Introduction
An acutely evolving and highly lethal respiratory infection caused by a hitherto uncatalogued coronavirus, later called COVID-19, had its first reports released in December 2019 based on cases that occurred in the Chinese city of Wuhan [
1]. The severe acute respiratory syndrome associated with this infection (SARS-CoV-2) has become a global concern. The rapid spread of the virus across the planet has caused mild to very serious infections. All this speed occurred without there being enough time to generate scientific knowledge to effectively prevent or treat the acute disease. The World Health Organization declared COVID-19 as Pandemic status in March 2020. Although there has been progress in understanding the disease, challenges persist in understanding the pathophysiology of the acute condition and its long-term consequences [
1].
Other devices suffered damage in addition to compromising the respiratory system. Survivors of the acute infection started to demonstrate clinical, laboratory and imaging sequelae changes. Thus, Nalbandian divided the late phase of the disease into: 1) post-acute; and 2) “long COVID” or “Post-COVID-19 Syndrome” (PC19S) [
2]. It is understood that both can bring consequences to their hosts, affecting 10 to 15% of those infected [
2]. Thus, the following among the signs and symptoms which commonly appear stand out: dyspnea, fatigue, tachycardia, thromboembolic phenomena, liver changes and cognitive dysfunctions. The latter can lead to memory changes, even months after the acute infectious condition has resolved, which can affect the quality of life of survivors [
2].
Thus, although SARS-CoV-2 reveals itself as an acute respiratory syndrome, cases have been reported of infected individuals who experienced a phenomenon later called “brain fog”, which consists of difficulties with memory, concentration and performing daily tasks, predominating after resolution of the infection’s acute symptoms [
3]. However, the prevalence and duration of individual symptoms remain difficult to determine due to the lack of standardized research methods in various analyzes and the limited follow-up of patients in clinical studies [
3].
In view of the above, this article aims to bring to light the knowledge gained so far about the possible cognitive effects of infection by the SARS-CoV-2 virus. The consequences are emphasized in terms of symptom recovery time and memory quality.
Materials and Methods
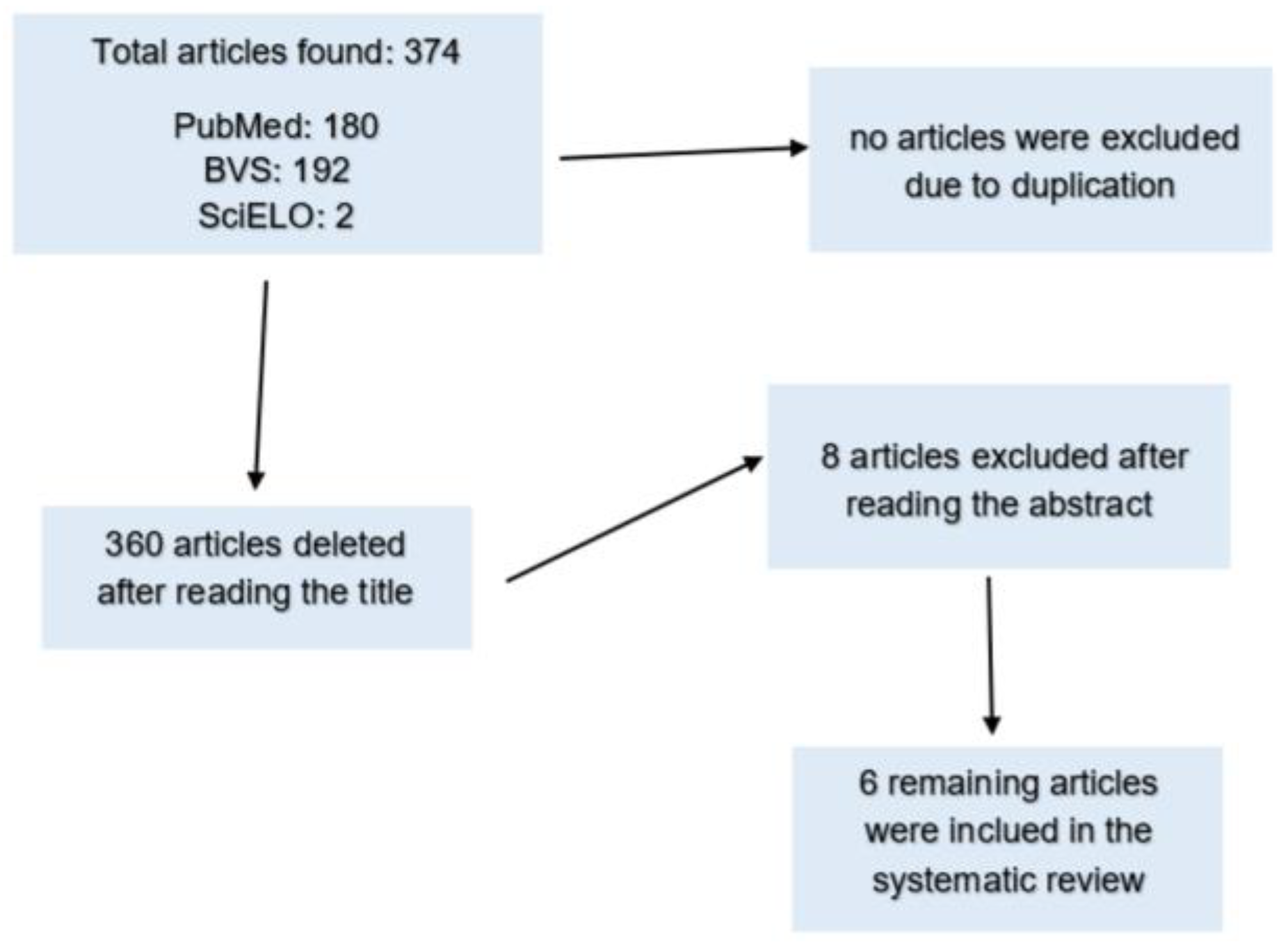
This study consists of a systematic literature review which was conducted in accordance with the statement of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020, attached to the PROSPERO platform (International prospective register of systematic reviews), with the registration code CRD42024519297. Articles indexed in the PubMed, SciELO, and VHL electronic databases were collected in the period between February 20 and April 28, 2024. Retrospective observational studies were selected using the following descriptors and keywords: (COVID-19) “AND” (Memory) “AND” (Reduction), which were obtained according to the Health Science Descriptors (DeCS). The Boolean term “AND” was used instead of the term “OR”, as an exact correlation was sought within the same publication between the chosen DeCS terms. Thus, 6 articles were selected according to the inclusion and exclusion criteria.
The inclusion criteria for selecting articles included: cross-sectional, longitudinal studies and review studies that addressed the relationship between COVID-19 infection and memory reduction (impairment) and articles translated into at least one of the following languages: English, Portuguese or Spanish. Articles that addressed a specific population (only older adults or children, for example), and articles published in languages other than those mentioned were excluded from this review.
A total of 374 articles were found in the initial search, of which there were 180 in PubMed, 192 in VHL and 2 in SciELO. None of the articles found were excluded due to duplication. Next, 360 were excluded after reading the titles. Among the remaining 14 articles, 8 were excluded after reading the abstract, leaving 6 articles selected to perform the present review. These were then read in full.
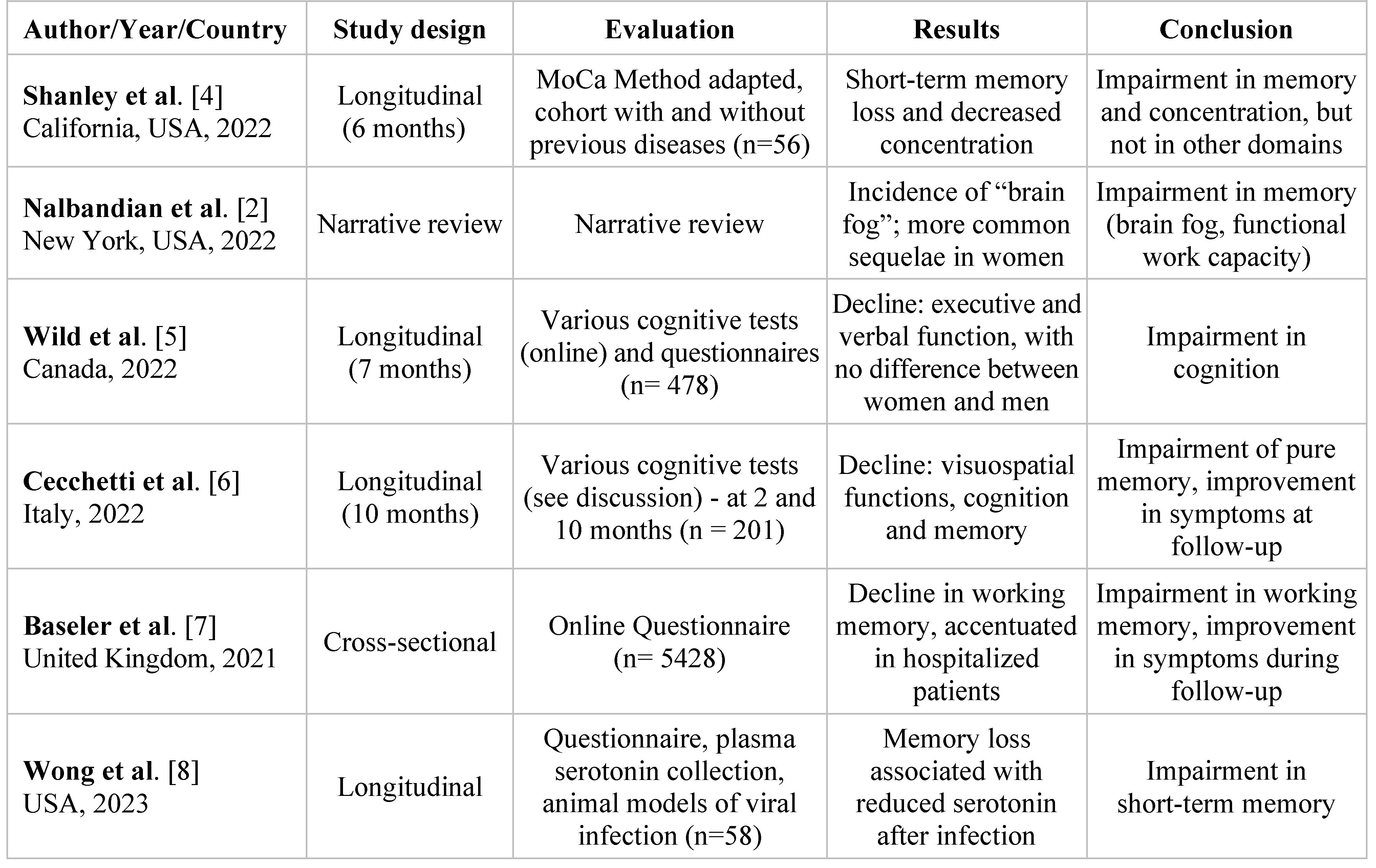
Articles were selected according to the qualifiers described in the methodology, and each article was subsequently read and discussed. Information in the articles was repeatedly presented which formed the emerging categories: memory quality, memory quantity, time, gender, previous neurological or psychological illness, age, number of people and memory assessment technique used in the article. Thus, the relevant information was organized in the
Table 1.
Figure 1.
Search strategy flowchart. Passo Fundo (RS), 2024.
Figure 1.
Search strategy flowchart. Passo Fundo (RS), 2024.
Results
The information highlighted in all selected articles formed the following categories: memory quality/quantity, time, gender, previous illnesses, age, number of people, technique and correlations. This information was distributed in the
Table 1 in order to facilitate the approach to the results that will be analyzed during this review.
According to the table below, Shanley analyzed working memory, attention and language within the MoCa (Montreal cognitive assessment) evaluation technique, a screening tool that evaluates different cognition and memory domains with the purpose of assisting in identification of neurocognitive disorder [
4]. The use of cohorts to compare post-acute neurological sequelae of SARS-COV-2 infection in patients without previous neurological diseases was an important difference in this article in relation to the others in this review. Based on the technique used, the study concluded that the most prominent symptoms in the 6-month follow-up were: short-term memory loss (68.8%) and decreased concentration (61.5%), but they did not obtain worsening in the other domains assessed, such as language, abstraction, executive functioning, orientation or visuospatial skills.
Nalbandian et al. highlighted the so-called “brain fog”, being defined as a post-COVID condition responsible for recent memory loss, difficulties with concentration and execution, in addition to slow reasoning [
2]. Regarding the technique used, the article was presented as a narrative review of the current understanding and general trends of the post-infectious sequelae of COVID-19, highlighting relevant findings and recognizing the limitations of the data available to date. Among the correlations that were cited is the association between cognitive disorders and decreased functional capacity at work, reported by 30% of people, aged 30 to 59. The study suggests a greater preponderance of sequelae among women, corroborating other studies of non-hospitalized patients who attended a neuro-COVID-19 clinic, where 70% of patients with neurological symptoms lasting more than 6 weeks were women [
5,
6,
7,
8,
9].
On the other hand, Wild et al. described the cognitive, physical and mental sequelae of COVID-19, classifying memory impairment into: short-term visual or spatial, logical, verbal, performance on cognitive tests and processing speed [
5]. The study approached 478 volunteers with an average of 42.6 years of age who underwent cognitive tests over a period of 7 months to evaluate memory, attention, problem solving and logic (reasoning), and in addition a questionnaire reporting their experience during the infection. Still under a technical bias, the article states that screening tests such as Mini-Mental State [
10] and MoCA were inconclusive for patients in the post-COVID period. The correlations pointed out by Wild et al. showed clear cognitive deficiencies after COVID-19 infection (discarded deficits due to ICU treatment), which may be more probable in patients who had greater physical exhaustion during the disease [
5]. Furthermore, it was concluded that executive function and verbal skills are key points that can be affected in COVID-19 survivors, with the greatest deficit observed in this study being in relation to the verbal and “thinking” domain. There was no difference in results between different genders or ages in this study, in which 70% of participants were women.
The following tests were applied in the study by Cecchetti et al. [
6]: 1) forward digit extension or the five-digit test (FDT), which analyzes cognitive processing speed; and 2) the VOSP (cube analysis and position discrimination), which assesses visuoconstructive and visuospatial functions. They found that 53% of patients presented disturbances in at least one cognitive domain 2 months after the resolution of COVID-19 and that 6% presented impairment of pure visuospatial function. Cognitive deficits were still evident at follow-up in 36% of patients. The study also analyzed episodic declarative memory (memory of facts experienced by the person and information acquired through the transmission of knowledge) using Rey’s Audio Verbal Learning Test (RAVLT) [
11], which showed pure memory impairment in 6% of patients. This also correlated lower performances with greater WMH (white matter hyperdensities) volumes in the left parieto-occipital region and pointed out that patients complaining of dysgeusia and hyposmia during the acute illness showed less improvement in that test over time compared to patients without dysgeusia/hyposmia. The test subsequently showed a significant improvement in memory at follow-up. In addition to the tests above, the study also included an electroencephalogram (EEG) and a Magnetic Resonance Imaging (MRI). The article was divided into a cross-sectional analysis carried out 2 months after hospital discharge, and a longitudinal analysis carried out 10 months after discharge. In these analyses, clinical assessment, all neuropsychological tests, EEG and MRI were used in the patients under study. A total of 201 individuals were evaluated in the neurological examination, and 49 patients who had a confirmed diagnosis of COVID-19 infection were recruited. The remaining healthy subjects were subdivided into 2 control groups, which only underwent EEG and MRI analysis. Therefore, from the tests used, it appears that despite improvement in memory and cognitive domains being observed during follow-up, a significant sample of patients persists with general impairment in these aspects.
Baseler et al. [
7] assessed working memory and objective memory using an online questionnaire developed using the Qualtrics platform, accessed through a license from the University of York, which in addition to asking about COVID-19 symptoms, investigated memory, concentration, language, thinking, tiredness after mental effort, bad mood and fatigue. Using this technique, the article concluded that objective memory scores were significantly reduced in the COVID positive test and hospitalized groups compared to the non-COVID group. These results suggest that SARS-CoV-2 affects working memory function, even more so in patients who were hospitalized, as opposed to patients between 18 and 24 years of age, who showed no difference in memory tests. However, a significant improvement in memory and executive performance was observed over time, with follow-up being conducted over 17 months in the article.
Furthermore, Wong et al. addresses the topic by relating memory loss to serotonin reduction from the after-effects of viral infection and inflammation caused by COVID-19 and making correlations with human cohort studies, animal models of viral infection and organoid cultures [
8]. This change occurs due to three mechanisms: decreased intestinal absorption of the serotonin precursor, tryptophan; platelet hyperactivation and thrombocytopenia, which affect serotonin storage; and increased serotonin renewal mediated by MAO (monoamine oxidase enzymes). The peripheral reduction of serotonin (which plays an important role in the hippocampus function) in turn impedes vagus nerve activity, and therefore impairs the responses and generation of memories that this system is responsible for, especially short-term ones.
Discussions
The total number of participants in the study covered in the 6 articles ranged from 56 to 5,428 people, with an average of 1,244.2 and a median of 201 people. Gender was specified in two of the six articles. The prevalence in both of these was close to 70% for females. The average age among articles that specified this factor was 47.55 years. The study by Baseler et al. only presented the information that they studied patients over 18 years of age [
7]. The analysis time for articles ranged from 6 to 17 months, with an average of 7.6 months and a median of 6 months.
Regarding the amount of memory, all six articles reveal that there was memory loss in the group of patients infected by COVID-19. As we can see in the
Table 1, according to the author Cecchetti et al., 53% of patients presented disturbances in at least one cognitive domain 2 months after discharge, and it was purely memory loss in 6% of them [
6]. Then, according to Shanley et al., memory impairment and decreased concentration continued to be present in 68.8% and 61.5% of patients with these complaints in the 6-month follow-up, respectively [
4]. However, according to Wild et al., the biggest deficit observed was in relation to the speed of verbal processing and reasoning, but little was associated with short-term visuospatial memory [
5].
Furthermore, patients’ memory during follow-up (recovery) was quantified in 3 of the selected articles: Shanley et al. [
4], Cecchetti et al. [
6] and Baseler et al. [
7], through the Montreal Cognitive Assessment (MoCA) (Shanley et al.) [
4], specific tests, such as the forward digit span test, the RAVLT and the VOSP (Cecchetti et al.) [
6] and an online and anonymous questionnaire (Baseler et al.) [
7]. The conclusion in the three articles mentioned was the same: significant improvement in memory and executive performance. According to Cecchetti et al., this occurred at 10 months [
6], according to Baseler et al. at 17 months [
7], while Shanley et al. did not specify the time [
4]. Finally, Baseler et al. reveals that the decrease in working memory was greater in patients who were admitted to hospitals, and there was no difference in memory tests in patients aged 18 to 24 between the control group and the test group [
7]. This refers to a lack of memory loss in younger patients.
The articles also assessed the existence of previous neurological or psychiatric illness in the patients studied. While the last three articles in the table do not address this topic, the others do. For example, the article by Shanley et al. aimed to evaluate the post-acute neurological sequelae of infection by the virus that causes SARS-CoV-2 in patients with and without previous neurological pathologies, comparing them [
4]. To do so, those recruited were subdivided into 2 Cohorts: Cohort 1, consisting of 40 participants who did not have a previous neurological disease; and Cohort 2, comprising 16 participants with a known previous neurological disease. Of these, 6 had multiple sclerosis; 6, migraine; 1, optic neuritis; 1, narcolepsy; 1, traumatic brain injury; and finally, 1 had Guillain-Barré Syndrome. It was then observed that symptoms in patients with previous neurological disease persisted for a period longer than 6 months, which was less pronounced in those who did not have it. However, COVID-19 impacted the quality of life in these patients more significantly. Although Nalbadian et al. did not address the existence of previous neurological pathology, it was only assessed that the presence of an underlying psychiatric illness is one of the risk factors for the onset of PC19S [
2]. In contrast, Wild et al. analyzed patients with previous debilitating conditions, but mostly non-neurological or psychiatric [
5]. Only 2 patients, less than 1% of those evaluated, reported a previous memory problem, regardless of the underlying condition, whether neurological/psychiatric or not. It was evident that the individuals’ good previous health proved to be a protective factor against infection - better test scores and fewer post-virus sequelae were identified in previously healthy patients.
The first five articles cited in
Table 1, excepting the third [
5] reported that the greater the severity of the SARS-CoV-2 infection, the greater the neurological sequelae involving memory. Cognition and executive functions were more altered, with at least one of their domains compromised, constituting an episode characterized as “brain fog”. In categorizing participants by gender and age, the impact was greater in women and patients older than 25 years, although the authors in Wild et al. [
5] and Wong et al. [
8] do not highlight these differences.
In terms of recovery, there was an improvement in memory and cognitive functions over time, concomitantly with a reduction in symptoms resulting from the COVID-19 infection. Despite significant improvement in memory after resolution of SARS-CoV-2, cognitive deficits were still evident in approximately 36% of patients; or with only a loss of executive functions. However, the majority of patients remained with impaired memory despite no longer presenting the infection symptoms; this corroborates the hypothesis of Kumaria [
12], which provides evidence that the new coronavirus affects endogenous neurogenesis, impairing neuroregeneration and contributing to neurodegenerative processes after COVID-19 infection.
Regarding memory quality, Nalbadian et al. [
2] relates COVID-19 infection to the incidence of the so-called “brain fog”, characterized as one of the most prevalent memory disorders in PC19S syndrome, and responsible for symptoms such as: recent memory loss, difficulties in concentrating and executing what was usual for people, in addition to slow reasoning [
3]. Furthermore, in the article it was concluded that 30% of people aged 30 to 59 who reported cognitive disorders also felt a decrease in functional capacity at work; this is a similar fact to the result found by Baseler et al. [
7], whose main finding was that objective memory scores were significantly reduced in the COVID-positive and hospitalized groups compared to the non-COVID group. In turn, Wong et al. highlights the importance of serotonin in short-term memory and suggests that its peripheral reduction was responsible for cognitive impairment due to dampening of vagal signaling, which impairs hippocampal responses and memory [
8].
Therefore, these results suggest that COVID-19 affects working memory function. It is suggested that working memory comprises a system of temporary storage and information manipulation, forming an important link between perception and controlled action [
13]. Thus, given the importance of working/short-term memory for everyday tasks such as conversing, making decisions, reading comprehension, carrying out a sequence of actions, it is reasonable to conclude that working memory deficits induced by COVID-19 may compromise performance in daily life.
However, according to Wild et al., the biggest deficit observed was in relation to verbal processing and reasoning speed [
5]. Therefore, in contrast to the authors Nalbadian et al. [
2] and Baseler et al. [
7], the syndrome was little associated with the loss of short-term visuospatial memory (a subcomponent of working memory); in turn (according to the article), concluding that the condition did not have a global impact on cognitive processing. Thus, it also opposes Cecchetti et al. [
6], which reveals that 6% of patients had loss in the purely memory domain and another 6% had visuospatial memory loss; this means that compared to healthy patients, all of them had worse cognitive performance in the domains evaluated 2 months after discharge from COVID-19 infection.
In line with the other authors, but using the Montreal Cognitive Assessment (MoCA) - an approximately 10-minute cognitive screening tool that assesses executive functioning, abstraction, short-term memory, language, orientation and visuospatial skills - Shanley et al. points out that the loss of short-term memory and decreased concentration stand out among the most prominent symptoms after six months of COVID-19 infection, despite improvements in the other assessed domains [
4].
Conclusions
Regarding the memory quantity, all five articles reveal that there was memory loss in the group of patients infected by COVID-19. There was a significant improvement in memory and executive performance at follow-up, with the decrease in working memory being greater in patients undergoing hospital admissions. Younger patients were spared memory loss.
Symptoms in patients with previous neurological disease were more pronounced. However, COVID-19 impacted quality of life more significantly in patients who did not have it. The presence of an underlying psychiatric illness is also one of the risk factors contributing to the onset of PC19S. Furthermore, previously healthy patients had better test scores and fewer post-virus sequelae. The first five articles reported that the greater the severity of the COVID-19 condition, the greater the neurological sequelae involving memory, with cognition and executive functions being those which showed the most changes. Women and patients over 25 years of age suffered the greatest repercussions.
There was an improvement in memory and cognitive functions over time after recovery. However, cognitive deficits remained evident in approximately 36% of patients, and the majority of patients had impaired memory, despite the end of infection symptoms. Finally, the types of memory affected by COVID-19 include working memory, verbal processing and reasoning speed, visuospatial memory, short-term memory and concentration.
Contributions
LLA: article advisor, conducted the analyzes and made the final review of the text; ADB: conceptualized the study, gathered data on memory impairment and COVID, data interpretation; BSA: summarized the results in tables, wrote the first draft of the article, final review of the article; CAS: wrote the first draft of the article, final revisions of the text; GR: conceptualized the study, data interpretation, wrote the first draft of the article; MCTP: gathered the data on memory impairment and COVID, conducted the analyzes and summarized the results in tables, wrote the first draft of the article; MEDK: conceptualized the study, contributed to the study design data interpretation, submitted the article; MFAC: wrote the first draft of the article; data interpretation; NLC: contributed to the study design, data interpretation, final revisions of the text; PSD: gathered data on memory impairment and COVID, summarized the results in tables; VGO: wrote the first draft of the article, conducted the analyzes and summarized the results in tables, final revisions of the text.