From COVID-19 to Long COVID: The Forms of the Neurological Manifestations
Abstract
:Introduction
Discussions
Long COVID
- Post-Acute COVID where symptoms last between 3-12 weeks.
- Chronic COVID where symptoms last beyond 12 weeks.
- Fatigue, headache, persistent cough, shortness of breath, sore throat, loss of smell and taste.
- Multiorgan involvement (myocardial infarction, cardiac failure, myocarditis, stroke, altered mental status, post-traumatic stress disorder, neuro-degenerative disorders) with fever and gastrointestinal manifestations (abdominal pain, nausea, irritable bowel syndrome, altered bowel motility).
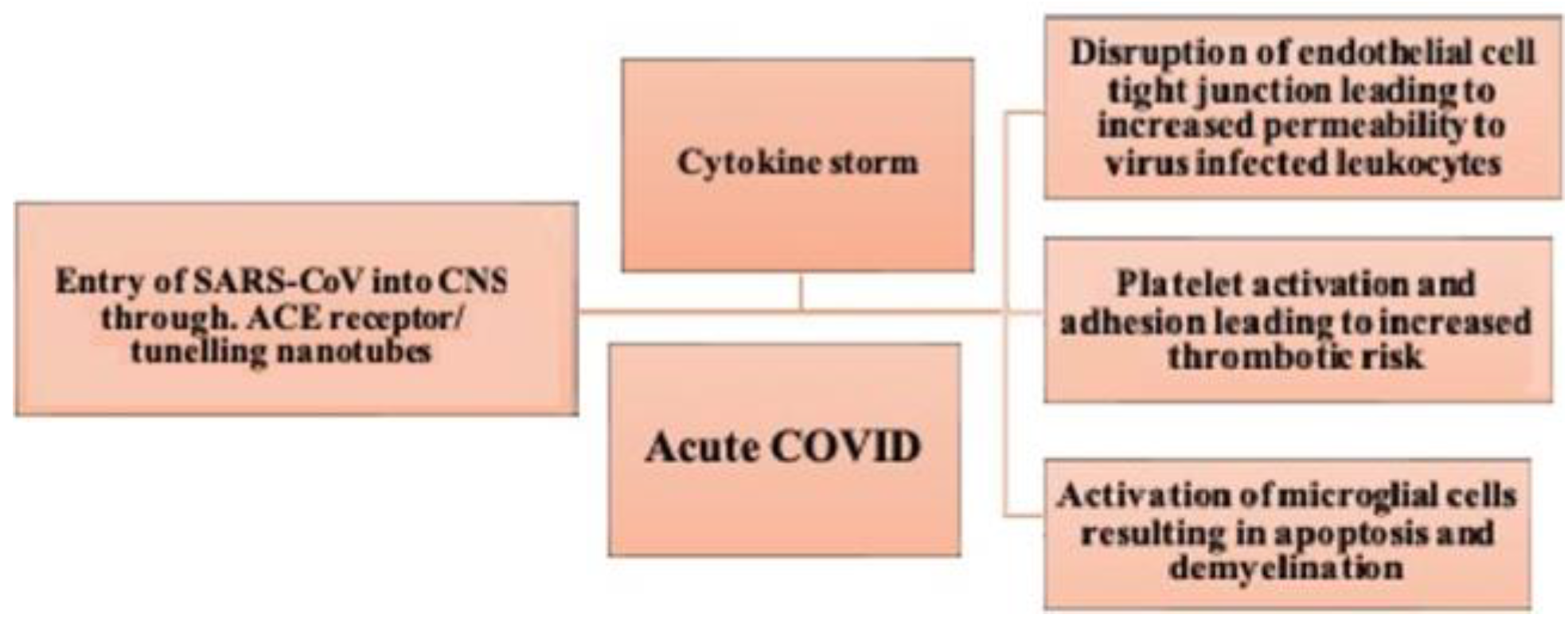
Pathophysiology of Neuropsychiatric Manifestations in COVID-19
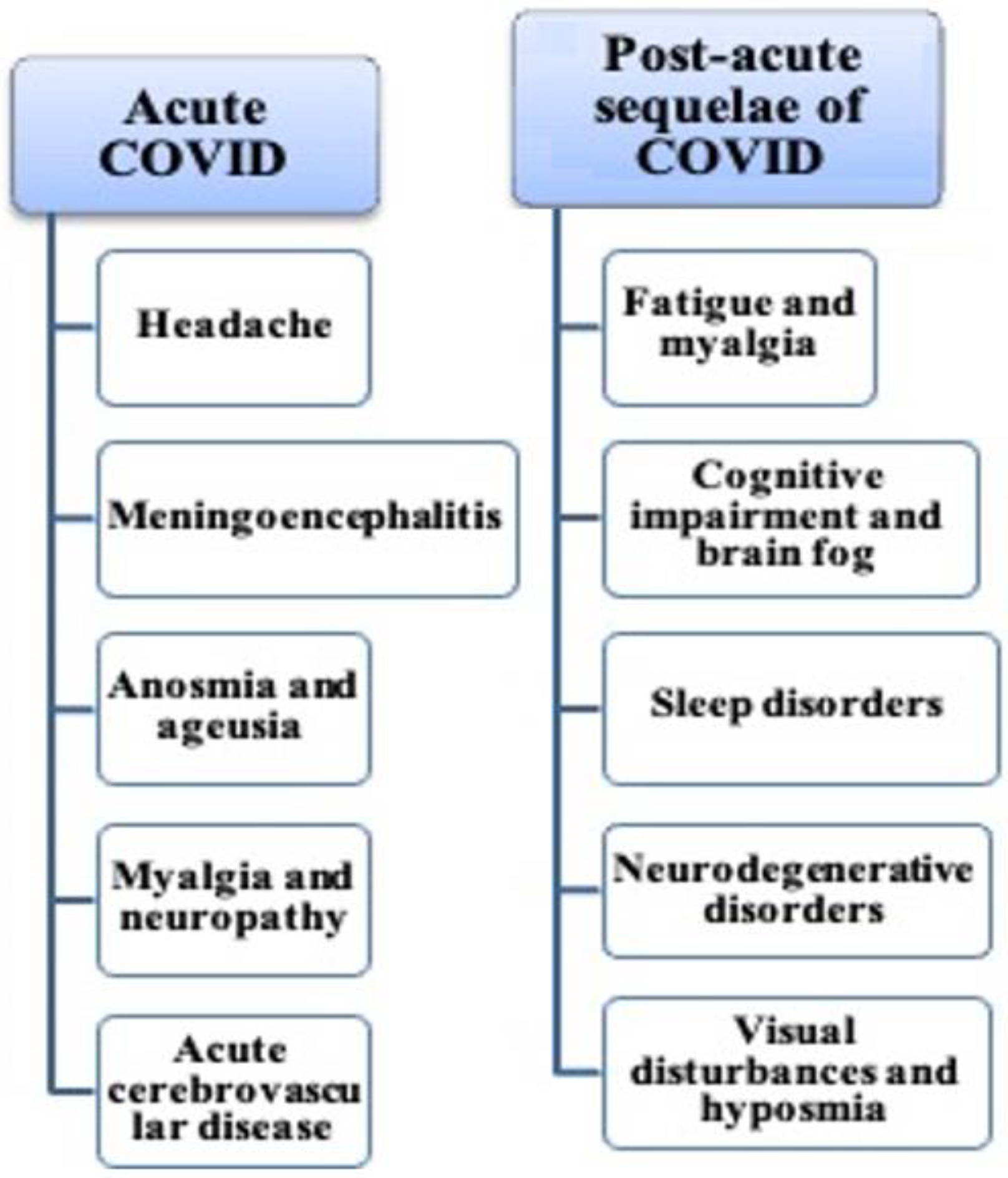
Neurological Manifestations of COVID-19
Headache
Encephalopathy and meningoencephalitis
Anosmia and ageusia
Myalgia and neuropathy
Acute cerebrovascular disease
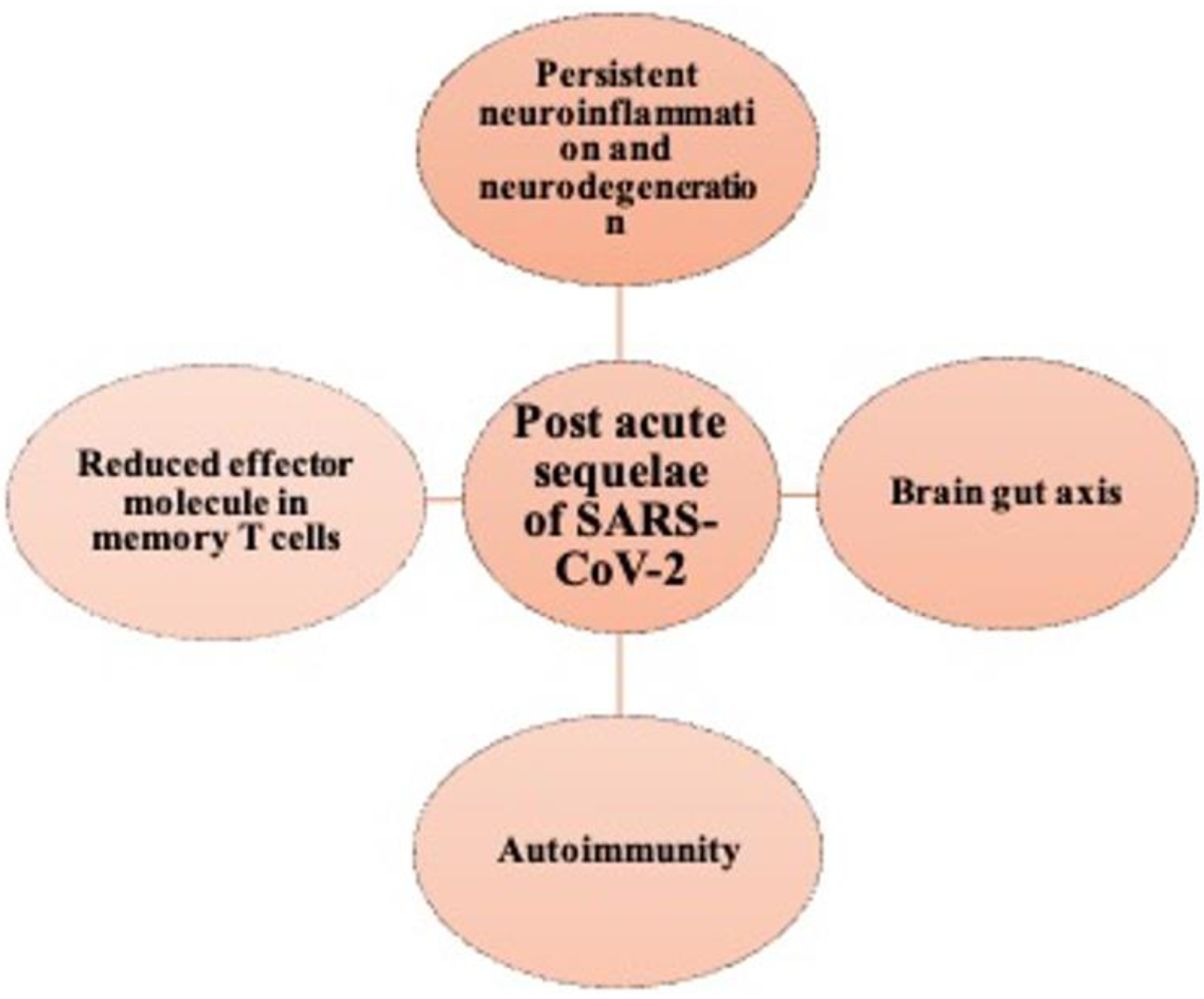
Pathogenesis of PASC
Neurological Sequelae of PASC
Fatigue and myalgia
Cognitive impairment
Sleep disturbances and mood/ anxiety disorders
Neurodegenerative disorders
Alteration in brain structure with COVID-19
Conclusions
Contributions
- Sana Ahuja: Conceptualization, design, literature search, manuscript preparation.
- Sufian Zaheer: Conceptualization, methodology, writing, review and editing, guarantor.
Compliance with ethical standards
Conflict of interest disclosure
References
- WHO COVID-19 Dashboard. Geneva: World Health Organization, 2020. Available online: https://covid19.who.int/ (accessed on 16 August 2022).
- O'Toole, Á.; Scher, E.; Underwood, A.; et al. Assignment of epidemiological lineages in an emerging pandemic using the pangolin tool. Virus Evol. 2021, 7, veab064. [Google Scholar] [CrossRef] [PubMed]
- Gheblawi, M.; Wang, K.; Viveiros, A.; et al. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ Res. 2020, 126, 1456–1474. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.; Wang, B.; Mao, J. The pathogenesis and treatment of the `Cytokine Storm' in COVID-19. J Infect. 2020, 80, 607–613. [Google Scholar] [CrossRef]
- Al-Aly, Z.; Bowe, B.; Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med. 2022, 28, 1461–1467. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Knight, M.; A'Court, C.; Buxton, M.; Husain, L. Management of post-acute covid-19 in primary care. BMJ. 2020, 370, m3026, Published 2020 Aug 11. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; et al. Attributes and predictors of long COVID. Nat Med. 2021, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.K.; Nguyen Truong, S.; Tran Thanh, L.; Le Hoang Gia, N.; Pham Trung, H.; Tran Dinh, B. Post-COVID condition: a survey of patients recovered from COVID-19 in Central Vietnam. J Infect Dev Ctries. 2023, 17, 1213–1220. [Google Scholar] [CrossRef] [PubMed]
- Carfì, A.; Bernabei, R.; Landi, F.; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020, 324, 603–605. [Google Scholar] [CrossRef]
- Troyer, E.A.; Kohn, J.N.; Hong, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020, 87, 34–39. [Google Scholar] [CrossRef]
- Pepe, A.; Pietropaoli, S.; Vos, M.; Barba-Spaeth, G.; Zurzolo, C. Tunneling nanotubes provide a route for SARS-CoV-2 spreading. Sci Adv. 2022, 8, eabo0171. [Google Scholar] [CrossRef]
- Aghagoli, G.; Gallo Marin, B.; Katchur, N.J.; Chaves-Sell, F.; Asaad, W.F.; Murphy, S.A. Neurological Involvement in COVID-19 and Potential Mechanisms: A Review. Neurocrit Care. 2021, 34, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Nalleballe, K.; Reddy Onteddu, S.; Sharma, R.; et al. Spectrum of neuropsychiatric manifestations in COVID-19. Brain Behav Immun. 2020, 88, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Moro, E.; Priori, A.; Beghi, E.; et al. The international European Academy of Neurology survey on neurological symptoms in patients with COVID-19 infection. Eur J Neurol. 2020, 27, 1727–1737. [Google Scholar] [CrossRef]
- Dos Anjos de Paula, R.C.; de Maria Frota Vasconcelos, T.; da Costa, F.B.S.; de Brito, L.A.; et al. Characterization of Headache in COVID-19: a Retrospective Multicenter Study. Mol Neurobiol. 2021, 58, 4487–4494. [Google Scholar] [CrossRef]
- Xu, X.W.; Wu, X.X.; Jiang, X.G.; et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020, 368, m606, Published 2020 Feb 19. [Google Scholar] [CrossRef] [PubMed]
- Varga, Z.; Flammer, A.J.; Steiger, P.; et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Toptan, T.; Aktan, Ç.; Başarı, A.; Bolay, H. Case Series of Headache Characteristics in COVID-19: Headache Can Be an Isolated Symptom. Headache. 2020, 60, 1788–1792. [Google Scholar] [CrossRef]
- Garg, R.K.; Paliwal, V.K.; Gupta, A. Encephalopathy in patients with COVID-19: A review. J Med Virol. 2021, 93, 206–222. [Google Scholar] [CrossRef]
- Nagarajan, P.; Vetrivel, A.; Kumar, J.; Howlader, A.; Rangarajalu, K.; Sabapathy, S.K.; Gopal, M.; Kumar, S. SARSCoV-2 Omicron (B.1.1.529) variant: structural features, biological characteristics, impact on scientific research, general precautions and protective procedures; a systematic review. J Mind Med Sci. 2022, 9, 224–235. [Google Scholar] [CrossRef]
- Beach, S.R.; Praschan, N.C.; Hogan, C.; Dotson, S.; et al. Delirium in COVID-19: A case series and exploration of potential mechanisms for central nervous system involvement. Gen Hosp Psychiatry. 2020, 65, 47–53. [Google Scholar] [CrossRef]
- Chou, S.H.; Beghi, E.; Helbok, R.; et al. Global Incidence of Neurological Manifestations Among Patients Hospitalized With COVID-19-A Report for the GCS-NeuroCOVID Consortium and the ENERGY Consortium. JAMA Netw Open. 2021, 4, e2112131. [Google Scholar] [CrossRef]
- Pilotto, A.; Masciocchi, S.; Volonghi, I.; Crabbio, M.; Magni, E.; De Giuli, V.; et al. Clinical Presentation and Outcomes of Severe Acute Respiratory Syndrome Coronavirus 2-Related Encephalitis: The ENCOVID Multicenter Study. J Infect Dis. 2021, 223, 28–37. [Google Scholar] [CrossRef]
- Benameur, K.; Agarwal, A.; Auld, S.C.; et al. Encephalopathy and Encephalitis Associated with Cerebrospinal Fluid Cytokine Alterations and Coronavirus Disease, Atlanta, Georgia, USA, 2020. Emerg Infect Dis. 2020, 26, 2016–2021. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.; Banks, S.; Bae, C.; Gelber, J.; Alahmadi, H.; Tichauer, M. COVID-19-associated acute disseminated encephalomyelitis (ADEM). J Neurol. 2020, 267, 2799–2802. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.H.; Faraji, F.; Prajapati, D.P.; Ostrander, B.T.; DeConde, A.S. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int Forum Allergy Rhinol. 2020, 10, 821–831. [Google Scholar] [CrossRef] [PubMed]
- Vaira, L.A.; Salzano, G.; Fois, A.G.; Piombino, P.; De Riu, G. Potential pathogenesis of ageusia and anosmia in COVID-19 patients. Int Forum Allergy Rhinol. 2020, 10, 1103–1104. [Google Scholar] [CrossRef]
- Xu, H.; Zhong, L.; Deng, J.; et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020, 12, 8, Published 2020 Feb 24. [Google Scholar] [CrossRef]
- Pushpass, R.G.; Pellicciotta, N.; Kelly, C.; Proctor, G.; Carpenter, G.H. Reduced Salivary Mucin Binding and Glycosylation in Older Adults Influences Taste in an In Vitro Cell Model. Nutrients. 2019, 11, 2280, Published 2019 Sep 24. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Cantador, E.; Núñez, A.; Sobrino, P.; et al. Incidence and consequences of systemic arterial thrombotic events in COVID-19 patients. J Thromb Thrombolysis. 2020, 50, 543–547. [Google Scholar] [CrossRef]
- Nannoni, S.; de Groot, R.; Bell, S.; Markus, H.S. Stroke in COVID-19: A systematic review and meta-analysis. Int J Stroke. 2021, 16, 137–149. [Google Scholar] [CrossRef]
- Hess, D.C.; Eldahshan, W.; Rutkowski, E. COVID-19-Related Stroke. Transl Stroke Res. 2020, 11, 322–325. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, Y.; Liang, X.; et al. COVID-19 Associated Ischemic Stroke and Hemorrhagic Stroke: Incidence, Potential Pathological Mechanism, and Management. Front Neurol. 2020, 11, 571996, Published 2020 Oct 27. [Google Scholar] [CrossRef] [PubMed]
- Valderrama, E.V.; Humbert, K.; Lord, A.; Frontera, J.; Yaghi, S. Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Ischemic Stroke. Stroke. 2020, 51, e124–e127. [Google Scholar] [CrossRef]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond). 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Holeva, V.; Nikopoulou, V.A.; Parlapani, E.; Karkaletsis, K.; Kokkoni, S.; Nouvakis, D.; Theocharis, P.; Diakogiannis, I. Fear of COVID-19, anxiety, depression and suicide among elderly patients with chronic physical or mental diseases. J Mind Med Sci. 2022, 9, 266–275. [Google Scholar] [CrossRef]
- Peluso, M.J.; Deitchman, A.N.; Torres, L.; et al. Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms. Cell Rep. 2021, 36, 109518. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021, 11, 16144. [Google Scholar] [CrossRef]
- Doykov, I.; Hällqvist, J.; Gilmour, K.C.; Grandjean, L.; Mills, K.; Heywood, W.E. 'The long tail of Covid-19' - The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Res. 2020, 9, 1349, Published 2020 Nov 19. [Google Scholar] [CrossRef]
- Wallukat, G.; Hohberger, B.; Wenzel, K.; et al. Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. J Transl Autoimmun. 2021, 4, 100100. [Google Scholar] [CrossRef]
- Wenzel, J.; Schwaninger, M. How COVID-19 affects microvessels in the brain. Brain. 2022, 145, 2242–2244. [Google Scholar] [CrossRef] [PubMed]
- Stefanou, M.I.; Palaiodimou, L.; Bakola, E.; et al. Neurological manifestations of long-COVID syndrome: a narrative review. Ther Adv Chronic Dis. 2022, 13, 20406223221076890, Published 2022 Feb 17. [Google Scholar] [CrossRef] [PubMed]
- Lambadiari, V.; Mitrakou, A.; Kountouri, A.; et al. Association of COVID-19 with impaired endothelial glycocalyx, vascular function and myocardial deformation 4 months after infection. Eur J Heart Fail. 2021, 23, 1916–1926. [Google Scholar] [CrossRef]
- Wu, Y.; Guo, C.; Tang, L.; et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020, 5, 434–435. [Google Scholar] [CrossRef] [PubMed]
- Kanberg, N.; Simrén, J.; Edén, A.; et al. Neurochemical signs of astrocytic and neuronal injury in acute COVID-19 normalizes during long-term follow-up. EBioMedicine. 2021, 70, 103512. [Google Scholar] [CrossRef]
- Twomey, R.; DeMars, J.; Franklin, K.; Culos-Reed, S.N.; Weatherald, J.; Wrightson, J.G. Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Phys Ther. 2022, 102, pzac005. [Google Scholar] [CrossRef]
- Peluso, M.J.; Sans, H.M.; Forman, C.A.; et al. Plasma Markers of Neurologic Injury and Inflammation in People With Self-Reported Neurologic Postacute Sequelae of SARS-CoV-2 Infection. Neurol Neuroimmunol Neuroinflamm. 2022, 9, e200003. [Google Scholar] [CrossRef]
- Pilotto, A.; Cristillo, V.; Cotti Piccinelli, S.; et al. Long-term neurological manifestations of COVID-19: prevalence and predictive factors. Neurol Sci. 2021, 42, 4903–4907. [Google Scholar] [CrossRef]
- Najjar, S.; Najjar, A.; Chong, D.J.; et al. Central nervous system complications associated with SARS-CoV-2 infection: integrative concepts of pathophysiology and case reports. J Neuroinflammation. 2020, 17, 231. [Google Scholar] [CrossRef]
- Komaroff, A.L.; Bateman, L. Will COVID-19 Lead to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome? Front Med (Lausanne). 2021, 7, 606824, Published 2021 Jan 18. [Google Scholar] [CrossRef]
- Morin, C.M.; Bjorvatn, B.; Chung, F.; et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021, 87, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Hartung, T.J.; Neumann, C.; Bahmer, T.; et al. Fatigue and cognitive impairment after COVID-19: A prospective multicentre study. EClinicalMedicine. 2022, 53, 101651. [Google Scholar] [CrossRef] [PubMed]
- Taquet, M.; Sillett, R.; Zhu, L.; et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022, 9, 815–827. [Google Scholar] [CrossRef]
- Xia, X.; Wang, Y.; Zheng, J. COVID-19 and Alzheimer's disease: how one crisis worsens the other. Transl Neurodegener. 2021, 10, 15, Published 2021 Apr 30. [Google Scholar] [CrossRef] [PubMed]
- Schirinzi, T.; Landi, D.; Liguori, C. COVID-19: dealing with a potential risk factor for chronic neurological disorders. J Neurol. 2021, 268, 1171–1178. [Google Scholar] [CrossRef]
- Douaud, G.; Lee, S.; Alfaro-Almagro, F.; et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022, 604, 697–707. [Google Scholar] [CrossRef]
- Long Covid Research Initiative. Available online: https://www.lc19.org/ (accessed on 14 November 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. 2023 Sana Ahuja, Sufian Zaheer
Share and Cite
Ahuja, S.; Zaheer, S. From COVID-19 to Long COVID: The Forms of the Neurological Manifestations. J. Mind Med. Sci. 2023, 10, 209-216. https://doi.org/10.22543/2392-7674.1403
Ahuja S, Zaheer S. From COVID-19 to Long COVID: The Forms of the Neurological Manifestations. Journal of Mind and Medical Sciences. 2023; 10(2):209-216. https://doi.org/10.22543/2392-7674.1403
Chicago/Turabian StyleAhuja, Sana, and Sufian Zaheer. 2023. "From COVID-19 to Long COVID: The Forms of the Neurological Manifestations" Journal of Mind and Medical Sciences 10, no. 2: 209-216. https://doi.org/10.22543/2392-7674.1403
APA StyleAhuja, S., & Zaheer, S. (2023). From COVID-19 to Long COVID: The Forms of the Neurological Manifestations. Journal of Mind and Medical Sciences, 10(2), 209-216. https://doi.org/10.22543/2392-7674.1403


