Can Intrapartum Ultrasonography Improve the Placement of the Vacuum Cup in Operative Vaginal Deliveries?
Abstract
1. Introduction
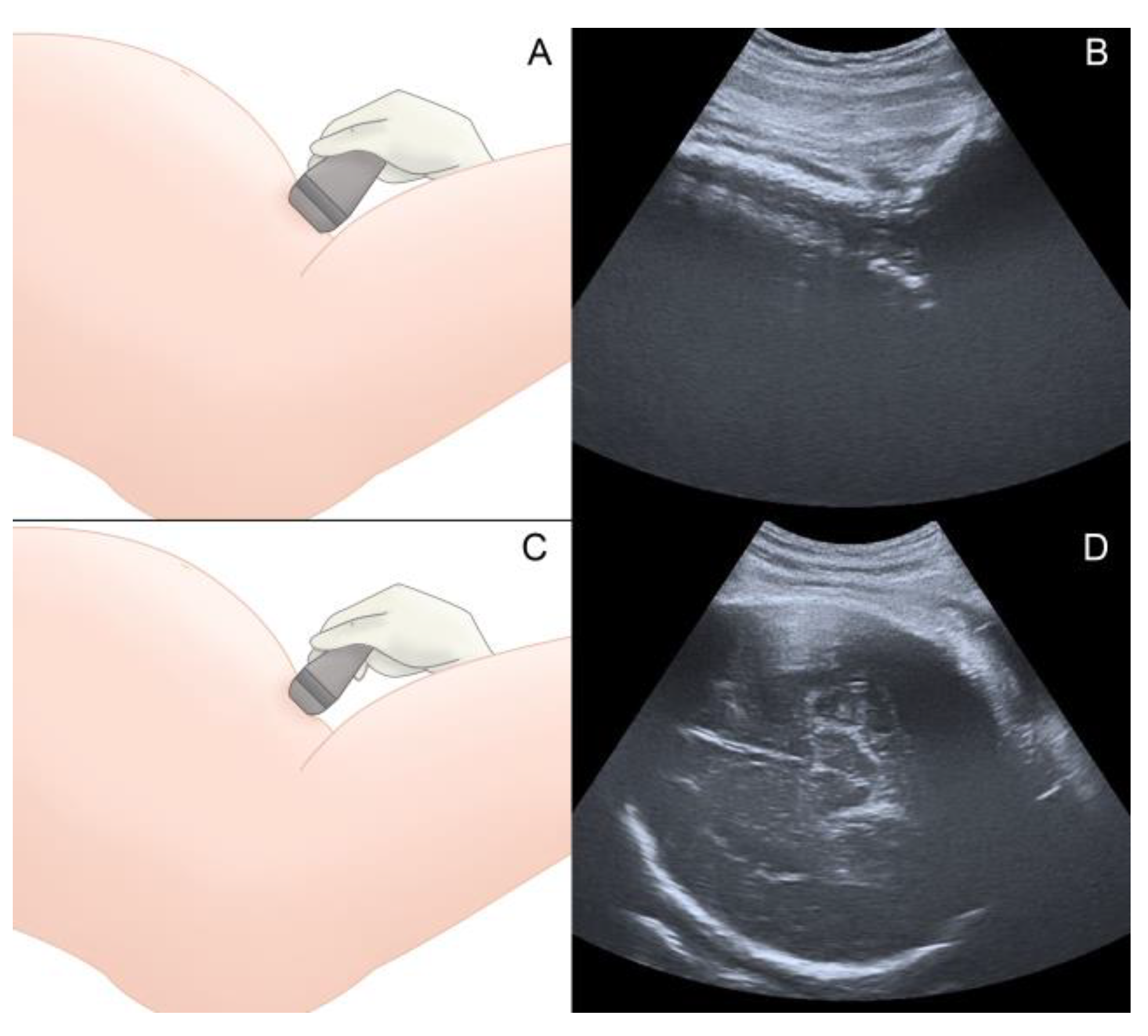
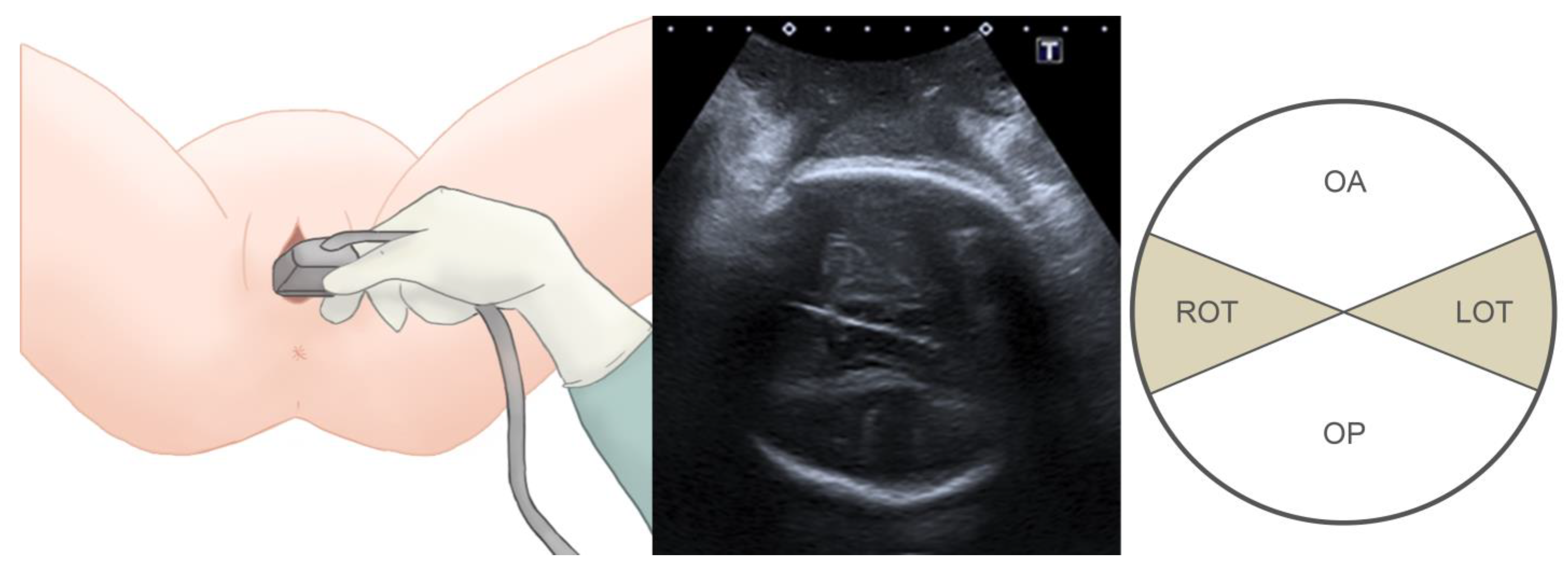
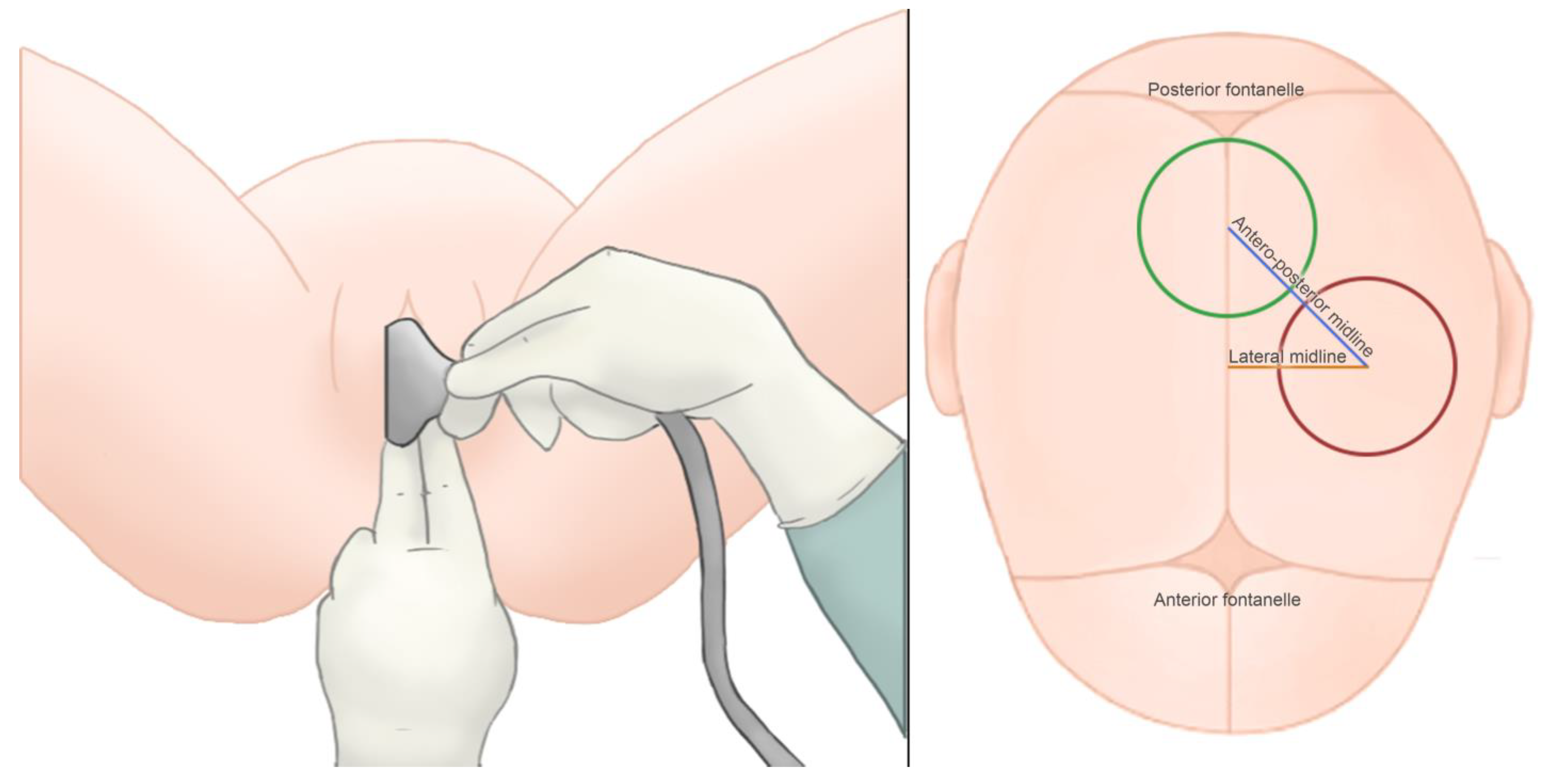
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bird, G.C. The importance of flexion in vacuum extractor delivery. Br. J. Obstet. Gynaecol. 1976, 83, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Vacca, A.; Keirse, M.J.N.C. Instrumental vaginal delivery. In Effective Care in Pregnancy and Childbirth; Chalmers, I., Enkin, M., Keirse, M.J.N.C., Eds.; Oxford University Press: Oxford, UK, 1989; pp. 1216–1233. [Google Scholar]
- Mola, G.D.; Amoa, A.B.; Edilyong, J. Factors associated with success or failure in trials of vacuum extraction. Aust N. Z. J. Obstet. Gynaecol. 2002, 42, 35–39. [Google Scholar] [CrossRef]
- Gei, A.F.; Smith, R.A.; Hankins, G.D. Brachial plexus paresis associated with fetal neck compression from forceps. Am. J. Perinatol. 2003, 20, 289–291. [Google Scholar] [PubMed]
- Dupuis, O.; Silveira, R.; Dupont, C.; Mottolese, C.; Kahn, P.; Dittmar, A. Comparison of “instrument-associated” and “spontaneous” obstetric depressed skull fractures in a cohort of 68 neonates. Am. J. Obstet. Gynecol. 2005, 192, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, O.; Ruimark, S.; Corrine, D.; Simone, T.; Andre, D.; Rene-Charles, R. Fetal head position during the second stage of labor, comparison of digital and vaginal examination and transabdominal ultrasonographic examination. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005, 123, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Akmal, S.; Kametas, N.; Tsoi, E.; Hargreaves, C.; Nicolaides, K.H. Comparison of transvaginal digital examination with intrapartum sonography to determine fetal head position before instrumental delivery. Ultrasound Obstet. Gynecol. 2003, 21, 437–440. [Google Scholar] [CrossRef]
- Sherer, D.M.; Miodovnik, M.; Bradley, K.S.; Langer, O. Intrapartum fetal head position II, comparison between transvaginal digital examination and transabdominal ultrasound assessment during the second stage of labor. Ultrasound Obstet. Gynecol. 2002, 19, 264–268. [Google Scholar] [CrossRef]
- Souka, A.P.; Haritos, T.; Basayiannis, K.; Noikokyri, N.; Antsaklis, A. Intrapartum ultrasound for the examination of the fetal head position in normal and obstructed labor. J. Matern. Fetal Neonatal Med. 2003, 13, 59–63. [Google Scholar] [CrossRef]
- Sherer, D.M.; Miodovnik, M.; Bradley, S.; Langer, O. Intrapartum fetal head position I, comparison between transvaginal digital examination and transabdominal ultrasound assessment during the active stage of labor. Ultrasound Obstet. Gynecol. 2002, 19, 258–263. [Google Scholar] [CrossRef]
- Kreiser, D.; Schiff, E.; Lipitz, S.; Kayam, Z.; Avraham, A.; Achiron, R. Determination of fetal occiput position by ultrasound during the second stage of labor. J. Matern. Fetal Med. 2001, 10, 283–286. [Google Scholar] [CrossRef]
- Akmal, S.; Tsoi, E.; Nicolaides, K.H. Intrapartum sonography to determine fetal occipital position, interobserver agreement. Ultrasound Obstet. Gynecol. 2004, 24, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Chou, M.R.; Kreiser, D.; Taslimi, M.M.; Druzin, M.L.; El-Sayed, Y.Y. Vaginal versus ultrasound examination of fetal occiput position during the second stage of labor. Am. J. Obstet. Gynecol. 2004, 191, 521–524. [Google Scholar] [CrossRef]
- Ramphul, M.; Kennelly, M.; Murphy, D.J. Establishing the accuracy and acceptability of abdominal ultrasound to define the foetal head position in the second stage of labour, a validation study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 164, 35–39. [Google Scholar] [CrossRef]
- Ramphul, M.; Ooi, P.V.; Burke, G.; Kennelly, M.M.; Said, S.A.; Montgomery, A.A. Instrumental delivery and ultrasound, a multicentre randomised controlled trial of ultrasound assessment of the fetal head position versus standard care as an approach to prevent morbidity at instrumental delivery. British ournal of Obstetrics and Gynaecology 2014, 121, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Operative Vaginal Birth: ACOG Practice Bulletin, Number 219. Obstet. Gynecol. 2020, 135, e149–e159. [Google Scholar] [CrossRef]
- Ghi, T.; Eggebø, T.; Lees, C.; Kalache, K.; Rozenberg, P.; Youssef, A.; Salomon, L.J.; Tutschek, B. ISUOG Practice Guidelines, intrapartum ultrasound. Ultrasound Obstet. Gynecol. 2018, 52, 128–139. [Google Scholar] [CrossRef]
- Akmal, S.; Tsoi, E.; Kametas, N.; Howard, R.; Nicolaides, K.H. Intrapartum sonography to determine the fetal head position. J. Matern. Fetal Neonatal Med. 2002, 12, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Zahalka, N.; Sadan, O.; Malinger, G.; Liberati, M.; Boaz, M.; Glezerman, M.; Rotmensch, S. Comparison of transvaginal sonography with digital examination and transabdominal sonography for the determination of fetal head position in the second stage of labor. Am. J. Obstet. Gynecol. 2005, 193, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Tutschek, B.; Braun, T.; Chantraine, F.; Henrich, W. A study of progress of labor using intrapartum translabial ultrasound, assessing head station, direction, and angle of descent. British ournal of Obstetrics and Gynaecology 2011, 118, 62–69. [Google Scholar] [CrossRef]
- Ramphul, M.; Kennelly, M.M.; Burke, G.; Murphy, D.J. Risk factors and morbidity associated with suboptimal instrument placement at instrumental delivery, observational study nested within the Instrumental Delivery & Ultrasound randomised controlled trial ISRCTN 72230496. British ournal of Obstetrics and Gynaecology 2015, 122, 558–563. [Google Scholar]
- Donnelly, V.; Fynes, M.; Campbell, D.; Johnson, H.; O’Connell, P.R.; O’Herlihy, C. Obstetric events leading to anal sphincter damage. Obstet. Gynecol. 1998, 92, 955–961. [Google Scholar] [PubMed]
- MacLennan, A.H.; Taylor, A.W.; Wilson, D.H.; Wilson, D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. British ournal of Obstetrics and Gynaecology 2000, 107, 1460–1470. [Google Scholar] [CrossRef] [PubMed]
- Olagundoye, V.; MacKenzie, I.Z. The impact of a trial of instrumental delivery in theatre on neonatal outcome. BJOG 2007, 114, 603–608. [Google Scholar] [CrossRef]
- Towner, D.; Castro, M.A.; Eby-Wilkens, E.; Gilbert, W.M. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N. Engl. J. Med. 1999, 341, 1709–1714. [Google Scholar] [CrossRef]
- Alexander, J.M.; Leveno, K.J.; Hauth, J.; Landon, M.B.; Thom, E.; Spong, C.Y.; Varner, M.W.; Moawad, A.H.; Caritis, S.N.; Harper, M.; et al. Fetal injury associated with cesarean delivery. Obstet. Gynecol. 2006, 108, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.J.; Liebling, R.E.; Patel, R.; Verity, L.; Swingler, R. Cohort study of operative delivery in the second stage of labor and standard of obstetric care. BJOG 2003, 110, 610–615. [Google Scholar] [CrossRef]
- Sadan, O.; Ginath, S.; Gomel, A.; Abramov, D.; Rotmensch, S.; Boaz, M.; Glezerman, M. What to do after a failed attempt of vacuum delivery? Eur. J. Obstet. Gynecol. Reprod. Biol. 2003, 107, 151–155. [Google Scholar] [CrossRef]
- Bhide, A.; Guven, M.; Prefumo, F.; Vankalayapati, P.; Thilaganathan, B. Maternal and neonatal outcome after failed ventouse delivery, comparison of forceps versus cesarean section. J. Fetal Neonatal Med. 2007, 20, 541–545. [Google Scholar] [CrossRef]
- Wanyonyi, S.Z.; Achila, B.; Gudu, N. Factors contributing to failure of vacuum delivery and associated maternal/neonatal morbidity. Int. J. Gynaecol. Obstet. 2011, 115, 157–160. [Google Scholar] [CrossRef]
- Ebulue, V.; Vadalkar, J.; Cely, S.; Dopwell, F.; Yoong, W. Fear of failure, are we doing too many trials of instrumental delivery in theatre? Acta Obstet. Gynecol. Scand. 2008, 87, 1234–1238. [Google Scholar] [CrossRef]
- Chadwick, L.M.; Pemberton, P.J.; Kurinczuk, J.J. Neonatal subgalealhaematoma, associated risk factors, complications and outcome. J. Paediatr. Child. Health 1996, 32, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Teng, F.Y.; Sayre, J.W. Vacuum extraction, does duration predict scalp injury? Obstet. Gynecol. 1997, 89, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, O.; Silveira, R.; Zentner, A.; Dittmar, A.; Gaucherand, P.; Cucherat, M.; Redarce, T.; Rudigoz, R.-C. Birth simulator, reliability of transvaginal assessment of fetal head station as defined by the American College of Obstetricians and Gynecologists classification. Am. J. Obstet. Gynecol. 2005, 192, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Kalache, K.D.; Duckelmann, A.M.; Michaelis, S.A.; Lange, J.; Cichon, G.; Dudenhausen, J.W. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses, how well does the ‘angle of progression’ predict the mode of delivery? Ultrasound Obstet. Gynecol. 2009, 33, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Bultez, T.; Quibel, T.; Bouhanna, P.; Popowski, T.; Resche-Rigon, M.; Rozenberg, P. Angle of fetal head progression measured using transperineal ultrasound as a predictive factor of vacuum extraction failure. Ultrasound Obstet. Gynecol. 2016, 48, 86–91. [Google Scholar] [CrossRef]
- Sainz, J.A.; Borrero, C.; Aquise, A.; Serrano, R.; Gutierrez, L.; Fernandez-Palacın, A. Utility of intrapartum transperineal ultrasound to predict cases of failure in vacuum extraction attempt and need of cesarean section to complete delivery. J. Matern. Fetal Neonatal Med. 2016, 29, 1348–1352. [Google Scholar] [CrossRef]
- Cuerva, M.J.; Bamberg, C.; Tobias, P.; Gil, M.M.; De La Calle, M.; Bartha, J.L. Use of intrapartum ultrasound in the prediction of complicated operative forceps delivery of fetuses in non-occiput posterior position. Ultrasound Obstet. Gynecol. 2014, 43, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Kahrs, B.H.; Usman, S.; Ghi, T.; Youssef, A.; Torkildsen, E.A.; Lindtjørn, E.; Østborg, T.B.; Benediktsdottir, S.; Brooks, L.; Harmsen, L.; et al. Sonographic prediction of outcome of vacuum deliveries, a multicenter, prospective cohort study. Am. J. Obstet. Gynecol. 2017, 217, 69.e1–69.e10. [Google Scholar] [CrossRef]
- Kasbaoui, S.; Severac, F.; Aïssi, G.; Gaudineau, A.; Lecointre, L.; Akladios, C.; Favre, R.; Langer, B.; Sananès, N. Predicting the difficulty of operative vaginal delivery by ultrasound measurement of fetal head station. Am. J. Obstet. Gynecol. 2017, 216, 507.e1–507.e9. [Google Scholar] [CrossRef]
- Wong, G.Y.; Mok, Y.M.; Wong, S.F. Transabdominal ultrasound assessment of the fetal head and the accuracy of vacuum cup application. Int. J. Gynaecol. Obstet. 2007, 98, 120–123. [Google Scholar] [CrossRef]
- Haikin, E.H.; Mankuta, D. Vacuum cup placement during delivery a suggested obstetric quality assessment measure. J. Matern. Fetal Neonatal Med. 2012, 25, 2135–2137. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Mean ± SD or n (%) |
|---|---|
| Mean maternal age | 31.50 ± 5.92 |
| History of cesarean section | 12 (11.8%) |
| Gestational disease | 18 (17.8%) |
| Gestational diabetes | 3 2.9%) |
| Hypertensive state of pregnancy | 3 (2.9%) |
| Intrauterine growth restriction | 7 (6.9%) |
| Others | 7 (6.9%) |
| Gestational weeks at delivery | 39.57 ± 1.55 |
| Induced deliveries | 27 (26.7%) |
| Chronological prolonged pregnancy | 6 (5.9%) |
| Ruptured membranes | 8 (7.9%) |
| Intrauterine growth restriction | 6 (5.9%) |
| Hypertensive state of pregnancy | 3 (2.9%) |
| Others | 4 (3.9%) |
| Epidural analgesia | 101 (100%) |
| Number of operative deliveries (vacuum) | 101 (100%) |
| Indication of operative delivery | |
| Prolonged second stage | 69 (68.3%) |
| Others | 32 (31.7%) |
| Tear of cesarean section scar | 3 (2.9%) |
| Parameter | Mean ± SD or n (%) |
|---|---|
| Newborn sex (females) | 47 (46.5%) |
| Newborn weight in grams | 3.332 ± 422.44 |
| APGAR at 1 min | 8.80 ± 1.051 |
| APGAR at 5 min | 9.96 ± 0.268 |
| Newborn umbilical artery pH | 7.24 ± 0.782 |
| Perinatal mortality | 0 (0%) |
| Perinatal morbidity | 3 (2.9%) |
| Head laceration | 2 (1.9) |
| Head trauma | 1 (0.9%) |
| Admission to NICU | 2 (1.9%) |
| Fetal Head Position | Identified by TUS | Identified by DE | Correct Position (DE) | Incorrect Position (DE) | DE DR (DE/TUS) | DE FNR |
|---|---|---|---|---|---|---|
| Direct occiput anterior | 10 (9.9%) | 18 (17.8%) | 10/18 (55.6%) | 8/18 (44.4%) | 100.0% (10/10) | 0.0% (0/10) |
| Right occiput anterior | 19 (18.8%) | 11 (10.8%) | 11/11 (100%) | 0/11 (0.0%) | 57.9% (11/19) | 42.1% (8/19) |
| Right occiput transverse | 21 (20.7%) | 23 (22.7%) | 17/23 (73.9%) | 6/23 (26.1%) | 81.0% (17/21) | 19.1% (4/19) |
| Left occiput anterior | 26 (25.7%) | 25 (24.7%) | 22/25 (88.0%) | 3/25 (12.0%) | 84.6% (22/26) | 15.4% (4/26) |
| Left occiput transverse | 12 (11.8%) | 11 (10.8%) | 8/11 (72.7%) | 3/11 (27.3%) | 66.7% (8/12) | 33.3% (4/12) |
| Direct occiput posterior | 13 (12.8%) | 8 (7.9%) | 6/8 (75.0%) | 2/8 (25.0%) | 46.2% (6/13) | 53.9% (7/12) |
| Not possible | 0 (0%) | 5 (4.9%) | ||||
| Total | 74/96 (77.1%) | 22/96 (22.9%) | 73.3% (74/101) | 26.7% (27/101) |
| Level of Descent of the Fetal Head (Hodge’s Planes; Lee’s Stations; Angle of Progression) | DE | DE DR (DE/TUS) |
|---|---|---|
| High (I/II; −1/−3; AOP < 116°) | 5 (4.9%) | 3/5 (60%) |
| Medium (III; 0; AOP = 116°) | 22 (21.7%) | 15/22 (68.1%) |
| Low (IV ;+3; AOP > 148°) | 74 (73.2%) | 56/74 (75.7%) |
| Total | 101 (100%) | 74/101 (73.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garcia-Jimenez, R.; Valero, I.; Borrero, C.; Garcia-Mejido, J.A.; Fernandez-Palacin, A.; Serrano, R.; Sainz-Bueno, J.A. Can Intrapartum Ultrasonography Improve the Placement of the Vacuum Cup in Operative Vaginal Deliveries? Tomography 2023, 9, 247-254. https://doi.org/10.3390/tomography9010019
Garcia-Jimenez R, Valero I, Borrero C, Garcia-Mejido JA, Fernandez-Palacin A, Serrano R, Sainz-Bueno JA. Can Intrapartum Ultrasonography Improve the Placement of the Vacuum Cup in Operative Vaginal Deliveries? Tomography. 2023; 9(1):247-254. https://doi.org/10.3390/tomography9010019
Chicago/Turabian StyleGarcia-Jimenez, Rocio, Irene Valero, Carlota Borrero, Jose Antonio Garcia-Mejido, Ana Fernandez-Palacin, Rosa Serrano, and Jose Antonio Sainz-Bueno. 2023. "Can Intrapartum Ultrasonography Improve the Placement of the Vacuum Cup in Operative Vaginal Deliveries?" Tomography 9, no. 1: 247-254. https://doi.org/10.3390/tomography9010019
APA StyleGarcia-Jimenez, R., Valero, I., Borrero, C., Garcia-Mejido, J. A., Fernandez-Palacin, A., Serrano, R., & Sainz-Bueno, J. A. (2023). Can Intrapartum Ultrasonography Improve the Placement of the Vacuum Cup in Operative Vaginal Deliveries? Tomography, 9(1), 247-254. https://doi.org/10.3390/tomography9010019






