Abstract
Introduction. Globally, over 230 million people have peripheral artery disease, often undiagnosed, leading to chronic limb-threatening ischemia. Revascularization is vital for preventing amputation and improving quality of life. While specific questionnaires for severe ischemia are lacking, the SF-36 questionnaire is widely used to assess quality of life, with variations like SF-12 and SF-8 for larger cohorts. Objectives. Our aim was to assess how different lower limb revascularization methods affect the postoperative quality of life in patients with chronic limb-threatening ischemia. Methods. This study was conducted at the St. Pantelimon Emergency Hospital of Bucharest, Romania. It included 166 adult patients with chronic limb-threatening ischemia who were monitored for 12 months. Quality of life was assessed using the SF-36 questionnaire. The patients were categorized into two groups: 112 underwent conventional surgery, and 54 had hybrid procedures. Data analysis involved t-tests, Mann-Whitney U tests and assessment of data reliability. Results. In the Conventional Surgery group, the average age was 70.5 years, predominantly male, with similar risk factors as the second group. The Hybrid Surgery group had an average age of 73 and exhibited more extensive distal arterial lesions, higher rates of ulcer/gangrene, and a higher occurrence of postoperative minor amputations. The SF-36 questionnaire showed low data reliability for the General Health and Social Functioning domains. Additionally, the Hybrid Surgery group had poorer preoperative perception in the Body Pain category. However, significant postoperative improvements in quality of life were observed in all domains for both groups with similar results. Conclusions. Revascularization improves the quality of life for patients with chronic limb-threatening ischemia, including those that also require minor amputations. SF-36 has good assessment for most QoL aspects, but reliability declines in severe ischemia.
Introduction
Globally, more than 230 million people have been diagnosed with peripheral artery disease (PAD) and approximately half of them are asymptomatic [1,2]. This may account for the significant underdiagnosis and inadequate management of arteriopathic patients, which, in turn, contributes to its progression into chronic limb-threatening ischemia (CLTI), the severe form of the disease. In Romania, there are currently no PAD screening programs available for the general population. Typically, patients are directed to vascular surgeons by general practitioners, frequently after they have already developed CLTI. Furthermore, the limited availability of vascular surgery departments often results in extended waiting periods for elective surgery. A recent study underscores the substantial disparities among countries in terms of the prevalence of vascular surgeons worldwide [3,4].
Revascularization plays a pivotal role in the prevention of amputation among CLTI patients and simultaneously enhances their quality of life (QoL). Although QoL is inherently subjective, it can be assessed through self-administered questionnaires, such as the SF-36 (Short Form 36 Health Profile) and the NHP (Nottingham Health Profile), both of which demonstrate reliability when used with patients who have PAD [3,4].
The SF-36 questionnaire comprises 36 questions organized into eight categories designed to assess overall health status. These categories include Physical Functioning (PF - 10 items), Role limitations due to Physical health (RP - 4 items), Role limitations due to Emotional problems (RE - 3 items), Energy/fatigue or Vitality (VIT - 4 items), Emotional well-being or Mental Health (MH - 5 items), Social Functioning (SF - 2 items), Bodily Pain (BP - 2 items), and General Health (GH - 5 items). The SF-36 stands as one of the most widely utilized tools for measuring QoL in the field of medicine, having been employed in thousands of studies over the past decades [5,6]. Derived from a questionnaire encompassing 149 items distributed across 40 domains, the SF-36 originally evolved as a component of the Medical Outcomes Study (MOS), which sought to assess the impact of medical care on patients' well-being [7,8]. In 1992, the RAND Corporation developed and licensed the SF-36, making it freely accessible for use, subject to adherence to the terms and conditions specified on their official website (https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html) [9,10]. This tool was designed to serve the purpose of conducting surveys within the general population as well as to facilitate application in clinical practice and research studies [11,12,13]. Other variants of this test, such as the SF-12, which comprises a concise 12-item questionnaire, and the SF-8, featuring just one question per category, have demonstrated enhanced utility when applied to large cohorts of patients, as opposed to smaller study groups [14,15].
Several questionnaires tailored to address specific stages of PAD have been created. Examples include the Intermittent Claudication Questionnaire (ICQ) [16], Walking Impairment Questionnaire (WIQ) [17], and Claudication Scale (CLAU-S) [18]. However, it's important to note that these questionnaires are not well-suited for patients with severe ischemia and as of now, there is no dedicated QoL measuring tool available for patients suffering from CLTI.
Our objective was to assess the influence of different lower limb revascularization methods on patients' postoperative quality of life perception in cases of chronic limb-threatening ischemia.
Materials and Methods
This was a single-center observational study conducted at the Saint Pantelimon Emergency Clinical Hospital of Bucharest, Romania, spanning from 2020 to 2022. A total of 213 adult patients diagnosed with CLTI were invited to participate in this study, out of which 166 were included. These patients were under observation for a 12-month duration, with standard follow-up appointments scheduled at 3-, 6-, and 12-months post-diagnosis.
Quality of life assessment was performed using the SF-36 questionnaire. Data collection occurred both prior to revascularization and during subsequent follow-up examinations. Attendance at these follow-up assessments showed a gradual decline, with attendance rates decreasing from 82% at the first check-up to 73% at the second and 66% at the third. Nevertheless, we successfully collected post-operative data from about four-fifths of our patients.
Originally, the results were recorded on paper and later digitally centralized. We included adult patients who had been diagnosed with CLTI, with or without trophic ulcers/gangrene, who were capable of effective communication and decision-making, and who did not have any other documented conditions that significantly limited their ability to walk. Disease staging followed international standards [19,20].
To analyze the data obtained, the patients were categorized into two groups: the first group consisted of 112 patients who underwent conventional surgery (CS), while the second group included 54 patients who underwent hybrid procedures (HS).
Data analysis involved the utilization of the t-test for independent samples. For each group, the median and Interquartile Ratio (IQR) were calculated separately for every domain of the SF-36. Differences between measurements were assessed using the Mann-Whitney U test. To evaluate data reliability, floor and ceiling effects were computed, along with Cronbach's alpha values. Statistical significance was set at a p-value of 5%. Data was considered reliable when floor-ceiling effects were less than 20% and alpha values exceeded 0.7.
It's essential to note that the data collected is subjective in nature and may be susceptible to bias. This study received approval from the research ethics committee of the Saint Pantelimon Emergency Clinical Hospital of Bucharest.
Results
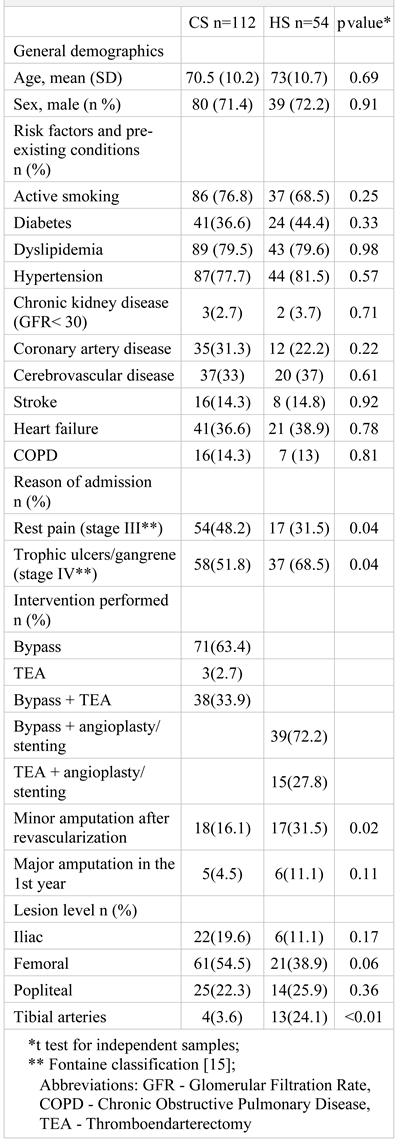
The average age was 70.5 years for the CS group and 73 years for the HS group. In both groups, more than two-thirds of the participants were male. Although there was a high prevalence of cardiovascular risk factors, there were generally no statistically significant differences in terms of demographic characteristics and pre-existing conditions between the CS and HS groups. However, it's worth noting that patients in the HS group had more extensive distal arterial lesions (24.1% vs. 3.6%, p < 0.01), a higher likelihood of presenting with trophic ulcers or gangrene at admission (68.5% vs. 51.8%, p = 0.04), and a higher percentage of minor amputations performed after revascularization (31.5% vs. 16.1%, p = 0.02) (Table 1).

Table 1.
General demographics and characteristics
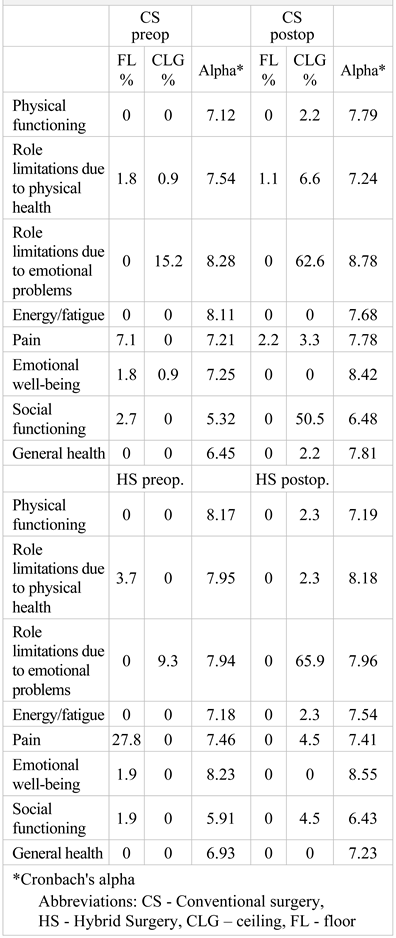
While a substantial floor effect was observed in the preoperative Body Pain domain for the Hybrid Surgery group (27.8%), the Cronbach's alpha value (HS: 7.46) still indicated reliability. High ceiling effects were also noted in the postoperative RE sections for both groups (CS: 62.6% and HS: 65.9%), again with robust alpha scores (CS: 8.25 and HS: 7.96). Preoperative assessments of General Health were deemed unreliable (CS: 6.45 and HS: 6.93), and none of the data related to the Social Functioning section met reliability standards (Table 2).

Table 2.
Floor - ceiling effects and data reliability
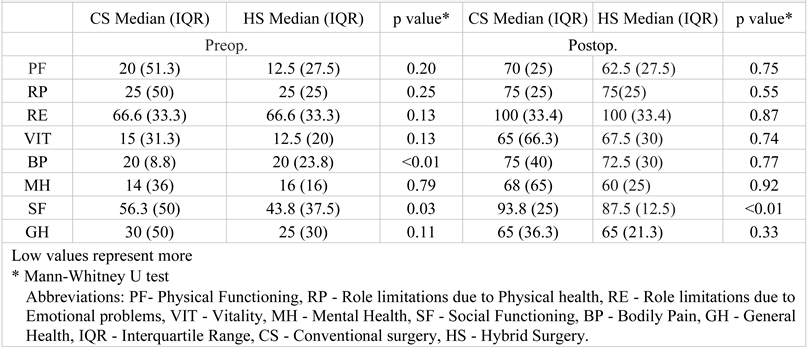
Preoperative evaluations of quality of life underscored a prevalent perception of poor health across most domains in both groups.
The preoperative QoL in the BP category (p < 0.01) and the SF category (p = 0.03) was statistically significantly worse for the HS group. This lower QoL in the SF domain also extended into the postoperative phase (p < 0.01). There were no other significant differences observed, as presented in the Table 3.

Table 3.
Differences between the two groups in all domains; pre- and post-operative results
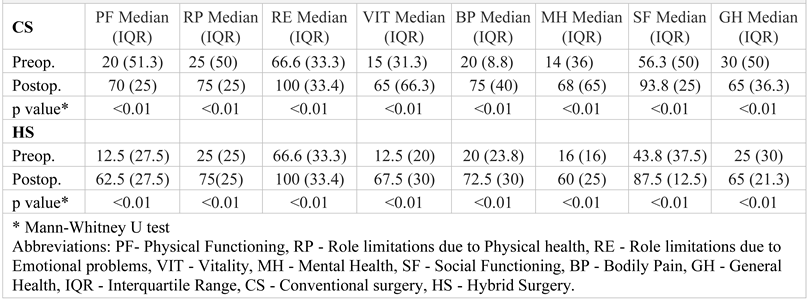
Upon directly comparing preoperative and post-operative self-perceived QoL, a remarkable and statistically significant improvement was observed across all domains for both study groups (p < 0.01). Notably, even though the Hybrid Surgery group underwent significantly more minor amputations, the postoperative QoL did not exhibit significant differences from that of the Conventional Surgery group in seven out of the eight domains. The sole category demonstrating a noticeable difference, namely Social Functioning, is marred by unreliable data. For a comprehensive yet detailed presentation of these findings as well as a visual representation of QoL improvement, please see Table 4 and Figure 1.

Table 4.
Quality of life improvement before and after revascularization for each group
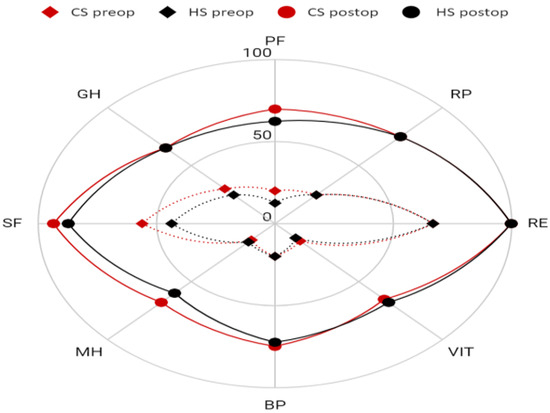
Figure 1.
Visual representation of QoL improvement for each group
A radar chart was chosen for a better visual effect. The outer circle represents perfect health. The larger the area inside the circle, the fewer perceived health related issues. A smaller area is associated with many perceived problems.
Abbreviations: PF- Physical Functioning, RP - Role limitations due to Physical health, RE - Role limitations due to Emotional problems, VIT - Vitality, MH - Mental Health, SF - Social Functioning, BP - Bodily Pain, GH - General Health, CS - Conventional surgery, HS - Hybrid Surgery.
Discussions
Chronic limb-threatening ischemia presents a multifaceted and formidable challenge, profoundly impacting the lives of individuals and posing a significant threat to their overall well-being. Often compared to terminal cancer and hypervirulent infectious diseases in terms of its disruptive impact [21,22,23], CLTI manifests with severe mortality and amputation rates, leading to substantial physical and psychological distress. Patients suffering from CLTI experience a marked deterioration in their quality of life, grappling with chronic pain, reduced mobility, and a reliance on long-term medical interventions. The burden of CLTI not only affects patients physically but also takes a toll on their mental health, leading to emotional distress and diminished well-being.
Despite these challenges, there are promising avenues for improving the quality of life of CLTI patients. Revascularization techniques, for instance, have emerged as critical interventions that play a pivotal role in preventing major amputations and preserving limb functionality. Successful revascularization not only aids in enhancing mobility but also contributes to a decrease in pain, thereby positively influencing both the physical and psychological aspects of patients' well-being.
Our research highlighted improvements even for patients undergoing a mandatory minor amputation after revascularization. Notably, other studies demonstrate significant enhancements even for those undergoing major amputations, particularly those capable of using a prosthesis afterward [24,25].
Comparative findings post-surgery indicates an enhanced quality of life for the majority of critically ill patients requiring revascularization. Both traditional bypass surgery and hybrid techniques serve as valuable resources in the arsenal of vascular surgeons. Hybrid procedures were employed for individuals with severe arterial lesions, yielding a postoperative quality of life outcome comparable to the control group.
Numerous other studies have investigated QoL enhancements following diverse methods of treatment for PAD patients. While medical treatment alone has shown to boost quality of life for intermittent claudication patients, the effect is not as pronounced as with endovascular treatment [26,27,28]. Surgical and endovascular revascularization demonstrate similar outcomes in terms of postoperative health status self-perception [29,30].
Furthermore, the collaborative efforts of multidisciplinary teams, including diabetologists, vascular specialists, and orthopedic surgeons, have proven instrumental in devising comprehensive treatment plans that address not just the physical health of patients but also provide crucial psychosocial support and guidance [31,32,33]. This comprehensive care approach acknowledges the interconnectedness of physical and mental health, recognizing the importance of holistic well-being in enhancing the quality of life of individuals battling CLTI.
To optimize the treatment approach further, the adoption of a patient-centric model could be the key. This approach recognizes the significance of tailoring treatments to individual patients, considering factors such as life expectancy and functional status. By involving patients in the decision-making process and considering their preferences and unique circumstances, this model promotes a sense of control and autonomy over their health, playing a vital role in enhancing their overall quality of life. The integration of patient preferences and values into the treatment plan fosters a more personalized and empathetic approach, allowing patients to feel heard and understood throughout their healthcare journey.
In addition to these approaches, advancements in drug-eluting technologies have shown promising results in reducing the need for repetitive interventions and amputations, thus alleviating the physical and emotional burden often associated with persistent medical procedures [34,35,36]. These cutting-edge innovations not only aim to improve clinical outcomes but also prioritize the overall well-being and comfort of patients, thereby contributing to an enhanced quality of life.
In the pursuit of more effective and comprehensive treatments, the field of regenerative medicine has shown significant promise. In particular, the use of stem cell therapy, specifically mesenchymal stem cells (MSCs), has emerged as a potential breakthrough in the management of CLTI [37,38,39]. Harnessing the regenerative and immunomodulatory properties of MSCs, this innovative approach aims to promote tissue regeneration and alleviate pain [40], ultimately enhancing the physical functioning and emotional well-being of patients. By addressing the underlying pathology and promoting healing at the cellular level, stem cell therapy offers a new ray of hope for individuals struggling with CLTI [41,42].
The economic burden imposed by CLTI cannot be overlooked, as it exerts significant strain on healthcare systems and affects the financial stability of affected individuals. With frequent hospitalizations, prolonged treatments, and high associated costs, the economic impact further amplifies the stress experienced by patients. As such, there is a pressing need to develop cost-effective interventions and optimize healthcare resources to alleviate the financial strain and ensure equitable access to quality care for all patients. By streamlining healthcare services and implementing efficient resource allocation strategies, healthcare systems can better support individuals affected by CLTI and contribute to an improved overall quality of life for these patients [43,44].
Furthermore, the integration of patient education and empowerment programs can play a crucial role in enhancing the overall quality of life for individuals with CLTI. By providing comprehensive information about the condition, treatment options, and self-management strategies, these programs can empower patients to take an active role in their healthcare journey. Through education and support, patients can gain a better understanding of their condition, make informed decisions about their treatment, and actively participate in their rehabilitation process. This sense of empowerment and engagement can significantly improve patients' overall well-being and foster a sense of control and agency in managing their health [45,46].
The importance of understanding and evaluating the QoL in patients with CLTI has garnered attention, yet the current assessment tools appear inadequate and insufficiently tailored to the complex nature of this condition. The available QoL assessment instruments for CLTI demonstrate heterogeneity, lack of consistency, and incomplete coverage of relevant domains. Unlike in patients with claudication, where there has been a recent emphasis on developing comprehensive measures for symptom assessment and QoL, the tools for CLTI patients have not received equal attention and validation.
Existing generic QoL assessment tools, such as EQ5-D and SF-12, have been utilized to assess QoL in CLTI patients, yet their generic nature fails to capture the specific challenges and limitations faced by individuals with CLTI. The limited specificity of these tools poses challenges in understanding the unique treatment pathways required for patients with CLTI. This lack of specificity is evident in various vascular instruments, including VascuQoL and PADQOL, which do not fully address the particular limitations experienced by CLTI patients [47,48].
The imperative need to address these limitations in the existing QoL questionnaires for CLTI lies in the necessity to accurately evaluate the efficacy of various treatment approaches, including medical, biologic, regenerative, revascularization, and non-revascularization interventions. It is vital to develop precise and comprehensive tools that can capture the multifaceted impact of CLTI and the diverse treatment effects [49,50].
The establishment of a universally applicable questionnaire for CLTI is essential for informed decision-making, comparative evaluation of treatment efficacy, and raising public awareness about this debilitating condition. Moreover, incorporating patient input in the development process is critical to ensure that the questionnaire can capture the full spectrum of the patient experience and account for individual variations in the disease trajectory.
The path to developing a reliable questionnaire for CLTI involves various stages, including data collection, qualitative analysis, survey design, and validation. Despite the challenges inherent in this process, efforts from a multidisciplinary team comprising experts from different specialties (including gene therapy) are crucial to ensure the success and widespread implementation of the newly derived instrument [51,52].
While the SF-36 form is validated for patients with intermittent claudication [53], and although our data was largely reliable, the absence of a dedicated questionnaire for severe ischemia represents a limitation of this study.
Conclusions
Revascularization dramatically enhances the quality of life for all CLTI patients, regardless of the surgical procedure selected. Additionally, patients who undergo minor amputations also experience improved postoperative quality of life. In the absence of a disease specific questionnaire when assessing patients with CLTI, the SF-36 serves as a valuable tool for evaluating most QoL aspects. However, its reliability decreases, particularly in domains like bodily pain and social functioning, when dealing with severe ischemia.
Highlights
- ✓
- Different methods of lower limb revascularization on the postoperative quality of life of CLTI patients highlights the multifaceted challenges they face, but underlines the significant improvement in QoL post-revascularization.
- ✓
- Despite the lack of a dedicated QoL measuring tool for CLTI patients, the study's findings suggest that both conventional surgery and hybrid procedures contribute to notable improvements in patients' QoL across various domains, underscoring the significance of tailored and comprehensive treatment approaches for these individuals.
Contributions
Conceptualization: Paius Cristian and Carap Alexandru; Data Curation: Paius Cristian; Formal Analysis: Tarus Andrei; Investigation: Paius Cristian; Methodology: Constantin Vlad Denis, Paius Cristian; Project Administration: Tinica Grigore; Resources: Carap Alexandru, Supervision: Tinica Grigore; Validation, Constantin Vlad Denis and Tinca Grigore, Visualization, Carap Alexandru and Tarus Andrei; Writing—Original Draft: Paius Cristian; Writing—Review and Editing: Tarus Andrei
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript. Informed consent was obtained from all subjects involved in the study.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- Aday, A.W.; Matsushita, K. Epidemiology of Peripheral Artery Disease and Polyvascular Disease. Circ Res. 2021, 128, 1818–1832. [Google Scholar] [CrossRef] [PubMed]
- Dhaliwal, G.; Mukherjee, D. Peripheral arterial disease: Epidemiology, natural history, diagnosis and treatment. Int J Angiol. 2007, 16, 36–44. [Google Scholar] [CrossRef]
- Bencheikh, N.; Zarrintan, S.; Quatramoni, J.G.; Al-Nouri, O.; Malas, M.; Gaffey, A.C. Vascular Surgery in Low-Income and Middle-Income Countries: A State-of-the-Art Review. Ann Vasc Surg. 2023, 95, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg. 2019, 69, 3S–125S.e40. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, J.; van Rijswijk, C.; Van Den Hoven, P.; Hamming, J.; van der Vorst, J.R. Chronic Limb-Threatening Ischemia: When is Enough Enough? J Endovasc Ther. 2023, 15266028231187604. [Google Scholar] [CrossRef]
- Corcoran, W.E.; Durham, C.F. Quality of life as an outcome-based evaluation of coronary artery bypass graft critical paths using the SF-36. Qual Manag Health Care. 2000, 8, 72–81. [Google Scholar] [CrossRef]
- Rasmussen, D.; Barnason, S.; Smith, J.; et al. Patient outcomes after peripheral revascularization surgery. J Vasc Nurs. 2001, 19, 108–116. [Google Scholar] [CrossRef]
- Tarlov, A.R.; Ware, J.E., Jr.; Greenfield, S.; Nelson, E.C.; Perrin, E.; Zubkoff, M. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA. 1989, 262, 925–930. [Google Scholar] [CrossRef]
- Hunt, S.M.; McKenna, S.P. Validating the SF-36. BMJ. 1992, 305, 645–646. [Google Scholar] [CrossRef]
- Constantin, V.D.; Socea, B.; Gaspar, B.S.; Epistatu, D.; Paunica, I.; Dumitriu, A.S.; Paunica, S.; Silaghi, A. Limb amputations; etiopathogenesis, diagnosis and the multidisciplinary therapeutic approach. J Mind Med Sci. 2022, 9, 209–223. [Google Scholar] [CrossRef]
- Brazier, J.E.; Harper, R.; Jones, N.M.; et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992, 305, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Almasri, J.; Adusumalli, J.; Asi, N.; et al. A systematic review and meta-analysis of revascularization outcomes of infrainguinal chronic limb-threatening ischemia. J Vasc Surg. 2018, 68, 624–633. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.A.; Donegan, D.; Albert, T. The 36-item short form. J Am Acad Orthop Surg. 2007, 15, 126–134. [Google Scholar] [CrossRef]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; et al. Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia. Eur J Vasc Endovasc Surg. 2019, 58, S1–S109.e33. [Google Scholar] [CrossRef]
- Chong, P.F.; Garratt, A.M.; Golledge, J.; Greenhalgh, R.M.; Davies, A.H. The intermittent claudication questionnaire: a patient-assessed condition-specific health outcome measure. J Vasc Surg. 2002, 36, 764–864. [Google Scholar] [CrossRef]
- Regensteiner, J.G.; Steiner, J.F.; Panzer, R.J.; Hiatt, W.R. Evaluation of walking impairment by questionnaire in patients with peripheral arterial disease. J Vasc Med Biol. 1990, 2, 142–152. [Google Scholar]
- Spengel, F.A.; Brown, T.M.; Dietze, S.; Kirchberger, I.; Comte, S. The Claudication Scale (CLAU-S). A new disease-specific quality of life instrument in intermittent claudication. Disease Management & Health Outcomes. 1997, 2, 65–70. [Google Scholar]
- Rutherford, R.B.; Baker, J.D.; Ernst, C.; et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997, 26, 517–538. [Google Scholar] [CrossRef]
- Kutsenko, O.; Sommerset, J.; Chandra, V.; Bryce, Y. Techniques Providing Endpoints for Revascularization in Chronic Limb-Threatening Ischemia. Semin Intervent Radiol. 2023, 40, 177–182, Published 2023 Jun 16. [Google Scholar] [CrossRef]
- Hata, Y.; Iida, O.; Okamoto, S.; et al. Japanese real-world population with chronic limb-threatening ischemia who meet the criteria of the BEST-CLI trial. Vasc Med. 2023, 1358863X231205229. [Google Scholar] [CrossRef]
- Iancu, G.; Serban, D.; Badiu, C.D.; Tanasescu, C.; Tudosie, M.S.; Tudor, C.; Costea, D.O.; Zgura, A.; Iancu, R.; Vasile, D. Tyrosine kinase inhibitors in breast cancer (Review). Exp Ther Med. 2022, 23, 114. [Google Scholar] [CrossRef]
- Serban, D.; Popa Cherecheanu, A.; Dascalu, A.M.; et al. Hypervirulent Klebsiella pneumoniae Endogenous Endophthalmitis-A Global Emerging Disease. Life (Basel). 2021, 11, 676. [Google Scholar] [CrossRef]
- Davie-Smith, F.; Coulter, E.; Kennon, B.; Wyke, S.; Paul, L. Factors influencing quality of life following lower limb amputation for peripheral arterial occlusive disease: A systematic review of the literature. Prosthet Orthot Int. 2017, 41, 537–547. [Google Scholar] [CrossRef]
- Yagshyyev, S.; Hausmann, P.; Li, Y.; et al. Intermittent negative pressure therapy in patients with no-option chronic limb-threatening ischemia. Vasa 2023, 10.1024/0301-1526/a001098. [Google Scholar] [CrossRef]
- Nylaende, M.; Abdelnoor, M.; Stranden, E.; et al. The Oslo balloon angioplasty versus conservative treatment study (OBACT)--the 2-years results of a single centre, prospective, randomised study in patients with intermittent claudication. Eur J Vasc Endovasc Surg. 2007, 33, 3–12. [Google Scholar] [CrossRef]
- Beach, J.M. Revascularization Strategies for Acute and Chronic Limb Ischemia. Cardiol Clin. 2021, 39, 483–494. [Google Scholar] [CrossRef]
- Berchiolli, R.; Bertagna, G.; Adami, D.; Canovaro, F.; Torri, L.; Troisi, N. Chronic Limb-Threatening Ischemia and the Need for Revascularization. J Clin Med. 2023, 12, 2682. [Google Scholar] [CrossRef]
- Khalil, E.; Ozcan, S. Health-related quality of life after vascular surgery and endovascular treatment in subjects with critical limb ischemia. Pak J Med Sci. 2020, 36, 877–883. [Google Scholar] [CrossRef]
- Vlajinac, H.; Marinkovic, J.; Tanaskovic, S.; et al. Quality of life after peripheral bypass surgery: a 1 year follow-up. Wien Klin Wochenschr. 2015, 127, 210–217. [Google Scholar] [CrossRef]
- Alexandrescu, V.; Hubermont, G.; Coessens, V.; et al. Why a multidisciplinary team may represent a key factor for lowering the inferior limb loss rate in diabetic neuro-ischaemic wounds: application in a departmental institution. Acta Chir Belg. 2009, 109, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Caetano, A.P.; Conde Vasco, I.; Veloso Gomes, F.; et al. Successful Revascularization has a Significant Impact on Limb Salvage Rate and Wound Healing for Patients with Diabetic Foot Ulcers: Single-Centre Retrospective Analysis with a Multidisciplinary Approach. Cardiovasc Intervent Radiol. 2020, 43, 1449–1459. [Google Scholar] [CrossRef]
- Tanasescu, D.; Moisin, A.; Fleaca, R.; et al. Modern therapeutic options in diabetic foot ulcer. J Mind Med Sci. 2022, 9, 285–293. [Google Scholar] [CrossRef]
- Liistro, F.; Porto, I.; Angioli, P.; et al. Drug-eluting balloon in peripheral intervention for below the knee angioplasty evaluation (DEBATE-BTK): a randomized trial in diabetic patients with critical limb ischemia. Circulation. 2013, 128, 615–621. [Google Scholar] [CrossRef]
- Liistro, F.; Grotti, S.; Porto, I.; et al. Drug-eluting balloon in peripheral intervention for the superficial femoral artery: the DEBATE-SFA randomized trial (drug eluting balloon in peripheral intervention for the superficial femoral artery). JACC Cardiovasc Interv. 2013, 6, 1295–1302. [Google Scholar] [CrossRef]
- Castro-Dominguez, Y.; Shishehbor, M.H. Team-Based Care in Patients with Chronic Limb-Threatening Ischemia. Curr Cardiol Rep. 2022, 24, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Lozano Navarro, L.V.; Chen, X.; Giratá Viviescas, L.T.; et al. Mesenchymal stem cells for critical limb ischemia: their function, mechanism, and therapeutic potential. Stem Cell Res Ther. 2022, 13, 345, Published 2022 Jul 26. [Google Scholar] [CrossRef]
- Huerta, C.T.; Voza, F.A.; Ortiz, Y.Y.; Liu, Z.J.; Velazquez, O.C. Mesenchymal stem cell-based therapy for non-healing wounds due to chronic limb-threatening ischemia: A review of preclinical and clinical studies. Front Cardiovasc Med. 2023, 10, 1113982, Published 2023 Feb 1. [Google Scholar] [CrossRef] [PubMed]
- Shirbaghaee, Z.; Hassani, M.; Heidari Keshel, S.; Soleimani, M. Emerging roles of mesenchymal stem cell therapy in patients with critical limb ischemia. Stem Cell Res Ther. 2022, 13, 462. [Google Scholar] [CrossRef]
- Babtan, A.M.; Ilea, A.; Feurdean, C.N.; et al. Biostimulation with low-level laser therapy and its effects on soft and hard tissue regeneration. Literature review. J Mind Med Sci. 2022, 9, 28–37. [Google Scholar] [CrossRef]
- Adamičková, A.; Gažová, A.; Adamička, M.; et al. Molecular basis of the effect of atorvastatin pretreatment on stem cell therapy in chronic ischemic diseases - critical limb ischemia. Physiol Res. 2021, 70, S527–S533. [Google Scholar] [CrossRef] [PubMed]
- Arango-Rodríguez, M.L.; Mateus, L.C.; Sossa, C.L.; et al. A novel therapeutic management for diabetes patients with chronic limb-threatening ischemia: comparison of autologous bone marrow mononuclear cells versus allogenic Wharton jelly-derived mesenchymal stem cells. Stem Cell Res Ther. 2023, 14, 221, Published 2023 Aug 25. [Google Scholar] [CrossRef]
- Shan, L.L.; Wang, J.; Westcott, M.J.; et al. A Systematic Review of Cost-Utility Analyses in Chronic Limb-Threatening Ischemia. Ann Vasc Surg. 2022, 85, 9–21. [Google Scholar] [CrossRef]
- Bensley, R.P.; Beck, A.W. Using the Vascular Quality Initiative to improve quality of care and patient outcomes for vascular surgery patients. Semin Vasc Surg. 2015, 28, 97–102. [Google Scholar] [CrossRef]
- Li, Q.; Birmpili, P.; Johal, A.S.; et al. Delays to revascularization for patients with chronic limb-threatening ischaemia. Br J Surg. 2022, 109, 717–726. [Google Scholar] [CrossRef]
- Shatnawi, N.J.; Al-Zoubi, N.A.; Al-Bakkar, L.A.; et al. Chronic Limb-Threatening Ischemia in Patients with Type 2 Diabetes: Revascularization Index as a Predictor for Primary Endovascular Intervention Outcome. Vasc Health Risk Manag. 2023, 19, 495–504, Published 2023 Jul 31. [Google Scholar] [CrossRef] [PubMed]
- Belowski, A.; Partyka, Ł.; Krzanowski, M.; et al. Clinical and linguistic validation of the Polish version of VascuQol: a disease-specific quality-of-life questionnaire assessing patients with chronic limb ischemia. Pol Arch Intern Med. 2019, 129, 167–174. [Google Scholar] [CrossRef]
- Serna Santos, J.; Söderström, M.; Helminen, R.; Aho, P.; Halmesmäki, K.; Venermo, M. Outcome after Hybrid Outflow Interventions for Chronic Limb-threatening Ischemia. Scand J Surg. 2021, 110, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Terabe, Y.; Kaneko, N.; Ando, H. Three years progress chronic limb-threatening ischemia case with simultaneous surgery. Int J Surg Case Rep. 2022, 95, 107212. [Google Scholar] [CrossRef]
- Kobayashi, T.; Kodama, A.; Okazaki, T.; et al. Prognostic Significance of Preoperative Functional Independence Measure (FIM) on Long-Term Outcomes in Patients with Chronic Limb-Threatening Ischemia (CLTI). Ann Vasc Surg. 2022, 83, 275–283. [Google Scholar] [CrossRef]
- Secară, C.A.; Cinteză, O.L.; Popescu, D.; Popa, C.V.; Hîrjeu, C.A.; Voinea, O.C.; Șerbănescu, L.G.; Păuna, A.M.; Tudosie, M.S. Innovative therapeutic approach to chemical burns produced by vesicants; an experimental study. J Mind Med Sci. 2022, 9, 294–303. [Google Scholar] [CrossRef]
- Simon, F.; Duran, M.; Garabet, W.; Schelzig, H.; Jacobs, M.; Gombert, A. Gene Therapy of Chronic Limb-Threatening Ischemia: Vascular Medical Perspectives. J Clin Med. 2022, 11, 1282, Published 2022 Feb 26. [Google Scholar] [CrossRef]
- Vaidya, A.; Kleinegris, M.C.; Severens, J.L.; et al. Comparison of EQ-5D and SF-36 in untreated patients with symptoms of intermittent claudication. J Comp Eff Res. 2018, 7, 535–548. [Google Scholar] [CrossRef] [PubMed]
© 2023 by the author. 2023 Cristian Traian Paius, Vlad Denis Constantin, Alexandru Carap, Andrei Tarus, Grigore Tinica