Comparing the Diagnostic Performance of ECG Gated versus Non-Gated CT Angiography in Ascending Aortic Dissection: A GRRAS Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Index Tests
2.3. Reference Tests
2.4. Statistical Analysis
3. Results
3.1. Agreement with Reference Tests
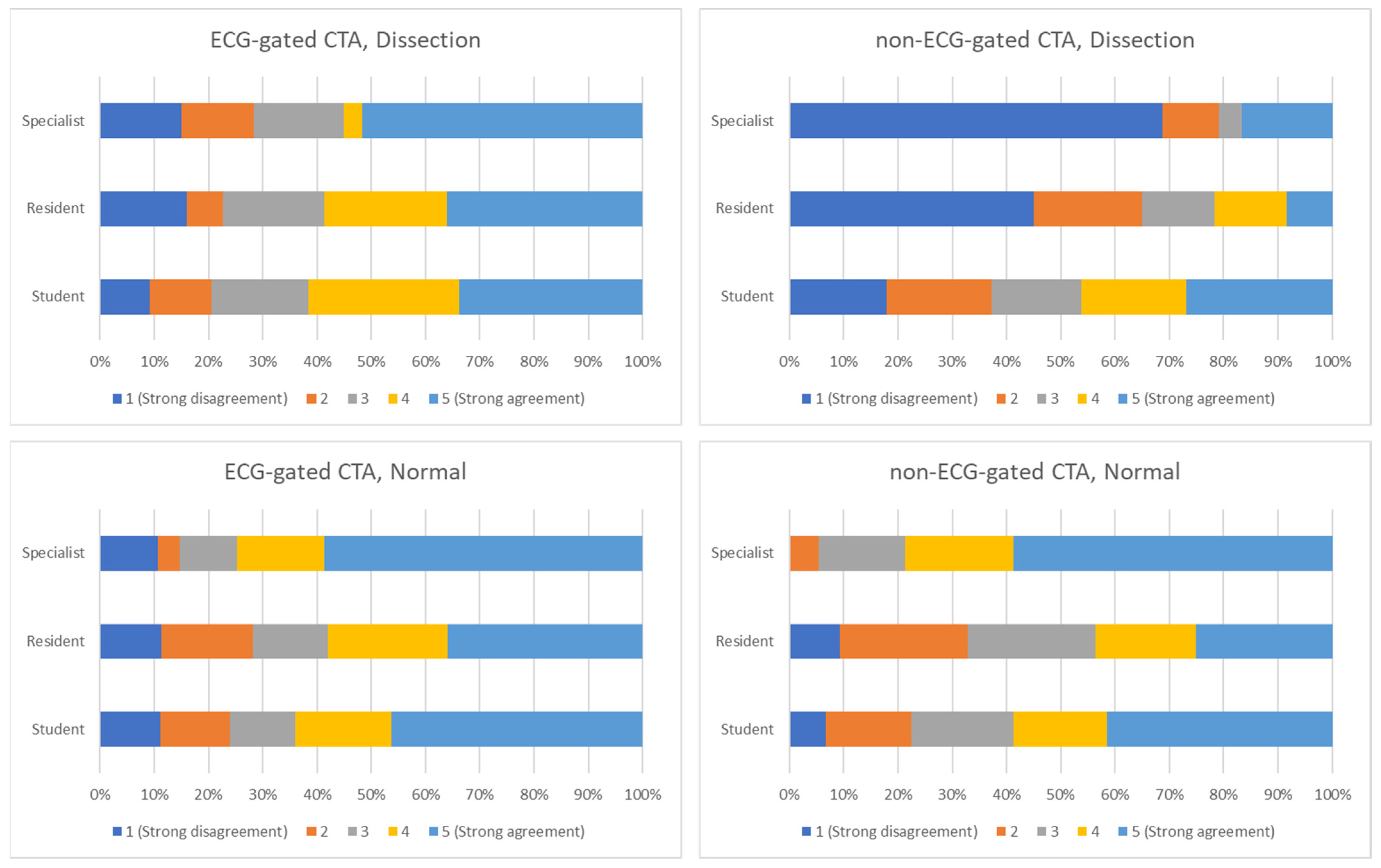
3.2. Inter-Rater Reliability
3.3. Intra-Rater Reliability
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fallenberg, E.; Juergens, K.; Wichter, T.; Scheld, H.H.; Fischbach, R. Coronary Artery Aneurysm and Type-A Aortic Dissection Demonstrated by Retrospectively ECG-Gated Multislice Spiral CT. Eur. Radiol. 2001, 12, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Hayter, R.G.; Rhea, J.T.; Small, A.; Tafazoli, F.S.; Novelline, R.A. Suspected Aortic Dissection and Other Aortic Disorders: Multi–Detector Row CT in 373 Cases in the Emergency Setting. Radiology 2006, 238, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, D.; Mitchell, R.S.; Miller, D.C. Acute Aortic Syndromes: New Insights from Electrocardiographically Gated Computed Tomography. Semin. Thorac. Cardiovasc. Surg. 2008, 20, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Vasile, N.; Mathieu, D.; Keita, K.; Lellouche, D.; Bloch, G.; Cachera, J.P. Computed Tomography of Thoracic Aortic Dissection. J. Comput. Assist. Tomogr. 1986, 10, 211–215. [Google Scholar] [CrossRef]
- Heiberg, E.; Wolverson, M.; Sundaram, M.; Connors, J.; Susman, N. CT Findings in Thoracic Aortic Dissection. Am. J. Roentgenol. 1981, 136, 13–17. [Google Scholar] [CrossRef]
- Godwin, J.D.; Herfkens, R.L.; Skiöldebrand, C.G.; Federle, M.P.; Lipton, M.J. Evaluation of Dissections and Aneurysms of the Thoracic Aorta by Conventional and Dynamic CT Scanning. Radiology 1980, 136, 125–133. [Google Scholar] [CrossRef]
- Gross, S.C.; Barr, I.; Eyler, W.R.; Khaja, F.; Goldstein, S. Computed Tomography in Dissection of the Thoracic Aorta. Radiology 1980, 136, 135–139. [Google Scholar] [CrossRef]
- Lardé, D.; Belloir, C.; Vasile, N.; Frija, J.; Ferrané, J. Computed Tomography of Aortic Dissection. Radiology 1980, 136, 147–151. [Google Scholar] [CrossRef]
- Thorsen, M.K.; San Dretto, M.A.; Lawson, T.L.; Foley, W.D.; Smith, D.F.; Berland, L.L. Dissecting Aortic Aneurysms: Accuracy of Computed Tomographic Diagnosis. Radiology 1983, 148, 773–777. [Google Scholar] [CrossRef]
- Burns, M.A.; Molina, P.L.; Gutierrez, F.R.; Sagel, S.S. Motion Artifact Simulating Aortic Dissection on CT. Am. J. Roentgenol. 1991, 157, 465–467. [Google Scholar] [CrossRef][Green Version]
- Godwin, J.D.; Breiman, R.S.; Speckman, J.M. Problems and Pitfalls in the Evaluation of Thoracic Aortic Dissection by Computed Tomography. J. Comput. Assist. Tomogr. 1982, 6, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Dake, M.D.; Wang, D.S. Will Stent-Graft Repair Emerge as Treatment of Choice for Acute Type B Dissection? Semin. Vasc. Surg. 2006, 19, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Dake, M.D.; Kato, N.; Mitchell, R.S.; Semba, C.P.; Razavi, M.K.; Shimono, T.; Hirano, T.; Takeda, K.; Yada, I.; Miller, D.C. Endovascular Stent–Graft Placement for the Treatment of Acute Aortic Dissection. N. Engl. J. Med. 1999, 340, 1546–1552. [Google Scholar] [CrossRef] [PubMed]
- Blanke, P.; Bulla, S.; Baumann, T.; Siepe, M.; Winterer, J.T.; Euringer, W.; Schäfer, A.-O.; Kotter, E.; Langer, M.; Pache, G. Thoracic Aorta: Prospective Electrocardiographically Triggered CT Angiography with Dual-Source CT—Feasibility, Image Quality, and Dose Reduction. Radiology 2010, 255, 207–217. [Google Scholar] [CrossRef]
- Wu, W.; Budovec, J.; Foley, W.D. Prospective and Retrospective ECG Gating for Thoracic CT Angiography: A Comparative Study. Am. J. Roentgenol. 2009, 193, 955–963. [Google Scholar] [CrossRef]
- Lee, J.; Jeong, Y.J.; Lee, G.; Kim, C.W.; Kim, J.Y.; Lee, N.K.; Lee, H.C.; Lee, J.W. Non-ECG-Gated High-Pitch CT Angiography versus Hybrid ECG-Gated CT Angiography for Aorta Using 512-Slice CT: Comparison of Image Quality and Radiation Dose. Acta. Radiol. 2022, 028418512210959. [Google Scholar] [CrossRef]
- Kim, T.J.; Lee, K.H.; Choe, Y.H.; Lee, K.S. Acute Aortic Diseases: Evaluation with Computed Tomography and Magnetic Resonance Imaging. In Emergency Chest Radiology; Springer Singapore: Singapore, 2021; pp. 63–88. [Google Scholar]
- Wong, Y.; Ong, C.; Liang, C.; Tan, C.; Teo, L. Image Quality, Contrast Enhancement and Radiation Dose of ECG-Triggered versus Non-ECG-Triggered Imaging of the Aorta on a Single Source 256-Slice CT Scanner. Singapore Med. J. 2021. [Google Scholar] [CrossRef]
- Nagpal, P.; Agrawal, M.D.; Saboo, S.S.; Hedgire, S.; Priya, S.; Steigner, M.L. Imaging of the Aortic Root on High-Pitch Non-Gated and ECG-Gated CT: Awareness Is the Key! Insights Imaging 2020, 11, 51. [Google Scholar] [CrossRef]
- Francone, M.; Budde, R.P.J.; Bremerich, J.; Dacher, J.N.; Loewe, C.; Wolf, F.; Natale, L.; Pontone, G.; Redheuil, A.; Vliegenthart, R.; et al. CT and MR Imaging Prior to Transcatheter Aortic Valve Implantation: Standardisation of Scanning Protocols, Measurements and Reporting—a Consensus Document by the European Society of Cardiovascular Radiology (ESCR). Eur. Radiol. 2020, 30, 2627–2650. [Google Scholar] [CrossRef]
- Blanke, P.; Weir-McCall, J.R.; Achenbach, S.; Delgado, V.; Hausleiter, J.; Jilaihawi, H.; Marwan, M.; Norgaard, B.L.; Piazza, N.; Schoenhagen, P.; et al. Computed Tomography Imaging in the Context of Transcatheter Aortic Valve Implantation (TAVI) / Transcatheter Aortic Valve Replacement (TAVR): An Expert Consensus Document of the Society of Cardiovascular Computed Tomography. J. Cardiovasc. Comput. Tomogr. 2019, 13, 1–20. [Google Scholar] [CrossRef]
- Kottner, J.; Audigé, L.; Brorson, S.; Donner, A.; Gajewski, B.J.; Hróbjartsson, A.; Roberts, C.; Shoukri, M.; Streiner, D.L. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) Were Proposed. J. Clin. Epidemiol. 2011, 64, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef] [PubMed]
- Kok, E.M.; de Bruin, A.B.H.; Robben, S.G.F.; van Merriënboer, J.J.G. Looking in the Same Manner but Seeing It Differently: Bottom-up and Expertise Effects in Radiology. Appl. Cogn. Psychol. 2012, 26, 854–862. [Google Scholar] [CrossRef]
- Waite, S.; Grigorian, A.; Alexander, R.G.; Macknik, S.L.; Carrasco, M.; Heeger, D.J.; Martinez-Conde, S. Analysis of Perceptual Expertise in Radiology–Current Knowledge and a New Perspective. Front. Hum. Neurosci. 2019, 13, 213. [Google Scholar] [CrossRef] [PubMed]
- Vardhanabhuti, V.; Nicol, E.; Morgan-Hughes, G.; Roobottom, C.A.; Roditi, G.; Hamilton, M.C.K.; Bull, R.K.; Pugliese, F.; Williams, M.C.; Stirrup, J.; et al. Recommendations for Accurate CT Diagnosis of Suspected Acute Aortic Syndrome (AAS)--on Behalf of the British Society of Cardiovascular Imaging (BSCI)/British Society of Cardiovascular CT (BSCCT). Br. J. Radiol. 2016, 89, 20150705. [Google Scholar] [CrossRef]
- Pop, M. Cardiothoracic CTA in Infants Referred for Aortic Arch Evaluation-Retrospective Comparison of Iomeprol 350, Ioversol 350, Iopromide 370 and Iodixanol 320. Children 2021, 8, 949. [Google Scholar] [CrossRef]
- Pop, R.-M.; Tenenboum, A.; Pop, M. Secular Trends in Height, Body Mass and Mean Menarche Age in Romanian Children and Adolescents, 1936-2016. Int. J. Environ. Res. Public Health 2021, 18, 490. [Google Scholar] [CrossRef]
- Wagner, M.; Butler, C.; Rief, M.; Beling, M.; Durmus, T.; Huppertz, A.; Voigt, A.; Baumann, G.; Hamm, B.; Lembcke, A.; et al. Comparison of Non-Gated vs. Electrocardiogram-Gated 64-Detector-Row Computed Tomography for Integrated Electroanatomic Mapping in Patients Undergoing Pulmonary Vein Isolation. Europace 2010, 12, 1090–1097. [Google Scholar] [CrossRef]
- Sun, Z. Coronary CT Angiography with Prospective ECG-Triggering: An Effective Alternative to Invasive Coronary Angiography. Cardiovasc. Diagn. Ther. 2012, 2, 28–37. [Google Scholar] [CrossRef]


| Medical Students (n = 39) | Radiology Residents (n = 15) | Radiology Consultants (n = 12) | |
|---|---|---|---|
| Median age (IQR) | 25 (24–26) | 28 (27–29.5) | 37 (34.5–38) |
| Male to female ratio | 1.16 | 0.36 | 0.5 |
| Years of CT training: Less than 1 1 to 5 years More than 5 years | 30 9 | 6 9 | 7 5 |
| ECG Gated Images ICC (95% CI) | Non-ECG Gated Images ICC (95% CI) | |
|---|---|---|
| Students | 0.319 (0.162–0.644) | 0.173 (0.078–0.417) |
| Residents | 0.481 (0.269–0.783) | 0.26 (0.117–0.552) |
| Specialists | 0.498 (0.273–0.797) | 0.227 (0.087–0.52) |
| ECG Gated Images ICC (95% CI) | NON-ECG Gated Images ICC (95% CI) | |
|---|---|---|
| Students vs. Residents | 0.425 (0.272–0.556) | 0.166 (0.006–0.317) |
| Students vs. Specialists | 0.452 (0.275–0.596) | 0.1 (0.01–0.117) |
| Residents vs. Specialists | 0.657 (0.535–0.752) | 0.291 (0.128–0.439) |
| ICC ECG Gated Images (95% CI) | ICC Non-ECG Gated Images (95% CI) | |
|---|---|---|
| Students | 0.692 (0.584–0.775) | 0.637 (0.516–0.733) |
| Residents | 0.711 (0.53–0.83) | 0.807 (0.675–0.889) |
| Specialists | 0.82 (0.676–0.9) | 0.593 (0.332–0.499) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Budeanu, R.G.; Broemmer, C.; Budeanu, A.R.; Pop, M. Comparing the Diagnostic Performance of ECG Gated versus Non-Gated CT Angiography in Ascending Aortic Dissection: A GRRAS Study. Tomography 2022, 8, 2426-2434. https://doi.org/10.3390/tomography8050201
Budeanu RG, Broemmer C, Budeanu AR, Pop M. Comparing the Diagnostic Performance of ECG Gated versus Non-Gated CT Angiography in Ascending Aortic Dissection: A GRRAS Study. Tomography. 2022; 8(5):2426-2434. https://doi.org/10.3390/tomography8050201
Chicago/Turabian StyleBudeanu, Razvan G., Christian Broemmer, Anamaria R. Budeanu, and Marian Pop. 2022. "Comparing the Diagnostic Performance of ECG Gated versus Non-Gated CT Angiography in Ascending Aortic Dissection: A GRRAS Study" Tomography 8, no. 5: 2426-2434. https://doi.org/10.3390/tomography8050201
APA StyleBudeanu, R. G., Broemmer, C., Budeanu, A. R., & Pop, M. (2022). Comparing the Diagnostic Performance of ECG Gated versus Non-Gated CT Angiography in Ascending Aortic Dissection: A GRRAS Study. Tomography, 8(5), 2426-2434. https://doi.org/10.3390/tomography8050201





