child and parent perspectives. J Nurs Res. 2019, 27, e48. [Google Scholar] [CrossRef]
- Pratt, K.; Cotto, J.; Xu, J.; Watowicz, R.; Walston, M.; Eneli, I. Adolescents' and Parents' Perspectives of a Revised Protein-Sparing Modified Fast (rPSMF) for Severe Obesity. Int J Environ Res Public Health. 2019, 16, 3385. [Google Scholar] [CrossRef]
- Finn, E.B.; Beck, A.; Sharifi, M. Equitable approaches to reducing the prevalence of pediatric obesity: school nutrition policies and beyond. Int J Obes (Lond). 2021, 45, 2289–2290. [Google Scholar] [CrossRef]
- Costa, S.; Benjamin-Neelon, S.E.; Winpenny, E.; Phillips, V.; Adams, J. Relationship Between Early Childhood Non-Parental Childcare and Diet, Physical Activity, Sedentary Behaviour, and Sleep: A Systematic Review of Longitudinal Studies. Int J Environ Res Public Health. 2019, 16, 4652. [Google Scholar] [CrossRef]
- Brown, T.; Overcash, F.; Reicks, M. Frequency of Trying to Lose Weight and Its Association with Children's Weight Perception and Dietary Intake (NHANES 2011-2012). Nutrients. 2019, 11, 2703. [Google Scholar] [CrossRef]
- Muñoz-Hernandez, V.; Arenaza, L.; Gracia-Marco, L.; et al. Influence of Physical Activity on Bone Mineral Content and Density in Overweight and Obese Children with Low Adherence to the Mediterranean Dietary Pattern. Nutrients. 2018, 10, 1075. [Google Scholar] [CrossRef]
- Gailite, J.; Apela, D.; Dzīvīte-Krišāne, I.; Gardovska, D. Short-Term Predictors for Weight Correction Success of the First Paediatric Weight Correction Programme in Children's Clinical University Hospital in Riga. Medicina (Kaunas). 2019, 55, 75. [Google Scholar] [CrossRef]
- Kim, Y.H.; Lee, J.H.; Yeung, J.L.; et al. Thermogenesis-independent metabolic benefits conferred by isocaloric intermittent fasting in ob/ob mice. Sci Rep. 2019, 9, 2479. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Vecchiato, M.; Pennella, S.; et al. The Impact of the COVID-19 Pandemic on Childhood Obesity and Lifestyle-A Report from Italy. Pediatr Rep. 2022, 14, 410–418. [Google Scholar] [CrossRef]
- Balasundaram, P.; Krishna, S. Obesity Effects on Child Health. In StatPearls; StatPearls Publishing: Treasure Island (FL), 10 April 2023. [Google Scholar]
- Goletzke, J.; De Haene, J.; Stotland, N.E.; et al. Effect of a Low-Glycemic Load Diet Intervention on Maternal and Pregnancy Outcomes in Obese Pregnant Women. Nutrients. 2021, 13, 748. [Google Scholar] [CrossRef] [PubMed]
- Dodd, J.M.; McPhee, A.J.; Deussen, A.R.; et al. Effects of an antenatal dietary intervention in overweight and obese women on 6 month infant outcomes: follow-up from the LIMIT randomised trial. Int J Obes (Lond). 2018, 42, 1326–1335. [Google Scholar] [CrossRef] [PubMed]
- Apperley, L.J.; Blackburn, J.; Erlandson-Parry, K.; Gait, L.; Laing, P.; Senniappan, S. Childhood obesity: A review of current and future management options. Clin Endocrinol (Oxf). 2022, 96, 288–301. [Google Scholar] [CrossRef]
- Vizzari, G.; Sommariva, M.C.; Dei Cas, M.; et al. Circulating Salicylic Acid and Metabolic Profile after 1-Year Nutritional⁻Behavioral Intervention in Children with Obesity. Nutrients. 2019, 11, 1091. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Ebbeling, C.B. The Carbohydrate-Insulin Model of Obesity: Beyond "Calories In, Calories Out". JAMA Intern Med. 2018, 178, 1098–1103. [Google Scholar] [CrossRef]
- Sanyaolu, A.; Okorie, C.; Qi, X.; Locke, J.; Rehman, S. Childhood and Adolescent Obesity in the United States: A Public Health Concern. Glob Pediatr Health. 2019, 6, 2333794X19891305 Published 2019 Dec 1. [Google Scholar] [CrossRef]
- Koo, H.C.; Poh, B.K.; Abd Talib, R. The GReat-Child™ Trial: A Quasi-Experimental Intervention on Whole Grains with Healthy Balanced Diet to Manage Childhood Obesity in Kuala Lumpur, Malaysia. Nutrients. 2018, 10, 156. [Google Scholar] [CrossRef]
- Ooi, D.S.Q; Ling, J.Q.R; Sadananthan, S.A.; et al. Branched-Chain Amino Acid Supplementation Does Not Preserve Lean Mass or Affect Metabolic Profile in Adults with Overweight or Obesity in a Randomized Controlled Weight Loss Intervention. J Nutr. 2021, 151, 911–920. [Google Scholar] [CrossRef]
- Nutrition and Metabolic Management Branch of China International Exchange and Promotive Association for Medical and Health Care, Clinical Nutrition Branch of Chinese Nutrition Society, Chinese Diabetes Society, Chinese Society for Parenteral and Enteral Nutrition, Chinese Clinical Nutritionist Center of Chinese Medical Doctor Association. Guidelines for medical nutrition treatment of overweight/obesity in China (2021). Asia Pac J Clin Nutr. 2022, 31, 450–482. [CrossRef]
- Droahnă, A.R.; Moroianu, L.A.; Pietroșel, V.A.; Bica, C.I.; Salmen, T.; Curis, C.; Merlo, E.M.; Stoica, R.A.; Moroianu, M. Anxio-depressive disorders in a pandemic context: A comparative analysis: year 2019 versus 2020. J Mind Med Sci. 2023, 10, 156–162. [Google Scholar] [CrossRef]
- Thrush, A.B.; Antoun, G.; Nikpay, M.; et al. Diet-resistant obesity is characterized by a distinct plasma proteomic signature and impaired muscle fiber metabolism. Int J Obes (Lond). 2018, 42, 353–362. [Google Scholar] [CrossRef]
- Durán Agüero, S.; Angarita Dávila, L.; Escobar Contreras, M.C.; et al. Noncaloric Sweeteners in Children: A Controversial Theme. Biomed Res Int. 2018, 2018, 4806534. [Google Scholar] [CrossRef] [PubMed]
- Ojeda-Rodríguez, A.; Morell-Azanza, L.; Azcona-Sanjulián, M.C.; Martínez, J.A.; Ramirez, M.J.; Marti, A. Reduced serotonin levels after a lifestyle intervention in obese children: association with glucose and anthropometric measurements. Nutr Hosp. 2018, 35, 279–285. [Google Scholar] [CrossRef]
- Pirini, F.; Rodriguez-Torres, S.; Ayandibu, B.G.; Orera-Clemente, M.; et al. INSIG2 rs7566605 single nucleotide variant and global DNA methylation index levels are associated with weight loss in a personalized weight reduction program. Mol Med Rep. 2018, 17, 1699–1709. [Google Scholar] [CrossRef]
- Moore, J.M.; Haemer, M.A.; Fox, C.K. Lifestyle and pharmacologic management before and after bariatric surgery. Semin Pediatr Surg. 2020, 29, 150889. [Google Scholar] [CrossRef]
- Wadolowska, L.; Hamulka, J.; Kowalkowska, J.; et al. Changes in Sedentary and Active Lifestyle, Diet Quality and Body Composition Nine Months after an Education Program in Polish Students Aged 11⁻12 Years: Report from the ABC of Healthy Eating Study. Nutrients. 2019, 11, 331. [Google Scholar] [CrossRef]
- Krishnan, S.; Adams, S.H.; Allen, L.H.; et al. A randomized controlled-feeding trial based on the Dietary Guidelines for Americans on cardiometabolic health indexes. Am J Clin Nutr. 2018, 108, 266–278. [Google Scholar] [CrossRef]
- Pantea, I.; Roman, N.; Repanovici, A.; Drugus, D. Diabetes Patients' Acceptance of Injectable Treatment, a Scientometric Analysis. Life (Basel). 2022, 12, 2055. [Google Scholar] [CrossRef]
- Curis, C.; Ciubară, A.B.; Nechita, A.; Nechita, L.; Kantor, C.; Moroianu, L.A. The role of the motivational interview in treatment acceptance. Case report. Rev. Med. Chir. Soc. Med. Nat. 2018, 112, 375–380. Available online: https://www.revmedchir.ro/index.php/revmedchir/article/view/1172/1021.
- Curis, C.; Moroianu, M.; Moroianu, L.A.; Pintilei, D.R.; Ardeleanu, V.; Bobirca, A.; Mahler, B.; Pantea Stoian, A. Intuitive Nutrition Co-factor of Emotional Equilibrium for Maintaining Nutritional Balance: A Prospective Study. Mediterranean Journal of Clinical Psychology. 2023, 11. [Google Scholar] [CrossRef]
- Stefan, D.S.; Lixandru, D.; Bajko, D.; et al. The evolution of resting metabolic rate and body composition after 6 and 12 months of lifestyle changes in obese type 2 diabetes patients. 3rd International Conference on Interdisciplinary Management of Diabetes Mellitus and its complications (INTERDIAB). 2017. INTERDIAB 2017: Diabetes Mellitus in Internal Medicine, pp 323-331.
- Drăghici, D.A.; Pantea, I.; Roman, N.; et al. In vitro mechanism whit pulsative laser on thrombolysis. Acta technica napocensis-series: applied mathematics, mechanics, and engineering. 2023, 65. Available online: https://atna-mam.utcluj.ro/index.php/Acta/article/view/1945.

© 2024 by the authors. 2024 Cecilia Curis, Valeriu Ardeleanu, Lavinia Alexandra Moroianu, Corina Manole, Roxana Adriana Stoica, Florentina Gherghiceanu, Anca Pantea Stoian
Share and Cite
Curis, C.; Ardeleanu, V.; Moroianu, L.A.; Manole, C.; Stoica, R.A.; Gherghiceanu, F.; Pantea Stoian, A. Obesity in Children: Systematic Review over a 6-Year Period, Including the COVID-19 Pandemic. J. Mind Med. Sci. 2024, 11, 310-320. https://doi.org/10.22543/2392-7674.1543
Curis C, Ardeleanu V, Moroianu LA, Manole C, Stoica RA, Gherghiceanu F, Pantea Stoian A. Obesity in Children: Systematic Review over a 6-Year Period, Including the COVID-19 Pandemic. Journal of Mind and Medical Sciences. 2024; 11(2):310-320. https://doi.org/10.22543/2392-7674.1543
Chicago/Turabian StyleCuris, Cecilia, Valeriu Ardeleanu, Lavinia Alexandra Moroianu, Corina Manole, Roxana Adriana Stoica, Florentina Gherghiceanu, and Anca Pantea Stoian. 2024. "Obesity in Children: Systematic Review over a 6-Year Period, Including the COVID-19 Pandemic" Journal of Mind and Medical Sciences 11, no. 2: 310-320. https://doi.org/10.22543/2392-7674.1543
APA StyleCuris, C., Ardeleanu, V., Moroianu, L. A., Manole, C., Stoica, R. A., Gherghiceanu, F., & Pantea Stoian, A. (2024). Obesity in Children: Systematic Review over a 6-Year Period, Including the COVID-19 Pandemic. Journal of Mind and Medical Sciences, 11(2), 310-320. https://doi.org/10.22543/2392-7674.1543



