Anxio-Depressive Disorders in a Pandemic Context: A Comparative Analysis: Year 2019 Versus 2020
Abstract
:Introduction
Materials and Methods
Results
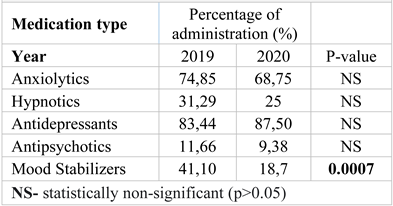
Discussions
Conclusions
Highlights
- ✓
- The COVID-19 pandemic led to an aggravation of the anxiety disorders because of isolation and fear of disease. In 2020 there were both fewer consultations and admissions compared to 2019.
- ✓
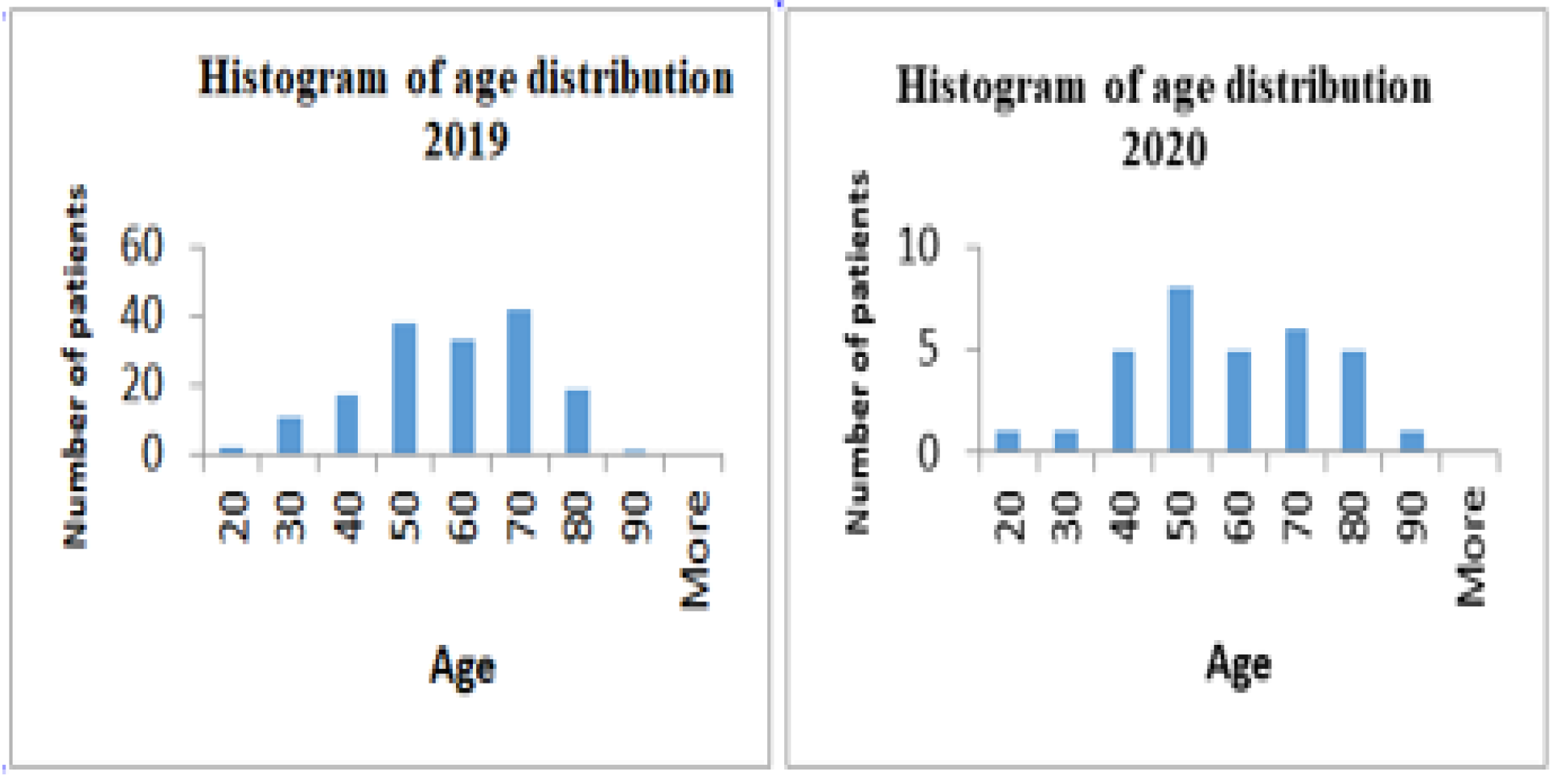
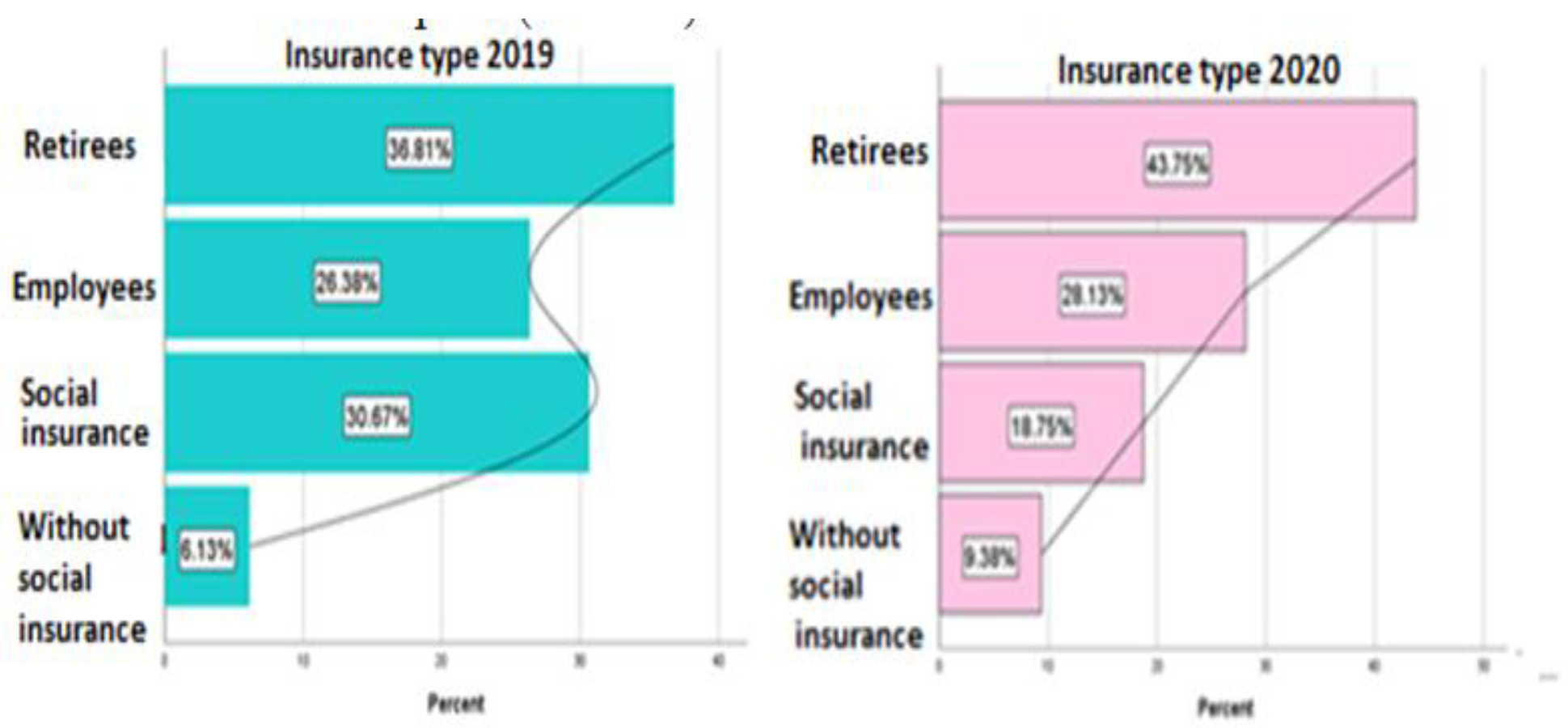
- There was no significant difference for age or gender between the groups. The average age for anxiety disorders is 53 years. In 2020 urban patients predominated, but the difference was not significant.
- ✓
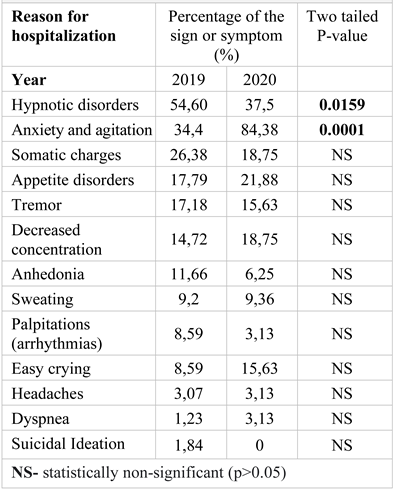
- More patients presented anxiety and psychomotor agitation in 2020.
Compliance with ethical standards
Conflict of interest disclosure
References
- Yamin, N.; Brown, T.A.; Rosellini, A.J. Longitudinal associations of chronic health stress and COVID-19-related anxiety among outpatients with anxiety and mood disorders [published online ahead of print, 2023 Apr 19]. Clin Psychol Psychother 2023, 10.1002/cpp.2852. [Google Scholar] [CrossRef]
- Noij, L.; Haarman, E.; Hashimoto, S.; et al. Depression, anxiety, and resilience during COVID-19 in Dutch patients with cystic fibrosis or primary ciliary dyskinesia and their caregivers [published online ahead of print, 2023 Apr 21]. Pediatr Pulmonol 2023, 10.1002/ppul.26427. [Google Scholar] [CrossRef]
- Paxton Willing, M.M.; Tate, L.L.; O'Gallagher, K.G.; Evatt, D.P.; Riggs, D.S. In-Theater Mental Health Disorders Among U. S. Soldiers Deployed Between 2008 and 2013. MSMR. 2022, 29, 11–17, Published 2022 Nov 1. [Google Scholar] [PubMed]
- Wolf, K.; Schmitz, J. Scoping review: longitudinal effects of the COVID-19 pandemic on child and adolescent mental health [published online ahead of print, 2023 Apr 21]. Eur Child Adolesc Psychiatry 2023, 10.1007/s00787-023-02206-8. [Google Scholar] [CrossRef]
- Mirucka, B.; Bielecka, U.; Mirucka, M.A. How do threat to life and state anxiety disturb the psychological functioning of Polish adults during coronavirus pandemic? Psychiatr Pol. 2022, 56, 957–967. [Google Scholar] [CrossRef]
- Merlo, E.M.; MacKenzie Myles, L.A.; Pappalardo, S.M. The VESPA Project: Virtual Reality Interventions for Neurocognitive and Developmental Disorders. J Mind Med Sci. 2022, 9, 16–27. [Google Scholar] [CrossRef]
- Andrews, J.L.; Li, M.; Minihan, S.; et al. The effect of intolerance of uncertainty on anxiety and depression, and their symptom networks, during the COVID-19 pandemic. BMC Psychiatry. 2023, 23, 261, Published 2023 Apr 17. [Google Scholar] [CrossRef]
- Burke-Garcia, A.; Berktold, J.; et al. Assessment of Mental Health and Coping Disparities Among Racial and Ethnic Groups Amid COVID-19 From the "How Right Now" Campaign. Public Health Rep. 2023, 138, 174–182. [Google Scholar] [CrossRef]
- Ogunleye, O.O.; Basu, D.; Mueller, D.; et al. Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: Successes, Challenges, and Implications for the Future. Front Pharmacol. 2020, 11, 1205, Published 2020 Sep 11. [Google Scholar] [CrossRef]
- Cono, J.; Casey, C.G.; Bell, D.M.; Centers for Disease Control and Prevention. Smallpox vaccination and adverse reactions. Guidance for clinicians. MMWR Recomm Rep. 2003, 52, 1–28. [Google Scholar]
- Fountoulakis, K.N.; Karakatsoulis, G.N.; Abraham, S.; et al. Results of the COVID-19 mental health international for the health professionals (COMET-HP) study: depression, suicidal tendencies and conspiracism [published online ahead of print, 2023 Mar 3]. Soc Psychiatry Psychiatr Epidemiol. 2023, 1–24. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020, 16, 57, Published 2020 Jul 6. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Solomou, I.; Constantinidou, F. Prevalence and Predictors of Anxiety and Depression Symptoms during the COVID-19 Pandemic and Compliance with Precautionary Measures: Age and Sex Matter. Int J Environ Res Public Health. 2020, 17, 4924, Published 2020 Jul 8. [Google Scholar] [CrossRef]
- Lijster, J.M.; Dierckx, B.; Utens, E.M.; et al. The Age of Onset of Anxiety Disorders. Can J Psychiatry. 2017, 62, 237–246. [Google Scholar] [CrossRef]
- Banstola, A.; Pokhrel, S.; Hayhoe, B.; Nicholls, D.; Harris, M.; Anokye, N. Economic evaluations of interventional opportunities for the management of mental-physical multimorbidity: a systematic review. BMJ Open. 2023, 13, e069270, Published 2023 Feb 28. [Google Scholar] [CrossRef]
- Anker, J.J.; Kushner, M.G. Co-Occurring Alcohol Use Disorder and Anxiety: Bridging Psychiatric, Psychological, and Neurobiological Perspectives. Alcohol Res. 2019, 40, arcr.v40–1.03, Published 2019 Dec 30. [Google Scholar] [CrossRef]
- Rogers, M.P.; White, K.; Warshaw, M.G.; et al. Prevalence of medical illness in patients with anxiety disorders. Int J Psychiatry Med. 1994, 24, 83–96. [Google Scholar] [CrossRef]
- Holeva, V.; Nikopoulou, V.A.; Parlapani, E.; Karkaletsis, K.; Kokkoni, S.; Nouvakis, D.; Theocharis, P.; Diakogiannis, I. Fear of COVID-19, anxiety, depression and suicide among elderly patients with chronic physical or mental diseases. J Mind Med Sci. 2022, 9, 266–275. [Google Scholar] [CrossRef]
- Erden, S.C.; Uygur, A.B.; Karakus, K. Evaluation of Coronavirus Anxiety Levels and Coping Strategies of Major Depressive Disorder, Generalized Anxiety Disorder, and Panic Disorder Patients During the Covid-19 Pandemic. Sisli Etfal Hastan Tip Bul. 2023, 57, 33–45. [Google Scholar] [CrossRef]
- Bossola, M.; Ciciarelli, C.; Di Stasio, E.; et al. Relationship between appetite and symptoms of depression and anxiety in patients on chronic hemodialysis. J Ren Nutr. 2012, 22, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Henry, C.; Van den Bulke, D.; Bellivier, F.; Etain, B.; Rouillon, F.; Leboyer, M. Anxiety disorders in 318 bipolar patients: prevalence and impact on illness severity and response to mood stabilizer. J Clin Psychiatry. 2003, 64, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Babtan, A.M.; Ilea, A.; Feurdean, C.N.; et al. Biostimulation with low-level laser therapy and its effects on soft and hard tissue regeneration. Literature review. J Mind Med Sci. 2022, 9, 28–37. [Google Scholar] [CrossRef]
- Moroianu, L.A.; Cecilia, C.; Ardeleanu, V.; Pantea Stoian, A.; Cristescu, V.; et al. Clinical Study of Serum Serotonin as a Screening Marker for Anxiety and Depression in Patients with Type 2 Diabetes. Medicina. 2022, 58, 652. [Google Scholar] [CrossRef]
- Adamo, D.; Calabria, E.; Canfora, F.; et al. Anxiety and depression in keratotic oral lichen planus: a multicentric study from the SIPMO [published online ahead of print, 2023 Feb 14]. Clin Oral Investig 2023, 10.1007/s00784-023-04909-3. [Google Scholar] [CrossRef]
- Han, C.; Wang, S.M.; Kato, M.; et al. Second-generation antipsychotics in the treatment of major depressive disorder: current evidence. Expert Rev Neurother. 2013, 13, 851–870. [Google Scholar] [CrossRef]
- Sisu, A.M.; Noditi, G.; Grigorescu, D.; Florescu, S.; Patrascu, J.M.; Patrascu Jr, J.M.; Pop, E.; Bolintineanu, S.L. The Benefits of the Plastination Techniques for the Anatomo Clinical Studies of Ankle Joint Ligaments Injuries. Materiale Plastice 2017, 54, 487–490. [Google Scholar] [CrossRef]
- Batelaan, N.M.; Bosman, R.C.; Muntingh, A.; Scholten, W.D.; Huijbregts, K.M.; van Balkom, A.J.L.M. Risk of relapse after antidepressant discontinuation in anxiety disorders, obsessive-compulsive disorder, and post-traumatic stress disorder: systematic review and meta-analysis of relapse prevention trials. BMJ. 2017, 358, j3927, Published 2017 Sep 13. [Google Scholar] [CrossRef]
- Papachristou, S.; Stamatiou, I.; Stoian, A.P.; Papanas, N. New-Onset Diabetes in COVID-19: Time to Frame Its Fearful Symmetry. Diabetes Ther. 2021, 12, 461–464. [Google Scholar] [CrossRef]
- Pantea-Stoian, A.; Toth, P.P.; Kempler, P.; Rizzo, M. Gender differences in the battle against COVID-19: Impact of genetics, comorbidities, inflammation and lifestyle on differences in outcomes. Int J Clin Pract. 2021, 75, e13666. [Google Scholar] [CrossRef]
- Moroianu, L.A.; Motofei, I.G.; Curis, C.; Barbu, R.E.; Toma, A. The Impact Of Anxiety And Depression On The Pediatric Patients With Diabetes. Mediterr. J. Clin. Psychol. 2020, 8. [Google Scholar] [CrossRef]
- Curis, C.; Ciubară, A.B.; Nechita, A.; Nechita, L.; Kantor, C.; Moroianu, L.A. The role of motivational interview in treatment acceptance – case report. The Medical-Surgical Journal. 2018, 122, 375–380. Available online: https://www.revmedchir.ro/index.php/revmedchir/article/view/1172/1021.
- Nițoi, L.; Moroianu, L.A. Serum Hemoglobin level and quality of life in end stage. The Medical-Surgical Journal. 2120, 24, 381–387. Available online: https://www.revmedchir.ro/index.php/revmedchir/article/download/2208/1673.
- Cotel, A.; Golu, F.; Pantea Stoian, A.; et al. Predictors of Burnout in Healthcare Workers during the COVID-19 Pandemic. Healthcare (Basel). 2021, 9, 304, Published 2021 Mar 9. [Google Scholar] [CrossRef]
- Chalmers, S.; Harrall, K.; Wong, S.Y.; Kablan, W.; Clunie, G. A retrospective study of patients presenting with speech and language therapy needs within multidisciplinary Long COVID services: A service evaluation describing and comparing two cohorts across two NHS Trusts [published online ahead of print, 2023 Mar 14]. Int J Lang Commun Disord 2023, 10.1111/1460-6984.12868. [Google Scholar] [CrossRef]
 |
 |
 |
© 2023 by the author. 2023 Andreea Roxana Droahnă, Lavinia-Alexandra Moroianu, Valeria-Anca Pietrosel, Cristina Ioana Bica, Teodor Salmen, Cecilia Curis, Emanuele Maria Merlo, Roxana Adriana Stoica, Marius Moroianu
Share and Cite
Droahnă, A.R.; Moroianu, L.-A.; Pietroșel, V.-A.; Bica, C.I.; Salmen, T.; Curis, C.; Merlo, E.M.; Stoica, R.A.; Moroianu, M. Anxio-Depressive Disorders in a Pandemic Context: A Comparative Analysis: Year 2019 Versus 2020. J. Mind Med. Sci. 2023, 10, 156-162. https://doi.org/10.22543/2392-7674.1392
Droahnă AR, Moroianu L-A, Pietroșel V-A, Bica CI, Salmen T, Curis C, Merlo EM, Stoica RA, Moroianu M. Anxio-Depressive Disorders in a Pandemic Context: A Comparative Analysis: Year 2019 Versus 2020. Journal of Mind and Medical Sciences. 2023; 10(1):156-162. https://doi.org/10.22543/2392-7674.1392
Chicago/Turabian StyleDroahnă, Andreea Roxana, Lavinia-Alexandra Moroianu, Valeria-Anca Pietroșel, Cristina Ioana Bica, Teodor Salmen, Cecilia Curis, Emanuele Maria Merlo, Roxana Adriana Stoica, and Marius Moroianu. 2023. "Anxio-Depressive Disorders in a Pandemic Context: A Comparative Analysis: Year 2019 Versus 2020" Journal of Mind and Medical Sciences 10, no. 1: 156-162. https://doi.org/10.22543/2392-7674.1392
APA StyleDroahnă, A. R., Moroianu, L.-A., Pietroșel, V.-A., Bica, C. I., Salmen, T., Curis, C., Merlo, E. M., Stoica, R. A., & Moroianu, M. (2023). Anxio-Depressive Disorders in a Pandemic Context: A Comparative Analysis: Year 2019 Versus 2020. Journal of Mind and Medical Sciences, 10(1), 156-162. https://doi.org/10.22543/2392-7674.1392



