India Ink Tattooing of Ureteroenteric Anastomoses
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Technique
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Surgical and Postoperative Demographics
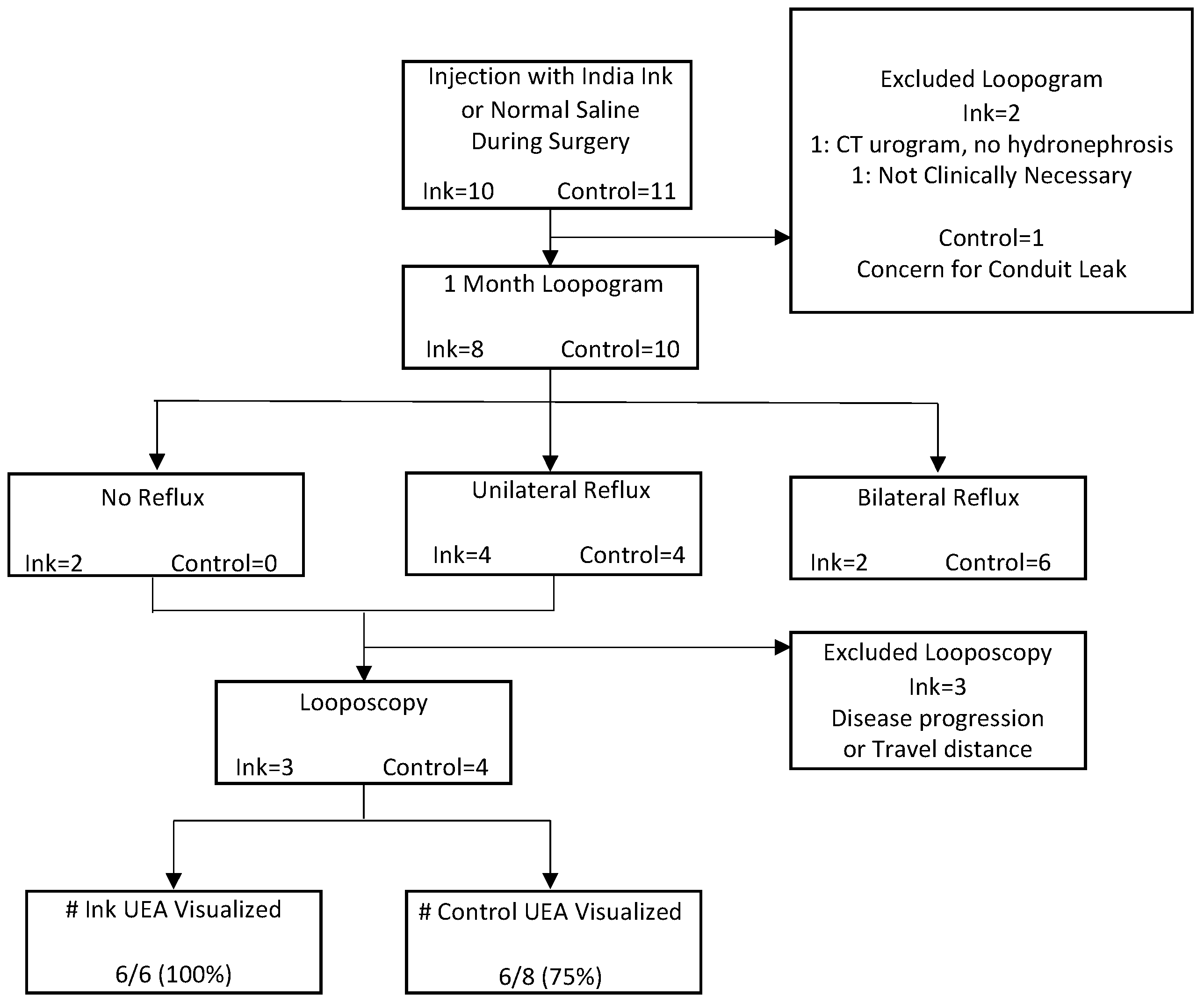
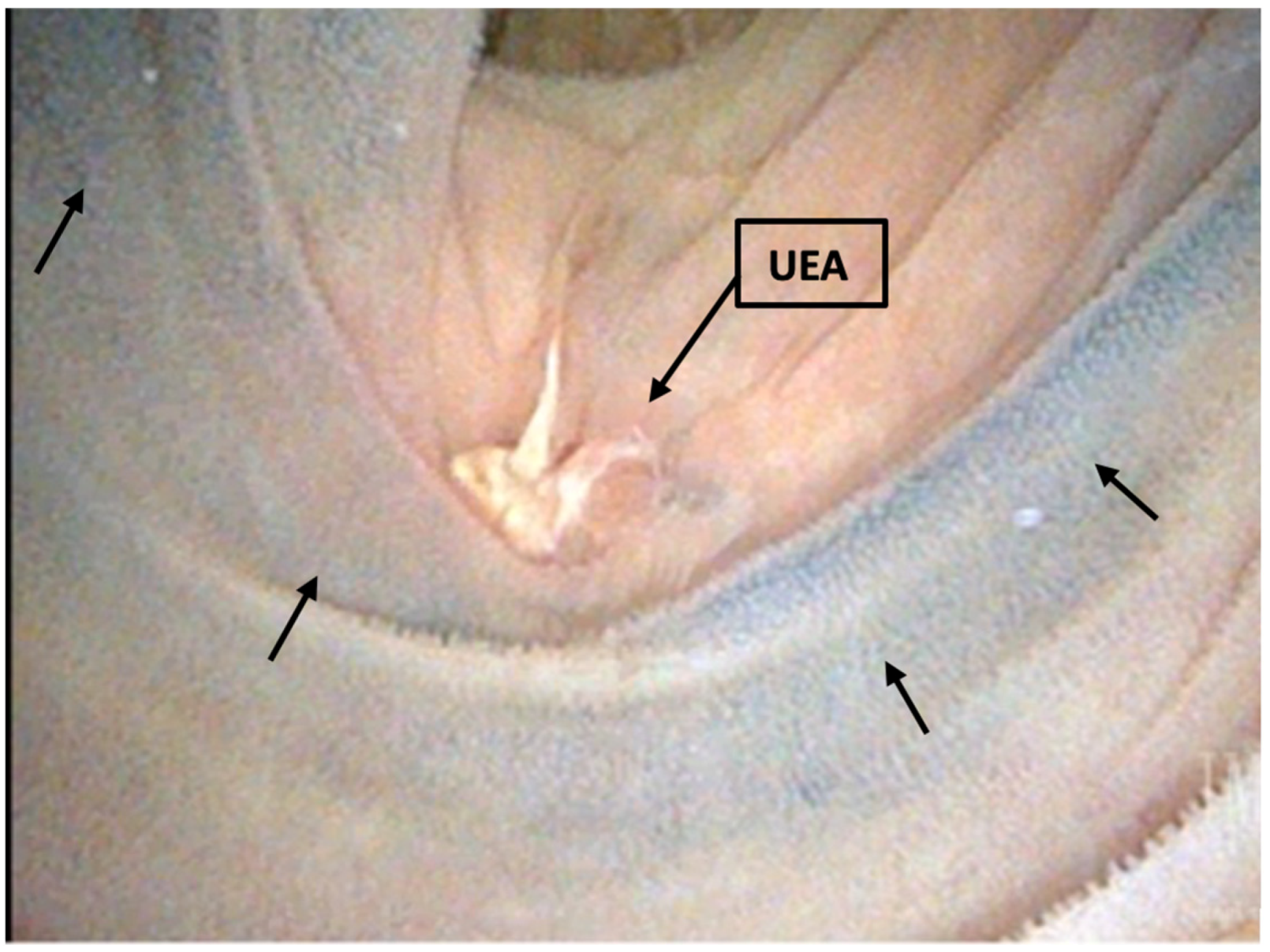
3.3. Loopogram and Looposcopy
3.4. Postoperative Complications and Additional Surgeries
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chesnut, G.T.; Rentea, R.M.; Leslie, S.W. Urinary Diversions And Neobladders. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: http://www.ncbi.nlm.nih.gov/books/NBK560483/ (accessed on 6 April 2022).
- Olson, L.; Satherley, H.; Cleaveland, P.; Zelhof, B.; Mokete, M.; Neilson, D.; Srirangam, S. Retrograde Endourological Management of Upper Urinary Tract Abnormalities in Patients with Ileal Conduit Urinary Diversion: A Dual-Center Experience. J. Endourol. 2017, 31, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Hyams, E.S.; Winer, A.G.; Shah, O. Retrograde Ureteral and Renal Access in Patients With Urinary Diversion. Urology 2009, 74, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Reid Pitts, W.; Muecke, E.C. A 20-Year Experience With Ileal Conduits: The Fate of the Kidneys. J. Urol. 1979, 122, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, C.E.; Schwartz, M.J.; Boorjian, S.A.; Lee, M.M.; Scherr, D.S. Ureteroileal anastomosis with intraluminal visualization: Technique and outcomes. Urology 2010, 76, 1496–1500. [Google Scholar] [CrossRef]
- Kouba, E.; Sands, M.; Lentz, A.; Wallen, E.; Pruthi, R.S. A Comparison of the Bricker Versus Wallace Ureteroileal Anastomosis in Patients Undergoing Urinary Diversion for Bladder Cancer. J. Urol. 2007, 178, 945–949. [Google Scholar] [CrossRef]
- Evangelidis, A.; Lee, E.K.; Karellas, M.E.; Thrasher, J.B.; Holzbeierlein, J.M. Evaluation of ureterointestinal anastomosis: Wallace vs. Bricker. J. Urol. 2006, 175, 1755–1758; discussion 1758. [Google Scholar] [CrossRef]
- Lee, C.T.; Chen, B.T.; Gong, E.; Hafez, K.S.; Sheffield, J.H.; Montie, J.E. Comparison of modified Taguchi and Bricker ureteral reimplantation techniques after radical cystectomy. Urology 2004, 64, 940–944. [Google Scholar] [CrossRef]
- Vandenbroucke, F.; Poppel, H.; Vandeursen, H.; Oyen, R.; Baert, L. Surgical versus Endoscopic Treatment of Non-malignant Uretero-ileal Anastomotic Strictures. BJU Int. 1993, 71, 408–412. [Google Scholar] [CrossRef]
- DiMarco, D.S.; LeRoy, A.J.; Thieling, S.; Bergstralh, E.J.; Segura, J.W. Long-term results of treatment for ureteroenteric strictures. Urology 2001, 58, 909–913. [Google Scholar] [CrossRef]
- Nassar, O.A.; Alsafa, M.E. Experience With Ureteroenteric Strictures After Radical Cystectomy and Diversion: Open Surgical Revision. Urology 2011, 78, 459–465. [Google Scholar] [CrossRef]
- Kramolowsky, E.V.; Clayman, R.V.; Weyman, P.J. Management of Ureterointestinal Anastomotic Strictures: Comparison of Open Surgical and Endourological Repair. J. Urol. 1988, 139, 1195–1198. [Google Scholar] [CrossRef] [PubMed]
- Schöndorf, D.; Meierhans-Ruf, S.; Kiss, B.; Giannarini, G.; Thalmann, G.N.; Studer, U.E.; Roth, B. Ureteroileal strictures after urinary diversion with an ileal segment-is there a place for endourological treatment at all? J. Urol. 2013, 190, 585–590. [Google Scholar] [CrossRef]
- Shatz, B.A.; Weinstock, L.B.; Swanson, P.E.; Thyssen, E.P. Long-term safety of India ink tattoos in the colon. Gastrointest. Endosc. 1997, 45, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, R.T.; Francis, J.M.; Carrougher, J.G.; Root, S.S.; Angueira, C.E.; Szyjkowski, R.; Kadakia, S.C. India ink tattooing in the esophagus. Gastrointest. Endosc. 1998, 47, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.K.; Song, M.H.; Yang, H.J.; Kim, D.S.; Lee, N.K.; Jeon, Y.S. Use of Cystoscopic Tattooing in Laparoscopic Partial Cystectomy. Korean J. Urol. 2012, 53, 401–404. [Google Scholar] [CrossRef] [PubMed]
- McCormick, B.; Beilan, J.; Baumgarten, A.; Martinez, D.; Ordorica, R.; Patel, T.; Hernandez, D. V4-08 india ink injection (tattooing) of the ureteric-intestinal anastomosis in urinary diversions: A simple and effective technique to aid in subsequent recognition in retrograde manipulations. J. Urol. 2016, 195, e519. [Google Scholar] [CrossRef]
- Turk, T.M.T.; Koleski, F.C.; Albala, D.M. Incidence of urolithiasis in cystectomy patients after intestinal conduit or continent urinary diversion. World J. Urol. 1999, 17, 305–307. [Google Scholar] [CrossRef]
- Shaw, N.M.; Lobo, J.M.; Zee, R.; Krupski, T.L. Management of Ureteroenteric Stricture: Predictive Modeling to Compare Cost. J. Endourol. 2016, 30, 1244–1251. [Google Scholar] [CrossRef]
- Yeaman, C.T.; Winkelman, A.; Maciolek, K.; Tuong, M.; Nelson, P.; Morris, C.; Culp, S.; Isharwal, S.; Krupski, T.L. Impact of radiation on the incidence and management of ureteroenteric strictures: A contemporary single center analysis. BMC Urol. 2021, 21, 101. [Google Scholar] [CrossRef]
- Amin, K.A.; Vertosick, E.A.; Stearns, G.; Fathollahi, A.; Sjoberg, D.D.; Donat, M.S.; Herr, H.; Bochner, B.; Dalbagni, G.; Sandhu, J.S. Predictors of Benign Uretero-enteric Anastomotic Strictures After Radical Cystectomy and Urinary Diversion. Urology 2020, 144, 225–229. [Google Scholar] [CrossRef]
- Ahmed, Y.E.; Hussein, A.A.; May, P.R.; Ahmad, B.; Ali, T.; Durrani, A.; Khan, S.; Kumar, P.; Guru, K.A. Natural History, Predictors and Management of Ureteroenteric Strictures after Robot Assisted Radical Cystectomy. J. Urol. 2017, 198, 567–574. [Google Scholar] [CrossRef] [PubMed]
| India Ink (n = 10) N (%) | Control (n = 11) N (%) | p Value | |
|---|---|---|---|
| Gender | |||
| Male | 9 (90) | 8 (73) | 0.59 |
| Female | 1 (10) | 3 (27) | |
| Median Age (IQR) | 72 (64, 74) | 61 (58, 66) | 0.04 |
| Race | |||
| White | 9 (90) | 11 (100) | 0.48 |
| Hispanic | 1 (10) | 0 (0) | |
| Median CCI (IQR) | 5 (3, 7) | 2 (2, 4) | 0.01 |
| Preoperative pathology | |||
| HGPUC | 8 (80) | 9 (82) | 1.00 |
| CIS | 0 (0) | 1 (9) | |
| Squamous Cell | 1 (10) | 1 (9) | |
| Non Malignant | 1 (10) | 0 (0) | |
| Clinical T stage | |||
| Tx | 1 (11) | 1 (9) | 0.66 |
| Ta | 2 (22) | 0 (0) | |
| Tis | 0 (0) | 1 (9) | |
| T1 | 2 (22) | 4 (36) | |
| T2 | 4 (44) | 4 (36) | |
| T4 | 0 (0) | 1 (9) | |
| Clinical N stage | |||
| N0 | 8 (89) | 9 (82) | 0.48 |
| N1 | 1 (11) | 0 (0) | |
| N2 | 0 (0) | 2 (18) | |
| Neoadjuvant Chemotherapy | |||
| No | 5 (50) | 7 (64) | 0.67 |
| Yes | 5 (50) | 4 (36) | |
| Median Preoperative GFR (IQR) | 65 (47, 80) | 64 (51, 79) | 0.81 |
| India Ink (n = 10) N (%) | Controls (n = 11) N (%) | p Value | |
|---|---|---|---|
| Type of Cystectomy | |||
| Radical | 8 (80) | 10 (91) | 0.34 |
| Partial | 2 (20) | 0 (0) | |
| Diversion only | 0 (0) | 1 (9) | |
| Median Hospital Length of Stay (IQR) | 7 (5, 12) | 8 (7, 10) | 0.37 |
| Number Hospital Complications | 2 (20) | 5 (50) | 0.34 |
| Clavien–Dindo Score | |||
| II | 0 (0) | 3 (27) | 0.29 |
| II | 0 (0) | 1 (9) | |
| IIIa | 1 (10) | 1 (9) | |
| IIIb | 1 (10) | 0 (0) | |
| Type of In Hospital Complication | |||
| Cardiovascular (MI, stroke, DVT) | 0 (0) | 0 (0) | |
| Bowel (ileus, fistula, and small Bowel Obstruction) | 1 (10) | 2 (18) | |
| Infection (pelvis abscess, wound infection, amd sepsis) | 1 (10) | 0 (0) | |
| Kidney (pyelonephritis and ureteral stricture) | 0 (0) | 0 (0) | |
| Other | 1 (10) | 3 (27) | |
| Number Patients Discharged with Ureteral Stents | 3 (30) | 2 (18) | 0.64 |
| Surgical Pathology | |||
| HGPUC | 5 (50) | 8 (73) | 0.84 |
| CIS | 1 (10) | 1 (9) | |
| Squamous Cell | 1 (10) | 0 (0) | |
| No Cancer | 3 (30) | 2 (18) | |
| Surgical Pathology T Stage | |||
| T0 | 0 (0) | 1 (9) | 0.21 |
| Ta | 3 (33) | 0 (0) | |
| Tis | 1 (11) | 1 (9) | |
| T1 | 0 (0) | 1 (9) | |
| T2 | 3 (33) | 2 (18) | |
| T3 | 1 (11) | 2 (18) | |
| T4 | 1 (11) | 4 (36) | |
| Surgical Pathology N Stage | |||
| Nx | 1 (11) | 1 (9) | 0.18 |
| N0 | 7 (78) | 5 (45) | |
| N1 | 0 (0) | 0 (0) | |
| N2 | 1 (11) | 5 (45) | |
| Median Postoperative GFR (<60 days) (IQR) | 44 (24, 69) | 57 (44, 69) | 0.43 |
| Median Postoperative GFR (<90 days) (IQR) | 47 (24, 70) | 60 (48, 72) | 0.13 |
| India Ink N (%) | Controls N (%) | p Value | |
|---|---|---|---|
| Number of Patients | 8 (80) | 9 (82) | |
| Median Days Since Surgery (IQR) | 51 (22, 124) | 33 (14, 73) | 0.28 |
| Clavien–Dindo Classification | |||
| 1 | 2 | 3 | 0.16 |
| 2 | 11 | 11 | |
| 3a | 7 | 1 | |
| 3b | 2 | 1 | |
| 4a | 0 | 2 | |
| 4b | 0 | 0 | |
| 5 | 2 | 4 | |
| Types of Complication | |||
| Cardiovascular (MI, stroke, DVT) | 1 | 2 | |
| Bowel (Ileus, fistula, small bowel obstruction) | 2 | 1 | |
| Infection (pelvis absess, wound infection, sepsis) | 14 | 16 | |
| Kidney (pyelonephritis, ureteral stricture) | 2 | 3 | |
| Other | 5 | 4 |
| India Ink N (%) | Controls N (%) | p Value | |
|---|---|---|---|
| Number of Surgeries | 6 (3 patients, 30%) | 1 (1 patient, 9%) | 0.31 |
| Surgery Types | |||
| PCN, Ureteral stent | 4 (67) | 1 (100) | |
| Endoscopic Dilation | 1 (17) | 0 (0) | |
| Ureteral Reimplant | 1 (17) | 0 (0) | |
| Drain Placement | 0 (0) | 0 (0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tuong, M.N.E.; Prillaman, G.E.; Culp, S.H.; Nelson, M.; Krupski, T.L.; Isharwal, S. India Ink Tattooing of Ureteroenteric Anastomoses. Tomography 2023, 9, 449-458. https://doi.org/10.3390/tomography9020037
Tuong MNE, Prillaman GE, Culp SH, Nelson M, Krupski TL, Isharwal S. India Ink Tattooing of Ureteroenteric Anastomoses. Tomography. 2023; 9(2):449-458. https://doi.org/10.3390/tomography9020037
Chicago/Turabian StyleTuong, Mei N. E., Grace E. Prillaman, Stephen H. Culp, Marc Nelson, Tracey L. Krupski, and Sumit Isharwal. 2023. "India Ink Tattooing of Ureteroenteric Anastomoses" Tomography 9, no. 2: 449-458. https://doi.org/10.3390/tomography9020037
APA StyleTuong, M. N. E., Prillaman, G. E., Culp, S. H., Nelson, M., Krupski, T. L., & Isharwal, S. (2023). India Ink Tattooing of Ureteroenteric Anastomoses. Tomography, 9(2), 449-458. https://doi.org/10.3390/tomography9020037






