Abstract
Laparoscopic surgery in patients with ventriculo-peritoneal shunt is challenging in terms of technical approach. The severity of possible complications and the lack of studies on this association increase the surgeon's discomfort with such surgery. The main complications that may occur are increased intracranial pressure, secondary pneumo-peritoneum pneumocephalus, encephalitis and the risk of catheter injury during laparoscopic procedures. We present the case of a 56-year-old patient operated in 2004 for a basilar artery top aneurysm with subarachnoid hemorrhage and secondary hydrocephalus, for which a ventriculo-peritoneal shunt was fitted. This patient presented in our clinic with diffuse abdominal pain, more accentuated in the right hypochondrium, nausea, postprandial biliary vomiting, inappetence, asthenia, fatigability, symptoms with onset about 6 months, but accentuated in the last 48 h. The patient underwent surgery and the evolution was favorable, being discharged without postoperative complications.
Introduction
Laparoscopy has become the standard approach for many surgical procedures, cholecystectomy being one of the most frequently performed [1,2,3]. However, it has been rarely described in patients with ventriculo-peritoneal (VP) shunt; on one hand, due to the low frequency of association between acute cholecystitis and ventriculo-peritoneal shunt, on the other hand due to the surgeon's reluctance to perform a laparoscopic procedure in a patient with such ventriculo-peritoneal shunt [2]. Although laparoscopic cholecystectomy is a well standardized procedure, which can be easily performed even in day care centers, in such patients the risk of associated complications during surgery is significantly higher [4,5]. Although these cases are rare, the surgical team must be aware of such possible complications in order to recognize and avoid them [4].
Hydrocephalus is an abnormal accumulation of cerebrospinal fluid (CSF) in the ventricles of the brain. The aetiology is variable and includes apeductal stenosis, myelomeningocele, intracranial hemorrhages, meningitis, tumours and traumatic brain injury [6]. Treatment involves shunting CSF to another area of the body, which is usually the abdominal cavity. Ventriculo-peritoneal shunting is the most common approach because distal catheter placement is technically simple and surgical revision is rare [6].
The first procedure to place a VP shunt was performed in 1908 and has since become a common neurosurgical procedure [2,7]. In 1995, of approximately 70.000 patients with hydrocephalus in the United States, nearly 33.000 of them required a VP shunt [4,7].
Currently in the United States the incidence per year of new cases of patients requiring a VP shunt is approximately 30.000 cases and the prevalence of cases exceeds 125.000 [8,9]. At the same time, according to a 10-year study in the UK and Ireland, approximately 42.000 VP shunt-placement procedures were performed [10]. The most common pathologies in infants and children requiring drainage were perinatal intraventricular hemorrhages (35.3%), brain tumours (40.5%) and congenital malformations (50.2%), while in adults the most common pathologies were normotensive hydrocephalus (14.2%), post-hemorrhagic hydrocephalus (16.2%) and brain tumours (24.6%) [10]. Mortality from this procedure is quite low, about 0.1%, but 3-15% of shunts can become infected and about 50% of them become non-functional after 2 years [11].
Important issues to consider when performing laparoscopic surgeries in these patients include knowing the type of shunt, as well as knowing its path from the lateral ventricle to the peritoneum, the potential for shunt malfunction, pneumocephalus, shunt infection, intra-operative anaesthesia monitoring, and shunt handling during surgery [2]. Laparoscopic surgery in patients with VP shunt has been described in procedures such as cholecystectomy, salpingectomy, ileocecal resection, colectomy, gastrectomy, adrenal surgery, ileostomies and bladder neck reconstruction [12].
Different approaches to shunt manipulation have been reported to allow laparoscopic surgery, either by simply ligating the shunt or by completely externalizing the shunt and draining the cerebrospinal fluid for several days [2]. These measures were taken to reduce the risk of infection and to avoid the development of pneumocephalus and increased intracranial pressure; the major concern facing the medical team at the time of surgery is the potential risk of developing pneumocephalus secondary to pneumo-peritoneum [2]. Also, the risk of catheter injury is extremely high when its topography is unknown.
Case Presentation
The aim of this paper is to illustrate the challenge of laparoscopic cholecystectomy in a patient with ventriculo-peritoneal shunt, the risks represented both by increased intra-abdominal pressure (IAP) with the risk of shunt failure and the occurrence of pneumocephalus, shunt injury during insertion of trocars, infection with the occurrence of encephalitis, and finally to depict a review of the literature.
We present the case of a 56-year-old patient operated in 2004 for a basilar artery top aneurysm with subarachnoid hemorrhage and secondary hydrocephalus, for which a ventriculo-peritoneal shunt (Unishunt type) was fitted and who presents to the Sibiu Emergency County Clinical Hospital, with diffuse abdominal pain, more accentuated in the right hypochondrium, nausea, postprandial biliary vomiting, inappetence, asthenia, fatigability, symptoms with onset about 6 months, but accentuated in the last 48 hours.
On physical exam the patient was in good general condition, conscious, cooperative, afebrile, hemo-dynamically and cardio-respiratory stable. Clinical exam revealed abdomen above the xipho-pubic plane due to excess adipose tissue, slightly tender to palpation in the right hypochondrium, positive Murphy sign. The Sars-Cov-2 test was negative. Laboratory tests showed a biological inflammatory syndrome, while abdominal ultrasonography steatosis and multiseptated gallbladder, with hyperechogenic images with posterior acoustic shadowing, up to 1 cm in size, slightly thickened walls (suggestive of acute lithiasic cholecystitis) (Figure 1). No fluid collections were detected in the peritoneal spaces to assess shunt patency.

Figure 1.
Gallbladder with multiple hyperechogenic images, with posterior acoustic shadowing, located at the infundibulum - sonographic appearance suggestive of acute lithiasic cholecystitis
Soft-tissue ultrasound examination to identify the topography of the ventriculo-peritoneal shunt was performed with the patient positioned in anti-Trendelenburg at a 20° angle and slightly to the left, so that the skin marking corresponded to that in the operative position. Thus, the course and position of the ventriculo-peritoneal shunt (Figure 2) were traced by skin marking to guide us where the supraumbilical incision trocar for the Veress needle and the first (the subxiphoid) working trocar, should be inserted.

Figure 2.
Skin marking: site of entry in the peritoneal cavity
The ultrasound depicts the shunt as having a shallow trajectory from the right latero-cervical region to the epigastrium (Figure 3), from where it enters deeply, the access at the peritoneal cavity being located in the right paraumbilical area, but without being able to visualize the distal end (Figure 4). Neurosurgical consultation was subsequently performed, which recommended temporary shunt ligation. Suturing and ligation of the shunt was performed with the recommendation of ligature thread suppression 24 hours postoperatively and reassessment as needed.
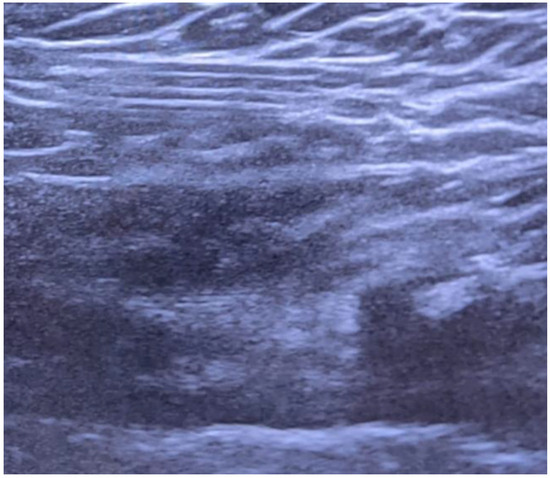
Figure 3.
Superficial shunt pathway in subcutaneous tissue
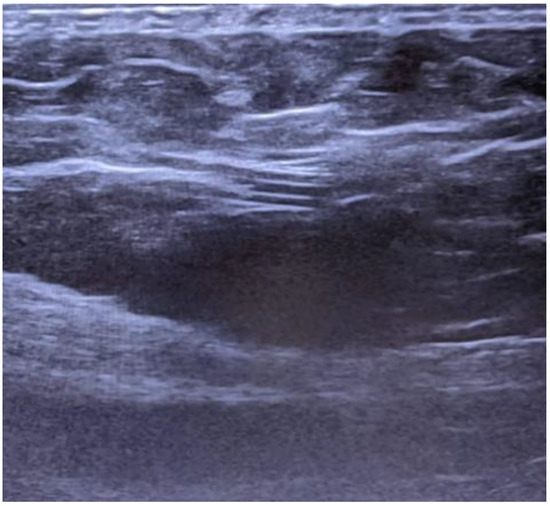
Figure 4.
Distal-end catheter entry in the peritoneal cavity
After adequate preoperative preparation, surgery was performed under general anaesthesia with orotracheal intubation, laparoscopic cholecystectomy, viscerolysis due to pericholecystic adhesions, lavage, subhepatic drainage. The surgery did not involve any other special surgical procedures. Postoperative evolution was favourable under conservative treatment with antibiotics, analgesics, antispasmodics, anti-inflammatory, antiemetics and hydro-electrolytic rebalancing therapy. The shunt ligature was transected through an incision. The patient was discharged in good general condition, conscious, cooperative, afebrile, hemodynamically and cardio-respiratory stable. The drain tube was permeable with 100 ml serocitrin drainage, so that it was suppressed the next postoperative day.
Pathological examination of the postoperative specimen described a gallbladder with multiple stones, 5-7 mm in diameter, with mucosa lined by a simple cylindrical epithelium, forming Rokitansky-Ashoff sinuses penetrating the muscular layer, which appeared hypertrophied with adjacent fibrosis. A rich mixed inflammatory infiltrate, predominantly neutrophilic, was seen in all layers. The blood vessels were congestive with hematic extravasation in all layers, more accentuated in the muscle and subserous. The final diagnosis was chronic cholecystitis in an acute stage.
The patient was discharged in good general condition, surgically healed. Recommendations were to maintain a healthy diet, avoid strenuous physical exertion, daily local compresses with antiseptic solutions, dispensing of associated conditions through the general practitioner and neurosurgical consultation through the outpatient clinic as needed.
Discussions
Brain shunts are indicated in patients with hydrocephalus to drain CSF into a cavity, to prevent an increase in intracranial pressure [12]. They consist of a silicone portion located in the lateral ventricle, the newer ones have a one-way only valve-mechanism and a free distal end, usually in the peritoneal cavity [12]. The unidirectional valve is intended to prevent reflux of cerebrospinal fluid or intraperitoneal collections [12].
The proximal end is inserted at the level of the non-dominant cerebral hemisphere, in the frontal horn of the lateral ventricle because the risk of blockage is low, the choroid plexus being less represented in this region [10]. From the lateral ventricle it is tunneled through the subcutaneous tissue to the peritoneal cavity for CSF drainage [13].
The second component of the drainage system, the valve, maintains unidirectional (cranio-caudal) flow and works by regulating CSF drainage [12]. This control occurs primarily through pressure regulation, flow regulation (flow control valves) and anti-siphon mechanisms [12]. A patent and functional shunt relieves increased intracranial pressure (ICP) secondary to hydrocephalus by continuously draining cerebrospinal fluid into the abdomen [12]. The unidirectional valve plays a role in preventing CSF reflux and intra-abdominal fluid [13].
We noted that our patient received an older shunt model that did not have a unidirectional valve. These older models being used frequently in post-hemorrhagic hydrocephalus, patients may benefit from a shorter hospital stay [14].
Post-hemorrhagic hydrocephalus occurs secondary to blood degradation products and extensive fibrosis in the leptomeninges and arachnoid granulations, reducing CSF circulation and uptake at this level [15]. The degree of hydrocephalus is also influenced by the therapeutic technique used; open-surgery procedures facilitate drainage of blood clots compared to endovascular treatment, and would allow better drainage, reducing the likelihood of chronic hydrocephalus [15].
In the case of valved shunts, the pressure at which the valve opens is called the set pressure [12]. There are low, medium and high-pressure valves referring to opening pressures of 5, 10 and 15 cm H2O respectively [12]. Most valves are designed to open and allow CSF flow when the intraventricular pressure rises above the opening pressure [12]. Once the proximal pressure falls below the closing pressure, the valve closes and CSF flow stops [12,16,17]. Distal end insertion can be done in several compartments, the other routes often used are ventriculo-atrial, ventriculo-pleural and lumbo-peritoneal shunts [16].
The physical principle behind the use of CSF shunts is quite simple and consists of diverting CSF flow either to intracranial structures, jugular system, right atrium, pleura, peritoneum or to other natural cavities such as the omental bursa [12,18,19]. All systems work by means of differential pressure (DP) between the proximal (ventricular) and distal (most commonly peritoneal) catheter [12]. There are several physical factors involved in cerebrospinal fluid drainage, such as the pressure difference between catheter ends, patient position, tube diameter and length, and fluid viscosity [12,19,20].
Stevin's hydrodynamic laws postulate that in connected hydrostatic systems and following the principle of communicating vessels, the pressure at a point varies with the height of the fluid column [9,16]. Thus, if two compartments are connected by a fluid conduit, flow will be directed from the place with the highest pressure to the place with the lowest pressure [12,19,20].
Intra-abdominal pressure (IAP) is a physiological pressure, defined as the steady-state pressure in the abdominal cavity [21]. Values up to 5 mm Hg are considered normal in adults under physiological conditions [21]. Intracranial pressure (ICP) is the pressure exerted by CSF and blood, and changes in ICP are attributed to changes in the volume of these constituents [21].
Current evidence strongly supports that intra-abdominal pressure is transmitted to the central nervous system via two pathways [22]. One pathway is retrograde flow through the venous plexus of the spinal canal and intracranial veins, and the second pathway is directly transferred to the thoracic compartment, which in turn results in increased jugular vein pressure and decreased CSF and blood drainage, leading to an increase in ICP [22]. Pneumoperitoneum created during laparoscopic surgery can increase ICP by various mechanisms, such as cerebral arteriolar vasodilation through hypercapnia or cerebral venous vasodilation through increased pressure on vena cava [22]. The correlations between intra-abdominal pressure and intracranial pressure have been confirmed by numerous animal studies [22].
Mohamed et al. studied the effects of increased AIP on ICP and cerebral perfusion pressure (CPP) on pigs [21]. They increased the AIP to 25 mmHg above baseline by inflating a balloon inserted into the peritoneal cavity, while measuring changes in ICP, demonstrating a significant and linear increase in ICP with increasing AIP, concluding that an increased AIP will lead to increased ICP and decreased CPP [21].
In 2004, Rad et al. reported a laparoscopic resection of an ovarian cyst and described the benefit of using transcranial Doppler ultrasound examination [23]. There was no difference in cerebral blood flow when the patient was positioned in Trendelenburg with an insufflation pressure of 10 mmHg [23]. However, there was a decrease in cerebral blood flow when the abdominal pressure reached 15 mmHg, but with a subsequent rapid improvement when the pressure dropped back to 10 mmHg [23].
In another animal study, Mohamed et al. studied the effect of pneumoperitoneum on ICP by recording arterial blood gas, mean arterial pressure (MAP) and ICP values at different values of AIP, both supine and in Trendelenburg [21]. They demonstrated a significant and linear increase in ICP with increased ICP values related to Trendelenburg position [21]. The association of Trendelenburg position favored increased IAP values of 16 mmHg and an ICP value growth of more than 150% [21]. They concluded that the surgeon should consider ICP and patient positioning when performing laparoscopic procedures, especially in patients with traumatic brain injury, cerebral aneurysms and associated conditions with increased ICP [21].
Modern techniques for indirect assessment of ICP include ultrasound measurement of optic nerve sheath diameter as a non-invasive indicator of increased intracranial pressure (ICP) [24]. The linear probe of the ultrasound machine is used, with a frequency of 7.5 MHz, placed gently on the superior and lateral side of the upper eyelid and tilted slightly caudal and medial until an axial view of the orbit is obtained and an image of the optic nerve is shown [24]. The sliders are placed on the outer contours of the dural sheath, 3 mm behind the eyeball, and the horizontal distance between two sliders is measured [24]. Normal values are in the range of 0.45-0.5 cm [24].
Differential diagnosis of acute abdominal pain in emergency is particularly challenging in patients with ventriculoperitoneal shunt. In these cases, among other possible pathologies such as perforated ulcer, acute appendicitis, Amyand hernia, or mesenteric ischemia, shunt related causes have to be also taken into account [25,26,27,28].
The safety of laparoscopic surgery in patients with ventriculo-peritoneal shunt has always been controversial [21]. Currently, there is no solid evidence to establish a consensus on the safety of the procedure in these patients [21]. There is still controversy about the safety of performing laparoscopic surgery in patients with VP shunt [29]. Unfortunately, there is little published data on the management of peri- and postoperative complications in laparoscopic surgery in patients with ventriculo-peritoneal shunt due to the small number of reported cases and the lack of meta-analyses [29]. Therefore, we strongly believe that each case should be revealed, in order to build an evidence-base that would allow future studies to be conducted.
Studies conducted by Sankpal et al. have shown that there is no evidence of increased clinically significant intracranial pressure in most patients with VP shunts undergoing laparoscopic surgery, with peri- and postoperative anesthetic monitoring being sufficient [16]. However, the study conducted by Li et al. recommends preoperative neurosurgical consultation to check the function of the VP shunt, identification of its pathway in the abdominal wall to avoid inadvertent damage during insertion of the working trocar, and checking the distal intraperitoneal portion of the catheter before abdominal decompression [30].
Mohamed et al. further suggested that pneumo-peritoneum may decrease patency through the distal peritoneal catheter, causing partial or complete shunt obstruction [21]. The risk of retrograde passage of CO2 from the abdomen to the brain is minimal with advances in biomaterials and biomedical engineering, but also with the occurrence of unidirectional valved ventriculo-peritoneal shunt catheters that can withstand much higher intra-abdominal pressures [21]. The hydro-dynamic profile of the shunt valve, as reported by catheter manufacturers, is a standard parameter indicating the opening pressure of the valve, the newer unidirectional valve catheters can withstand up to a pressure of 300 mmHg, while the pressure used in laparoscopy being 12-15 mmHg [21].
The risk of shunt valve malfunction (in vitro model) was studied on nine different shunts, subjected to increased back pressure, none of which failed [21]. The risk of valve failure is minimal even at IAPs up to 80 mmHg [18]. Similarly, other authors studied five different types of valves in a closed system, with no back pressure up to 25 mmHg [21].
Sankpal et al. observed 19 laparoscopic surgeries in patients with ventriculo-peritoneal shunts, with a mean insufflation pressure of 16 mm Hg and a mean operative time of 3h [16]. They found no clinically significant increase in intracranial pressure [16]. However, routine pre- and postoperative anesthetic monitoring should remain the standard of care [16].
Sankpal et al. found no cases of gas embolism in a study of over 51 laparoscopic procedures in this category of patients [16]. The risk of valve system reflux was found to be minimal even at intra-abdominal pressures of up to 80 mmHg [16].
A study conducted during 2014-2016 in the surgical department of Toyonaka Hospital, a group of 582 patients underwent laparoscopic cholecystectomy, four of whom had ventriculo-peritoneal shunt [31]. Similar to our case, they sought neurosurgical consultation where temporary shunt ligation was indicated, the other case was cholecystectomized without shunt ligation as it was considered to be already occluded [24]. In all cases, the trocars were carefully inserted to avoid injuring the catheters, considering useful the decision of our team to perform preoperative ultrasound to be able to locate the shunt path, both to avoid injuring it and to make it easier to ligate [31]. Although in our patient's case, the operative time was prolonged due to pericholecystic adhesions, the outcome was favorable, as a similar case described by them, which also had a good evolution, without complications [31]. Similar to the case described by Al-Mufarrej et al., we found it useful to ligate the distal end of the shunt in our patient during surgery, as the shunt was not provided with a unidirectional valve and the exact pattern used could not be documented [32].
According to the presented case and literature data available by now, the insufflation pressure must be the minimum required, and at all times less than 16 mmHg [16] The operative time allowed for such patients, approximately 3 hours, has been shown to be safe [16].
The major concern related to laparoscopic procedures in patients with VP shunt is that of encephalitis, especially in procedures with a high risk of contamination [30]. The risk of infection and damage to the shunt can lead to peritonitis or ventriculitis, sepsis, and uncontrolled hydrocephalus, factors that can promote altered mental status and sometimes even death [30]. When a patient with VP shunt requires laparoscopic surgery, the attending surgeon must determine appropriate perioperative shunt management; in addition, neurosurgeons are frequently consulted because of concerns about shunt infection [30].
In one of the largest reported studies, which included laparotomies and laparoscopic procedures, no infection was observed in patients with VP shunt [4].
Over the past few years, several techniques have been developed to prevent possible infection through contamination with intestinal contents or urine, including exteriorization of the distal end of the catheter, ventriculo-atrial shunt conversion, ligation, and placement of the distal end in an intracorporeal pouch [33]. As for prophylactic antibiotic therapy, there is currently no consensus in the published data, with indications ranging from single-dose antibiotic administration to a triple antibiotic regimen for 1-2 days [34].
At the same time, the authors of the present study (Goel et al.) suggest that a single dose of broad-spectrum antibiotic is indicated for surgery such as laparoscopic cholecystectomy [35].
The study conducted by Li et al. on a group of 26 patients demonstrated the efficacy of administering a single dose of Cephalosporin antibiotic preoperatively and one day postoperatively in patients who had not undergone surgery with increased infectious risk [30]. Savlovschi et al. also reported a postoperative infection rate in patients with VP shunt, of 9% within 30 days of discharge [26]. This was comparable to the 5% to 7% shunt infection rate reported after shunt fitting or revision [26]. Thus, the infectious risk in patients with VP shunt cannot be fully attributed to the laparoscopic procedure, since laparoscopic surgery has been shown to have a significantly lower infectious risk compared to laparotomies (0.62% vs. 1.82%) [2,33].
From the perspective of the spread of infection, it can travel upward along the catheter to the lateral ventricle (LV) [26]. Recently, research has shown that some antibiotic-impregnated catheters can significantly reduce the rate of infection [26]. Of the pathogens, the most frequently implicated were Staphylococcus aureus, Staphylococcus epidermidis, Staphylococcus capitis, Staphylococcus sciuri, Enterococcus faecium, and Enterococcus baumanii [33,34].
An episode of infection was defined as the presence of clinical features consistent with a positive culture from CSF, the distal end of the VP or from exudate samples obtained from VP lesions, and the time window to confirmation of infection was defined as the number of days that had elapsed since the placement of the VP shunt or its last surgical revision and the onset of symptoms [30]. In laparotomy there is also a higher risk of postoperative adhesions, with the possibility of distal catheter blockage and pseudocyst formation that could promote infection and shunt occlusion [4]. Also, the shunt tube is itself an intraperitoneal foreign body, which may increase the chance of developing infection [4]. This risk can be managed intraoperatively with simple maneuvers such as perioperative antibiotic administration and exteriorization of the peritoneal end of the shunt [4].
The surgical team should be aware that VP shunt infections can mimic an acute surgical abdomen [4]. In such cases, the recommended treatment is shunting discharge, antibiotic therapy and shunt replacement after the acute phase has subsided [4].
Also, from an infectious risk perspective, different studies have shown that shunt infection correlates with the number of shunt exposures to surgical gloves [23]. The advantage of laparoscopic procedures is a reduced risk of adhesion formation and limited contact between gloves and shunt [23].
Some authors demonstrated in a study spanning 1994-2003 and including 23 cases, that laparoscopic surgery may have a 9% risk of infection at 30 days post-operatively, requiring shunt removal and replacement [23,35,36]. It has been documented that the two patients who required replacement of the shunt, did not receive prophylactic pre- and postoperative antibiotic therapy compared to other patients [23]. This series included only patients undergoing laparoscopic cholecystectomy and reported that an infection rate of 9% was equivalent to that seen when other types of laparoscopic surgery are performed in the presence of a VP shunt [23]. Postoperative adhesions prevention, by minimizing the peritoneal and organ trauma is also important to achieve favourable long-term results [37,38].
Other authors found that 53% of postoperative infections are not identified, only until after the patient has been discharged from hospital [39,40]. It is therefore recommended to educate patients and their caregivers about the signs and symptoms that may occur as a result of shunt damage (such as headache and photophobia) [20]. In our patient's case, the post-operative course was good, with no neurological or infectious complications.
Also, due to the lack of data available so far, a recent study by Goel et al., based on procedures performed in their London neurosurgery center, proposed a guideline on the management of these patients which is divided into pre-, peri- and post-operative aspects [35]. Pre-operative aspects involved locating the shunt, ensuring that the shunt is compatible if an MRI investigation is performed and antibiotic prophylaxis to avoid infections [35]. Peri-operative aspects included pneumoperitoneum, functioning and protection of the shunt, and surgical technique. Post-operatively they stated the importance of correct diagnosis and treatment of neurological symptoms and signs, treatment of pain and the effects of adhesions of the shunt [35].
Part of the relative contraindication of performing surgery on newly introduced shunts, comes from Almayouf et al., they reported a unique complication in the form of subcutaneous emphysema and distention along the catheter pathway during laparoscopic cholecystectomy in a patient with a newly inserted VP shunt, causing a rapid increase in end-tidal CO2 pressure and peak inspiratory flow, evoking the benefit of timing the procedure to initially allow for fibrosis of the catheter tunnelling tract [2]. Shunt malfunction has been reported in patients undergoing laparoscopic surgery, and methods proposed to avoid complications were ICP monitoring, ultrasound examination and temporary shunt exteriorization [41]. Proposed methods to avoid postoperative VP shunt complications are to check at the beginning, during and after laparoscopic surgery for free CSF drainage from the distal end of the catheter and to use the lowest possible pressure of pneumoperitoneum in the shortest possible frame of time [41,42].
It is important for an anesthesiologist to realize the possible complications of laparoscopy performed in patients with ventriculo-peritoneal shunt [43,44,45]. These patients should be kept under close observation in the postoperative period for signs and symptoms suggestive of shunt malfunction [46,47]. Therefore, preoperative neurologic evaluation and postoperative neurologic observation are critical for these patients.
Conclusions
Correlating our therapeutic approach with the data currently available in the literature, we consider laparoscopic cholecystectomy a procedure that can be safely performed in patients with ventriculo-peritoneal shunt. Tissue marking of shunt topography under ultrasound control is an extremely important aspect to prevent catheter injury during laparoscopic procedures. In the case of an older model shunt with bidirectional flow, preoperative ligation is mandatory, with release 24 hours postoperatively after intraperitoneal drainage tube suppression.
Communication between anesthetist, neurosurgeon and surgeon is important to prevent and treat theoretically possible, but rare complications that may occur in patients with ventriculo-peritoneal shunts undergoing laparoscopic surgery.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- Serban, D.; Socea, B.; Balasescu, S.A.; et al. Safety of Laparoscopic Cholecystectomy for Acute Cholecystitis in the Elderly: A Multivariate Analysis of Risk Factors for Intra and Postoperative Complications. Medicina (Kaunas). 2021, 57, 230, Published 2021 Mar 2. [Google Scholar] [CrossRef] [PubMed]
- Almayouf, M.; Al-Sabahi, T.; Alburakan, A.; Nouh, T. Laparoscopy in a Patient With a Ventriculoperitoneal Shunt: A Case Report and Literature Review. International Surgery. 2021, 105, 515–520. [Google Scholar] [CrossRef]
- Serban, D.; Badiu, D.C.; Davitoiu, D.; et al. Systematic review of the role of indocyanine green near-infrared fluorescence in safe laparoscopic cholecystectomy (Review). Exp Ther Med. 2022, 23, 187. [Google Scholar] [CrossRef] [PubMed]
- Lykoudis, P.M.; Nastos, C.; Dellaportas, D.; et al. Laparoscopic cholecystectomy in patients with ventriculoperitoneal shunts: A case series. Hellenic J Surg. 2017, 89, 163–165. [Google Scholar] [CrossRef]
- Serban, D.; Brănescu, C.M.; Smarandache, G.C.; et al. Safe surgery in day care centers: focus on preventing medical legal issues. Rom J Leg Med. 2021, 29, 60–64. [Google Scholar] [CrossRef]
- Cobianchi, L.; Dominioni, T.; Filisetti, C.; et al. Ventriculoperitoneal shunt and the need to remove a gallbladder: Time to definitely overcome the feeling that laparoscopic surgery is contraindicated. Ann Med Surg (Lond). 2014, 3, 65–67, Published 2014 Jun 21. [Google Scholar] [CrossRef]
- Hammill, C.W.; Au, T.; Wong, L.L. Laparoscopic cholecystectomy in a patient with a ventriculoperitoneal shunt. Hawaii Med J. 2010, 69, 103–104. [Google Scholar]
- Paff, M.; Alexandru-Abrams, D.; Muhonen, M.; Loudon, W. Ventriculoperitoneal shunt complications: A review. Interdisciplinary Neurosurgery. 2018, 13, 66–70. [Google Scholar] [CrossRef]
- Bondurant, C.P.; Jimenez, D.F. Epidemiology of cerebrospinal fluid shunting. Pediatr Neurosurg. 1995, 23, 254–259. [Google Scholar] [CrossRef]
- Fernández-Méndez, R.; Richards, H.K.; Seeley, H.M.; Pickard, J.D.; Joannides, A.J.; UKSR collaborators. Current epidemiology of cerebrospinal fluid shunt surgery in the UK and Ireland (2004-2013). J Neurol Neurosurg Psychiatry. 2019, 90, 747–754. [Google Scholar] [CrossRef]
- Metwally, I.H.; Metwally, I.H. Laparoscopic Hysterectomy in a Patient with Ventriculo-Peritoneal Shunt after Multiple Cesarean Sections. Annals of Minimally Invasive Surgeries. 2021, 3, 31–34. [Google Scholar] [CrossRef]
- Oliveira, M.F.; de Pereira, R.M.; Pinto, F.G. Updating technology of shunt valves. Medical Express 2014, 1, 166–169. [Google Scholar] [CrossRef]
- Chaudhari, N.; Khopde, S.; Thombare, B.; Shah, H.K. Safety of laparoscopic cholecystectomy in patients with ventriculoperitoneal shunt. National Journal of Medical and Allied Sciences 2014, 3, 36–39. [Google Scholar]
- Andreasen, T.H.; Holst, A.V.; Lilja, A.; et al. Valved or valveless ventriculoperitoneal shunting in the treatment of post-haemorrhagic hydrocephalus: a population-based consecutive cohort study. Acta Neurochir (Wien). 2016, 158, 261–270. [Google Scholar] [CrossRef]
- Kuo, L.T.; Huang, A.P. The Pathogenesis of Hydrocephalus Following Aneurysmal Subarachnoid Hemorrhage. Int J Mol Sci. 2021, 22, 5050, Published 2021 May 10. [Google Scholar] [CrossRef]
- Sankpal, R.; Chandavarkar, A.; Chandavarkar, M. Safety of Laparoscopy in Ventriculoperitoneal Shunt Patients. J Gynecol Endosc Surg. 2011, 2, 91–93. [Google Scholar] [CrossRef]
- Bouzerar, R.; Tekaya, I.; Bouzerar, R.; Balédent, O. Dynamics of hydrocephalus: a physical approach. J Biol Phys. 2012, 38, 251–266. [Google Scholar] [CrossRef][Green Version]
- Penn, R.D.; Linninger, A. The physics of hydrocephalus. Pediatr Neurosurg. 2009, 45, 161–174. [Google Scholar] [CrossRef]
- Symss, N.P.; Oi, S. Theories of cerebrospinal fluid dynamics and hydrocephalus: historical trend. J Neurosurg Pediatr. 2013, 11, 170–177. [Google Scholar] [CrossRef]
- Wilson, M.H. Monro-Kellie 2.0: The dynamic vascular and venous pathophysiological components of intracranial pressure. J Cereb Blood Flow Metab. 2016, 36, 1338–1350. [Google Scholar] [CrossRef]
- Mohamed, S.A.; Mohamed, A.A. Safety of Laparoscopy in Patients with Ventriculoperitoneal Shunts. Iberoamerican Journal of Medicine 2021, 3, 130–137. [Google Scholar] [CrossRef]
- Herrera García, W.E.; Pérez Vertí Ramírez, J.; Lares-Asseff, I. Colecistectomía laparoscópica en un paciente con sistema de derivación ventriculoperitoneal [Laparoscopic cholecystectomy in a patient with ventriculoperitoneal shunt system]. Bol Med Hosp Infant Mex. 2014, 71, 303–306. [Google Scholar] [CrossRef]
- Rad, M.T.; Bogdanyova, S.; Wilhelm, L.M.; Konczalla, J.; Raimann, F.J.; Wallwiener, M.; Becker, S. Laparoscopic Intervention after Ventriculoperitoneal Shunt: A Case Report, Systematic Review, and Recommendations. World Journal of Laparoscopic Surgery 2020, 13, 35–42. [Google Scholar] [CrossRef]
- Bala, R.; Bansal, P.; Malhan, S.; Mittal, H. Anesthetic management of a patient undergoing abdominal surgery with bilateral ventricular peritoneal shunt in situ. Ain-Shams Journal of Anesthesiology 2021, 13, 38. [Google Scholar] [CrossRef]
- Dumitrescu, D.; Savlovschi, C.; Borcan, R.; et al. Caz clinic--hernie diafragmatică voluminoasă--abdomen acut chirurgical: dificultăţi diagnostice şi terapeutice [Clinical case--voluminous diaphragmatic hernia--surgically acute abdomen: diagnostic and therapeutical challenges]. Chirurgia (Bucur). 2011, 106, 657–660. [Google Scholar]
- Savlovschi, C.; Brănescu, C.; Serban, D.; et al. Hernia Amyand--caz clinic [Amyand's hernia--a clinical case]. Chirurgia (Bucur). 2010, 105, 409–414. [Google Scholar]
- Chen, P.R.; Spetzler, R.F. Persistent lower abdominal pain induced by long peritoneal shunt catheter. Acta Neurochir (Wien). 2008, 150, 829–831. [Google Scholar] [CrossRef]
- Serban, D.; Tribus, L.C.; Vancea, G.; et al. Acute Mesenteric Ischemia in COVID-19 Patients. J Clin Med. 2021, 11, 200, Published 2021 Dec 30. [Google Scholar] [CrossRef]
- Mohamed, A.A.R.; Ali Abbasi, S. Safety of Laparoscopy without Intraoperative Intracranial Pressure Monitoring In Patients with Ventriculoperitoneal Shunt: Case Report and Literature Review. EAS J Anesthesiol Crit Care 2019, 1, 1–4. [Google Scholar] [CrossRef]
- Li, G.; Dutta, S. Perioperative management of ventriculoperitoneal shunts during abdominal surgery. Surg Neurol. 2008, 70, 492–497. [Google Scholar] [CrossRef]
- Takeda, Y.; Tomimaru, Y.; Yokota, Y.; et al. Outcomes of laparoscopic cholecystectomy for xanthogranulomatous cholecystitis. Mol Clin Oncol. 2019, 11, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Al-Mufarrej, F.; Nolan, C.; Sookhai, S.; et al. Laparoscopic procedures in adults with ventriculoperitoneal shunts. Surg Laparosc Endosc Percutan Tech. 2005, 15, 28–29. [Google Scholar] [CrossRef] [PubMed]
- Qin, B.; Chen, G.; Chen, J. Shunt infection in a single institute: a retrospective study. Chin Neurosurg J. 2018, 4, 8, Published 2018 May 7. [Google Scholar] [CrossRef][Green Version]
- Pelegrín, I.; Lora-Tamayo, J.; Gómez-Junyent, J.; et al. Management of Ventriculoperitoneal Shunt Infections in Adults: Analysis of Risk Factors Associated With Treatment Failure. Clin Infect Dis. 2017, 64, 989–997. [Google Scholar] [CrossRef]
- Goel, A.; Craven, C.; Matloob, S.; Thompson, S.; Watkins, L.; Toma, A. CSF-diverting shunts: Implications for abdominal and pelvic surgeons; a review and pragmatic overview. Ann Med Surg (Lond). 2019, 48, 100–104. [Google Scholar] [CrossRef]
- Charalabopoulos, A.; Botha, A.J. Laparoscopic cholecystectomy in the presence of lumboperitoneal shunt. Case Rep Surg. 2013, 2013, 929082. [Google Scholar] [CrossRef]
- Fometescu, S.G.; Costache, M.; Coveney, A.; Oprescu, S.M.; Serban, D.; Savlovschi, C. Peritoneal fibrinolytic activity and adhesiogenesis. Chirurgia (Bucur). 2013, 108, 331–340. [Google Scholar]
- Tuchila, C.; Baconi, D.L.; Pirvu, C.D.; Balalau, D.O.; Vlasceanu, A.M.; Stan, M.; Balalau, C. Therapeutic drug monitoring and methods of quantitation for carbamazepine. J Mind Med Sci. 2017, 4, 100–114. [Google Scholar] [CrossRef]
- Constantin, V.D.; Motofei, I. Severe Forms of Acalculous Acute Pancreatitis in Young Female Patients. A Preliminary Study. Chirurgia (Bucur). 2022, 117, 463–471. [Google Scholar] [CrossRef]
- Albu, C.V.; Pădureanu, V.; Boldeanu, M.V.; Bumbea, A.M.; Enescu, A.Ş.; Albulescu, D.M.; Siloși, C.A.; Enescu, A. Vascular neurocognitive disorders and the vascular risk factors. J Mind Med Sci. 2018, 5, 7–15. [Google Scholar] [CrossRef]
- Narayanan, M.K.; Venkataraju, A. Transient shunt malfunction following laparoscopy in a patient with Ventriculoperitoneal shunt. BJA: British Journal of Anaesthesia 2009, 103. [Google Scholar] [CrossRef]
- Bratu, D.; Boicean, A.; Tanasescu, C.; Sofariu, C.; Mihetiu, A.; Cernusca Mitariu, I.S.; Ognean, L.; Moldovan, C.; Boitor, C. Textile Polypropylene Allografts and their Postoperative Tissue Reaction in the Surgery of Inguinal Hernia. Materiale Plastice. 2017, 54, 119–121. [Google Scholar] [CrossRef]
- Wang, Y.M.; Liu, Y.C.; Ye, X.D.; Chia, Y.Y.; Liu, K. Anesthetic management of laparoscopic surgery in a patient with a ventriculoperitoneal shunt. Acta Anaesthesiol Sin. 2003, 41, 85–88. [Google Scholar] [PubMed]
- Tănăsescu, C.; Faur, M.; Sabău, D. Day-case Surgery in the Context of Inguinal Hernia Repair by the Modified Lichtenstein Technique - A Single Centre Experience. Chirurgia (Bucur). 2019, 114, 115–120. [Google Scholar] [CrossRef]
- Radu, N.; Roman, V.; Bostan, M.; Radu, E.; Tanasescu, C. Influence of some spice food based bioproducts on human monocytic cells line type THP-1. Molecular Crystals and Liquid Crystals. 2017, 655, 114–123. [Google Scholar] [CrossRef]
- Rumba, R.; Vanags, A.; Strumfa, I.; Pupkevics, A.; Pavars, M. Laparoscopic Cholecystectomy for a Patient with a Lumboperitoneal Shunt: A Rare Case. Chirurgia (Bucur). 2016, 111, 263–265. [Google Scholar]
- Yu, Q.; Lou, C.; Feng, T.; Liu, Y. Ventriculoperitoneal shunt malfunction due to chronic cholecystitis: A case report. Medicine (Baltimore). 2020, 99, e20565. [Google Scholar] [CrossRef]
© 2023 by the author. 2023 Carmen Popa, Andrei Moisin, Mihai Faur, Mihaela Racheriu, Ramona Coca, Cristian Mihai Branescu, Tiberiu Trotea, Denisa Tănăsescu